Nail fungus on the hands is much less common than on the toes, and this phenomenon depends on gender - in women, fungus on the hands is three times more common than in men. There are reasons for this: household chemicals, water, manicure, infection through other contacts. This unpleasant disease in our country affects 20-25% of the population. How to get rid of fungus and its manifestations on fingernails?
- Where do “legs grow” from?
- Is there a panacea
- When everything is running, treat the whole body
- Alternative treatments for mycoses
- Preventive measures
- Get a detailed answer in similar material:
Where do “legs grow” from?
 Fungal infection of fingernails
Fungal infection of fingernails
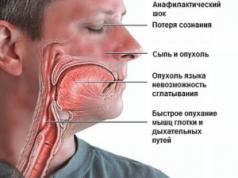
The main problem with fungal diseases is that people often do not consider them to be something serious and treat them carelessly, as if they were an ordinary cosmetic defect, unaware of the possible consequences. And they can be very negative, for example, through damaged skin and nail plates, all kinds of infections enter the body. Since any type of fungus is contagious, family members, co-workers, travel companions, etc. can become ill with it.
Fungus on the fingernails primarily causes a negative attitude among others, because the aesthetics of the affected nail plates is visible to everyone and causes understandable fear among people who are afraid of infection through contact with the hands of a sick person. Serious health problems often lead to damage to fingernails:
- endocrine system disorders,
- general weakening of the body during menopause in men and women,
- vascular diseases,
- weakened immunity as a result of infections or poor diet and lifestyle.
The beginning of the manifestation of a fungal infection is, as a rule, a change in the color of the nail, the appearance of a white or gray area with speckles on the surface of a yellowish tint. When a fungus is detected, you must consult a doctor in order to verify its presence and receive the necessary treatment in a timely manner. Otherwise, your nails will start to turn green, then turn brown and then turn black. In addition, they will be covered with longitudinal dark protruding stripes and take on the appearance of completely rotted dead tissue. Treating fungus at this stage is much more difficult than at the initial stage. There are forms of damage to fingernails: distal, superficial, proximal. Most often, onychomycosis (fungal disease) occurs in the distal form. An advanced form of the disease is dystrophic onychomycosis, when the nails completely separate, literally crumble, and the fungus spreads to the skin around the nail and enters the blood.
Is there a panacea
 Antifungal cream Clotrimazole
Antifungal cream Clotrimazole
Both doctors and traditional healers say: yes! Let's start with medications, time-tested and completely new. Before starting treatment of hand nails with an initial degree of damage, it is necessary to prepare a nail bath: dilute laundry soap (40-50 g) with the addition of soda (1 tablespoon) in 3-5 liters of water (the container should be separate so that other family members do not become infected ). Having immersed your hands in water, hold them until the nail plates soften, and then carefully treat your nails with manicure tweezers and a file, giving them a normal shape (if possible). Manicure accessories should be purchased specifically for these purposes so that other people do not use them.
The next step will be to apply medicinal ointments or creams with antifungal action to the nails, of which our pharmacies offer quite a lot today. The procedure for lubricating nails is carried out at least twice a day, so the work and rest regime should be structured so that the treatment is carried out on time and without carrying out any manual work at home or at work. Doctors advise using the following fungal remedies:
- Clotrimazole.
- Nizoral.
- Lamisil.
- Exoderil.
- Batrafen (varnish).
- Candide.
- Loceril.
- Triderm.
- Nystatin ointment.
- Levorin ointment.
- Nikozan.
- Mycoseptin.
One of the most popular products is “Exoderil” in the form of an ointment and a solution equipped with a dispenser, which are respectively used on the skin and nail plates. Varnishes containing antifungal drugs are a very convenient and effective remedy. The varnish can be used no more than once a week or according to a schedule determined by the doctor. Antifungal varnish fights 58 types of fungi and is used for up to six months for complete recovery. The fungicidal substances of the varnish penetrate into the most inaccessible places of the nail and under it, eliminating the most viable fungi in its bed. Treatment of fungal diseases can take quite a long time - from 2 months to a year, depending on the complexity and severity of the disease, and the entire complex of treatment procedures can last for several years.
When everything is running, treat the whole body
 Systemic drug Ketoconazole
Systemic drug Ketoconazole
If the fungal infection is advanced, internal medications are used - antimycotics:
- diflucan;
- flucostat;
- orungal;
- lamisil;
- griseofulvin;
- ketoconazole.
Before using orally, you must consult a doctor, as these drugs have side effects and contraindications. In some cases, removal of the nail plate followed by treatment is required. The new nail may be a little uneven, but it’s healthy!
It is important to note that oral medications are prescribed for certain types of lesions: nail hyperkeratosis, infection of more than three nails, age-related indications. The drugs kill fungal spores, preventing them from multiplying, and also soften the horny masses of the nail. The doctor can use the so-called pulse therapy, which is based on small amounts of internal medications in a short time and allows you to determine the correctness of the treatment. The dosage must be clearly prescribed and supervised by a doctor.
One of the modern popular types of treatment for fungal diseases has become laser therapy. This is a painless procedure that allows you to destroy fungal spores, clean the nail bed, sterilize it, and also irradiate the blood in the veins using laser irradiation. The laser is not only a good fungicide, it also has an antipruritic, desensitizing effect, and also dries the skin and nail tissue and relieves them of inflammation. Laser irradiation of nails must be carried out 3-4 times; its effectiveness is very high and is visible after the first session.
In advanced cases, hardware cleaning of the nail plates is also useful and necessary. It allows you to speed up the healing process by half and promotes rapid cleansing of the nail bed for complete penetration of medications there.
There is some originality in the treatment of Candida fungi. Candidiasis is treated for a long time and constantly, so you need to be prepared for such a process. Baths with boric acid are used, followed by treatment of nails with fucorcin, iodicerin, miramistin, chlorhexidine. Then the nails need to be lubricated with ichthyol ointment to relieve inflammation. After anti-inflammatory procedures, nails should be lubricated with fungicidal ointments or varnishes. Zinc, iron, and nicotinic acid preparations are very useful in the treatment of candidiasis. Marine and dairy products high in fluoride and calcium should be added to the diet.
Another type of fungus that affects fingernails is dermatomycetes with long filaments of mycelium that penetrate very deeply into living tissue. Terbinafine and its derivatives help well with dermamycetosis. Local treatment is carried out by applying the medicine to clean hands for several weeks 1-2 times a day. The drug accumulates in the nail plate and lasts for six months or more, which prevents relapses of the disease. Terbinafine has been successfully used to treat elderly people and is approved for use in the treatment of children. Terbinafine is available in spray form, which is more convenient for treating fingernails.
Alternative treatments for mycoses
 Iodine solution for fungus
Iodine solution for fungus
For centuries, people have sought to get rid of fungal diseases that manifest on their feet, hands, and nails. Healers offered a variety of medications for this purpose. Let's look at some of them.
- Bath with strong coffee. This type of treatment does not require instant coffee, but natural ground coffee. The coffee infusion should be very strong. It helps quite quickly, after several uses.
- Ointment with vinegar, butter and chicken egg. Requires vinegar essence (70%) - 100 g, 200 g of oil, egg in shell. Place the butter and egg in vinegar and refrigerate. After a week, the shells will dissolve in vinegar and the ointment is ready. Apply 2 times a day and store only in the refrigerator.
- Novocaine lotion. Cotton wool is moistened with novocaine and applied to the sore spot overnight. Effective after several procedures.
- It is useful to rinse hands affected by a fungal infection with strong tea.
- Butter with garlic in the form of cream. The ingredients are mixed in equal parts and applied to the affected nails several times a day, changing the lotions. Gradually the fungus disappears forever.
Decoctions of medicinal herbs are useful:
- chamomile;
- calendula;
- Echinacea.
They act as drugs that strengthen the immune system and the body as a whole, without side effects.
- A solution based on Kalanchoe (100 g), apple cider vinegar (1 tbsp), honey (1 tbsp) and eucalyptus oil (30 g) works well in the fight against fungi. The mixture is infused for 3 days in a cool, dark place. Apply once a day until complete healing.
- Celandine has shown itself to be excellent in the fight against fungal infections. It is used in the form of a decoction, fresh plant juice, or tincture.
- Ordinary 5% iodine also works well, burning out fungal spores.
- The fungus is treated with a 20% propolis solution, applying it to a cotton swab and pressing it to the sore nail.
- There is also a known recipe, the main component of which is tea tree oil. It is necessary to dilute 10 g of oil and a teaspoon of shower gel in half a liter of water. In the resulting composition, you need to steam the nail plates affected by fungi for 15 minutes every day before going to bed.
- Kombucha works great against onychomycosis. It is used as a compress at night, wrapping sore spots with mushroom with polyethylene on top.
- Another remedy available to everyone is hydrogen peroxide, which is used to wipe sore nails or dip it by pouring the peroxide into a bowl.
- Euphorbia juice, as well as speedwell in the form of a decoction for baths, is deadly against fungi on the hands and nails.
The use of traditional methods combined with medications, as a rule, gives the best treatment effect, but in any case, you need to consult a doctor so as not to harm yourself.
Preventive measures
 Keeping your feet clean
Keeping your feet clean
The main condition for prevention was, is and will be, compliance with the rules of personal hygiene. This is due to the fact that most often people become infected with fungi in public places: baths, showers, swimming pools, gyms, and beaches. You can become infected from someone else's shoes, and even by wearing new shoes in a store if they were tried on by a person with a fungal disease before you. It is necessary to regularly care for your feet and hands, and carefully look at changes in the surface of the skin and nails. You cannot wear tight shoes and use your own closed rubber slippers in common areas. Hands should be washed after traveling on public transport, visiting shops, banks, hospitals and other crowded places. In case of real fungal infection, immediately consult a doctor - a mycologist to determine the type of disease, the necessary therapy, who will prescribe medications to destroy the fungus.
