The cause of poisoning can be any chemicals and technical fluids used in industry, agriculture and at home, as well as drugs. Therefore, they are conditionally divided into professional, household and drug poisoning. The lecture will mainly consider those measures of assistance that are provided in case of poisoning with drugs. However, the basic principles of treatment remain valid for other poisonings.
From drugs, poisoning most often occurs when using sleeping pills, analgesics, neuroleptics, antiseptics, chemotherapeutic, anticholinesterase drugs, cardiac glycosides, etc. Poisoning depends on the substance that caused it, on the body and the environment. The substance that caused the poisoning determines the picture of poisoning and the severity. For example, in case of poisoning with anticholinesterase substances (organophosphorus insecticides), symptoms of a sharp increase in the tone of the cholinergic system come to the fore. In case of poisoning with alcohol, sleeping pills, drugs, deep depression of the central nervous system is observed. The speed, severity and some symptoms of poisoning depend on the organism. First of all, the route of entry of the poison into the body (gastrointestinal tract, respiratory tract, skin, mucous membranes) is important, which must be taken into account when providing emergency care. The effect of the poison depends on the age and condition of the victim. Especially sensitive are children and the elderly, in whom poisoning is more severe. The action of the poison is also influenced by environmental factors (temperature, humidity, atmospheric pressure, radiation, etc.).
Emergency care for poisoning includes general and specific measures. They pursue the following goals: 1) prevention of further absorption of the poison into the body; 2) chemical neutralization of the absorbed poison or elimination of its action with the help of an antidote; 3) acceleration of the removal of poison from the body; 4) normalization of impaired body functions with the help of symptomatic therapy. When carrying out these activities, the time factor is of great importance: the earlier therapy is started, the greater the chance of a favorable outcome. The order of the listed measures of assistance may vary in each case and be determined by the nature and severity of the poisoning. For example, with a sharp respiratory depression, the urgent restoration of pulmonary gas exchange is of decisive importance. This is where the doctor's actions should begin.
Prevention of further absorption of the poison. The nature of the measures depends on the way the poison enters the body. If poisoning has occurred by inhalation (carbon monoxide, nitrogen oxides, insecticide aerosols, gasoline vapors, etc.), the victim must be immediately removed from the poisoned atmosphere. If the poison gets on the mucous membranes and skin, it must be washed off with water. If the poison has entered the stomach, it is necessary to do a lavage. The earlier it started washing, the more efficient it is. If necessary, repeat washing is done, since sparingly soluble substances and tablets can linger in the stomach for several hours. Washing is best done through a probe to prevent aspiration of poison and wash water. Simultaneously with washing neutralization or binding of poison in the stomach. For this purpose, potassium permanganate, tannin, magnesium oxide, activated carbon, egg whites, milk are used. Potassium permanganate oxidizes organic poisons, but does not react with inorganic substances. It is added to water during washing at the rate of 1:5000–1:10000. After washing, it must be removed from the stomach, as it has an irritating effect. Activated carbon is a universal adsorbent. It is administered into the stomach in the amount of 20–30 g in the form of an aqueous suspension. The adsorbed poison can be split off in the intestines, so the reacted coal must be removed. Tannin precipitates many poisons, especially alkaloids. It is used in the form of a 0.5% solution. Since the poison can be released, the tannin must also be removed. Magnesium oxide - weak alkali, therefore neutralizes acids. She is appointed at the rate of 3 tbsp. spoons for 2 liters of water. Since magnesium depresses the central nervous system, after washing it must be removed from the stomach. egg whites form insoluble complexes with poisons and have enveloping properties. Has a similar effect milk, however, in case of poisoning with fat-soluble poisons, it cannot be used. If gastric lavage is not possible, you can use emetics. Usually prescribed apomorphine hydrochloride 0.5-1 ml of 0.5% solution s / c. Vomiting can be induced with mustard powder (1 teaspoon per glass of water) or table salt (2 tablespoons per glass of water). When the victim is unconscious, emetics should not be used. Used to remove poison from the intestines saline laxatives. It is better to use sodium sulfate, since magnesium sulfate can cause CNS depression.
