Anaphylactic shock is a condition that develops suddenly as a result of exposure to an allergen, poses a threat to life, causes circulatory disorders, leading to the development of vascular insufficiency and hypoxia of all vital organs.
Epidemiology
Among all allergic diseases, the frequency of this pathology is about 5%. People with a predisposition to allergies are much more likely to experience shock than others. The mortality rate from this disease is about 4%.
Causes
Anaphylactic shock is manifestation of the mechanism of anaphylaxis, which is caused by sensitization and increased sensitivity of the body to the action of various allergens. The factors that most often cause the development of AS include: various drugs (about 20% of all cases of shock, most often antibiotics and non-steroidal anti-inflammatory drugs), poisons of hymenoptera insects (about 3%, mainly bees and wasps), latex (0 .5% of cases in the population), food allergens (egg white, milk, peanuts, soy), pollen, bacterial allergens, serums and vaccines. True shock occurs when an allergen enters the human body a second time; the first contact with it, as a rule, occurs unnoticed.
What is anaphylactic shock? pathogenesis point of view?
AS is an extreme degree of severity of an anaphylactic reaction or excessive sensitivity of the body to substances foreign to it. Its mechanism belongs to the category of allergic reactions of immediate development or IgE-mediated.
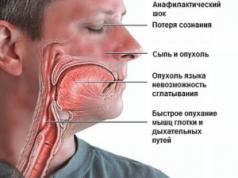
The basis for the development of shock will be a sudden drop in vascular tone, as a result of the influence of histamine and other mediators, and dilation of the veins. This leads to a relative decrease in the volume of blood circulating through these vessels and the emergence of a discrepancy between it and the volume of the vascular bed. There is a drop in the filling of the veins, which causes a decrease in the amount of blood that flows to the heart, a decrease in the filling of the heart chambers, a decrease in cardiac output and a drop in blood pressure. Violation of the pumping function of the heart also contributes to a direct violation of the ability of the heart muscle to contract.
All of the above factors lead to a deterioration in blood circulation in small capillary vessels, resulting in a problem with the delivery of oxygen and nutrients, and the removal of products formed during the metabolic process. This causes the development of hypoxia and disruption of microcirculation of organs and tissues. In addition, as a result of exposure to active biological substances, there is a rapid increase in the permeability of surface membranes in the cell, which leads to the occurrence of tissue edema (primarily in the brain and lung tissue) due to the transition of the liquid component of the blood into the interstitial space. It also causes blood to thicken and further reduce the volume of circulating blood. Against this background, in parallel, spasm of the larynx, as well as large and small bronchi, develops very quickly, which is manifested by the appearance of clinical signs of acute respiratory failure. In addition to the above, spasms of the smooth muscles of the intestines, bladder and uterus are also characteristic.
Classification
Depending on the nature of clinical symptoms, there are five main forms of anaphylactic shock:
- Hemodynamic, the clinical picture of which is dominated by signs of dysfunction of the cardiovascular system;
- Asphyxial - the main clinical manifestation will be the development of acute respiratory failure;
- Abdominal - characterized by abdominal pain;
- Cerebral, in which signs of impaired cerebral blood flow dominate;
- With damage to mucous membranes and skin.
Based on the nature of the shock, there are:
- Acute malignant shock;
- Benign;
- Protracted;
- Recurrent;
- With an erased flow.
Clinical
This pathology is characterized by a sharp and sudden onset, the time for the development of a pronounced clinical picture is usually several seconds. Although in some cases it can take a couple of hours. The main signs of shock are caused by the development of blood flow disturbances and a drop in blood pressure, which can be wave-like. In addition, symptoms of dysfunction in other organs and systems are also characteristic:

After relief of the shock state, over the next three to four weeks the patient may retain signs of changes in function in various organs and their systems.
Delayed reactions of the allergic type, various pathological processes in the central nervous system, myocarditis of allergic etiology, glomerulonephritis, inflammation of blood vessels (vasculitis), nerve damage (neuritis), etc. may occur. That is why these patients require longer and enhanced medical supervision.
There are four degrees of severity of anaphylactic shock, which depend on the nature and severity of blood flow disturbance:

- Grade 1 AS is characterized by a decrease in blood pressure by no more than forty mm. Hg Art. from its normal value. Precursors of the development of shock may appear: skin itching, rashes, cough, sore throat, etc. The patient’s consciousness is preserved, while he may be excited or lethargic, characterized by depression, anxiety, and fear of death. The skin turns red, urticaria and Quincke's edema may appear on it. A cough is also common. At this stage, all symptoms are easily relieved with the help of drugs from the groups of sympathomimetics and glucocorticoids;
- Stage 2 severity of anaphylactic shock: blood pressure drops below one hundred mm. Hg Art., but above 60 mm. Hg Art. Consciousness at this stage is still preserved or is lost, but not immediately. A prodromal period may develop with the appearance of anxiety, fear of death, weakness, itching, urticaria, Quincke's edema, hoarseness (up to its complete disappearance), difficulty swallowing, dizziness, headache, tinnitus, paresthesia. Pain syndrome may also occur with pain localized in the abdomen, lower back and around the heart. Upon examination, you can see pale skin, often with a bluish tint, shortness of breath, difficulty breathing, pulmonary wheezing, and an increase in heart rate. Vomiting and involuntary passage of urine and feces as a result of relaxation of the sphincters of the rectum and bladder are also likely;
- Stage 3 shock is characterized by loss of consciousness, which occurs very quickly, blood pressure drops below 60 mm. Hg Art. Very often, tonic and clonic convulsions occur, the patient becomes covered in sticky and cold sweat, the lips turn blue, and the pupils dilate. Heart sounds become muffled, the heart rhythm becomes irregular, the pulse becomes threadlike. At this stage, therapy rarely gives a positive result;
- Stage 4 anaphylactic shock is characterized by rapid development with immediate loss of consciousness, blood pressure cannot be measured, heart sounds cannot be heard, and there is no breathing. At this stage, there is practically no response to therapy with sympathomimetics and glucocorticoids.
treatment-simptomy.ru
The first signs of anaphylactic shock
Compared to the body’s usual negative reaction to an allergen, anaphylaxis is characterized by a tenfold increase in the rate of pathological changes in the victim’s body, as well as their severity. Almost all vital systems are affected:
- respiratory;
- circulatory;
- heart;
- skin;
- brain;
- mucous membranes.
Anaphylactic shock is especially dangerous for children who have not yet sufficiently developed all body systems, and also because of the narrowness of the respiratory lumen.
The table below discusses the characteristics of symptoms of anaphylaxis depending on exposure to the allergen.
| Symptoms of anaphylactic shock | ||
| Classification | Form | Symptoms |
| Localization | Typical | Skin swelling, difficulty breathing, disruption of the circulatory system. |
| Asphyxial | Spasm of the respiratory tract, swelling of the larynx and other respiratory organs, asphyxia. | |
| Cerebral | Damage to the central nervous system, up to cerebral edema (behavioral disturbances, excitability, fatigue). | |
| Abdominal | From the gastrointestinal tract there are all signs of poisoning (pain, vomiting, stool disturbances, nausea, flatulence, heartburn, belching, weakness, irritability). | |
| Hemodynamic | Disruption of the cardiovascular system (chest pain of varying nature and severity, interruptions in heart function, shortness of breath, swelling, changes in skin color, headaches and dizziness). | |
| Heaviness | 1 type | Blood pressure is below normal (systolic 110/120 and diastolic 70/90) by 30-40 units. The victim is conscious, but in a state of panic, there is a fear of death. Drug antishock treatment was successful on the first attempt. |
| Type 2 | Blood pressure is below normal (systolic 110/120 and diastolic 70/90) by 40-60 units. There is a possibility of loss of consciousness, which is confused. Numbness. The response to antishock therapy is good. | |
| Type 3 | The pressure is below normal and cannot be determined by the meter (systolic 110/120 and diastolic 70/90) by 60-80 units. The victim is on the verge of losing consciousness. Very weak response to antishock therapy. | |
| 4 type | Pressure cannot be determined. The victim is unconscious. There is no response to drug antishock therapy. | |
| Speed | Malignant-acute | A sudden and significant drop in pressure, bronchospasm, respiratory failure, confusion, pulmonary edema, skin rashes, possible coma and death. |
| Benign-acute | Manifestations from various body systems reach their peak (respiratory failure, skin manifestations, gastrointestinal disorder, central nervous system dysfunction) and gradually subside in response to timely anti-shock treatment. | |
| Abortive | Very mild manifestations, mainly from the respiratory system. Symptoms often go away without the use of medications. | |
| Protracted | All the symptoms of typical anaphylactic shock appear, but the response to treatment is weak. A relapse occurs with a sharp drop in pressure and other signs of anaphylaxis. | |
| Lightning fast | Symptoms appear within seconds (up to half a minute) and the condition worsens too quickly for therapy to be successful. There is a chance to survive only if adrenaline and other medications are administered almost simultaneously with the allergen. | |
Anaphylactic shock: emergency care
Anaphylactic shock is an allergic reaction in which providing assistance in the first minutes of the onset of negative symptoms can help the patient survive.