A simple way to understand whether there is a fungal infection on the nails has long been to dip your hands in a solution of potassium permanganate. Normal healthy nails will darken, but areas with fungal infections will remain the same color.
Each sick person can check with a doctor or pharmacy how much a particular drug costs in order to choose a drug that suits their budget. A variety of antifungal drugs allow you to do this, so you shouldn’t delay if you notice that something unpleasant is happening to your nails, but you should immediately go to see a doctor, otherwise you will have to deal with daily treatment of onychomycosis for the next months, or even years.
Video: Treatment of fingernail fungus with hydrogen peroxide
Candidiasis (yeast fungus): symptoms, how and how to treat
With the birth of a person, microscopic organisms begin to populate him. As the fetus moves through the birth canal, they end up on the skin and its derivatives, penetrate the mouth, and infect the respiratory tract, intestines, and mucous membranes. This is how the microflora of these organs is formed, where both host-friendly and pathogenic microbes live. The delicate balance between the two groups of microorganisms greatly influences human health.
Biological characteristics of the pathogen
Yeast fungi are conditionally pathogenic microbes, that is, being ordinary “peaceful” inhabitants of the intestines and vagina, under certain conditions they escape the control of the dominant beneficial species, begin to multiply intensively and cause a lot of trouble to humans.
Conditions that contribute to this include:
- weakened immune system;
- vitamin deficiencies due to oral contraceptives, antibiotics and steroids;
- gastritis;
- diabetes.
A starch-containing diet also works in favor of fungi. Consuming glucose from the blood, they lead to a drop in its level, the appearance of hunger and, ultimately, obesity. Yeast colonies grow in the presence of toxins (mercury, fluoride, chlorine) contained in some types of cosmetics and medicines, water and food.
Symptoms of candidiasis
Fungi from the genus Candida, which numbers about 150 species, provoke a disease called “candidiasis.” In 95% of cases, the culprit of the disease is the yeast fungus Candida albicans. In a pathogenic state, it damages the intestinal wall, resulting in not only toxins released by candida, but also some food components. This is accompanied by a number of physical symptoms, including:
- craving for sweets and alcohol;
- intolerance to certain foods;
- cystitis;
- sinusitis;
- joint pain.
A person may also be bothered by mental symptoms, namely:
- irritability;
- feeling of unreasonable anxiety;
- depressive states.
The activity of pathogens of fungal infections can provoke the appearance of allergic reactions on the skin in the form of urticaria and dermatitis. In the most severe cases, candida is found in the heart valves and meninges.
This variety of manifestations of candidiasis is explained by the multitude of toxins secreted by the fungus, poisoning different organ systems. One of them, for example, is distinguished by an “estrogen-like” effect, as a result of which a woman suffers from “hot flashes”, premenstrual tension, and in some cases from endometriosis.
Diagnosis of candidiasis
The presence of certain symptoms cannot be the basis for a diagnosis of candidiasis. To confirm and identify the degree of yeast infection, laboratory diagnostic methods are used, yeast fungi are determined in the urine and blood, and skin tests are performed.
If candidiasis is suspected, a comprehensive analysis is performed, which determines, for example, yeast fungi in the child’s stool. The feces are placed in a special medium to determine the rate of yeast reproduction and establish or refute the diagnosis of mycosis. Blood is examined to determine the level of immunoglobulins.
Yeast is usually absent in the urine of a healthy person. Therefore, an important analysis is to examine urine for traces of fungal infection.
Before treating yeast fungus in women, it is necessary to find out whether this type of candida provoked the disease. To do this, the gynecologist, after an examination on the chair, takes a smear from the vaginal mucosa. Yeast fungi in a smear are detected by microscopic examination. Bacterial culture is also carried out with the cultivation of colonies and determination of their susceptibility to various antimycotic drugs. A qualitative analysis of Candida colonies is mandatory.
Types of candidiasis
Candidiasis can be of two types:
- Superficial. It most often affects overweight people and those suffering from diabetes. Accompanied by erosions, itching, and rashes developing under the breasts, in the area of the nail fold, and the intergluteal fold.
- Internal. It can be transmitted through sexual contact, since the yeast fungus constantly lives in the female reproductive system. In the vagina, its numbers are controlled by lactic acid bacteria. When the balance is imbalanced towards candida, it begins to “dominate” in the woman’s genital tract, causing burning and itching. Thrush develops, which opens the gates for other infectious agents. Candida does not live in a man's urethra, but after sexual intercourse with a sick partner, his penis may become inflamed.
Important! Yeast reserves are located in the intestines.
After taking a number of medications and poor nutrition, the beneficial intestinal microflora is suppressed and ceases to synthesize antimycotic enzymes. That is why, in order to cure any form of candidiasis, it is necessary to normalize the composition of the intestinal microflora and follow an appropriate diet. Otherwise, even taking antifungal drugs does not give the desired long-term effect.
Treatment of candidiasis
Treatment of yeast fungus in men, as in women, requires a lot of time and even more effort. After all, a yeast fungus can become covered with a capsule and wait until “better times”; it can develop resistance to the medications used against it and “resurrect” after long-term therapy. That is why many experts even have the opinion that candidiasis is incurable. Although this is less about the pathogen and more about the approach to treatment. If it was not brought to its logical conclusion or was inadequate in relation to the patient’s condition, then the disease will return again and again.
The state of a person’s immune system is judged by the presence of candidiasis. In addition to correcting the intestinal microflora, a diet excluding refined foods, yeast and sugar, full-scale anti-candida therapy is necessary. When women are affected by a fungal infection, treatment is carried out using:
- herbal preparations;
- medicines;
- allergy medications.
Important! The selection of probiotics requires special attention, since lactic bacteria, widely used for treatment, do not fight the fungus, but coexist perfectly with it.
In children, thrush is treated with solutions of sodium bicarbonate and chlorhexidine. They are used to treat the child's oral cavity. General antifungal therapy is used only in difficult cases.
Yeast fungus in men is treated with ointments such as Miconazole, Ketoconazole, Econazole, Clotrimazole. These formulations can be purchased at a pharmacy without a prescription, but it is better to consult with your doctor first to avoid burning and itching in patients with particularly sensitive skin. To relieve skin irritation, medications containing corticosteroids are used.
Self-medication for a fungal infection can lead to serious complications, so all medications are taken only after the approval of a specialist and strictly according to the treatment regimen prescribed by him.
How to treat thrush in men. Drugs that work
Although in some men the signs of thrush do not appear clearly and go away quickly, if the disease is not diagnosed and treated in a timely manner, complications can arise. Today, doctors clearly understand how to treat thrush in men (medicines in pharmacies, as a rule, have a good effect). The therapy regimen has been tested for years and guarantees excellent results. 
Causes of thrush
Quite often, thrush is transmitted during intimacy, but most situations are not associated with this. That is why vaginal candidiasis is not classified as a sexually transmitted disease. The symptoms of such ailments are quite similar, and therefore it would not be superfluous to be examined by a venereologist.
Among the factors contributing to the appearance of thrush are:

In addition, stress, dysbiosis, local infection, and local trauma are considered causative agents of Candida.
Male candiosis, which occurs after sexual intercourse with a woman with vaginitis, is called conjugal thrush. Quite often, candidiasis in men develops after sexual contact with a pregnant wife. The fungus is also introduced from the lining of the rectum.
Oral remedies for thrush
For the treatment of male thrush with a prolonged course or in case of complications, antifungal drugs for oral use are prescribed:
1. Fluconazole is a drug that has an antifungal effect and suppresses the production of sterols in the cells of the Candida fungus, neutralizing them. A characteristic feature is the rapid absorption of the substance and preservation in the blood plasma for a long time. It is taken once a day, 50-100 mg. The course of treatment ranges from a week to a month. 
2. Itraconazole is a broad-spectrum agent with great effectiveness. It promotes the destruction of the cell membrane of the fungus. The active substance quickly spreads throughout the organs, accumulates and remains in matter for a long time. You need to take the drug once a day for three days. 
3. Flucostat is an antimycotic, the main substance of which is fluconazole. Its rapid dissolution in the digestive tract allows for a high concentration of the drug in biological fluids and tissues. 
Ointments for candidiasis
These medications are characterized by several advantages: convenient application, reduction of external symptoms of infection, and fastest possible action. The price of ointments is affordable for patients. As a rule, doctors prescribe ointments for thrush:
1. Nystatin is an antibiotic prescribed for acute and chronic forms of candidiasis. Therapy lasts ten days, during which the affected area is lubricated with cream twice a day. 
2. Clotrimazole is the most effective medicine with a strong antimycotic effect. When it enters the body, it quickly searches for Candida fungus cells, blocks their spread and destroys them completely, eliminating the symptoms of the disease. The ointment is used at least twice a day, rubbing into the damaged areas. In addition, the ointment is characterized by an antibacterial, anti-amebic, anti-trichomonas effect, eliminating the causes of the disease. 
3. Tetraborate is an effective antiseptic with increased bacteriostatic activity. It does not allow the mycelium of the fungus to attach to the surface of the mucosa and slows down its reproduction. 