Neutralization of the absorbed poison with the help of antidotes. There are substances that can neutralize the action of poisons by chemical binding or functional antagonism. They are called antidotes (antidotes). The action is carried out on the basis of chemical or functional interaction with poisons. Such antidotes as unithiol, dicaptol, sodium thiosulfate, complexones, methemoglobin formers and demethemoglobin formers have chemical (competitive) interactions. Unithiol and dicaptol, due to the presence of two sulfhydryl groups, can bind metal ions, metalloids, cardiac glycoside molecules. The resulting complexes are excreted in the urine. Inhibition of enzymes containing sulfhydryl groups (thiol enzymes) is eliminated. The drugs are highly effective in case of poisoning with antimony, arsenic, mercury, gold compounds. Less effective in case of poisoning with bismuth preparations, salts of chromium, cobalt, copper, zinc, nickel, polonium, cardiac glycosides. In case of poisoning with salts of lead, cadmium, iron, manganese, uranium, vanadium, etc., they are ineffective. Uitiol is administered intramuscularly as a 5% solution. Sodium thiosulfate is used for poisoning with compounds of arsenic, lead, mercury, cyanides, with which it forms low-toxic complexes. Assign in / in the form of a 30% solution. Complexones form pincer (chelate) bonds with most metals and radioactive isotopes. The resulting complexes have low toxicity and are excreted in the urine. To speed up this process, plenty of fluids and diuretics are prescribed. Ethylenediaminetetraacetate (EDTA) is used in the form of disodium salt and calcium disodium salt - tetacine-calcium. Demethemoglobin formers are substances capable of converting methemoglobin to hemoglobin. These include methylene blue, used in the form of "chromosmon" (1% solution of methylene blue in 25% glucose solution), and cystamine. They are used for poisoning with substances that cause the formation of methemoglobin (nitrites and nitrates, phenacetin, sulfonamides, levomycetin, etc.). In turn, substances that cause the formation of methemoglobin (methemoglobin metabolizers) amyl nitrite, sodium nitrite are used to neutralize hydrocyanic acid compounds, since the 3-valent iron of methemoglobin binds cyanions and thereby prevents the blockade of respiratory enzymes. Cholinesterase reactivators (dipiroxime, isonitrosine and etc.), interacting with organophosphorus compounds (chlorophos, dichlorvos, etc.), release the enzyme acetylcholinesterase and restore its activity. They are used for poisoning with anticholinesterase poisons. Widely used for poisoning functional antagonism: for example, the interaction of anticholinergics (atropine) and cholinergic agonists (muscarine, pilocarpine, anticholinesterase substances), histamine and antihistamine drugs, adrenoblockers and adrenergic agonists, morphine and naloxone.
Accelerating the removal of absorbed poison from the body. Treatment of poisoning by method "body wash" occupies a leading position. It is carried out by the introduction of a large amount of fluid and fast-acting diuretics. There is a dilution (hemodilution) of the poison in the blood and tissues and a decrease in its concentration, and the appointment of osmotic diuretics or furosemide accelerates its excretion in the urine. If the patient is conscious, a plentiful drink is prescribed, if unconscious, an intravenous 5% glucose solution or isotonic sodium chloride solution is administered. This method can only be used while maintaining the excretory function of the kidneys. To accelerate the excretion of acidic compounds, urine is alkalized with sodium bicarbonate, alkaline compounds are excreted faster with acidic urine (ammonium chloride is prescribed). In case of poisoning with barbiturates, sulfonamides, salicylates, and especially poisons that cause hemolysis, apply exchange transfusion and plasma replacement solutions(reopoliglyukin, etc.). With damage to the kidneys (for example, with sublimate poisoning), use the method hemodialysis artificial kidney machine. An effective way to detoxify the body is hemosorption, carried out with the help of special sorbents that adsorb poisons in the blood.
Symptomatic therapy of functional disorders. It is aimed at eliminating the symptoms of poisoning and restoring vital functions. In case of violations breathing shown intubation, suction of the contents of the bronchi, artificial ventilation of the lungs. When the respiratory center is depressed (hypnotics, drugs, etc.), analeptics (caffeine, cordiamine, etc.) can be administered. In case of morphine poisoning, its antagonists (nalorphine, naloxone) are used to restore breathing. If pulmonary edema occurs, complex treatment is carried out (see lecture 16). The development of bronchospasm is an indication for the appointment of bronchodilators (agonists, anticholinergics, aminophylline). Of great importance is the fight against hypoxia. For this purpose, in addition to drugs that normalize breathing and blood circulation, oxygen inhalation is used. Under oppression cardiac activity fast-acting cardiac glycosides (strophanthin, corglicon), dopamine are used, and in case of heart rhythm disturbances, antiarrhythmic drugs (novocainamide, aymalin, ethmozine, etc.) are used. In acute poisoning, in most cases it decreases vascular tone and blood pressure. Hypotension leads to a deterioration in the blood supply to tissues and the retention of poisons in the body. To combat hypotension, vasopressor drugs (mezaton, norepinephrine, epinephrine, ephedrine) are used. In case of poisoning with poisons that excite the central nervous system, convulsions often occur, for the relief of which sibazon, sodium oxybutyrate, thiopental sodium, magnesium sulfate, etc. are used. Allergic reactions may be accompanied by the development of anaphylactic shock, which requires urgent measures: the introduction of adrenaline, glucocorticoids hydrocortisone), bronchodilators, cardiac glycosides, etc. One of the frequent symptoms of severe poisoning is a coma. Coma usually occurs when poisoning with poisons that depress the central nervous system (alcohol, barbiturates, morphine, etc.). Treatment is carried out taking into account the type of coma, its severity, and is aimed at restoring impaired functions and metabolism. When pain occurs, narcotic analgesics are used, but the state of breathing must be taken into account. Great importance is attached to the correction of water and electrolyte balance and the acid-base state of the body.