Emergency care for anaphylaxis is divided into pre-medical and medical (a table with the main algorithm of actions is presented below).
| Type of "emergency" | Algorithm of actions |
| First aid | 1. Ensuring normal blood flow (especially to the heart). To do this, the victim is placed on a flat surface, and his legs are raised above body level, using a roller made of clothing or other objects. 2. Ensuring the flow of oxygen and stopping the action of the allergen. To do this, open all the windows in the room where the patient is, and unbutton his clothes. 3. Call an ambulance. 4. Checking the victim’s mouth for displaced dentures that are interfering with breathing. If he has a recessed tongue, then you need to place a hard object between the teeth and turn your head to the left or right. 5. If the allergen entered the patient’s bloodstream through an injection or insect bite, then the area above the area of exposure should be tied with a tourniquet. Apply ice to the manipulation area. 6. Tell the emergency doctors about all the actions taken and the symptoms observed. |
| Health care | 1. Administration of adrenaline solution in various ways, depending on the severity of the patient’s condition. Injection of the injection or bite site with a solution of adrenaline (0.1% at 4-6 points in a circle). 2. Intravenous or infusion administration of one of the following drugs: prednisolone, hydrocortisone or dexamethasone. 3. Introduction of a large volume of sodium chloride into the patient’s body (depending on the patient’s weight). 4. Inhalation of oxygen to the patient through a special mask. If necessary, a tracheotomy is performed. 5. Administration of antihistamines (with caution). 6. Observe the patient in the hospital for a week to avoid relapse. |
What are the consequences of anaphylactic shock?
In addition to a possible relapse within 2-3 days, anaphylactic shock entails the following ailments:
- kidney disease (glomerulonephritis);
- bronchial asthma (chronic form);
- disturbances in the functioning of the central nervous system;
- toxic nerve pathology (polyneuropathy);
- inflammation of the heart muscle (myocarditis);
- bleeding in the gastrointestinal tract;
- bronchospasms;
- pulmonary edema;
- cerebral edema;
- cerebral hemorrhage;
- to whom.
A victim of anaphylaxis can only be helped if immediate medical attention is provided. Healthy people who have relatives with allergies of any type need to be prepared for this severe reaction and take preventive measures (attentiveness to food and medications, caution during the seasonal flowering of certain plants, etc.).
oballergiya.ru
State of shock
 Symptoms of anaphylactic shock
Symptoms of anaphylactic shock As you know, at the moment almost every second person on earth suffers from allergies. This can be a chronic form, in which the patient constantly experiences allergy symptoms, and sometimes an acute reaction appears only once and never overtakes the person again. But there are conditions that are not similar to a typical allergic reaction, and yet they can be fatal.
Shock is a state of the body in which it is under severe stress and cannot function normally. Metabolic processes in the brain are disrupted, which lead to irreversible consequences. Every fifth person who experiences this condition dies from anaphylactic shock, since symptoms develop very quickly, and first aid is often not provided at the right time. That is why it is worth knowing in detail what this condition is, how to recognize the first signs of anaphylaxis and help a person.
Causes of anaphylaxis
 Chocolate is a strong allergen
Chocolate is a strong allergen Most often, anaphylactic shock is caused by poison entering the body. This could be a snake bite, an insect bite, or the penetration of chemicals. Currently, cases of anaphylaxis after the administration of medications, as well as due to doctors’ errors during blood transfusions, immunotherapy, provocative tests and other manipulations, have become more frequent.
The main causes of anaphylactic shock:
Very often, foods cause severe reactions. Most often, such allergens are: chocolate, nuts, milk, citrus fruits. A person may have a very strong individual intolerance to a particular product. There are many cases of anaphylactic shock when eating peanut butter or chocolate. Moreover, this reaction most often develops in children. According to statistics, by the age of 16, those children who had allergies in childhood, but did not come into contact with a dangerous substance for many years, tolerate it normally in their youth.
In addition, there are a number of factors that influence susceptibility to anaphylaxis. These include bronchial asthma, Quincke's edema, eczema, and allergic rhinitis. If a person experiences frequent acute allergic reactions, there is a risk that anaphylactic shock may develop. If a person is constantly in contact with an allergen, this contributes to a state of shock. The longer the contact is, the lower the risk becomes. Therefore, prevention of anaphylactic shock includes complete avoidance of contact with allergens and constant monitoring by a doctor.
Pathogenesis of the disease
Anaphylaxis is based on hypersensitivity, and it has a lightning-fast character. Symptoms can develop in just a few minutes. In rare cases, anaphylactic shock develops up to 5 hours, and the longer the symptoms take to develop, the easier it is to save the person.
The main and significant symptom of anaphylactic shock is poor circulation due to the active production of histamine and other substances. As a result, blood pressure drops to critical levels, brain starvation occurs, the person often loses consciousness, and convulsions may begin.
The reaction mainly develops from a large dose of the allergen (from bites or injections), as well as upon repeated contact, when antibodies combine with newly received allergens and spread internally through the bloodstream. The longer a person is in contact with a substance, the greater the likelihood of shock. Treatment of anaphylactic shock is a long and difficult process, with assistance in the first minutes of the onset of anaphylaxis playing a key role.
Types of anaphylaxis
There are several varieties of this condition:
Let us dwell in more detail on anaphylactic shock itself and its types.
Lightning Shock
This condition develops very quickly, literally in a few minutes, and the person feels a sharp deterioration in health. If you do not get your bearings in time and do not start emergency care, a rapid onset of death is possible.
Every fifth person dies from this condition because those around them do not have time to provide help.
Characterized by the following symptoms:
Lightning shock may not even be accompanied by the usual allergy symptoms, so it is very difficult to distinguish it from other types of shock conditions. It is necessary to devote all efforts to maintaining the patient’s stable condition, immediately call an ambulance and not panic.
Acute anaphylactic shock
 Anaphylactic shock headaches are more common in older people
Anaphylactic shock headaches are more common in older people With anaphylactic shock, the condition begins to develop like a typical allergy. Within a few minutes the following symptoms appear:
After all these symptoms, shock becomes lightning fast if the necessary assistance is not provided at the first stage. With an acute anaphylactic reaction, the chances of saving the patient's life are much higher, since anaphylaxis is easier to recognize and symptoms develop more slowly. However, this does not reduce the danger, so an ambulance should be called immediately.
Subacute anaphylactic shock
If we compare the prognosis for the course of the disease, then this type of shock is the most favorable, since in this case the symptoms develop even more slowly than in the acute form. The person manages to take antihistamines or limit contact with the allergen. If this does not happen, the reaction develops further, moving along the chain into acute and then lightning fast. This is why preventing anaphylactic shock is so important. If you notice allergy symptoms, take immediate action to prevent the condition from getting worse, otherwise it can lead to dire consequences.
First aid
In case of anaphylactic shock, first aid plays a key role, which must be provided to the person who is next to the victim. This will help save a person’s life and maintain his condition until the ambulance arrives.
The algorithm of actions is as follows:
First aid
This stage is carried out by an ambulance team that arrives on call. First of all, doctors administer a dose of adrenaline and prednisole to the victim in order to stop the development of anaphylactic shock. Further measures are carried out on the way to the hospital. It is necessary to provide the patient with access to oxygen if the airways become swollen. For this, doctors use aminophylline, which is administered intravenously by stream or drip. If measures do not help, opening the trachea and artificial ventilation of the lungs is possible. The patient is given a large dose of hormonal drugs to stabilize the condition. Further measures are carried out in a hospital setting.
Inpatient treatment of anaphylactic shock
 Dropper for purifying blood from antibodies
Dropper for purifying blood from antibodies At this stage, doctors direct all efforts to stabilize metabolic processes, since the consequences of anaphylactic shock can lead to irreversible changes in the brain. The patient is prescribed droppers that cleanse the blood of antibodies, as well as therapy, which includes taking antihistamines as prescribed by a doctor, anti-inflammatory drugs, and other medications. It is necessary to completely restore all functions of the internal organs and establish the reason why such a reaction occurred.
When the patient returns to normal, it is necessary to conduct a diagnosis to identify which substances caused anaphylactic shock. If these were medications, this data should be entered into the medical record so that there is no relapse. You will have to stay away from provoking foods. During recovery, a hypoallergenic diet is prescribed so that nothing provokes the production of histamine in the body.
It should be remembered: the most common reason leading to anaphylactic shock is self-administration of medications without the consent of a doctor. You should not self-medicate, it can be very dangerous!
Sometimes such a reaction is caused by provocative tests, which are carried out under the careful supervision of doctors, only in a hospital setting. Such studies are not prescribed to young children, and adults are warned in advance what the consequences may be. However, if anaphylaxis develops, doctors are ready to immediately provide the necessary assistance to stabilize the patient’s condition.
Allergies are a very dangerous disease if not taken seriously. Even the slightest ailments can develop into dangerous conditions, such as anaphylactic shock, so you need to monitor your body, do not neglect the advice of doctors and do not prescribe any medications yourself.
allergiyainfo.ru
Features of the disease
Anaphylactic shock (anaphylaxis, allergic shock) is an acute, rapidly developing pathological reaction of the body in response to an attack (shock) of allergens, in which all systems and organs experience extremely pronounced painful changes, often incompatible with life (every 5 - 10 patient). The speed of all processes characteristic of a banal allergy, in the case of shock, accelerates, and their severity increases tens of times.
Affected:
- all organs and respiratory tracts, vessels and capillaries;
- brain, heart;
- organs of the gastrointestinal system;
- skin and mucous membranes.
The video below will tell you what anaphylactic shock is:
Children
Anaphylaxis poses a particular danger to the child’s body due to the insufficient development of many systems and organs, protective function, anatomical and physiological characteristics. For example, swelling of the larynx in a child is a critical condition, since the respiratory lumen is extremely small and swelling of the mucous membrane to a thickness of only 1 mm will easily block the access of air to a newborn and infant.
At this age, vaccinations and medications often provoke an acute allergic reaction. But if in adults shock usually occurs during the secondary penetration of allergens into the blood, then in children anaphylaxis can develop upon first contact with the provocateur of allergic shock, if the mother used a certain medication during pregnancy and breastfeeding, and it passed through the placenta or milk into the blood. baby's blood. Moreover, neither the dose nor the method of administration of the pharmacological agent matters if the child is already sensitized (has increased sensitivity to a specific substance).
In addition, children are more likely to develop anaphylaxis to foods.
Pregnancy
 Pregnancy also creates special vulnerabilities for the expectant mother and fetus. With the overload experienced by the heart and vascular system during anaphylaxis, the likelihood of miscarriages, early placental abruption, premature birth and intrauterine death is very high. The pregnant woman herself is also at risk for catastrophic bleeding, stroke, respiratory failure, and heart failure.