During therapy, it is important to follow the rules of personal hygiene, namely: do not touch the genitals with dirty hands, change underwear, and follow hygiene procedures after visiting the toilet.
Protected sexual intercourse is considered the best prevention of thrush.
Candidiasis of the penis is manifested primarily by itching and burning of the glans and foreskin. Colonies of pathogenic fungi that have multiplied on the mucous membranes disrupt the healthy microflora. Soreness and even sometimes sharp pain during sexual intercourse is the next sign of penile candidiasis. A careful examination of the genital area will help determine the disease. Redness in the genital area, swelling of the foreskin and head of the penis indicate the presence of a pathogenic process. The appearance of a whitish coating, as well as cheesy discharge from the urethra with an unpleasant sour odor are sure signs of penile candidiasis.
Thrush in men can occur in the form of various diseases, the clinical picture of which depends on the localization of the process.
Balanitis is a candidal infection of the outer surface of the penis. One common cause is sexual intercourse. The skin and mucous membranes on the glans penis become red, and slight erosion, rash or maceration (moist softening of cells) may appear. The head swells and may become covered with a grayish or white coating. The long course of the disease causes painful changes in the inguinal folds.
Balanoposthitis is a pathological process that extends not only to the glans penis, but also affects the foreskin. If the disease is not treated, then inflammation in the foreskin causes scarring and leads to phimosis - narrowing of the foreskin.
With urethritis, candida affects the urethra. Urethritis is often confused with gonorrhea or other sexually transmitted diseases when a whitish fluid is discharged.
Cystitis is a lesion of the bladder, the clinical course of which does not differ from cystitis, which is caused by another pathogen. In this case, there is a feeling of heaviness in the pubic area, a painful burning sensation and increased frequency of urination, cloudy urine and the appearance of blood.
Pyelocystitis is a complicated course of penile candidiasis, in which the infection spreads upward to the urinary tract. Symptoms of candidal pyelonephritis are signs of deterioration in general condition and ascending infection. The causative agent of the disease, a yeast fungus of the genus Candida, is detected in the urine.
Despite the unpleasant signs of the symptoms listed above, the most dangerous is the asymptomatic and painless course of candidiasis of the penis. In this case, the man, unaware of the disease, becomes a source of infection for his sexual partners. That is why it is very important that when symptoms of thrush are detected in a man, his “other half” also undergoes examination and treatment.
Causes
In most cases, the occurrence of candidiasis is not associated with sexual contact, although this route of infection also occupies a significant position in the statistics. Therefore, if you have a trusting relationship with your man, do not rush to accuse him of all mortal sins. And although penile candidiasis is often classified as a sexually transmitted disease, it can be considered together with them only solely because of similar clinical manifestations.
The following factors contribute to the development of the disease:
- congenital and acquired immunodeficiency conditions (HIV infection);
- long-term use of broad-spectrum antibiotics;
- general weakening of the immune system due to climate change, emotional stress, chronic fatigue, hypothermia, etc.;
- endocrine diseases, primarily diabetes mellitus;
- infectious diseases and intoxication of the body;
- weakening of the resistance of tissues and mucous membranes of the body due to injuries, burns (mechanical, thermal, chemical), maceration, malfunction of the glandular epithelium due to chronic or acute inflammatory diseases of the genitourinary system;
- dysbacteriosis of the mucous membranes under the influence of endogenous and exogenous factors;
- surgical and other interventions on the genitourinary system.
Treatment and prevention
Timely contact with a qualified specialist helps to quickly cope with a fungal disease. When following the doctor’s recommendations and prescriptions, treatment of penile candidiasis is quick and successful. For diagnosis and subsequent treatment, the following tests are prescribed: a smear for microflora, bacterial culture of secretions and DNA diagnostics to determine the nature of the pathogen.
Treatment of penile candidiasis involves the use of various antifungal drugs as prescribed by a doctor - both for internal use and for external use. It is recommended to treat areas affected by candidiasis with a soda solution. It is very important to complete the entire course of treatment for penile candidiasis, without interrupting it at the first signs of relief. You should also not drink alcohol even in small doses, as this will significantly reduce the effectiveness of the drugs or even reduce all results to zero. After completing the course, you must take all tests again and make sure there is no disease.
To prevent the occurrence of penile candidiasis, the following recommendations should be followed:
- compliance with personal hygiene rules using individual products;
- you need to wear underwear only made from natural fabrics, since synthetics do not provide sufficient air ventilation, prevent the evaporation of moisture and contribute to the formation of an environment favorable for the development of infections;
- it is important to eat foods that have a natural antifungal effect (grapefruit, lingonberries, propolis, hot peppers, garlic, etc.);
- use a condom for casual sexual intercourse;
- parallel use of antifungal drugs during antibiotic treatment;
- eat foods that contain live lactobacilli (kefir, yogurt), which help normalize the body's microflora and increase overall immunity;
- take care of the general strengthening of the body and increasing immunity.
Following simple measures and rules will help you forget about troubles forever and fully enjoy a healthy life without illness.
Preparations and ointments for the treatment of thrush in men
Candidiasis in men is rare due to the characteristics of the body. The fungus is removed from the genitourinary system along with urine. But there are times when a man still gets thrush. This should immediately alert him, since the disease indicates that not everything is in order with his body. It should be remembered that thrush is not a harmless disease.
Most people have this type of fungus. Thrush begins to form if there is too much fungus as a result of rapid reproduction in favorable conditions. Usually the disease occurs with complications only in women, especially during pregnancy. But despite this, the male half of the population also encounters a similar problem.
According to statistics, this disease develops in men much less frequently than in women. The significant difference is explained by the fact that men and women have different genitourinary systems. Another reason is that men with thrush neglect its symptoms and medical help.
Causes of thrush
 The circumstances of the development of male candidiasis differ from female ones. A man becomes infected with it during sex with a partner who has thrush.
The circumstances of the development of male candidiasis differ from female ones. A man becomes infected with it during sex with a partner who has thrush.
The chances of contracting thrush in men increase if a person has been diagnosed with HIV, diabetes, and has undergone chemotherapy to treat cancer. Thrush in men has another important feature: it is almost in no way associated with dysbacteriosis.
It is possible to understand that a man is infected only by such signs as itching and rash on the penis. This sign of the disease is not characteristic, so at first it is not alarming. If the disease is neglected, it will lead to the development of complications, for example, chronic inflammation of the genital organ.
In case of further spread, the disease is complicated by urethritis. Reddened or erythematous lesions appear on the penis.
The infection begins to spread throughout the urethra. There is a possibility of fungal cystitis and prostatitis. If you get thrush, the likelihood of developing male infertility increases.
An asymptomatic form of male thrush is often found. In this case, signs of the disease appear only after the action of provoking factors, for example, after drinking alcohol. In this situation, thrush can be mistaken for an allergy to alcohol-containing drinks.
It is not uncommon for men to develop such infections during their partner's pregnancy. This is explained by the fact that the changes that occur in a woman’s body during pregnancy reduce immunity. The fungus begins to grow and multiply and is transmitted from woman to man during sexual intercourse.
Thrush in men: treatment
 What are the basic principles of treating male thrush? To get rid of fungus permanently, men should use antifungal agents. It can be a cream, solution, ointment. These include triderm, pimafucin, clotrimazole and others. These drugs are used 3 times a day. Treatment lasts 7 days.
What are the basic principles of treating male thrush? To get rid of fungus permanently, men should use antifungal agents. It can be a cream, solution, ointment. These include triderm, pimafucin, clotrimazole and others. These drugs are used 3 times a day. Treatment lasts 7 days.
In case of a protracted course of the disease with complications, antifungal medications for oral administration should be added to the above drugs: flucostat, diflucan and others. Before you begin treatment for candidiasis in men, you must visit a doctor.
There are cases when treatment of thrush in men is delayed. In such a situation, a man needs not just an ointment, but also a competent approach from a qualified specialist. In order for recovery to occur as soon as possible, along with thrush, you should begin to treat those diseases that provoked the disease and complicated its course. Candida fungus should not be allowed to grow and develop. To do this, it is necessary to maintain the weakening body at a normal level. The doctor will definitely recommend that the patient start taking vitamins, immunomodulators and other medications.
Drugs for treatment
Treatment of the disease can be called complete if it is carried out comprehensively, combining local medications with fungicidal agents.
 The latter include a drug such as Fluconazole. It can be used in a variety of treatments. If you follow the regimen indicated on the package, the effect will not take long, and the fungal infection will disappear forever. We can recommend another antimycotic drug - Itraconazole. It has also proven itself to be an effective remedy.
The latter include a drug such as Fluconazole. It can be used in a variety of treatments. If you follow the regimen indicated on the package, the effect will not take long, and the fungal infection will disappear forever. We can recommend another antimycotic drug - Itraconazole. It has also proven itself to be an effective remedy.
The dose and frequency of taking such drugs used to treat male thrush are determined based on the individual parameters of the patient and his characteristics. To cure the disease, you should follow all the recommendations given by the doctor. This promotes rapid recovery.
There are cases when candidiasis is familial, that is, both partners suffer from it. In such a situation, complex treatment is required, which is prescribed to both men and women. This especially applies to those men who do not have obvious signs of thrush. Indeed, in this case, the man is still a carrier of the infection. If joint treatment is not carried out, new relapses are possible.
 Not a single comprehensive treatment regimen for an infection will give the expected result if a man neglects the necessary rules of intimate hygiene. Everyone knows that cleanliness is the key to our health. Remember: a man’s hands should always be clean. Particular attention should be paid to keeping your hands clean before using the toilet and after leaving it. Most often, men forget about this simple rule. At the same time, dirty hands several times increase the chance of developing an infection, and not only a fungal one.