Thus, emergency care for acute poisoning includes a set of measures, the choice and sequence of which depend on the nature of the poisoning and the condition of the victim.
APPS
QUESTIONS TO PREPARE FOR THE PHARMACOLOGY EXAM
1. Cardiac glycosides. The history of the appearance in medicine of plants containing cardiac glycosides. Types of drugs. pharmacological effects.
2.MD of cardiac glycosides. Criteria for evaluating the therapeutic effect.
3. Comparative characteristics of cardiac glycoside preparations (activity, absorption in the gastrointestinal tract, development rate and duration
actions, cumulation).
4. Clinical manifestations of intoxication with cardiac glycosides, their treatment and prevention.
5. Classification of antiarrhythmic drugs.
6. Comparative characteristics of antiarrhythmic drugs, which are dominated by a direct effect on the heart. Indications for use.
7. Comparative characteristics of antiarrhythmic drugs acting through autonomic innervation. Indications for use.
8. Classification of drugs used in coronary heart disease, based on the principles of eliminating oxygen deficiency and on application.
9. Means that reduce myocardial oxygen demand and improve its blood supply (nitroglycerin preparations, calcium antagonists).
10.Means that reduce myocardial oxygen demand (beta-blockers, amiodarone).
11. Means that increase the delivery of oxygen to the heart (coronary active).
12. Means used in myocardial infarction. Principles of drug therapy for myocardial infarction.
13. Classification of antihypertensive drugs. Principles of antihypertensive therapy.
14. Hypotensive drugs that lower the tone of vasomotor centers. Main and side effects.
15. Mechanism of hypotensive action of ganglioblockers. main effects. Application. Side effect.
16. Localization and mechanism of hypotensive action of sympatholytics and alpha-blockers. Side effects.
17. Mechanism of hypotensive action of beta-blockers. Main and side effects. Application in cardiology.
18. Myotropic antihypertensive drugs (peripheral vasodilators). Mechanism of hypotensive action of calcium channel blocker. Main and side effects. Application.
19. Mechanism of hypotensive action of agents affecting water-salt metabolism (diuretics), their use.
20. The mechanism of the hypotensive action of substances that affect the renin-angiotensin system, their use.
21. Means used to relieve hypertensive crisis. 22. Hypertensive drugs. Indications for use. Side effect.
23. Means used for cerebral circulation insufficiency. The main groups of drugs and the principles of therapy for cerebrovascular accidents.
24.Basic principles and remedies for migraine liver.
25. Anti-atherosclerotic drugs. Classification. MD and principles of application of anti-atherosclerotic drugs.
26. Classification of drugs that affect the blood system. Means that stimulate erythropoiesis (antianemic). MD and application.
27. Means stimulating and inhibiting leukopoiesis: MD, application. 28. Means that prevent platelet aggregation: MD, application.
29. Direct acting anticoagulants: MD, indications for use, contraindications, side effects.
30. Anticoagulants of indirect action: MD, indications and contraindications, PE.
31. Fibrinolytic and antifibrinolytic agents. MD, application.
32. Means that increase blood coagulation (coagulants): MD, application, PE.
33. Classification of diuretics. Localization and MD of diuretics affecting the function of the epithelium of the renal tubules. Their comparative characteristics, application.
34. Xanthine derivatives and osmotic diuretics: MD, indications for use.
35. Antigout agents: MD, indications and contraindications.
36. Means used to enhance and weaken labor activity: MD, main and side effects.
37. Means used to stop uterine bleeding: MD, effects.
38. Classification of vitamins, types of vitamin therapy. Preparations of vitamins B1, B2, B5, b6. Influence on metabolic processes, pharmacological effects, application.
39. Preparations of vitamins PP, C, R. Influence on metabolism. main effects. Indications for the use of individual drugs.
40. Vitamin D preparations: influence on calcium and phosphorus metabolism, Application, PE.
41. Preparations of vitamins A, E, K: main effects, application, PE.
42. Hormonal preparations. Classification, sources of obtaining,
application.
43. Preparations of adrenocorticotropic, somatotropic and thyroid-stimulating hormones of the anterior pituitary gland. indications for their use.
44. Preparations of hormones of the posterior pituitary gland. Indications for appointment.
45. Preparations of thyroid hormones. Main and side effects. Indications for appointment.
46. Antithyroid drugs: MD, indications for prescription, PE.
47. Parathyroid hormone preparation: main effects, application. Significance and use of calcitonin.
48. Preparations of pancreatic hormones. MD of insulin, influence on metabolism, main effects and application, overdose complications, their treatment.