Pregnancy also creates special vulnerabilities for the expectant mother and fetus. With the overload experienced by the heart and vascular system during anaphylaxis, the likelihood of miscarriages, early placental abruption, premature birth and intrauterine death is very high. The pregnant woman herself is also at risk for catastrophic bleeding, stroke, respiratory failure, and heart failure.
Read about the types and forms of anaphylactic shock below.
Classification
According to flow forms
Classification according to the forms of anaphylactic shock (AS) is based on key signs of disorder of specific systems and target organs, which are the main targets of allergen aggression.
According to the course, anaphylaxis is divided into forms:
- Typical. It occurs most often, accompanied by dysfunction of blood vessels, organs and respiratory tracts, skin and subcutaneous edema.
- Hemodynamic. Accompanied by impaired blood circulation, insufficient functioning of the myocardium and heart vessels.
- Asphyxial, with the dominance of manifestations of acute respiratory failure, swelling and spasms of the respiratory tract, reaching the degree of asphyxia (suffocation).
- Abdominal or gastrointestinal form with symptoms of acute poisoning, “acute abdomen,” diseases of the stomach and intestines.
- Cerebral, with characteristic lesions of the central trunks of the nervous system, cerebral vessels, developing to cerebral edema.
- Form of AS, provoked physical overload.
According to severity
The severity of the pathology according to the criteria:
| Basic criterion | Severity | |||
|---|---|---|---|---|
| I | II | III | IV | |
| Blood pressure in mm Hg. Art. | below the normal value 110 – 120 / 70 – 90 by 30 – 40 units | Systolic (upper) 90 – 60 and below, diastolic (lower) 40 and below | Upper 60 – 40, lower - up to 0 (not determined during measurement) | Not defined |
| Consciousness | Saved. Severe panic, fear of death | Confused consciousness, state of stupor (numbness), possibility of loss of consciousness | High risk of loss of consciousness | Sudden loss of consciousness |
| Patient's response to antishock treatment | Active | Good or satisfactory | Weak | Weak or absent |
The severity of the shock determines the time of onset of the first signs. The sooner symptoms begin to appear from the moment the allergen enters the body, the more severe the manifestations of anaphylaxis.
By type of flow
Classification of AS according to the type of flow:
| Leakage / type | Peculiarities |
|---|---|
| Acute malignant. More common in the typical form. |
|
| Acute benign | The main pathological manifestations are quite pronounced. But during therapy they are not characterized by an increase, they can be reversed and subside. A favorable prognosis is highly likely with emergency treatment. |
| Abortive | Pathological symptoms are mild and quickly suppressed, often without the use of drugs. Occurs in asthma patients taking hormones (Prednisolone, Dexamethasone). |
| Lingering | Both types are characterized by:
Treatment for a protracted type of course gives a temporary, partial effect. The relapsing course is characterized by a secondary sharp drop in blood pressure after it has stabilized and the patient has recovered from the acute condition. The remaining symptoms are not as pronounced as in acute types of pathology, but are difficult to respond to therapy. It is more often observed when patients take long-acting medications (for example, Bicillin) for a long time. |
| Recurrent | |
| Lightning fast | Lightning-fast development of an anaphylactic reaction - within 10 – 30 seconds. More often this happens when the medicine is injected into a vein. The prognosis is disappointing. A favorable outcome is possible only with the equally immediate administration of adrenaline and other antishock agents. |
Read more about the causes of anaphylactic shock.
Causes
Development mechanism
Stage I
Sensitization (abnormal increase in sensitivity to a specific allergen substance).
The initial ingress of an allergen is perceived by the immune system as the penetration of a foreign agent, to which special protein compounds are produced - immunoglobulins E, G, after which the body is considered sensitized, that is, ready for a sharp allergic reaction when the allergen is reintroduced. Immunoglobulins bind to immune (mast) cells.
Stage II
 Directly - an anaphylactic reaction.
Directly - an anaphylactic reaction.
When the allergen enters the blood again, immunoglobulins immediately come into contact with it, after which specific substances are released from mast cells that regulate allergic and inflammatory reactions, the main of which is histamine. It causes swelling, itching, vasodilation - and, as a result, a drop in pressure and breathing problems. During anaphylactic shock, histamine is released simultaneously and in a huge volume, which leads to catastrophic disruption of the functioning of all organs.
Main reasons
Among the many reasons for the development of AS, they include, firstly, the administration of drugs, including:
- antibiotics (penicillin, aminoglycosides, Metronidazole, Trimethoprim, Vancomycin);
- Aspirin, other non-hormonal anti-inflammatory drugs (NSAIDs);
- ACE inhibitors (drugs for hypertension - Enalapril, Fosinopril, Captopril, even if the medicine had been taken for several years before);
- sulfonamides, iodinated drugs, B vitamins;
- plasma expanders, iron supplements, nicotinic acid, No-spa, immunoglobulins.
Other reasons for the development of AS:
Risk factors:
- Existing allergic diseases (urticaria, atopic dermatitis, allergic rhinitis)
- Chronic diseases of the respiratory organs, including asthma, chronic pneumonia, bronchitis, bronchial obstruction).
- Diseases of the heart and blood vessels
- The presence of previous anaphylactic reactions.
- Concomitant treatment of the patient with the following drugs:
- beta-blockers (the reaction of the respiratory tract to histamine, bradykinin increases and the effect of adrenaline used to bring the patient out of shock decreases).
- MAO inhibitors (suppress the enzyme that breaks down adrenaline, thus increasing the side effects of adrenaline).
- ACE inhibitors (can cause swelling of the larynx, tongue, pharynx with the development of suffocation, “Capoten cough”).
Signs of anaphylactic shock

Symptoms
The initial manifestations of the rapid development of anaphylaxis are observed already in the first seconds after the allergen enters the blood. This usually happens when the medicine is injected into a vein. The typical increase in symptoms ranges from 5 to 40 minutes.
But a two-phase course of anaphylactic shock is often observed, when after all the signs subside against the background of intensive treatment, after a day or three, a second wave of anaphylaxis may suddenly begin.
The basic symptoms of anaphylactic shock are often combined or manifested in a complex manner - in accordance with the forms of AS:
| Frequency of manifestations | Signs |
|---|---|
| 9 times out of 10 |
|
| In half of the patients |
|
| In a third of patients |
|
| Each has 3–4 patients |
|
| In 5 – 10% of anaphylaxis: |
|
Diagnostics
If episodes of an anaphylactic reaction have never been detected in a patient before, then studies are not able to predict its manifestation in the future, that is, to predict its development. However, the probability of its occurrence can be predicted to one degree or another:
- absolutely everyone who suffers from any form of allergy;
- in people whose relatives (especially parents) have experienced a similar experience of anaphylaxis.
Since anaphylaxis is a condition in which all manifestations increase very quickly, the diagnosis is most often made already during the development of the pathology, based on the speed of development of symptoms, and even more often - after treatment or death. Since delay in such a situation leads to the death of the patient, a detailed study of each symptom at this moment is impossible and simply extremely dangerous.
The danger of a false diagnosis
On the other hand, due to lack of time and lack of professionalism, false diagnoses are often made.
- For example, with the development of gastrointestinal (abdominal form) anaphylaxis, all the signs are very similar to the symptoms of acute poisoning, appendicitis, pancreatitis, biliary colic.
- In the hemodynamic form, with its severity of heart pain and manifestations of insufficiency, the person is diagnosed with myocardial infarction.
- Bronchial spasms, shortness of breath and even swelling of the larynx are considered signs of an asthmatic attack, and brain and neurological disorders are considered to be strokes, meningitis and other diseases that have nothing to do with anaphylactic shock.
Such false diagnoses are deadly for the patient, since there is simply no time left for proper treatment.
Actions for AS

Identifying the problem
Identification of the aggressor allergen that caused anaphylactic shock is a very important stage that should be included directly in the treatment of the pathology. If the patient has not experienced allergic reactions, special studies are carried out. They are able to confirm the diagnosis of allergization of the body as a whole, as well as the causative allergen in a specific case of anaphylaxis.
Among them are:
- skin, skin, patch tests (Patch test);
- blood test for the presence of immunoglobulins E (IgE), responsible for allergic reactions;
- provocative tests.
To ensure the safety of the patient's health in the event of a sharp response to an allergy provocation, all studies are carried out with a high degree of caution. The safest radioimmunological method is considered to be the allergen sorbent test (RAST), which most accurately determines the anaphylactic allergen without affecting the structure of the body.
Safety is ensured by conducting the analysis outside the patient’s body. Different types of allergens are added alternately to the blood taken from the patient. If, after the next interaction of blood with an allergen, an abnormal amount of antibodies is released, this indicates this allergen as the cause of an anaphylactic reaction.
This video will tell you about first aid for anaphylactic shock:
Treatment
In the hospital - in the intensive care unit and intensive care unit, the main treatment of anaphylactic shock is carried out.
Basic principles
Basic principles of treatment of anaphylactic shock:
- Elimination of serious dysfunctions in the functioning of the heart muscle, blood vessels, respiratory and nervous systems.
- Prevention of a sudden drop in pressure and the development of coma.
- Prevention of pulmonary edema, cerebral edema, asphyxia, cardiac arrest.
- Removing life-threatening edema of the larynx, trachea, and bronchi.
- Suppression of further releases of histamine, bradykinin, kallikrein and removal of allergen substances from the blood.
We will talk further about whether adrenaline is administered for anaphylactic shock and what other medications are needed.
Activities and medications
- Intramuscular injections of Adrenaline (epinephrine) 0.1% after 10 - 15 minutes, 0.2 - 0.8 ml. When calculating children's doses, take into account the norm of 0.01 mg (0.01 ml) per kilogram of the baby's weight. If a positive reaction does not occur, administer intravenous injection of 1 ml of adrenaline in 10 ml of NaCl solution - slowly - 5 minutes to prevent myocardial ischemia. Or 1 ml of medicine in 400 ml of NaCl through a dropper, which is more rational.