Not a single comprehensive treatment regimen for an infection will give the expected result if a man neglects the necessary rules of intimate hygiene. Everyone knows that cleanliness is the key to our health. Remember: a man’s hands should always be clean. Particular attention should be paid to keeping your hands clean before using the toilet and after leaving it. Most often, men forget about this simple rule. At the same time, dirty hands several times increase the chance of developing an infection, and not only a fungal one.
Intimate hygiene also includes cleanliness of the entire body. To ensure this, you need to follow simple rules: change your underwear daily, exclude synthetic fabrics, wear loose underwear made from natural materials. Cotton is ideal for these purposes, as it creates optimal conditions for the body to interact with the environment. It is known that in synthetic underwear, fungal spores begin to grow like in a greenhouse. If you neglect these tips, it will become much more difficult to defeat male thrush, and the duration of treatment for candidiasis will increase. Consequently, the patient will have to spend much more money to purchase the necessary medications.
 Daily washing of the genitals must be carried out exclusively with the use of products suitable for this purpose. These include cosmetics such as creams, shower gels, specially created for washing various parts of the body, in particular the genitals. These products are different from ordinary types of soap. They do not irritate the skin and mucous membranes. Laundry soap has contraindications for use in cases of fungal inflammation. Special care products for intimate areas of the body suppress the proliferation of pathogenic fungi.
Daily washing of the genitals must be carried out exclusively with the use of products suitable for this purpose. These include cosmetics such as creams, shower gels, specially created for washing various parts of the body, in particular the genitals. These products are different from ordinary types of soap. They do not irritate the skin and mucous membranes. Laundry soap has contraindications for use in cases of fungal inflammation. Special care products for intimate areas of the body suppress the proliferation of pathogenic fungi.
To prevent the development of the fungus, men are advised to protect themselves from sexual contact with unfamiliar women, since even a condom does not protect a man from the risk of contracting thrush.
In addition, the use of most medications, antibiotics and hormones requires mandatory clinical justification. Otherwise, there is a risk of intestinal dysbiosis, which reduces the body’s immunity, which means additional treatment may be required.
Remember: treatment will not give a positive result if you do not follow simple rules of intimate hygiene. You should wash your hands and body regularly, change your underwear daily - all these rules must be followed, and then you will not be afraid of candidiasis.
 You can completely rid yourself of thrush even at home. The patient should not be in the hospital 24 hours a day. The main thing in self-treatment is not to make certain mistakes. Before treating thrush in men at home, an examination by a dermatologist is still required. Further actions must be strictly followed according to his instructions and recommendations, otherwise the disease will begin to actively progress.
You can completely rid yourself of thrush even at home. The patient should not be in the hospital 24 hours a day. The main thing in self-treatment is not to make certain mistakes. Before treating thrush in men at home, an examination by a dermatologist is still required. Further actions must be strictly followed according to his instructions and recommendations, otherwise the disease will begin to actively progress.
It is known that candidiasis occurs due to infection with the Candida fungus. Therefore, treatment should be aimed at eliminating its causes. Antimycotic drugs will help you with this. These products are suitable for topical use or can be used as an addition to systemic treatment.
If the patient requires topical treatment to get rid of candida fungus, the drug should be applied directly to the genitals. The patient can perform the actions necessary for treatment himself at home. The main thing is to stock up on all the necessary products, which can be purchased at any pharmacy.
http://youtu.be/kVRHiSHj5hs
As a rule, to get rid of thrush, fungicidal preparations are used, available in different forms: ointments, creams, gels. Most often, patients use ointments and creams Declosid, Candide and others. These products show maximum results if applied 3 times a day to the affected skin and mucous membrane of the genitals. The course of local treatment with ointment should be continued for 7-12 days. During the time when thrush in men is being treated, it is strictly forbidden to have sex. If thrush occurs in men, the drugs will not have an effect if he does not follow this rule. Otherwise, the disease will remind itself of itself with constant relapses.
What does Biseptol help with and what is its mechanism of action?
 Pathogenic bacteria are present in the surrounding space of a person, and therefore in his body. Immune cells do not allow pathogenic microflora to develop, but when immunity is weakened or other factors occur, microbes begin to actively multiply in the body, causing various diseases.
Pathogenic bacteria are present in the surrounding space of a person, and therefore in his body. Immune cells do not allow pathogenic microflora to develop, but when immunity is weakened or other factors occur, microbes begin to actively multiply in the body, causing various diseases.
Pathogenic microorganisms include bacteria, viruses, and fungi. Since these are different biological objects, treatment should be prescribed in accordance with the pathogen. The doctor prescribes a medicine that will be effective in the fight against a particular microbe. One of the most commonly prescribed drugs against bacteria is Biseptol. What Biseptol helps with and how to take it, we’ll look at it in the article.
For the treatment of various inflammatory diseases, two types of drugs are prescribed: antibacterial and antimicrobial. The former contain substances that kill bacterial cells, while the latter inhibit protein synthesis in the enemy cell and stop its vital activity.
The active ingredients of Biseptol do not have components present in the natural environment, and therefore the medicine does not belong to the group of antibiotics. In other words, the drug is completely synthetic.
Composition of the medicine:
- sulfamethoxazole - the main active ingredient, stops the growth and development of bacteria;
- trimetroprin - has an auxiliary effect, prevents the restoration and reproduction of pathogenic microflora.
Co-trimozole is synonymous with sulfonamides. It is part of Trimethoprim, an antibiotic that is widely used to treat diseases of the urinary system.
Pharmachologic effect:
The bacteriostatic property of the drug is achieved by blocking the biosynthesis of folic acid in bacterial cells by the active substances. Folic acid is involved in metabolic processes in which microbial protein synthesis occurs with the help of nucleic acids. Violation of biochemical reactions in the cell leads to a stop in reproduction and to its death from the inside.
Biseptol actively affects the following microorganisms:
- gram-positive and gram-negative bacteria;
- protozoa;
- staphylococci;
- toxoplasma;
- streptococci;
- mushrooms;
- coli.
Pathogenic microflora causing syphilis and tuberculosis are resistant to sulfonamides.
Indications for use
Biseptol is indicated for the treatment of infectious diseases caused by microorganisms sensitive to the active substances of the component. Asking the question: “What does Biseptol help with?” It should be understood that you cannot self-medicate. Only a doctor can correctly determine whether a drug will be effective or not after examining the patient.
- The medicine helps with inflammatory diseases of the respiratory system: rhinitis, bronchitis, pharyngitis, pneumonia, laryngitis and others.
- Bispetol is often prescribed for infectious lesions of the genitourinary system: prostatitis, inflammation of the uterine appendages, pathological processes in the kidneys, bladder, urethra.
- The drug is effective for the treatment of the digestive system: inflammation of the pancreas (pancreatitis), inflammatory processes in the small and large intestines (enterocolitis), gastritis.
- Biseptol is prescribed for pathologies of the ENT organs accompanied by infection: inflammation of the maxillary sinuses (sinusitis), inflammatory processes occurring in the inner and outer ear (otitis), purulent inflammation in the tonsils.
Therapeutic effect on prostatitis
Biseptol for prostatitis is one of the most powerful medications to combat the disease. It is prescribed if the pathology of the prostate gland is infectious. The active ingredients of the drug penetrate deep into the prostate tissue, stopping the development of pathogenic bacteria. Reducing the number and activity of bacteria reduces pain, swelling of the prostate, and eliminates other symptoms.
Prostatitis should be treated with Biseptol only on the recommendation of a doctor. Self-medication may be useless or even harmful. After the examination, the specialist will calculate the dosage that will be optimal.
You need to take the drug for inflammation in the prostate for at least two weeks. For the first few days, the doctor prescribes the maximum dosage, which is then reduced. The patient feels relief after 2-3 days, but it is important not to interrupt the course of treatment, since bacteria can develop resistance to the drug. This, in turn, can lead to a chronic form of prostatitis, which is difficult to treat.
Some patients believe that since Biseptol is not an antibiotic, it can be taken uncontrolled, but this is not so. The drug has serious side effects, and an increased dose of the drug will not cure prostatitis faster. It is necessary to follow the treatment regimen for prostate inflammation and follow all doctor’s recommendations.
Therapeutic effect on other pathologies
Biseptol is prescribed for many inflammatory diseases of the respiratory system and ENT organs. And sometimes people believe that it can be taken for acute respiratory infections, but in this case the drug is useless, since these diseases are caused by viruses. But Biseptol treats tonsillitis, tonsillitis, sinusitis and other diseases complicated by bacterial microflora perfectly.
 In the case of diseases of the genitourinary area and intestines, the situation is the same. In order to understand whether Biseptol is needed, the cause of the painful conditions should be determined. If it is bacteria, then the use of the medication is justified.
In the case of diseases of the genitourinary area and intestines, the situation is the same. In order to understand whether Biseptol is needed, the cause of the painful conditions should be determined. If it is bacteria, then the use of the medication is justified.
You should be careful when treating Biseptol when it comes to children. Even if in the past the doctor prescribed a drug to treat, for example, a sore throat, then if the disease recurs, in no case should you give the child the medicine yourself.
Otherwise, the bacteria will become resistant, and sore throat will appear again and again.
The therapeutic effect of sulfonamides on different organs manifests itself in the same way, since the principle of action on bacterial cells is the same. But the doctor determines the dosage and course of treatment individually.