49. Synthetic antidiabetic agents. Possible MD, application.
50. Hormones of the adrenal cortex. Glucocorticoids and their synthetic substitutes. Pharmacological effects, indications for use, PE.
51. Mineralocorticoids: influence on water-salt metabolism, indications for use.
52. Female sex hormones and their preparations: main effects, indications for use. contraceptives.
53. Preparations of male sex hormones: main effects, application.
54. Anabolic steroids: influence on metabolism, application, PE.
55. Acids and alkalis: local and resorptive action, use to correct the acid-base state. Acute acid and alkali poisoning. principles of treatment.
56. Participation of sodium and potassium ions in the regulation of body functions. The use of preparations of catria and potassium.
57. The role of calcium and magnesium ions in the regulation of body functions. The use of calcium and magnesium preparations. Antagonism between calcium and magnesium ions.
58. Principles of correction of water and electrolyte balance disorders. Plasma substitute solutions. Solutions for parenteral nutrition.
59. Basic antiallergic drugs: MD and indications for use.
60. Antihistamines: classification, MD and indications for use.
61. Immunostimulating (immunomodulatory) agents: MD application.
62. The history of the use of antiseptics (A.P. Nelyubin, I. Zemelweis, D. Lister). Classification of antiseptics. Conditions that determine antimicrobial activity. Basic MD.
63. Halogen-containing substances, oxidizing agents, acids and alkalis: MD. application.
64. Metal compounds: MD, local and resorptive action, features of the use of individual drugs. Poisoning with salts of heavy metals. Principles of therapy.
65. Antiseptic agents of aliphatic and aromatic series and group of dyes. Features of action and application.
66. Detergents, derivatives of nitrofuran and biguanides. Their antimicrobial properties and uses.
67. Classification of chemotherapeutic agents. Basic principles of chemotherapy of infectious diseases.
68. Sulfanilamide preparations: MD, classification, use, PE.
69. Sulfanilamide preparations acting in the intestinal lumen. Indications for appointment. Combined preparations of sulfonamides with trimethoprim: MD, application. Sulfonamides for local use.
70. Antimicrobial agents of the nitrofuran group: MD, indications for use.
71. Antimicrobial agents of different groups: mechanisms and spectra of action, indications for use, PE.
72. History of obtaining antibiotics (research by L. Pasteur, I. I. Mechnikov, A. Fleming, E. Chain, Z. V. Ermolyeva). Classification of antibiotics according to the spectrum, nature (type) and mechanism of antimicrobial action. The concept of basic and reserve antibiotics.
73. Biosynthetic penicillins. Spectrum and MD. Characteristics of drugs. PE.
74. Semi-synthetic penicillins. Their features in comparison with biosynthetic penicillins. Characteristics of drugs.
75. Cephalosporins: spectrum and MD, characteristics of preparations.
76. Antibiotics of the erythromycin group (macrolides): spectrum and MD, characteristics of preparations, PE.
77. Antibiotics of the tetracycline group: spectrum and MD, characteristics of drugs, PE, contraindications.
78. Antibiotics of the chloramphenicol group: spectrum and MD, indications and contraindications for prescription, PE.
7 9. Antibiotics of the aminoglycoside group: spectrum and MD, drugs, PE.
80. Antibiotics of the polymyxin group: spectrum and MD, application, PE.
81. Complications of antibiotic therapy, prevention and treatment measures.
82. Anti-spirochetal (anti-syphilitic) drugs: MD of certain groups of drugs, their use, side effects.
83. Anti-tuberculosis drugs: classification, MD, application, PE.
84. Antiviral agents: MD and application.
85. Antimalarial drugs: the direction of action of drugs on various forms of plasmodium, the principles of treatment, individual and public chemoprophylaxis of malaria. PE drugs.
86. Protivoame6nye drugs: features of the action of drugs on amoebas in different places of localization, indications for use, PE.
87. Means used for the treatment of giardiasis and trichomonadosis. Comparative efficacy of drugs.
88. Means used for the treatment of toxoplasmosis, balantidiasis, leishmaniasis. Characteristics of drugs.
89. Antifungal agents. Differences in the spectrum of action and indications for the use of individual drugs, PE.
90. Classification of antihelminthic drugs. Means used for intestinal nematodes. Characteristics of preparations, PE.
91. Means used for intestinal cestodosis. Preparations, application, PE,
92. Means used for the treatment of extraintestinal helminthiases.
93. Anticancer drugs. Classification. PE drugs. Characterization of alkylating agents.
94. Characteristics of antitumor agents of the antimetabolite group, herbal agents. Complications in the appointment of antiblastoma drugs, their prevention and treatment.
95. Antibiotics with antitumor activity. Hormonal and enzyme preparations used in tumor diseases.
96.0 basic principles of treatment of acute poisoning with pharmacological substances. The use of antidotes, functional antagonists and stimulants of functions.