- Infusion of fluids to prevent coma: 1 liter of NaCL solution, then 0.4 liters of Polyglucin. Initially, a jet injection of up to 500 ml is provided in 30 - 40 minutes, later - through a dropper. It is believed that colloidal solutions fill the vascular bed more actively, but crystalloid liquids are safe, since dextrans themselves can cause anaphylaxis.
- Glucocorticoids.
- Hydrocortisone into a muscle or vein: adults from 0.1 to 1 gram. For children, intravenous injections from 0.01 to 0.1 grams.
- Dexamethasone: 4 – 32 mg intramuscularly, daily dose for intravenous injections 3 mg per kilogram. After the patient has recovered from the acute condition, Dexamethasone tablets are prescribed in a daily dose of up to 15 mg. Children's doses are calculated based on the weight of the children: from 0.02776 to 0.16665 mg per kilogram.
- Prednisolone: 150–300 mg once intramuscularly, infants up to one year old per kilogram of weight 2–3 mg, from 1 year to 14 years 1–2 mg.
- Means for restoring respiratory patency and relieving bronchospasm, suppressing histamine releases.
- Eufillin 2.4% 5 – 10 ml intravenously. Drip administration provides a dose of 5.6 mg per kilogram (20 ml of the drug is diluted in 20 ml of 0.9% NaCl and 400 ml of saline). The highest doses per day per kilogram of weight: 10 - 13 mg, children from 6 years old - 13 mg (0.5 ml), from 3 to 6, 20 - 22 mg (0.8 - 0.9 ml). Eufillin is used with caution in the last trimester of pregnancy, since tachycardia is possible in the mother and fetus.
- In addition to Euphyllin, Aminophylline, Albuterol, and Metaproterol are used.
- Medicines to activate the heart. Atropine 0.1% subcutaneously 0.25 – 1 mg. Children's single doses are prescribed according to weight and age in the range of 0.05 - 0.5 mg.
- Medicines that prevent low blood pressure and increase cardiac output.
- Dopamine. Use intravenously after dilution in a solution of 5% glucose or sodium chloride. Adults (per kilogram of body weight per minute) from minimum dosages of 1.5 - 3.5 mcg (infusion rate 100 - 250 mcg / min) to 10.5 - 21 mcg (750 - 1500 mcg per minute). For children over 12 years of age, the highest dose per kilogram is 4 - 8 mcg (per minute).
- In pregnant patients, Dopamine is used only when there is a threat to the life of the mother; no teratogenic (disfiguring) effect of Dopamine has been identified. Breastfeeding is stopped.
- Antihistamines, which stop the release of allergy-provoking substances into the blood, eliminate itching, swelling, and hyperemia. It is rational to prescribe after restoration of the circulating blood volume, since they can lower blood pressure.
- Intramuscular: Suprastin (20 mg) 2 – 4 ml; initial pediatric doses: 6 – 14 years up to 1 ml, 1 – 6 years 0.5 ml, from a month to a year 0.25 ml. The highest single dose per kilogram of weight cannot exceed 2 mg.
- Pipolfen, Tavegil, Diphenhydramine are also used.
After the acute period has passed, the patient is prescribed glucocorticosteroids in tablets with a gradual reduction in dosage over 7 to 10 days, and antihistamines.
Therapeutic treatment

- Oxygen therapy. Helps with increasing oxygen starvation of tissues and bronchospasm.
- Hemosorption– a special extrarenal technique for removing allergens from the blood by passing it through sorbents.
All patients who have experienced anaphylaxis should be observed in the hospital for up to 2–3 weeks, due to the likelihood of developing repeated anaphylaxis and late complications from the heart, blood vessels, respiratory and urinary systems.
Therefore, in the hospital they do the following several times:
- blood and urine tests;
- study of urea and creatinine levels in the blood;
- electrocardiogram or ultrasound of the heart;
- stool examination for Gregersen's reaction.
Disease prevention
To reduce the risk of developing AS in people with a high likelihood of exposure to an allergen, it is necessary to:
- It is mandatory to have a set of emergency medications (we wrote separately about the standard of care for anaphylactic shock):
- adrenaline solution;
- Prednisolone in ampoules;
- Ventolin, Salbunanol;
- Suprastin or Tavegil or Diphenhydramine (ampoules)
- tourniquet
- be able to use an automatic syringe for injecting adrenaline (Epi-pen, Allerjet);
- avoid insect bites (cover open areas, do not eat sweets and ripe fruits outside the home), use special repellents;
- correctly evaluate the components in the products you eat to avoid the penetration of allergens through the stomach;
- at work, avoid contact with industrial chemicals, inhalation and skin allergens;
- do not use β-blockers if there is a risk of developing severe anaphylaxis, replacing them with medications of another group;
- when conducting studies using radiopaque agents, inject Prednisolone in advance
- do allergy tests from medications and other substances;
- choose medications in tablets rather than injections;
- always have with you a “passport” (card, bracelet, pendant) with information about allergic diseases and medications that help with AS.
Read on to learn about possible complications after an allergic reaction such as anaphylactic shock.
Complications
- Severe complications can be diagnosed:
- Glomerulonephritis
- Intestinal and stomach bleeding
- Cardiac pathologies, including myocarditis
- Bronchospasm and pulmonary edema;
- Swelling and bleeding in the brain
If help is delayed, the pulse becomes weak, the person loses consciousness, and there is a high risk of death.
Forecast
The prognosis is favorable only in case of immediate medical assistance with an accurate diagnosis and emergency hospitalization of the patient.
However, even relief of an acute state of anaphylaxis with medications does not mean that everything ended well, since there is a high probability of a secondary drop in pressure and the development of anaphylaxis (usually within 3 days, but a longer period also occurs).
This video will tell you what to do when anaphylactic shock occurs:
Laying anaphylactic shock in the treatment room
Crimean Republican Institution "KTMO "University Clinic"
(director P.S. Mikhalchevsky)
“Complications of drug therapy: Anaphylactic shock.
Serum sickness"
(for doctors of all specialties, general practitioners - family medicine, junior specialists with medical and pharmaceutical education from healthcare institutions of all levels of medical care)
Simferopol,
The organizational and methodological department recommends the use of methodological recommendations for doctors of all specialties, general practitioners - family medicine, junior specialists with medical and pharmaceutical education at health care facilities at all levels of medical care.
Konyaeva E.I.– Associate Professor, Head of the Department of Clinical Pharmacology and Pharmacotherapy, Head of the regional department of the State Research Center of the Ministry of Health of Ukraine in the Autonomous Republic of Crimea and Sevastopol;
Matveev A.V.– Associate Professor of the Department of Clinical Pharmacology and Pharmacotherapy
Zagrebelnaya N.B.– Head of the organizational and methodological department of the KRU “KTMO “University Clinic”
Every year in all countries there is an increase in the number of patients with allergic pathology. According to the World Health Organization, during the 21st century. In terms of prevalence in the world, it will take 2nd place, second only to mental disorders. In the last decade, allergies have been called a disease of civilization. In highly developed countries, the proportion of people suffering from allergies, mainly among the young population, is significantly higher than in developing and underdeveloped countries. According to statistics from many countries of the world (Germany, Great Britain, France, etc.), 10-30% of the urban and rural population living in regions with highly developed economic potential suffer from allergic diseases.
Drug allergy (DA) refers to complications of drug therapy, the development of which is mediated by immune mechanisms. It is a serious independent disease, which has its own etiology, pathogenesis, clinical picture, methods of diagnosis, treatment and prevention. It is known that JIA can develop as a response to the administration of almost any drug, but the mechanisms of development of hypersensitivity to JIC are different and include reactions of anaphylactic, cytotoxic, immune complex, delayed and mixed types.
The most severe, life-threatening condition in a patient with J1A is anaphylactic shock.
According to the State Enterprise “State Expert Center” of the Ministry of Health of Ukraine, based on the results of the pharmaceutical surveillance system in Ukraine in 2012. 11,674 adverse reactions to drugs, serums and vaccines were registered (of which 988 were in the ARC).
Of these, different types of allergic reactions (localization of manifestations - skin, sensory organs, gastrointestinal tract, respiratory system, etc.) account for 30% to 50% of reports.
In 2012 in health care institutions of the Autonomous Republic of Crimea, according to card reports submitted by doctors of various specialties and health care institutions, 16 cases of anaphylactic shock and 37 cases of angioedema were registered. Traditionally, among the groups of drugs that most often cause allergic reactions, the leaders are antibacterial agents, NSAIDs, local anesthetics, and polyyl solutions. Every year, the trend towards an increase in allergic reactions to serums and vaccines continues.
Anaphylactic shock (AS)- an acutely developing, life-threatening pathological process caused by a generalized immediate allergic reaction that occurs when an allergen is reintroduced into the body. Characterized by severe disruption of vital organs and systems.
Etiology:
The most common causes of anaphylactic shock are:
therapeutic and diagnostic interventions - the use of drugs (penicillin and its analogues, novocaine, streptomycin, vitamin B1, amidopyrine, etc.), immune serums, iodine-containing radiocontrast agents; skin testing and hyposensitizing therapy using allergens; errors in transfusion of blood, blood substitutes, etc.
insect bites
less common: food products (chocolate, peanuts, oranges, mangoes, various types of fish), inhalation of pollen or dust allergens.
Risk factors for developing drug-induced anaphylactic shock:
History of drug allergies and other allergic diseases.
Long-term use of medications, especially repeated courses.
Use of depot drugs.
Polypharmacy.
High sensitizing activity of the drug.
Long-term professional contact with drugs.
The presence of dermatomycosis (athlete's foot), as a source of sensitization to penicillin.