Before starting to take the drug, it is necessary to exclude contraindications. Biseptol is not used in the following cases:
- anemia (low folate levels);
- hypersensitivity to active substances;
- pregnancy and lactation;
- severe renal dysfunction;
- childhood hyperbilirubinemia;
- damage to the liver parenchyma;
- at risk of developing hemolysis.
When taking the drug, people suffering from bronchial asthma and pathologies in the thyroid gland should be careful.
The drug can negatively affect various body systems: nervous, respiratory, digestive, musculoskeletal, and hematopoietic systems.
Taking the drug may be accompanied by the following side effects:
- dizziness and pain in the head;
- depression, apathy and peripheral neuritis;
- abdominal pain, nausea, diarrhea, vomiting;
- urticaria, rash, erythema;
- cough, suffocation, bronchospasm;
- anemia, neutropenia, agranulocytosis, thrombocytopenia;
- increased urea concentration, impaired renal function;
- myalgia, arthralgia.
How to take Biseptol for children and adults
For ease of use, Biseptol is available in different dosage forms.
- The tablet form is available in two dosages:
- 120 mg - for children;
- 480 mg - for adults.
- Suspension for children with strawberry scent in a bottle of 80 ml. 1 dose - 5 ml contains 240 mg of active substances.
- Concentrate for preparing a solution for infusion. 1 ampoule contains 480 mg of active substances.
How to take Biseptol and in what dosage forms depends on the disease and age of the patient.
Treatment in adolescents and adults:
The minimum dose for treatment longer than 14 days is 480 mg every 12 hours. The standard dosage is 960 mg twice a day; for severe infections, the dose is increased to 1440 mg every 12 hours.
- The course of treatment for respiratory tract and ENT infections is ten days.
- Treatment of inflammatory diseases of the genitourinary system lasts from fourteen to twenty-one days.
- Diseases of the gastrointestinal tract are treated for at least five days.
- Treatment for infectious diseases of the genital organs (chancroid) lasts from seven to fourteen days.
- To treat acute urinary tract infections in women, “shock” therapy is used, in which a single dose is up to 2880 mg.
- Pneumonia is treated with 960 mg twice a day. The individual dosage is calculated at 30 mg/kg.
- Nocardiosis is treated at a dosage of 2880 mg for at least three months, acute brucellosis - four weeks, typhoid fever - three months.
How to drink Biseptol in tablets and suspension?
 How to drink Biseptol tablets is described in detail in the instructions for use of the drug.
How to drink Biseptol tablets is described in detail in the instructions for use of the drug.
The tablets are taken every 12 hours, so the medication should be taken in the morning and evening. The drug should be taken only after meals, the tablet should be washed down with plenty of clean water.
Do not take the medicine on an empty stomach, otherwise it may cause side effects.
Treatment in children
Up to five years of age, the medicine is prescribed in a standard dosage of 240 mg in the morning and evening. From six to twelve years - 480 mg twice a day. The duration of treatment is seven days.
For children from two months to six months of age, born from a mother infected with HIV, the dosage is 120 mg.
For children, Biseptol is most often prescribed for the treatment of intestinal infections, sore throat, otitis media, laryngitis and other infectious diseases of the respiratory tract.
The syrup is used from two months of age, and 120 mg tablets from two years of age.
For individual dosage, the suspension is calculated based on 36 mg of the drug per 1 kg of weight.
How to drink Biseptol in suspension?
The child should be given the medicine after meals; it is advisable to maintain a 12-hour interval between taking the suspension. The medicine is taken with a special measuring syringe through the neck of the bottle. Before taking the suspension, shake the bottle well to agitate the liquid. There are special divisions on the syringe that determine the dosage.
Biseptol suspension has a pleasant berry taste, so children drink it easily. If the child wants to drink the medicine, you can give him clean water.
It is important to give the child the medicine exactly in the dose prescribed by the doctor; in no case should you be independent in this matter.
The minimum dosage is calculated as follows:
- up to six months - 2.5 ml morning and evening;
- up to three years of age - 2.5-5 ml twice a day;
- up to the age of six - 5-10 ml every 12 hours;
- up to twelve years - 10 ml every 12 hours.
- Tablets 120 mg 20 pieces - 30 rubles;
- Tablets 480 mg 28 pieces - 90 rubles;
- Suspension 240 mg / 80 ml - 120 rubles.
How do Erespal and Biseptol combine when taken?
Biseptol does not combine well with various drugs and alcohol. For inflammatory diseases of an infectious nature, it is prescribed first; if the medicine does not help, the doctor adjusts the treatment.
Erespal is prescribed for the treatment of infectious diseases of the upper respiratory tract. The drugs have different pharmacological effects on the body, so the question of combining Erespal and Biseptol techniques is best answered by the attending physician.
Over the past 20 years, the number of fungal infections (mycoses) has increased dramatically. This is mainly due to the introduction of new medical technologies and a significant increase in the number of patients with immunodeficiency. The range of pathogens causing mycoses is rapidly expanding; currently, more than 400 species of fungi are known to cause diseases in humans.
Clinical manifestations of infections caused by fungi vary widely from relatively harmless superficial lesions of the mucous membranes and skin to life-threatening invasive mycoses, which can affect almost any organ.
This chapter presents indications for treatment (diagnostic criteria) for the most common mycoses, the main directions of treatment, doses of antifungals and timing of their use.
Since mycoses usually develop in patients with certain disorders in the anti-infective defense system (risk factors), their elimination or reduction in severity should be an obligatory component of the treatment and prevention of relapse of mycoses. It is not the scope of this chapter to provide a detailed analysis of these activities; only a few of them are indicated. In addition to the use of antifungal drugs and elimination of risk factors, a prerequisite for effective treatment of some invasive mycoses is timely surgical removal of the affected tissue.
CANDIDIASIS
Main pathogens
The main causative agents of candidiasis are C.albicans, C.tropicalis, C.parapsilosis, C.glabrata And C.krusei. Much less common C.lusitaniae, C.guillermondii, C.rugosa etc. Despite the fact that the most common pathogen remains C. albicans, over the past 15-20 years there has been a significant increase in the number of infections caused by C.tropicalis, C.parapsilosis, C.glabrata And C.krusei.
View Candida spp. correlates very clearly with sensitivity to antifungal drugs (). The vast majority of strains C. albicans, C. tropicalis And C. parapsilosis sensitive to systemic azoles (fluconazole, itraconazole) and amphotericin B. At the same time, the possibility of development of resistance of these pathogens to antimycotics should be taken into account during long-term treatment of candidiasis in patients with immunodeficiency. Most strains are resistant to fluconazole C.krusei and some isolates C.glabrata, and to itraconazole - almost half of the strains C.glabrata and a third of strains C.krusei. Often resistant to amphotericin B C.lusitaniae And C.guillermondii, and for infections caused C.glabrata And C.krusei, it is necessary to increase the dose of this drug.
Table. Sensitivity of the main causative agents of candidiasis to antifungal drugs
| Fluconazole | Itraconazole | Amphotericin B | |
|---|---|---|---|
| C. albicans | H | ||
| C.tropicalis | |||
| C. parapsilosis | |||
| C.glabrata | |||
| C.krusei | |||
| C.lusitaniae |
In practice, it is recommended to determine the type of pathogen in case of invasive candidiasis, as well as in case of recurrent course and/or resistance of superficial candidiasis to standard therapy.
Candida spp. are inhabitants of the human body. They are detected by culture from the mucous membrane of the oral cavity and gastrointestinal tract in 30-50% of healthy people and from the mucous membrane of the genitals in 20-30% of healthy women. Therefore, it is important to be able to distinguish between candidiasis and colonization of the mucous membranes or skin.
Risk factors
Risk factors for the development of candidiasis are a decrease in the number and dysfunction of neutrophils and T-lymphocytes of various origins; endocrinopathies; malignant neoplasms; use of catheters (vascular, urinary, peritoneal, etc.); injuries, widespread burns and surgical interventions; the use of broad-spectrum AMPs, glucocorticoids, immunosuppressants and infusion therapy; premature birth; transplantation of organs and tissues.
Classification
The range of diseases caused Candida spp., very wide. The manifestations of this infection vary from superficial candidiasis with damage to mucous membranes, skin and nails up to invasive And disseminated damage to various organs and tissues.
INVASIVE CANDIDIASIS
Invasive candidiasis is characterized by the severity of clinical manifestations and high (30-70%) mortality. In this regard, the adequacy of antifungal therapy in patients with invasive candidiasis is of particular importance. The main antimycotics for the treatment of invasive candidiasis are amphotericin B and fluconazole. The role of other azoles is less significant due to variable oral bioavailability and relatively little experience in treatment. When choosing a drug, you should take into account the type of pathogen and its sensitivity to antimycotics.
Empirical antifungal therapy is the prescription of antifungal drugs to patients with a high risk of invasive mycosis before its laboratory confirmation. Currently, empirical antifungal therapy is recommended for patients with antibiotic-resistant neutropenic fever, as well as for those at high risk of developing acute disseminated candidiasis in certain categories of patients without neutropenia. Unjustified empirical use of antifungals in groups with a low risk of invasive candidiasis may be accompanied by adverse reactions and contribute to the selection of strains resistant to antifungal drugs Candida spp.
An important component of the treatment of invasive candidiasis is the elimination or reduction of risk factors (removal of IV or urinary catheters, compensation for diabetes mellitus, etc.).
CANDIDEMIA AND ACUTE DISSEMINATED CANDIDIASIS
Indications for therapy
Candidemia:
- single allocation Candida spp. when inoculating blood obtained during a period of body temperature rising above 38 o C or the presence of other signs of a systemic inflammatory reaction.