97. Treatment of poisoning with anticholinesterase agents.
Note: here are questions on the topics of the 2nd part of the course of lectures; the rest of the exam questions are contained in the 1st part.
MEDICINES YOU NEED TO BE ABLE TO PRESCRIBE IN THE PHARMACOLOGY EXAM
Note: when prescribing drugs in prescriptions, the student must know their group affiliation, the main MD, the features of pharmacokinetics and pharmacodynamics, indications and contraindications for prescribing, PE, be able to calculate doses for elderly and senile patients and young children.
Lecture 18. Cardiac glycosides. 3
Lecture 19. Antiarrhythmic drugs. 9
Lecture 20. Antianginal drugs. 15
Lecture 21. Antihypertensive (hypotensive) drugs. Hypertensive agents. 21
Lecture 22. Drugs used for cerebrovascular insufficiency. Anti-atherosclerotic agents. 29
Lecture 23. Drugs affecting the blood system. 36
Lecture 24. Diuretics. Anti-gout agents. 44
Lecture 25. Drugs affecting the contractile activity of the myometrium. 50
Lecture 26. Vitamin preparations. 53
Lecture 27. Hormonal drugs. 60
Lecture 28. Hormonal drugs (continued). 65
Lecture 29. Drugs for the regulation of water and electrolyte balance, acid-base status and parenteral nutrition. 71
Lecture 30. Antihistamines and other antiallergic drugs. Immunomodulating agents. 77
Lecture 31. Disinfectants and antiseptics. Basic principles of chemotherapy. 81
Lecture 32. Antibiotics. 85
Lecture 33 Nitrofuran derivatives. Synthetic antimicrobial drugs of different structure. Antisyphilitic drugs. Antiviral drugs. Antifungal drugs. 94
Lecture 34. Antituberculous drugs. Antiprotozoal drugs. 101
Lecture 35 Antitumor agents. 108
Lecture 36. Principles of therapy for acute poisoning. 114
Questions to prepare for the pharmacology exam. 118
Drugs to be able to write prescriptions in the pharmacology exam 123
Regardless of the poisonous substance, the treatment of all acute poisonings is carried out according to the following principles:
1. Assessment of vital functions and correction of identified disorders.
2. Stopping the entry of poison into the body.
3. Removal of unabsorbed poison.
4. The use of antidotes.
5. Removal of absorbed poison.
6. Symptomatic therapy.
1. The assessment of the state is carried out according to the algorithm "ABCD".
"A" - restoration of airway patency.
"B" - effective ventilation. If necessary, conducting auxiliary ventilation or, if necessary, artificial lung ventilation (ALV) through an endotracheal tube.
"C" - assessment of blood circulation. Evaluate the color of the skin, blood pressure (BP), heart rate (HR), saturation (SpO 2), electrocardiography (ECG), diuresis. Catheterization of the veins and the installation of a urinary catheter are performed, if necessary, an appropriate medical correction.
"D" is an assessment of the level of consciousness. Depression of consciousness is the most common complication of poisoning. With depression of consciousness, it is necessary to perform tracheal intubation, since this is often combined with respiratory depression. In addition, inhibition of cough and gag reflexes can lead to the development of aspiration.
The presence of pronounced arousal, convulsions also require medical treatment.
In the presence of impaired consciousness, it is necessary to carry out differential diagnosis with CNS injuries, hypoglycemia, hypoxemia, hypothermia, CNS infections, even if the diagnosis is obvious.
"E" - re-evaluation of the patient's condition and the adequacy of the actions performed. It is carried out systematically after each manipulation.
2. Preventing poison from entering the body performed during the first aid phase. Necessary:
Remove the victim from the atmosphere that caused the poisoning;
If poison enters through the skin (gasoline, FOS), wash the skin with running water and soap. (In case of FOS poisoning, the skin can be treated with a 2-3% solution of ammonia or a 5% solution of baking soda (sodium bicarbonate); then with 70% ethyl alcohol and again with running water and soap). Skin rubbing should be avoided.
If the poison gets on the mucous membrane of the eyes, it is recommended to rinse the eyes with isotonic sodium chloride solution.
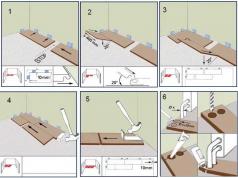
3. Removal of unabsorbed poison. The main way to remove poison from the gastrointestinal tract is gastric lavage. However, in case of poisoning with mushrooms, berries, preparations in the form of large tablets, initially (before gastric lavage) it is advisable to induce vomiting (if there was none) by pressing on the root of the tongue in order to remove large fragments. Contraindications to the reflex induction of vomiting: poisoning with substances that damage the mucous membrane, convulsive readiness and convulsions, impaired consciousness and coma.