Pathogenesis:
Anaphylactic shock is caused by type I (anaphylactic) immediate allergic reactions (IRT). It is characterized by increased production of class E immunoglobulins (reagins). With repeated (permissive) introduction of the allergen, an antigen-antibody complex is formed (immunological stage), which acts on mast cells, blood basophils and other cells of the human body. As a result (pathochemical stage) a number of biologically active substances (BAS) are released - histamine, serotonin, etc., which cause the development of anaphylaxis (pathophysiological stage).
Anaphylactic reactions should be distinguished from anaphylactoid ones:
Anaphylactoid reactions clinically similar to anaphylactic ones, but are caused not by the interaction of the Antigen with the antibody, but by various substances, for example anaphylatoxins C3, C5a. These substances directly activate basophils and mast cells and cause their degranulation or act on target organs.
Commonly used drugs that can cause anaphylactic reactions and their most likely mechanisms
|
Mechanisms |
A drug |
|
Ig-E-mediated |
penicillin antibiotics, cephalosporins, albumin, adjuvants to medicinal substances (parabens, sulfites), latex and products made from it (including surgical gloves), benzodiazepines, succinylcholine, chymopapain |
|
Activation of the complement system |
X-ray contrast agents, dextrans, vascular prostheses, protamine, perfluorocarbons, propanidide, altesin, nylon components of oxygenator membranes, cellophane components of dialyzers |
|
Histamine liberatory effect |
dextrans, radiocontrast agents, albumin, mannitol and other hyperosmolar substances, morphine, meperidine, polymyxin B, sodium thiopental, protamine, tubocurarine, methocurine, atracurium |
|
Other mechanisms |
plasma protein fractions, non-steroidal anti-inflammatory drugs |
Clinical picture
Most often, symptoms of anaphylactic shock occur 3-15 minutes after the body comes into contact with the allergen. But sometimes the clinical picture develops several hours after contact with the allergen.
The following variants of the course of anaphylactic shock are distinguished:
Acute benign - rapid onset of clinical symptoms, shock is completely relieved under the influence of appropriate intensive therapy.
Acute malignant - rapid development, death can quickly occur even with timely qualified assistance.
Protracted course - initial signs develop rapidly with typical clinical symptoms, active anti-shock therapy gives a temporary and partial effect. Subsequently, the clinical symptoms are not so acute, but are resistant to therapeutic measures.
Recurrent course - characterized by the occurrence of a repeated condition after the initial relief of its symptoms; secondary somatic disorders often occur.
Abortive course - shock passes quickly and is easily stopped without the use of any medications.
The most typical is acute course anaphylactic shock. It is characterized by the sudden appearance of feelings of anxiety, fear, severe general weakness, dizziness, headache, widespread skin itching, skin hyperemia, possible appearance of urticaria, angioedema of various localizations, including in the larynx (Quincke), which is manifested by hoarseness of voice, up to to aphonia, difficulty swallowing, and the appearance of stridor breathing. Patients are bothered by a pronounced feeling of lack of air, breathing becomes hoarse and can be heard at a distance. Many patients experience numbness in their fingers, lips, and tongue; nausea, vomiting, abdominal pain, lumbar pain, cramps, involuntary urination and defecation. The pulse in the peripheral arteries is frequent, threadlike or undetectable, the blood pressure level is reduced or undetectable, and objective signs of shortness of breath are detected. Due to pronounced edema of the tracheobronchial tree and total bronchospasm, auscultation may produce a picture of a “silent lung.” In people suffering from pathology of the cardiovascular system, the course of AS is quite often complicated by cardiogenic pulmonary edema.
Despite the generalized clinical manifestations of anaphylactic shock, depending on the leading syndrome There are 6 clinical options: typical, hemodynamic (collaptoid), asphyxial, cerebral, abdominal, thromboembolic.
Typical option observed in the clinic more often than others. Characteristic symptoms: change in skin color (skin hyperemia or pallor, cyanosis), various exanthemas, swelling of the eyelids, face, nasal mucosa, cold sticky sweat, sneezing, coughing, itching, lacrimation, vomiting, clonic spasms of the limbs (sometimes convulsive seizures), motor restlessness, involuntary release of urine, feces, gases.
Due to the development of Quincke's edema, the patient cannot open his eyes. Rash and hyperemia on the back.
An objective examination reveals: frequent thread-like pulse (on peripheral vessels); tachycardia (less often bradycardia, arrhythmia); heart sounds are muffled; blood pressure (BP) decreases quickly (in severe cases, lower pressure is not determined). In relatively mild cases, blood pressure does not decrease below the critical level of 90-80 mm Hg. Art. In the first minutes, sometimes blood pressure may rise slightly; breathing problems (shortness of breath, difficulty wheezing with foam at the mouth); the pupils are dilated and do not respond to light.
Hemodynamic variant characterized by the prevalence in the clinical picture of hemodynamic disorders with the development of severe hypotension (shock), vegetative-vascular changes and functional (relative) hypovolemia. In the clinical picture, the symptoms of impaired cardiovascular activity come first: severe pain in the heart area; a sharp decrease in blood pressure; weakness of the pulse and its disappearance; heart rhythm disturbance; spasm of peripheral vessels (pallor) or their dilation (generalized “flaming hyperemia”); dysfunction of microcirculation (marbling of the skin, cyanosis).
With asphyxial variant the dominant ones are the development of broncho- and laryngospasm, laryngeal edema with the appearance of signs of severe acute respiratory failure. The development of adult respiratory distress syndrome with severe hypoxia is possible.
Cerebral option. A distinctive feature of this clinical variant is the development of convulsive syndrome against the background of psychomotor agitation, fear, and disturbance of the patient’s consciousness. Quite often, this option is accompanied by respiratory arrhythmia, vegetative-vascular disorders, meningeal and mesencephalic syndromes.
Abdominal option is characterized by the appearance of symptoms of the so-called “false acute abdomen” (sharp pain in the epigastric region and signs of peritoneal irritation), which often leads to diagnostic errors.
Differential diagnosis of anaphylactic shock is carried out with acute heart failure, myocardial infarction, epilepsy (with convulsions), stroke.
A classic example of an immune complex JIAP is serum sickness (SS).
SB occurs not only with the introduction of foreign serum (against tetanus, diphtheria, botulism, gangrene, rabies), vaccines, blood plasma and its components, immunoglobulins, tetanus toxoid for therapeutic and prophylactic purposes, but also with the introduction of certain JICs (for example, penicillin, sulfonamides, cytostatics, non-steroidal anti-inflammatory drugs, insulin, ACTH, iodides, bromides).
The clinical picture of SB is also distinguished by the variety of symptoms and course of the disease, which is due to differences in the types and titers of antibodies formed. Symptoms of SB usually occur 1-3 weeks after J1C administration, but in sensitized individuals the latent period may be shortened to several hours or 1-5 days. During the prodromal period, the following symptoms can be observed: hyperemia and hyperesthesia of the skin, enlargement of regional lymph nodes, small rashes around the injection site. Further, an acute onset of the disease is more often observed with an increase in body temperature from subfebrile levels to 39-40°C. At the same time, itchy rashes appear on the skin in the form of urticaria with symptoms of angioedema, maculopapular rash, erythematous spots, measles or scarlet-like rash, sometimes a hemorrhagic rash occurs and areas of skin necrosis form.
An increase in body temperature and the appearance of a rash are later accompanied by systemic enlargement of the lymph nodes, swelling and pain in the knee, ankle, elbow, wrist joints, small joints of the hands and feet.
There may be abdominal pain and dyspeptic symptoms (nausea, vomiting, diarrhea), and an enlarged spleen. The disease can be complicated by the development of anaphylactic shock, myocarditis, neuritis, radiculitis, glomerulonephritis, hepatitis, and broncho-obstructive syndrome.
Rare manifestations of SB include Guillain-Barré syndrome (acute inflammatory demyelinating polyradiculoneuropathy), systemic vasculitis, glomerulonephritis, hepatitis, peripheral neuropathy, meningoencephalitis. When examining the blood, leukocytosis or leukopenia with relative lymphocytosis, neutropenia, sometimes eosinophilia, an increase in the number of plasma cells, a moderate increase in the ESR level, thrombocytopenia, and hypoglycemia are found.
If long-acting drugs (for example, bicillin) are used, symptoms of the disease may persist for several weeks or even months.
Based on the intensity of clinical manifestations, 4 forms of SB are distinguished: mild, moderate, severe and anaphylactic. Mild form of SB observed in approximately half of patients. The patient's general condition remains satisfactory despite an increase in body temperature to 39°C. A rash of an urticarial or other nature, angioedema, and enlargement of the lymph nodes appear slight and short-lived (within 2-3 days). Joint pain is relatively rare.
The moderate form of SB is characterized by itching, burning, pain, swelling and hyperemia near the site of allergen injection, moderate enlargement of regional lymph nodes, and urticarial skin rash. At the same time, the patient is worried about headache, sweating, tachycardia, hypotension, polyarthralgia, nausea and vomiting. Body temperature reaches 38-39°C and is maintained for 1-2 weeks. In the blood there is moderate leukocytosis with a tendency to subsequent leukopenia with relative lymphocytosis and eosinophilia, and an increase in ESR levels. Traces of protein are detected in the urine. The duration of this condition ranges from 5-7 days to 2-3 weeks.
Severe form of SB differs from the previous ones in a short latent period, acute onset of the disease, the appearance of a widespread morbilliform or hemorrhagic rash, hyperemia of the pharynx and conjunctiva, more pronounced nausea, vomiting, diarrhea, pain in the joints and along the nerves, the development of synovitis and neuralgia, significant enlargement and soreness of the lymph nodes , high (up to 39-40°C).