Acute disseminated candidiasis:
- candidemia in combination with detection Candida spp. during histological examination and/or culture of material from deep tissues (including subcutaneous tissue)
- identification Candida spp. during histological examination and/or culture of material from deep tissues of two or more localizations.
The choice of antimycotic depends on the type of pathogen and its sensitivity to antifungal agents, as well as the clinical condition of the patient.
All patients with candidemia are advised to have early removal (replacement) of all intravascular catheters.
Duration of therapy: at least 2 weeks after the disappearance of all clinical signs of candidemia and acute disseminated candidiasis and the last diagnosis Candida spp. when inoculating blood and biosubstrates from lesions. After completion of treatment, observation for at least 2 months is indicated to exclude the occurrence of late foci of hematogenous dissemination.
EMPIRICAL ANTIFUNGAL THERAPY IN PATIENTS WITH ANTIBIOTIC-RESISTANT NEUTROPENIC FEVER
Indications for therapy
- agranulocytosis (the number of band and segmented neutrophils in peripheral blood is less than 0.5 x 10 9 /l);
- fever of unknown etiology, resistant to adequate treatment with broad-spectrum antibiotics, lasting more than 4-6 days.
Choice of antimicrobials
Flushing the bladder with amphotericin B (50-200 mcg/ml) is usually accompanied by a temporary cessation of candiduria, but this treatment method is ineffective when the overlying parts of the urinary tract are affected.
Urinary catheters need to be removed or replaced.
For asymptomatic candiduria in patients without risk factors for the development of acute disseminated candidiasis, the use of antimycotics is not recommended; elimination or reduction of the influence of risk factors is indicated (removal or replacement of the urinary catheter, optimization of antimicrobial agents, correction of diabetes mellitus, etc.).
ANTIFUNGAL PREVENTION OF INVASIVE CANDIDIASIS
The use of antimycotics for the primary prevention of invasive candidiasis is recommended only for patients with a high (at least 15%) risk of this complication. Currently, controlled clinical studies have proven the effectiveness of antifungal prevention of invasive candidiasis in recipients of bone marrow and liver transplants, as well as in surgical patients with repeated gastrointestinal perforation. Unjustified prophylactic use of antifungals in groups with a low risk of invasive candidiasis is not only useless, but also harmful, since it can be accompanied by adverse reactions and contribute to the selection of strains resistant to antifungal drugs Candida spp.
PREVENTION OF INVASIVE CANDIDIASIS IN PATIENTS WITH NEUTROPEIA
Indications
Prolonged agranulocytosis (the number of band and segmented neutrophils in the peripheral blood is less than 0.5 x 10 9 / L) in recipients of hematopoietic stem cell transplants.
Prevention
CANDIDIASIS OF THE MUCOUS MEMBRANES, SKIN AND ITS APPENDIXES
The main drugs for the treatment of candidiasis of the mucous membranes, skin and its appendages are antimycotics of the azole group. They are characterized by high efficiency and low toxicity, and can be used both locally and systemically.
A significant problem is the recurrence of mucosal candidiasis in certain categories of patients. In some of them, the reason for the high frequency of relapses has been determined (relapses of oropharyngeal candidiasis in patients with AIDS), in other cases it remains unclear (relapses of candidal vaginitis in women with normal immunity).
Effective treatment should include not only the rational use of antifungals, but also the elimination or reduction of risk factors. When choosing an antifungal drug, the possibility of gradual development of resistance during long-term use should be taken into account.
CANDIDIASIS OF THE ORAL CAVITY, PHYNARS
Indications for therapy
Therapy is indicated if the following symptoms are present:
- Clinical signs;
- identification Candida spp. by microscopy (pseudomycelium or budding cells) and/or culture of material from affected areas of the mucous membranes.
Choice of antimicrobials
Acute candidiasis of the oral cavity, pharynx
Indications for therapy
Therapy is indicated if the following symptoms are present:
- identification Aspergillus spp. with microscopy, histological examination and culture of material from lesions;
- computed tomography, magnetic resonance imaging or radiographic signs of invasive mycosis.
Choice of antimicrobials
The choice of antimycotic is determined by the patient’s condition, the localization of the process and, to a lesser extent, the type of pathogen. The main drug for the treatment of invasive aspergillosis is amphotericin B. Itraconazole is usually used after stabilization of the patient's condition, liposomal amphotericin B - if indicated (see section "Candidemia and acute disseminated candidiasis"). In case of brain damage, the use of liposomal amphotericin B is recommended due to the low effectiveness of the standard one. Amphotericin B-resistant pathogens of invasive aspergillosis ( A.flavus, A.nidulans, A.conicus, A.terreus) are rare. Important conditions for reducing mortality are antifungal prophylaxis and empirical antifungal therapy:
- amphotericin B 1.0-1.5 mg/kg/day up to a total dose of 2.0-2.5 g;
- amphotericin B 1.0-1.5 mg/kg/day until the patient’s condition is stabilized, then itraconazole 0.4 g/day for 2-6 months;
- liposomal amphotericin B 3.0-5.0 mg/kg/day;
- in clinically stable patients - itraconazole 0.6 g/day for 4 days, then 0.4 mg/day for 2-6 months.
Invasive cerebral aspergillosis:
- liposomal amphotericin B 3.0-5.0 mg/kg/day;
- surgical removal of affected tissue.
Prevention of relapse
Performed with each subsequent course of cytostatic therapy:
- amphotericin B 1.0 mg/kg every other day from the beginning to the end of the period of neutropenia (more than 1.0 x 109/l);
- itraconazole 0.4 g/day - from the beginning of cytostatic chemotherapy until the end of the period of neutropenia (more than 1.0 x 109/l);
- granulocyte or granulocyte-macrophage colony-stimulating factors in the period of neutropenia.
Surgical removal of single lesions is performed.
Empirical antifungal therapy
It is performed for fever of unknown etiology, resistant to adequate therapy with broad-spectrum antimicrobial agents, lasting more than 4-6 days in a patient with agranulocytosis (the number of band and segmented neutrophils in the peripheral blood is less than 0.5 x 10 9 /l). Can be discontinued 7 days after body temperature normalizes, as well as upon completion of the period of neutropenia (more than 1.0 x 10 9 /l):
- amphotericin B 0.6-0.7 mg/kg/day;
- liposomal amphotericin B 3.0 mg/kg/day.
CHRONIC NECROTIZING PULMONARY ASPERGILLOSIS
It develops predominantly in patients with impaired T-cell immunity. The severity and course of the disease depend on the degree of immunosuppression.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- characteristic changes during bronchoscopy;
- identification of mycelium Aspergillus spp. in stained smears and/or evidence of invasive fungal growth in biopsy material, or isolation Aspergillus spp. when inoculating bronchoalveolar lavage and biopsy material.
Choice of antimicrobials
Fusarium
Pathogens are fungi of the genus Fusarium: F.solani, F.oxysporum And F.moliniforme- can cause damage to the skin and subcutaneous tissue, the cornea of the eye, and also cause disseminated fusarium. The main risk factor for the development of local fusarium is trauma, and for disseminated fusarium - prolonged agranulocytosis. Disseminated fusarium is characterized by high mortality.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- identification Fusarium spp. with microscopy, histological examination and culture of material from lesions, blood.
Choice of antimicrobials
Fusarium of the skin and subcutaneous tissue
Alternative drugs:(if local treatment is ineffective): amphotericin B 0.3-0.5 mg/kg/day; itraconazole 0.2-0.4 g/day.
Surgical treatment is performed.
Disseminated fusarium
COCCIDIOIDOSIS
The causative agent is a dimorphic fungus Coccidioides immitis. Distribution - separate regions of North, Central and South America.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- identification C.immitis by microscopy, histological examination and/or culture in material from lesions;
- positive results of a serological test (determination of IgM or IgG to C.immitis in serum or CSF).
Choice of antimicrobials
Primary pulmonary coccidioidosis
For asymptomatic cases: observation, antimycotics are not indicated.
With progression
PENICILLIOSIS
The causative agent is a dimorphic fungus Penicillium marneffei. Distribution - individual regions of Southeast Asia. Typically develops in HIV-infected patients.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- identification P. marneffei with microscopy, histological examination and culture of material from lesions;
- determination of antibodies to P. marneffei in blood serum.
Choice of antimicrobials
Moderate illness
CHROMOMYCOSIS
Pathogens: Fonsecaea pedrosoi, Fonsecaea compacta, Phialophora verrucosa, Botryomyces caespitosus, Rhinocladiella aquaspersa, Exophiala spinifera And Exophiala jeanselmei. Chromomycosis is a chronic disease that affects the skin and subcutaneous tissue. Infection usually occurs as a result of injury.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- Clinical signs;
- identification of characteristic signs by microscopy and histological examination of material from lesions (granulomas with the presence of microabscesses containing dark tissue forms of the fungus);
- To identify the pathogen, long-term (4-6 weeks) cultivation of material from the lesion is usually required.
Choice of antimicrobials
Drugs of choice: itraconazole 0.1-0.3 g/day for 12-24 months.
Alternative drugs: terbinafine 0.5 g/day for 6-12 months.
Surgical treatment is performed.
DERMATOMYCOSIS
Dermatomycosis is a disease of the skin, scalp and nails caused by dermatomycetes, i.e. filamentous fungi of the genera Trichophyton, Microsporum And Epidermophyton. About 10 species of dermatomycetes can cause mycosis in humans. Currently, the most common and contagious dermatomycete is T.rubrum 0.25 g/day for 6 weeks; when the feet are affected - fluconazole 0.15 g/week for 6-12 months, terbinafine 0.25 g/day for 12 weeks.