Gastric lavage is an obligatory part of medical care, the stomach is washed, regardless of the period of exposure to the poison. There are no absolute contraindications for this method. In case of poisoning with some poisons, the washing procedure has some limitations. So, in case of poisoning with cauterizing poisons, washing is possible only in the first hour, because. in the future, this procedure can lead to perforation of the gastrointestinal tract. In case of poisoning with barbiturates, gastric lavage is carried out in the first 2-3 hours, then the tone of smooth muscles decreases, the cardiac sphincter and regurgitation may open, therefore, in the future, only suction of the stomach contents is performed.
In unconscious patients, gastric lavage is performed after tracheal intubation, because. aspiration is possible. Flushing is carried out through a probe, the setting of which is performed orally, which allows the use of a thicker probe. The depth of standing is determined by the distance from the edge of the teeth to the xiphoid process. Cool tap water is used for washing, a single volume of liquid in adults is not > 600 ml, in children under 1 year old - 10 ml / kg, after 1 year - 10 ml / kg + 50 ml for each subsequent year. The contents of the stomach are drained and sent for toxicological examination. The total volume of liquid is< 7 л (до 10-15 л), промывают до чистых промывных вод. При отравлении липофильными ядами (ФОС, анальгин, морфин, кодеин) желательны повторные промывания через 2-3 часа, т.к. возможна печеночно-кишечная рециркуляция. Повторение процедуры также необходимо при отравлении таблетированными формами, поскольку их остатки могут находиться в складках желудка 24-48 часов.
After gastric lavage, it must be injected into the stomach with orbents: activated carbon - 0.5-1.0 / kg in powder form. Re-appointment of activated charcoal is carried out with the aim of interrupting the enterohepatic circulation.
Along with charcoal are usually recommended laxatives- vaseline oil 0.5-1 ml / kg, it is possible to use a 10-20% magnesium solution at a dose of 250 mg / kg Their necessity is due to the fact that the sorbent binds the toxin only for 2-2.5 hours, and then splits off again, therefore it is necessary to withdraw this complex as soon as possible. Contraindications to the appointment of laxatives: poisoning with iron preparations, alcohol, lack of peristalsis, recent operations on the intestines.
To remove unabsorbed poison from the intestine, it is possible to carry out intestinal lavage, setting high siphon enemas.
4. Specific (pharmacological) antidote therapy.
The radical neutralization of the poison and the elimination of the consequences of its action can in many cases be achieved with the help of antidotes. An antidote is a drug that can eliminate or weaken the specific effect of a xenobiotic by immobilizing it (for example, with chelating agents), reducing the penetration of a poison to effector receptors by reducing its concentration (for example, with adsorbents) or counteracting at the receptor level (for example, with pharmacological antagonists). There is no universal antidote (an exception is activated carbon - a non-specific sorbent).
Specific antidotes exist for a small number of toxicants. the use of antidotes is far from a safe measure, some of them cause serious adverse reactions, so the risk of prescribing antidotes should be comparable to the effect of its use.
When prescribing an antidote, one should be guided by the basic principle - it is used only if there are clinical signs of poisoning with the substance for which this antidote is intended.
Classification of antidotes:
1) Chemical (toxicotropic) antidotes affect the physicochemical state of the substance in the gastrointestinal tract (activated charcoal) and the humoral environment of the body (unithiol).
2) Biochemical (toxicokinetic) antidote s provide a beneficial change in the metabolism of toxic substances in the body or the direction of biochemical reactions in which they participate, without affecting the physicochemical state of the toxic substance itself (cholinesterase reactivators in case of FOS poisoning, methylene blue in case of poisoning with methemoglobin formers, ethanol in case of methanol poisoning).
3) Pharmacological (symptomatic) antidotes have a therapeutic effect due to pharmacological antagonism with the action of the toxin on the same functional systems of the body (atropine in case of poisoning with organophosphorus compounds (FOS), prozerin in case of poisoning with atropine).
4) Antitoxic immunotherapy received the greatest distribution for the treatment of poisoning with animal venoms when bitten by snakes and insects in the form of antitoxic serum (anti-snake - "antigyurza", "anticobra", polyvalent anti-snake serum; anti-karakurt; immune serum against digitalis preparations (digitalis antidote)).
Antidote therapy retains its effectiveness only in the early, toxicogenic phase of acute poisoning, the duration of which is different and depends on the toxicokinetic characteristics of a given toxic substance. Antidote therapy plays a significant role in the prevention of conditions of irreversibility in acute poisoning, but does not have a therapeutic effect in their development, especially in the somatogenic phase of these diseases. Antidote therapy is highly specific, and therefore can be used only if there is a reliable clinical and laboratory diagnosis of this type of acute intoxication.
5. Removal of absorbed poison is carried out by strengthening the natural and the use of artificial detoxification of the body, as well as with the help of antidote detoxification.
Stimulation of natural detoxification achieved by stimulating excretion, biotransformation and activity of the immune system.
The basic principles of detoxification in the event of drug poisoning are as follows:
1. It is necessary to provide the patient with a delay in the absorption into the blood of a toxic substance that has entered the body.