The anaphylactic form of serum sickness most often occurs when serum is reintroduced during an injection or immediately after it. Clinically, it manifests itself as a shock reaction - sudden deafening of the patient, a drop in blood pressure and an increase in body temperature. Later, stupor gives way to excitement, convulsions appear, spontaneous passage of urine and feces, protein deficiency, shortness of breath, cyanosis develop, and death may occur. Such severe complications of serum sickness as myocarditis, endocarditis, exudative pericarditis, nephritis, hepatitis, allergic encephalitis, meningitis, polyneuritis, diffuse connective tissue damage, necrosis of the skin and subcutaneous tissue at the injection site of the causative allergen have been described.
Treatment patients with JIA developing according to the immune complex type, is based on the general principles of treatment of JIA, but also has a number of features. General principles of treatment for a patient with JIA include:
Cancel all JICs except vital ones (eg insulin).
Prescribing a fasting break or a hypoallergenic diet. Drinking plenty of fluids and a cleansing enema are indicated. Laxative, enterosorbents, infusion therapy.
Antihistamines (AGP) for the development of JIAP mainly in type I; for all other types of J1AP, glucocorticosteroids (GCS) must be used.
For JIAP that develops predominantly in type III (for example, serum sickness), long-term use of corticosteroids and proteinase inhibitors, hemosorption, and enterosorption are indicated.
With the development of cell-mediated JIAP, corticosteroids are administered orally and topically (allergic contact dermatitis).
Syndromic therapy of the main clinical manifestations of JIA.
Mandatory recording of data on the development of JIA in medical records.
In the case of the development of anaphylactic shock and the anaphylactic form of serum sickness, treatment tactics are determined in accordance with the degree of its severity and must comply with the recommendations of the Protocol for the provision of medical care to patients with anaphylactic shock, which were approved by the Ministry of Health of Ukraine by orders No. 767 of December 27, 2005 “On approval of the Protocols diagnosis and treatment of allergic diseases in children" and No. 432 of 07/03/2006 "On approval of protocols for the provision of medical care in the specialty "Allergology". For this purpose it is necessary:
Immediately discontinue administration of JIC or the immunobiologic drug if the patient begins to notice changes in general health or signs of development of JIAP. Lay the patient on a hard couch on his back, raise his legs, throw back his head and turn it to the side, fix his tongue, remove existing dentures.
Inject the injection site of the allergen with 0.3-0.5 ml of 0.1% adrenaline solution with 4.5 ml of 0.9% sodium chloride solution. Repeated administration should be carried out at intervals of 15 minutes.
Apply an ice pack or cold water to the injection site for 10-15 minutes.
If the drug was injected into a limb, apply a tourniquet above the injection site (loosen after 15-20 minutes for 2-3 minutes). Inject 0.3-0.5 ml of 0.1% adrenaline solution into the limb (for children - 0.15-0.3 ml).
If necessary, perform a venesection and install a catheter into the vein to administer adrenaline and plasma replacement fluids.
Inject subcutaneously 0.3-0.5 ml (for children - 0.15-0.3 ml) of a 0.1% solution of adrenaline hydrochloride at intervals of 10-15 minutes until a therapeutic effect occurs (total dose up to 2 ml, children - up to 1 ml) or there will be no side effects (usually tachycardia).
If there is no effect, 0.2-1 ml of 0.2% norepinephrine or 0.5-2 ml of 1% mezatone solution in 400 ml of 5% glucose solution or isotonic sodium chloride solution is administered intravenously (rate 2 ml/min., for children - 0.25 ml/min.).
At the same time, GCS is administered intramuscularly or intravenously (in a stream and then drip at 20-30 drops per minute): a single dose of 60-120 mg of prednisolone (for children - 40-100 mg) or dexamethasone 8-16 mg (for children - 4-8 mg ) or hydrocortisone 125-250 mg IV per 20.0 ml of 0.9% sodium chloride solution. Repeated administration of GCS is carried out after 4 hours. GCS used in large doses (small pulse therapy) have a pronounced positive effect on the patient’s hemodynamics. The use of GCS in standard doses (1-2 mg/kg body weight per prednisolone) is designed primarily to desensitize the patient and prevent relapse of AS. The hyposensitizing effect of GCS develops no earlier than 1-2 hours after intravenous administration of drugs of this group (hydrocortisone has the fastest positive effect, since the drug is closest in properties to endogenous hydrocortisone). It is this period of time that is necessary for the synthesis of specific immunosuppressive proteins in the patient’s body.
When systolic pressure is above 90 mm Hg. 2 ml of 0.1% tavegil (children - 0.5-1.5 ml) or 2.5% suprastin are administered intravenously or intramuscularly.
Water-salt solutions are administered intravenously. Plasma replacement solutions (0.9% sodium chloride solution, 5% glucose solution). Injection of crystalloid solutions helps to reduce relative hypovolemia both due to an increase in the volume of circulating blood and due to the reflex vasoconstrictor effect upon irritation of the vascular endothelium by the injected drug. The advantages of crystalloid plasma substitutes are their ability to quickly leave the vascular bed, which makes it possible to quickly eliminate hypervolemia, as well as their low allergenicity in comparison with dextran derivatives: Reopoliglucin, refortan. For each liter of fluid, 2 ml of Lasix or 20 mg of furosemide are administered intravenously or intramuscularly.
Drugs from the group of H-1 histamine blockers. Drugs in this group are effective in approximately 65 - 70% of patients with symptoms of urticaria or angioedema. 1st generation H-1 histamine blockers (suprastin, tavegil) prevent further effects of histamine to a greater extent than help relieve already developed manifestations of anaphylactic shock. Drugs of the 2nd and 3rd generations of H-1 histamine blockers are produced only in dosage forms for oral administration, which limits their use in urgent situations, but allows the use of these drugs to prevent relapse of AS. If treatment with HI-receptor antagonists is effective, the dose of the drug must be reduced gradually to avoid exacerbation of the disease: 1st generation H1-histamine receptor antagonists, after hemodynamic stabilization - Suprastin 2% - 2.0 ml IV or Tavegil 0.1% - 2 .0 i/v.
For bronchospasm, 10.0 ml (for children - 2.8 ml) of a 2.4% solution of aminophylline in a 0.9% solution of sodium chloride or dexamethasone (20-40 mg) is administered intravenously. Drugs from the p2 group - adrenergic agonists in inhalers (Berotek, Salbutomol).
Cardiac glycosides, respiratory analeptics (strophanthin, korglykon, cordiamine) are administered according to indications.
If necessary, mucus from the respiratory tract and vomit should be sucked out and oxygen therapy humidified with oxygen should be performed.
15. All patients with an anaphylactic form of serum sickness should be hospitalized in hospitals where resuscitation measures can be carried out. Monitoring of patients after their recovery from a serious condition should be carried out for at least 3 days.
Prevention:
Consists of primary and secondary.
Primary Prevention consists of limiting the occurrence of drug sensitization. To do this you need:
avoid contact with potential allergens
For patients with a known allergy to anything (medicines, food, insect bites), any drugs with a high allergenic potential should be avoided.
avoid polypharmacy,
do not use novocaine as a solvent,
avoid repeated courses of the same antibiotic,
do not prescribe medications without sufficient indications,
improve the working conditions of workers who come into contact with medicinal substances (exhaust ventilation, personal protective equipment, etc.).
Secondary Prevention is aimed at preventing relapses of drug allergies. Particular attention should be paid to collecting anamnesis. In this case, the following points become clear:
Does the patient or his blood relatives suffer from allergic diseases?
Has the patient received this drug before and has there been an allergic reaction to it?
What medications did the patient take for a long time?
Have there been any allergic reactions or exacerbation of the underlying disease after taking medications and which ones exactly, and how long after taking the medications?
Did the patient receive injections of serums and vaccines and were there any complications during their administration?
Does the patient have professional contact with medicinal substances and which ones?
Does the patient have fungal diseases?
Good day, dear readers!
In today’s article we will look at one of the most life-threatening types of allergic reactions, anaphylactic shock, as well as its symptoms, causes, types, emergency care algorithm, treatment and prevention of anaphylactic shock.
What is anaphylactic shock?
Anaphylactic shock (anaphylaxis)– an acute, rapidly developing and deadly allergen in the body.
Anaphylactic shock is an immediate allergic reaction, most often manifested when the allergen re-enters the body. The development of anaphylaxis is so rapid (from a few seconds to 5 hours from the beginning of contact with the allergen) that if the emergency care algorithm is incorrect, death can occur literally within 1 hour!
As we have already noted, anaphylactic shock, in fact, is a super-strong (hyperergic) response of the body to the entry of a foreign substance into it. When an allergen comes into contact with antibodies, which have the functions of protecting the body, special substances are produced - bradykinin, histamine and serotonin, which contribute to the disruption of blood circulation, disruption of the muscular, respiratory, digestive and other systems of the body. Due to disruption of normal blood flow, organs throughout the body do not receive the necessary nutrition - oxygen, glucose, nutrients, starvation occurs, incl. brain. At the same time, it falls, dizziness appears, and loss of consciousness may occur.
Of course, the manifestations described above are not a normal reaction of the body to an allergen. What is observed with anaphylaxis indicates a malfunction in the immune system, therefore, after providing emergency care for anaphylactic shock, therapy is also aimed at normalizing the functioning of the immune system.
According to statistics, anaphylaxis is fatal in 10-20% of cases if it is caused by the administration of a drug (drug allergy). In addition, from year to year, the number of manifestations of anaphylactic shock is growing. This is due, first of all, to the deterioration of the general health of a large number of people, the low quality of modern food products and the frivolous use of medications without consulting doctors. Statisticians also note that the manifestation of anaphylaxis is more noticeable in women and young people.
For the first time, the term “Anaphylactic shock” appeared in the scientific world at the beginning of the 20th century, when it was introduced into use by 2 people - Alexander Bezredka and Charles Richet.
Anaphylactic shock. ICD
ICD-10: T78.2, T78.0, T80.5, T88.6;
ICD-9: 995.0.