Alternative drugs: when the hands are affected - itraconazole 0.4 g/day, two weekly courses with a 3-week break or itraconazole 0.2 g/day for 3 months; when the feet are affected - itraconazole 0.4 g/day, three to four weekly courses with a 3-week break or itraconazole 0.2 g/day for 3-4 months.
Preparations for external use are not effective enough.
MYCOSIS OF THE SCALP
Main pathogens
Trichophyton spp. And Microsporum spp.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- Clinical signs;
- detection of dermatomycete mycelium by microscopy of affected hair and/or isolation of the pathogen when inoculating material from the lesion.
Choice of antimicrobials
Drugs of choice: terbinafine 0.25 g/day for 4 weeks (if the pathogen Trichophyton spp.) or 8 weeks (if the pathogen Microsporum spp.)
Alternative drugs: fluconazole 0.4 g/week for 8-12 weeks; itraconazole 0.2-0.4 g/day for 4 weeks; griseofulvin 0.5 g/day for 6-12 weeks.
The use of antifungals for external use (for example, ketoconazole) reduces the likelihood of infecting others.
Pityriasis versicolor
Superficial skin infection caused by yeasts of the genus Malassezia: M.furfur, M.sympodialis, M.globosa, M.restricta, M.obtusa And M.slooffia.
Indications for therapy
Therapy is indicated if the following symptoms are present:
- Clinical signs;
- identification Malassezia spp. during microscopy of material from skin lesions.
Choice of antimicrobials
Drugs of choice: antifungals for external use in the form of solutions, sprays, creams, ointments or shampoos (terbinafine, bifonazole, isoconazole, ketoconazole, clotrimazole, miconazole, oxiconazole, econazole, naftifine, etc.) for 10-14 days.
Alternative drugs: fluconazole 0.4 g once; itraconazole 0.2-0.4 g/day for 3-7 days; ketoconazole 0.2 g/day for 5-10 days.
Disruption of the normal microflora of the vagina, unfortunately, is familiar to almost every woman. Excruciating itching of the external genitalia, copious liquid or thick vaginal discharge, with or without odor, pain during urination or sexual intercourse - all this is a reason to be examined by a gynecologist.
It would be fundamentally wrong to try to establish a diagnosis, much less prescribe treatment for yourself. This can lead to dangerous consequences.
One of the most common gynecological problems is vaginal candidiasis. It is more popularly known as thrush.
This is the diagnosis most often made by women when any of the above symptoms appear. For many of them, suppositories or tablets indicated for this ailment help instantly, but for others such treatment turns out to be useless.
Few people know that in addition to banal thrush, there is such a disorder of the vaginal microflora as bacterial vaginosis, as well as a more complex one - bacterial candidiasis. It is the latter that we will dwell on in more detail.
- What is meant by bacterial candidiasis?
- Causes and methods of prevention
- Clinical picture of bacterial candidiasis
- What can modern medicine offer for treatment?
What is meant by bacterial candidiasis?
In fact, you will not find the name of such a pathology in any medical textbook. Why? It's simple, this is not one independent disease, but two parallel deviations in the state of the vaginal microflora: bacterial vaginosis and vaginal candidiasis. These diseases are completely different and most often develop separately from each other. But it happens that they arise simultaneously.
 Bacterial vaginosis involves the uncontrolled proliferation of opportunistic microbes on the vaginal mucosa.
Bacterial vaginosis involves the uncontrolled proliferation of opportunistic microbes on the vaginal mucosa.
Conditionally pathogenic are those microorganisms that are part of a healthy microflora, but under certain conditions can cause the development of pathology.
Since most of the bacteria that cause vaginosis are gardnerella, the second name for this disease is gardnerellosis.
Vaginal candidiasis, also known as thrush, occurs due to the active proliferation of a yeast-like fungus of the genus Candida inside the vagina. The latter is a permanent resident of the vagina of any woman and, like Gardnerella, belongs to opportunistic microorganisms.
Causes and methods of prevention
Since vaginal candidiasis and bacterial vaginosis can develop in a woman’s vagina at the same time, it is logical to suggest that they are caused by similar causes. So, the combination of these two pathologies, called bacterial candidiasis, can occur under the following conditions:

An additional cause of vaginal thrush is infection with a fungus from a sexual partner. The fungus of the genus Candida can develop on any mucous membranes on the human body, so infection is also possible through oral sex.
In most cases, a man may not even suspect that he is a carrier of the disease, since he is generally asymptomatic.
Sometimes there may be redness of the glans penis, a white coating on it, and pain during urination or sex.
How can you protect yourself from this disease, which is quite difficult to treat? In view of the listed factors that can lead to its formation, there are the following measures to prevent the development of the disease. So, it is necessary:

In addition, try not to change sexual partners or use condoms and special antimicrobial suppositories.
Clinical picture of bacterial candidiasis
The disease in question, as we found out, consists of two completely different pathologies that have distinctive manifestations. Pay attention to the comparative table of symptoms of bacterial vaginosis and vaginal candidiasis.
We can say that a fishy smell most often helps to recognize bacterial vaginosis, and a cheesy discharge and severe itching help to recognize thrush.
As you can see, pathologies have a completely different set of symptoms, so the presence of one of them can be easily guessed, especially by an experienced physician. But the fact that you have suffered from bacterial candidiasis can be indicated by a combination of certain symptoms of two diseases.
 For example, the following combinations should lead to a similar conclusion:
For example, the following combinations should lead to a similar conclusion:
- smell of fish + curd discharge,
- fishy smell + severe itching/pain,
- foamy yellow discharge + severe itching/pain.
The above information should in no way serve as an incentive to make an independent diagnosis.
What can modern medicine offer for treatment?
What are the features of the treatment of bacterial candidiasis? In each individual case, the course prescribed by a specialist must be individual. But almost always it takes place in three stages:

During the entire course of treatment for bacterial thrush, it is extremely important to abstain from sex.
Since a man can easily carry yeast-like fungi, with each sexual intercourse he can infect a woman again and again. Doctors often advise partners to undergo treatment together.
The combination of two different abnormalities in the state of the vaginal flora, popularly called bacterial candidiasis, is not always easy to recognize, and even more difficult to cure. The best advice that can be given to a woman suffering from a similar disease is to trust a specialist.
What is candida crouzei and how to treat it?
 In nature, there are a huge number of fungi that are sporophytes. Only when they find themselves in certain comfortable conditions do they become pathogens. Candida krusei is one such pathogen that may be involved in the development of certain types of candidiasis. According to medical statistics, this type of microorganism causes thrush in approximately 1 - 3% of patients, and the disease most often occurs in a chronic form due to incorrect initial diagnosis. Making a mistake when making a diagnosis is completely unforgivable, so not only doctors, but also patients should know what candida cresei is and how to treat it.
In nature, there are a huge number of fungi that are sporophytes. Only when they find themselves in certain comfortable conditions do they become pathogens. Candida krusei is one such pathogen that may be involved in the development of certain types of candidiasis. According to medical statistics, this type of microorganism causes thrush in approximately 1 - 3% of patients, and the disease most often occurs in a chronic form due to incorrect initial diagnosis. Making a mistake when making a diagnosis is completely unforgivable, so not only doctors, but also patients should know what candida cresei is and how to treat it.
Candida crouzei is a tiny microorganism that belongs to the Candida genus of fungi. Humans become infected with it very rarely, although the fungi are present in the air and are found in soil, meat products, vegetables and milk. A person should not have it as part of the microflora. The fungus Candida Cruze infects individuals who have weak immunity. The cause of this condition can be any chronic disease, or the presence of HIV infection or malignant neoplasms.
The habitat of Candida krusei after entering the body is the oral cavity or esophagus. Much less often, it settles on the mucous membranes of the genitals and causes vaginal candidiasis.
Treatment of thrush caused by candida crouzei fungi
While there are many drugs available to treat Candida albicans, the situation with the fungus Candida krusei is much more serious. This pathogen is resistant to antifungal drugs, so they are not only ineffective for the course of therapy, but also extremely dangerous, since the disease becomes chronic. To determine how to treat Candida crouzei fungus, you must first conduct a diagnosis and identify the type of pathogen.
 Fluconazole, unfortunately, is not suitable for fighting such a difficult infection. Citrosept is used to treat candida cruzei. This drug is an extract obtained from grapefruit seeds. It is produced in the form of drops that patients need to take orally. In case of superficial fungal infection of the mucous membranes, you can dilute the extract with vegetable oil and treat the affected surfaces with this composition. The skin can be treated with undiluted medicine. The product actively acts on the cell membrane of the fungus, destroying it, after which its development stops.
Fluconazole, unfortunately, is not suitable for fighting such a difficult infection. Citrosept is used to treat candida cruzei. This drug is an extract obtained from grapefruit seeds. It is produced in the form of drops that patients need to take orally. In case of superficial fungal infection of the mucous membranes, you can dilute the extract with vegetable oil and treat the affected surfaces with this composition. The skin can be treated with undiluted medicine. The product actively acts on the cell membrane of the fungus, destroying it, after which its development stops.