2. An attempt should be made to remove the toxic substance from the patient's body.
3. It is necessary to eliminate the effect of the substance that has already been absorbed into the body.
4. And of course, adequate symptomatic therapy for any manifestations of acute poisoning will be necessary.
1) To do this, induce vomiting or wash the stomach. Vomiting is induced mechanically, by taking concentrated solutions of sodium chloride or sodium sulfate, by administering the emetic apomorphine. In case of poisoning with substances that damage the mucous membranes (acids and alkalis), vomiting should not be induced, as additional damage to the esophageal mucosa will occur. More effective and safe gastric lavage with a probe. To delay the absorption of substances from the intestines give adsorbents and laxatives. In addition, bowel lavage is carried out.
If the substance that caused intoxication is applied on the skin or mucous membranes, Rinse them thoroughly (preferably with running water).
When exposed to toxic substances through the lungs stop inhaling
At subcutaneous injection of a toxic substance, its absorption from the injection site can be slowed down by injections of an adrenaline solution around the injection site, as well as cooling this area (an ice pack is placed on the skin surface). If possible, apply a tourniquet
2) If the substance has been absorbed and has a resorptive effect, the main efforts should be aimed at removing it from the body as soon as possible. For this purpose, forced diuresis, peritoneal dialysis, hemodialysis, hemosorption, blood replacement, etc. are used.
forced diuresis method consists in a combination of water load with the use of active diuretics (furosemide, mannitol). The forced diuresis method can only remove free substances that are not associated with blood proteins and lipids.
At hemodialysis (artificial kidney)) the blood passes through the dialyzer with a semi-permeable membrane and is largely freed from non-protein-bound toxic substances (eg barbiturates). Hemodialysis is contraindicated with a sharp decrease in blood pressure.
Peritoneal dialysis consists in washing the peritoneal cavity with an electrolyte solution
Hemosorption. In this case, toxic substances in the blood are adsorbed on special sorbents (for example, on granular activated carbon coated with blood proteins).
Blood replacement. In such cases, bloodletting is combined with a transfusion of donor blood. The use of this method is most indicated for poisoning with substances that act directly on the blood,
3) If it is established which substance caused the poisoning, then they resort to detoxifying the body with the help of antidotes.
Antidotes name the means used for the specific treatment of chemical poisoning. These include substances that inactivate poisons through chemical or physical interaction or through pharmacological antagonism (at the level of physiological systems, receptors, etc.)
4) First of all, it is necessary to support vital functions - blood circulation and respiration. For this purpose, cardiotonic drugs are used, substances that regulate the level of blood pressure, agents that improve microcirculation in peripheral tissues, oxygen therapy is often used, sometimes respiratory stimulants, etc. If unwanted symptoms appear that aggravate the patient's condition, they are eliminated with the help of appropriate drugs. So, convulsions can be stopped with the anxiolytic diazepam, which has a pronounced anticonvulsant activity. With cerebral edema, dehydration therapy is carried out (using mannitol, glycerin). Pain is eliminated by analgesics (morphine, etc.). Much attention should be paid to the acid-base state and, in case of violations, the necessary correction should be carried out. In the treatment of acidosis, sodium bicarbonate solutions, trisamine are used, and in alkalosis, ammonium chloride is used. It is equally important to maintain fluid and electrolyte balance.
Thus, the treatment of acute drug poisoning includes a complex of detoxification measures combined with symptomatic and, if necessary, resuscitation therapy.
Emergency care for acute poisoning implies the implementation of therapeutic measures aimed at stopping the further intake of poison into the body and accelerating its elimination by active detoxification methods; pathogenetic treatment - the use of specific antidotes (neutralizing, reducing the toxicity of a toxic substance or changing its metabolism in the body); symptomatic therapy (maintenance and protection of the functions of organs and systems of the body that have undergone a predominant lesion); transportation of the patient to the hospital.
Detoxification therapy includes measures to reduce adsorption (accumulation of poison in the body), which is achieved by inducing vomiting (“restaurant method”), gastric tube lavage, the introduction of sorbents (for example, activated charcoal) inside, if necessary, again, increasing the elimination of poison by introducing fluid and stimulating diuresis .
Primary emergency care depends on the route of entry of the toxic substance. If poison gets inside, an emergency is required gastric lavage through the probe. It is most effective in the first hour of poisoning, therefore, if the patient cannot be immediately hospitalized, this procedure is performed where the poisoning occurred (at home, at work, etc.).
If the patient is conscious, in the absence of a gastric tube, gastric lavage is sometimes carried out, causing artificial vomiting. Previously, the patient is given 4-5 glasses of water to drink, and then they press with a spatula on the root of the tongue or irritate the back wall of the pharynx. In some cases, drugs that cause vomiting are used (injections of apomorphine, emetine, etc.).