The cause of anaphylactic shock can be an incredible number of different allergens, so we will note the most common of them:
Insect bites
Animal bites
Food
Due to the fact that the body, due to various GMO products, does not receive the required amount of vitamins and minerals, as well as the replacement of normal food by many people - fast food products and others, many people experience various disturbances in the functioning of the body. In addition, allergies to various products are increasingly observed, with about 30% of allergy sufferers susceptible to anaphylaxis.
Highly allergenic food products include:
- nuts and their derivatives – peanuts and peanut butter, almonds, hazelnuts, etc.;
- seafood - shellfish, crabs, some types of fish;
- dairy products, eggs;
- berries and fruits - citrus fruits, strawberries, grapes, bananas, pineapples, pomegranates, raspberries, apricots, mangoes;
- other products: tomatoes, chocolate, green peas, .
Medicines
Due to the rapid development of the media, many people, without consulting their doctor, often unwisely use certain drugs that can not only cure, but also significantly worsen a person’s health condition. You need to understand that some drugs are prescribed only in combination with other drugs, but all the details are usually outlined by the doctor based on an examination and thorough diagnosis of the patient.
Let's look at medications that carry a risk of developing anaphylaxis:
Antibiotics, especially penicillin (“Ampicillin”, “Bicillin”, “Penicillin”) and tetracycline series, sulfonamides, “”, “Streptomycin”, etc. The statistics of cases of anaphylaxis is 1 in 5000.
Nonsteroidal anti-inflammatory drugs (NSAIDs)– “Aspirin”, “Ketoprofen”, “”, etc. The statistics of cases of anaphylaxis is 1 in 1500.
Angiotensin-converting enzyme (ACE) inhibitors, used in the treatment of hypertension - “Captopril”, “Enalopril”, etc. The statistics of cases of anaphylaxis is 1 in 3000.
Anesthetics, used in various surgical interventions - Ketamine, Propofol, Thiopental, Halothane, Sevovluran, etc. The statistics of cases of anaphylaxis is 1 in 10,000.
Other medications: vaccines, serums.
Contrast agents
Contrast agents are injected into the human body intravenously to conduct a number of radiological health tests - angiography and fluoroscopy. Contrast agents literally highlight various organs for more detailed diagnostics. The incidence rate of anaphylaxis is 1 in 10,000.
Other reasons
Other causes of anaphylaxis include household chemicals (direct contact and inhalation of vapors), animal hair, inhalation of vapors (perfumes, deodorants, varnishes, paints, house dust), cosmetics (hair dyes, mascara, lipstick, powder), artificial materials (latex), etc.
Symptoms of anaphylactic shock
Signs of anaphylactic shock can appear within a few seconds after contact with the allergen.
The first symptoms of anaphylactic shock:
- , clouding of consciousness;
- feeling of heat in the body;
- convulsions;
- cardiopalmus;
- involuntary urination, defecation;
- strong fear, panic;
- hyperemia, as well as;
- increased sweating.
Other symptoms of anaphylactic shock include:
- changes in the skin - severe itching, Quincke's edema;
- disorders of the respiratory system - shortness of breath, suffocation, swelling of the mucous membranes of the respiratory system and spasms in the upper respiratory tract, a feeling of a lump in the throat;
- swelling of the facial part - eyes, lips, tongue;
- dilated pupils;
- stuffy ears
- taste disturbances;
- increased tactile sensitivity;
- blueness of fingers and toes;
Types of anaphylactic shock
Anaphylactic shock is classified as follows:
With the flow:
- Mild flow;
- Moderate course;
- Heavy current.
According to clinical manifestations:
Typical option. General symptoms.
Hemodynamic option. Anaphylaxis is accompanied by disturbances in the functioning of mainly the cardiovascular system - pain in the heart, a drop in blood pressure, disturbances in the rhythm of the heart, disturbances in blood flow. The hemodynamic variant of anaphylaxis has 4 degrees of severity.
Asphyxial option. Anaphylaxis is accompanied by disturbances in the functioning of primarily the respiratory system - breathing problems, swelling of the respiratory tract (throat, bronchi, lungs), shortness of breath.
Cerebral option. Anaphylaxis is accompanied by disturbances in the functioning of mainly the central nervous system (CNS) - fears, cerebral edema, dizziness, convulsions, loss of consciousness, cardiac and respiratory arrest.
Abdominal option. Disturbances occur mainly in the abdominal region - abdominal pain, nausea, vomiting, spontaneous urination and defecation, swelling of the gastrointestinal tract.
According to the nature of the flow
- Acute malignant
- Benign
- Zyatyazhnoe
- Recurrent
- Abortive.
Diagnosis of anaphylactic shock
Diagnosis of anaphylactic shock is usually determined by the clinical picture. A full diagnosis is carried out after first aid, because Literally every second counts. Of course, if an allergic reaction begins, it is advisable to tell the doctor when it appeared, as well as how much time has passed since contact with the allergen.
After emergency care, a detailed diagnosis of the patient includes the following studies:
- allergy history;
- skin and patch tests (Patch test);
- blood test for total immunoglobulin (IgE);
- provocative tests.
The purpose of the research is to determine the causative agent of the allergic reaction.

 The algorithm of actions for anaphylactic shock includes the following points of first emergency aid (pre-hospital):
The algorithm of actions for anaphylactic shock includes the following points of first emergency aid (pre-hospital):
1. It is necessary to immediately stop contact with the allergen.
2. Lay the victim, if possible, so that his head is below the level of his feet; for this, you can put something under his feet. Turn your head to the side so that if it appears, the person does not choke on vomit. If the person has dentures, remove them.
3. Remove tight clothing from the person and provide free access to air.
4. If an allergic substance was injected into a limb, apply a tourniquet above the injection site (for 25 minutes), which will prevent the rapid spread of the antigen throughout the body.
5. If blood pressure does not drop, give the victim an antihistamine to drink: “”, “Tavegil”. If possible, administer them intramuscularly, which will speed up their action.
6. Inject a 0.1% solution of adrenaline into the frenulum of the tongue (sublingually) or intramuscularly. The dose for adults is 0.3-0.5 ml, for children - 0.05-0.1 ml/year of life. To administer adrenaline intravenously, it must be diluted with saline in a ratio of 1:10 to obtain a solution of 0.01% adrenaline.
7. Also inject the injection site with a solution of adrenaline, in dosages for adults - 0.3-0.5 ml, children - 0.1 ml/year of life, diluted with 4.5 ml of saline.
8. If you know the place where the allergen got in (insect bite, injection, etc.), apply something cold there. Ice or a chilled bottle of water is a great option. This will slow down the process of absorption of the allergic substance by the body.
9. Call a doctor immediately. It would be great if someone called a doctor at the very beginning, during an emergency.
Important! When providing first aid for anaphylactic shock, do not forget.
10. If the heart stops, start artificial ventilation and.
First medical aid for anaphylactic shock
The following measures are taken if the victim’s condition does not improve, but rather worsens.
1. Adrenaline solution is continued to be administered intramuscularly and intravenously, in dosages for adults - 0.3-0.5 ml, for children - 0.05-0.1 ml/year of life. The frequency of injections is 5-10 minutes. The dose may be increased if blood pressure continues to fall and clinical manifestations worsen. A single dose of 0.1% adrenaline solution should not exceed 2 ml.
2. If the blood pressure level does not normalize, it is necessary to start intravenous drip administration of 0.2% norepinephrine (Dopamine, Mezaton), at a dose of 1.0-2.0 ml per 500 ml of 5% glucose solution. Instead of glucose, you can use saline solution.
3. Glucocorticosteroids are administered intravenously:
- "Dexamethasone": adults - 8-20 mg, children - 0.3-0.6 mg/kg;
- "Prednisolone": adults - 60-180 mg, children - 5 mg/kg.
Hormones are administered over 4-6 days.
4. After normalizing blood pressure, an antihistamine is administered intramuscularly:
- "Suprastin" (2% solution): adults - 2.0 ml, children - 0.1-0.15 ml/year of life;
- "Tavegil" (0.1% solution): adults - 2.0 ml, children - 0.1-0.15 ml/year of life;
Symptomatic treatment
With bronchospasm. A 2.4% solution of aminophylline in saline is administered intravenously, in a dose for adults - 10.0 ml, for children - 1 ml/year of life. Additionally, respiratory analeptics and cardiac glycosides (Digoxin, Strophanthin) can be administered.
If vomit enters the respiratory tract begin their suction, apply oxygen therapy.
For anaphylaxis from penicillin antibiotics 1670 IU of penicillinase diluted with 2 ml of saline solution is injected intramuscularly.
After providing emergency medical care for anaphylactic shock, the patient must be hospitalized for a minimum period of 10 days. During inpatient observation and symptomatic treatment, the patient may still experience late allergic reactions after anaphylactic shock. At this time, it is very important to receive qualified medical care.
Treatment of anaphylactic shock
After anaphylactic shock, symptomatic treatment of the patient is continued, which includes:
Taking antihistamines, which are used for outbreaks of an allergic reaction - “”, “”, “”.
Taking decongestants, which are used for allergic reactions in the respiratory system - “Xylometazoline”, “Oxymetazoline”. Contraindications: nursing mothers, children under 12 years of age, hypertension.
Use of leukotriene inhibitors, which relieve swelling of the respiratory organs and eliminate bronchospasms - “Montelukast”, “Singulair”.
Hyposensitization. This method involves the systematic gradual introduction of small doses of a large number of allergens, which is aimed at developing the body's resistance to allergens, and accordingly minimizing repeated attacks of acute allergic reactions, including anaphylactic shock.
Prevention of anaphylactic shock
Prevention of anaphylactic shock includes the following rules and recommendations:
— storage of a medical card indicating all information about allergic reactions to a particular substance;
- if you are allergic, always carry with you an allergy passport and a set of emergency medications: antihistamines (Suprastin, Tavegil), a tourniquet, a solution of adrenaline with saline, cardiac glycosides (Digoxin, Strophanthin).