The most effective suppositories for thrush or vaginal candidiasis
Candidal colpitis is a condition of the vaginal flora. Many people mistakenly consider this a sexually transmitted infection. In fact, thrush reflects the state of a woman’s immunity in the current period. It is provoked by many factors - from increased blood sugar levels to gynecological diseases. Treatment of pathology should be comprehensive, taking into account the cause of its occurrence. Often, even the most effective suppositories for thrush can only help for a short period of time if the provoking moments are not eliminated.
Principles of pathology treatment
Only a specialist can prescribe competent treatment. After examination, the gynecologist sometimes recommends additional examination, since thrush is often a marker of other diseases. Such dysbiosis is caused by diabetes mellitus or impaired glucose tolerance (latent form), chronic inflammatory diseases (tuberculosis, HIV, etc.), pathology of the digestive system and others. A predisposition to one or another disease can only be noticed at an appointment.
What should be taken into account during treatment:
- At the beginning of therapy, it is recommended to take a vaginal flora culture to detect fungi of the genus Candida, which are the ones that cause pathology. The study must necessarily include determination of sensitivity to various drugs. The fact is that uncontrolled use of medications often leads to resistance of these fungi to basic drugs. And this way the treatment will be reliably effective.
- In case of candidal colpitis, it is imperative to be examined for sexually transmitted infections. Often women begin to use various suppositories against thrush, which will always be ineffective if there is some additional pathogenic flora.
- It is advisable to sanitize your sexual partner, even if nothing bothers him.
- Chronic forms of candidal colpitis should be treated locally with suppositories and systemically with tablets. In this case, it is advisable to prevent relapse with medication for 3–6 months after the main course.

In the process of treating candidal colpitis, suppositories with different principles of action can be prescribed. Main groups:
- antifungal drugs;
- antibiotics with effects on candida;
- complex suppositories, which contain, in addition to the antifungal agent, other drugs;
- medications to strengthen local immunity.

Effective suppositories for thrush
Fungi of the genus Candida, like bacteria, are rapidly becoming resistant to various drugs. This is primarily due to improper prescription and use of drugs. Today, antifungal drugs, which have long gone out of general use, are sometimes even more effective than the most popular and advertised ones.
Zalain
The active ingredient is sertaconazole, it is one of the latest antifungal drugs. To reduce the symptoms of thrush, the manufacturer recommends using just one candle. This quantity is included in the package. Zalain can be used without worry during menstruation, unlike most similar suppositories.
In chronic forms of candidal colpitis or with a clear clinical picture, the course of treatment should be repeated after one week.
Livarol
The drug contains the active ingredient ketoconazole. This is one of the first antifungal agents. The course requires from 5 to 10 candles. They should be placed into the vagina once a day; it is most convenient to do this at night.
Resistance to ketoconazole quickly develops, so this drug is not suitable for the treatment of recurrent candidal colpitis. It is also not recommended to use Livarol during pregnancy at any stage.
McMiror complex
The product includes nystatin and nifurotel. The course of treatment consists of at least eight suppositories; the medicine can be used during pregnancy and breastfeeding.
Nifurotel is an antibiotic, also active against candida. By prescribing such a drug, one can hope not only for the treatment of candidal colpitis, but also sexually transmitted infections.
Nystatin is one of the first antifungal drugs. For some time, this medicine was supplanted by other, modern analogues, but there are fewer stable forms of it. If you need suppositories for thrush that are inexpensive but effective, you can opt for them.
Clotrimazole
Ginesol
The suppositories contain miconazole. This is an antifungal agent to which resistance develops very slowly, so ginesol is often used for recurrent thrush. The course will require at least seven candles, this is one package. If thrush appears during pregnancy or breastfeeding, suppositories for the treatment of this group can be used without fear.
Miconazole is also included in some complex products, for example, Klion-D, Neo-Penotran. In addition to the main active ingredient, they contain others, for example, antibacterial components.
Gyno-pevaril
The drug contains econazole, one of the latest developed in the treatment of thrush, and this is responsible for its high effectiveness. Depending on the dosage, it can be taken for either three (if 150 mg) or 14 days (if 50 mg). In the first case - for the treatment of acute, first-time candidiasis, in the second - for a recurrent form.
Pimafucin
The composition includes natamycin, an antibiotic from the macrolide group with a pronounced antifungal effect. It is allowed to be prescribed during pregnancy and lactation. The course of treatment is from three to six days. This is one of the most effective and safe drugs.
Lomexin
The active ingredient in the suppositories is fenticonazole, one of the latest antifungal drugs developed. For treatment, only one suppository is needed; in chronic forms, the dose can be increased to two at intervals of a week. Candida resistance to the drug develops very slowly and is well tolerated. But during pregnancy and lactation its use is prohibited. Lomexin is a highly effective vaginal suppository for thrush.
Terzhinan
These are combined action candles. Contains ternidazole, neomycin, nystatin and prednisolone. The advantage of the drug is the parallel treatment of other pathogenic flora, for example, bacterial vaginosis. Also included in the composition, prednisolone quickly relieves itching and burning, which are always present with thrush. Therefore, after the first candle, the woman feels a significant improvement in her health. Terzhinan is a suppository for vaginitis and thrush at the same time.
Polygynax
Also a complex action drug. Contains neomycin, polymyxin and nystatin. They should be used with caution during pregnancy and breastfeeding. This drug is effective for treating not only thrush, but also accompanying inflammation. The course requires from 6 to 12 candles.
Candida colpitis is a signal from the body about a decrease in local defenses. Thrush should be interpreted not as a sexually transmitted infection, but as a state of the vaginal biocenosis. The treatment of pathology should be taken very seriously, since spontaneous prescription of drugs often leads to the development of chronic forms. Only a specialist can prescribe the best suppositories for thrush after a thorough examination.
A rare subspecies of fungi of the genus Candida is Candida krusei. The spores of these fungi are found in the soil, air, and food. The disease affects the oral cavity, esophagus, and mucous membranes of the genitourinary organs. Treatment of candidiasis is complicated by the resistance of Candida krusei to antifungal medications, so the disease often becomes chronic.
Causes of the disease
There are 150 subspecies of Candida fungus. Only 6 of them affect the human body. In 1% of cases, the causative agent of the disease is Candida krusei.
Candida krusei is a tiny microorganism. It is not contained in the microflora of a healthy person. Against the background of weakened immunity, the infectious agent affects the mucous membranes of the gastrointestinal tract, nasopharynx, reproductive organs and urinary system. The causes of fungal infection include:
- HIV infections;
- malignant neoplasms;
- diseases of the endocrine system - diabetes mellitus;
- taking antibiotics or steroid drugs;
- imbalance of the hormonal system;
- lack of vitamins and microelements;
- exhaustion of the body;
- unprotected sexual intercourse;
- failure to comply with personal hygiene rules;
- wounds and scratches on the skin.
Main symptoms
 Vaginal discharge has a strong, unpleasant odor.
Vaginal discharge has a strong, unpleasant odor. Symptoms of the disease depend on the location of the fungus, the speed of its spread and the affected area. A characteristic sign of the disease is an imbalance in the microflora of the mucous membranes. The main symptoms include:
- white coating on the mucous membranes;
- pungent specific odor;
- severe itching in the affected area;
- redness of the mucous membranes;
- erosion in damaged areas;
- pain and burning when swallowing, urinating, sexual intercourse;
- white curdled vaginal discharge;
- white plaque on the head of the penis;
- urethritis, balanitis.
Diagnostic methods
The main task of diagnostic procedures is to determine the causative agent of the disease. Methods for diagnosing Candida cruzei are:
- Microscopy of a smear of discharge. Determines the presence of fungal spores in scrapings from lesions.
- Bacteriological culture. Studies the morphology of the fungus and its sensitivity to antifungal drugs.
- PCR method. Confirms the presence of a yeast-like fungus in the scraping and determines its species.
What is the danger of Candida cruzei?
 A weakened immune system is unable to stop the active growth of the fungus.
A weakened immune system is unable to stop the active growth of the fungus. Candida cruzei has the ability to create a biofilm - a matrix of fungi protected from the immune system. Such colonies of fungal infection are able to resist most antifungal drugs. Therefore, the disease often develops into a chronic form of candidiasis. In the human body, Candida crocus fungi:
- cause allergic reactions;
- release toxins that damage the liver;
- suppress the immune system;
- weaken the body;
- infect the fetus during pregnancy.
Treatment of Candida cruzei
Treatment for Candida crouzea depends on the location of the fungus and the symptoms of the disease. The causative agent of the disease has increased resistance to antifungal therapy. Therefore, it is necessary to treat a fungal infection in a complex manner. The main medications to combat Candida cruzei are presented in the table:
| Medication | Medicinal properties |
|---|---|
| "Citrosept" | The natural composition has an antibacterial effect, prevents the development of pathogenic flora |
| "Clotrimazole", "Ketoconazole", "Tioconazole" | They have a powerful antifungal effect and prevent the development of fungal infections |
| "Nattokinase", "Lumbrokinase" | Restores the functionality of the endocrine, cardiovascular and immune systems |
| "Lactoferrin" | Destroys viral fungal infections |
| "Levorin", "Nystatin" | Antibiotics of natural origin destroy fungal cells |
| "Itraconazole", "Amphotericin B", "Caspofugin" | Have an effective antifungal effect against esophageal candidiasis |
| "Enterol" | Normalizes intestinal microflora and has a pronounced etiopathogenetic effect |
| "Betadine", "Chlorhexidine" | Disinfect affected areas, prevent the spread of fungal infection |
| "Hilak Forte", "Linex" | Normalize the microflora of the gastrointestinal tract |
Treatment of candidiasis caused by the fungus Candida cruzei is carried out only as prescribed by a doctor.