- do not use medications without consulting a doctor, especially injections;
- use traditional methods of treating diseases only after consulting a doctor;
- try to wear clothes mainly made from natural fabrics;
— use household cleaning products with gloves;
— use chemicals (varnishes, paints, deodorants, etc.) only in well-ventilated areas;
- exclude immunotherapy if uncontrolled;
- avoid contact with stinging insects - wasps, bees, hornets, bumblebees, as well as other animals - snakes, spiders, exotic frogs and other representatives of exotic fauna;
Anaphylactic shock is a severe allergic condition that poses a threat to human life, which develops as a result of exposure to various antigens on the body. The pathogenesis of this pathology is due to an immediate reaction of the body, in which substances such as histamine and others suddenly enter the blood, which causes an increase in the permeability of blood vessels, spasms of the muscles of internal organs and other multiple disorders. As a result of these disorders, blood pressure drops, which leads to the brain and other organs not receiving the proper amount of oxygen. All this leads to loss of consciousness and the development of many internal disorders.
Etiology and pathogenesis
Anaphylactic shock is an overreaction of our body to a foreign influence from the outside. The severity of the patient's condition is directly related to the failure of the body's immunological response to the invasion of a foreign agent.
Most often, this reaction develops in children, but also in adults who are prone to allergies, such a powerful response from the immune system is possible. The cause of such a reaction is often the bites of certain insects, for example, bees, as well as the administration of medications (antibiotics, vaccines). Less commonly, a super-strong immunological response develops in response to the consumption of certain foods with a high allergenicity index, such as nut butters, peanuts, oranges and other foods. Even less commonly, anaphylactic shock develops due to inhalation of pollen from certain plants.
There is a tendency to develop anaphylaxis in people with pronounced symptoms, who, when exposed to cold wind and water, can develop allergic reactions such as and. The most powerful reaction to irritants is sometimes anaphylactic shock.
At times, the reaction appears unexpectedly - in people who have not previously had a tendency to allergies. For example, this is often encountered by pet owners who, when keeping a pet for a long time, may develop signs of an allergy to the fur or epithelium of their pet, and the final (and often unexpected) reaction is anaphylactic shock.
Symptoms
After an allergen accidentally enters the body, symptoms of anaphylactic shock appear either instantly or within half an hour. Moreover, the earlier they appear, the worse the prognosis for the course of an allergic reaction, because this means that the human immune system is completely unable to cope with the allergen. In some cases, people die from a super-powerful allergic reaction even before the administration of the drug that caused it is completed, but these are rather exceptional cases.
Symptoms of anaphylactic shock may be more or less severe. Lightning-fast vascular collapse is the most dangerous sign of this pathology, but most often a person begins to complain of weakness and a tingling sensation in the feet, palms, and face. If these complaints are ignored, the further development of the situation becomes uncontrollable - the feeling of weakness intensifies, the person turns pale, begins to feel fear, he develops profuse sweating and pain in the abdomen. A sharp drop in blood pressure causes loss of consciousness and even involuntary urination and defecation.
Sometimes there are other signs of a pathology such as an anaphylactic reaction:
- itching on the body;
- swelling of the ears, tongue, eyelids;
- the appearance of rashes on the skin;
- lacrimation and mucus discharge from the nasal passages;
- the appearance of noisy difficulty breathing.
Subsequently, the clinic is characterized by loss of consciousness and vascular collapse.
It should be said that the patient’s condition with such an allergic reaction as anaphylactic shock is very serious and therefore the person urgently requires qualified medical care, without which he can die in a matter of minutes. That is why in manipulation rooms and dental offices there is always a first aid kit with medications ready to stop an attack of AS.
Note that before loss of consciousness and the onset of collapse, patients usually behave very restlessly - they are scared, and they breathe heavily, and in those people who have central nervous system disorders or cardiovascular pathologies, the clinical picture is aggravated by specific symptoms, for example,. Due to a spasm of smooth muscles, breathing is impaired and occurs, and as a consequence -.
Unfortunately, every tenth case of such an overreaction is fatal, and there is an especially high mortality rate from a pathology such as anaphylactic shock in children, whose immune system responds very violently to the introduction of the antigen. Note that in children the signs of anaphylaxis are somewhat different than in adults. Young patients initially experience great fear and shortness of breath. Then children develop cold sweats and cramping abdominal pain, followed by vomiting, dizziness, foaming at the mouth and the development of seizures.
The pulse in children is thread-like, practically not palpable, the tongue and larynx swell, which leads to impaired respiratory function and the development of cyanosis.
First aid
The main thing that should be done in an emergency is to take immediate measures to relieve an attack of anaphylaxis. Emergency care consists of providing pre-medical and medical care. Pre-hospital emergency care for anaphylactic shock is represented by a set of measures aimed at stopping or eliminating the effect of the irritant and introducing antihistamines into the body.
If a patient has developed anaphylactic shock, there is no time to delay. First of all, it is necessary to provide access to fresh air to the victim of a bite or injection of an allergen in another way, lay the person on a horizontal surface and free his body from tight clothing. The legs should be slightly raised and the head should be turned to the side to prevent the victim from choking on vomit.
Among the antihistamines that you should try to give to the victim, you can use Tavegil or Suprastin, or another remedy that is at hand.
If anaphylactic shock occurs in a medical facility, the doctor provides emergency care to the patient on site. Also, medical assistance is provided upon the ambulance’s arrival at the scene of the incident, and it consists of administering a solution of adrenaline, which increases blood pressure.
In addition, the person is administered glucocorticosteroids and aminophylline, which eliminates respiratory failure. The following actions of doctors are as follows:
- the respiratory tract is cleared of vomit;
- symptoms of heart failure are eliminated;
- Oxygen is supplied through a nasal catheter.
Emergency care for children is carried out similarly, with the only difference being that the necessary drugs are administered every 15 minutes until the little patient’s condition is stabilized.
Further treatment of anaphylactic shock after stabilization of the patient's condition is carried out in a hospital setting. It involves cleansing the body of toxins and replenishing blood volume. In severe cases, treatment of anaphylactic shock requires the use of resuscitation equipment to maintain the vital functions of internal organs.
Adults and children who have suffered this allergic reaction are left under observation in the hospital for two weeks. This is necessary in order to eliminate the likelihood of complications, for example, disruption of the heart or urinary system. Discharge from the hospital is carried out after tests and an ECG. In the future, to prevent the clinic from happening again, it is necessary to completely eliminate contact with the allergen that caused the super-powerful allergic reaction.
Anaphylactic shock is a severe, life-threatening pathological condition that develops when the body comes into contact with certain foreign substances (antigens). Anaphylactic shock refers to allergic reactions immediate type, in which the combination of antigen with antibodies causes the release of a number of biologically active substances (histamine, bradykinin) into the bloodstream. These substances cause increased permeability of blood vessels, impaired blood circulation in small blood vessels, spasm of the muscles of internal organs and a number of other disorders. Blood accumulates in the periphery, blood pressure drops, internal organs and the brain do not receive enough oxygen, which is the main reason.
You need to understand that such a reaction of the body to foreign substances is inadequate, hyperergic (i.e. super strong). The severity of a person’s condition is due to a failure of the immunological response of the body itself.
Causes of anaphylactic shock
The most common causes of anaphylactic shock are insect bites and the administration of medications (such as penicillin, sulfonamides, serums, etc.). Such reactions occur less frequently for food products(chocolate, peanuts, oranges, mangoes, various types of fish), inhalation of pollen or dust.
Symptoms of anaphylactic shock
The clinical picture of anaphylactic shock is characterized by rapid development; symptoms appear within a few seconds or minutes after contact with the allergen.
- depression of consciousness;
- drop in blood pressure;
- convulsions;
- involuntary urination.
In most patients, the disease begins with the appearance of a feeling of heat, skin flushing, fear of death, and chest pain. Blood pressure drops sharply, the pulse becomes thready.
Possible variants of anaphylactic shock with a predominant lesion:
- skin with increasing skin itching, hyperemia, the appearance of widespread urticaria and Quincke's edema;
- nervous system (cerebral variant) with the development of severe headache, nausea, increased tactile sensitivity, convulsions with involuntary urination and defecation, loss of consciousness;
- respiratory organs ( asthmatic variant) with dominant suffocation due to swelling of the mucous membrane and spasm of the smooth muscles of the upper respiratory tract;
- heart (cardiogenic) with the development of a picture of acute myocarditis or myocardial infarction.
The diagnosis is usually made based on the clinical picture.
What can you do (first aid for anaphylactic shock)
At the slightest suspicion of the development of anaphylactic shock, you should immediately call an ambulance. Before the doctor arrives, you should try to stop further entry of the allergen into the body. If anaphylactic shock occurs as a result of an insect bite, a tourniquet should be applied above the bite site. This way, you will stop the allergen from entering the general bloodstream. Try to place the victim in a horizontal position on his back with his head tilted to the side, to prevent asphyxia due to retraction of the tongue or aspiration of vomit, then release the neck, chest, abdomen, and ensure an influx of oxygen.
What can a doctor do?
The doctor’s first actions will also be aimed at preventing further entry of the allergen into the bloodstream: a tourniquet is applied above the injection site or bite site or an epinephrine solution is injected (). They provide fresh air, allow oxygen to be inhaled from an oxygen cushion, and administer antiallergic drugs. Further treatment of anaphylactic shock is aimed at normalizing cardiovascular and respiratory activity, reducing the permeability of the vascular wall and preventing late complications from internal organs.
Prevention
It is impossible to predict the occurrence of anaphylactic shock in most cases. But you should pay attention to manifestations of an allergy to a particular substance (drug, food product, etc.) and in the future try to avoid reintroducing this substance into the body. Patients who have previously suffered anaphylactic shock must have a card with them indicating their allergen.