Intentional induction of vomiting and the use of emetics are strictly contraindicated in children under 5 years of age, patients in a soporous or unconscious state (in the absence of vanilla and laryngeal reflexes, there is a high risk of aspiration of vomit into the respiratory tract), as well as in case of poisoning with cauterizing poisons (if the substance passes again through the esophagus, additional harm will be done to the body).
To prevent aspiration of vomit into the respiratory tract and to prevent lung damage in case of poisoning with caustic substances (for example, strong acids, alkalis, or if the patient is unconscious), gastric lavage is performed after preliminary intubation of the trachea with a tube with an inflated cuff. Gastric lavage is best done with the patient lying on his left side, with his head down, through a thick gastric tube, at the end of which a funnel is fixed.
Before the start of the procedure, the patient is removed with a tampon mucus and vomit from the mouth, remove dentures, free from tight clothing. The probe is lubricated with vaseline or sunflower oil and inserted inside along the back of the pharynx. The funnel of the probe is raised to the level of the patient's face and 300-500 ml of water at room temperature (18 ° C) is poured into it. The funnel filled with liquid is raised 25-30 cm above the patient's head, and when the liquid level reaches the neck of the funnel, the latter is lowered 25-30 cm below the level of the patient's face and overturned.
If, after lowering the funnel, the liquid does not flow back, you should change the position of the probe in the stomach or rinse the probe with water using a Janet syringe. The first portion of the wash water is collected for testing for the content of the poison, after which the procedure is repeated until clean wash water is obtained. The presence of blood in the wash water is not an indication to complete the procedure. An adult patient for a thorough gastric lavage usually requires at least 12-15 liters of water.
Salt is usually added to the water (2 tablespoons per 1-2 liters), which causes spasm of the pyloric part of the stomach, thus creating an obstacle to the entry of poison into the small intestine, where the main absorption of toxic substances occurs. Table salt should not be used in case of poisoning with cauterizing poisons (acids, alkalis, salts of heavy metals), since in this case it has an additional irritating effect.
Patients who are in an unconscious state (for example, in case of severe poisoning with sleeping pills or organophosphorus compounds), washing is repeated 2-3 times during the first day from the moment of poisoning. This is due to the fact that in a coma, the absorption of a toxic agent is sharply slowed down, and a significant amount of unabsorbed substance is usually deposited in the gastrointestinal tract. In addition, some substances (morphine, benzodiazepines) are excreted by the gastric mucosa, and then absorbed again. Finally, tablets in the folds of the gastric mucosa may not dissolve for a long time.
After washing, as a laxative, in order to accelerate the release of intestinal contents, 100-150 ml of a 30% solution of sodium sulfate or magnesium sulfate is injected into the stomach (for poisoning with water-soluble poisons) or 100 ml of vaseline oil (for poisoning with fat-soluble poisons). The use of saline laxatives in case of poisoning with cauterizing poisons is contraindicated.
Adsorption of toxic substances in the gastrointestinal tract(including alkaloids - atropine, cocaine, strychnine, opiates, etc., cardiac glycosides) are carried out with activated charcoal inside. The stomach is washed with a suspension of activated carbon (2-4 tablespoons per 250-400 ml of water), it is administered through a tube before and after washing in the form of a slurry (1 tablespoon of powder or 50-100 mg of activated carbon in the form of tablets is dissolved in 5-10 ml of water).
Toxic substances, usually deposited in the small intestine, are removed with the help of "intestinal lavage" - endoscopic sounding of the intestine and washing it with a specially prepared electrolyte solution. A cleansing enema may be given.
With inhalation poisoning with gaseous poisons first of all, it is necessary to take the victim out of the affected atmosphere (medical personnel working in the affected area must have insulating protective equipment - a gas mask), lay him in such a way as to ensure the patency of the respiratory tract, first freeing him from restrictive clothing, warm up and start oxygen inhalation.
Exposure of toxic substances to exposed skin or mucous membranes requires their immediate removal by washing the affected surface with cool running water (not higher than 18 ° C) or an antidote. In case of acid contact with the skin, clean water with soap or a soda solution is used, in case of alkali burns, a 2% solution of citric acid is used. When washing the eyes and nasopharynx, in addition to running water, you can use a 1% solution of novocaine. If toxic substances have been introduced into the body cavities, they are also washed with cool water or sorbents using an enema or douching.
With s / c, / c, / m administration of toxic doses of drugs or snake bites, ice packs are applied to this area for 6-8 hours. To reduce the absorption of poison, 0.3 ml of a 0.1% solution of adrenaline and 5 ml of a 0.5% solution of novocaine are injected directly into the injection site, above the injection site toxins conduct a circular novocaine blockade of the limb, provide immobilization of the limb for the duration of the edema.
With a high concentration of the injected drugs during the first 30 minutes after the injection, you can make a cruciform incision at the injection site and apply a bandage with a hypertonic solution. The imposition of a tourniquet on a limb is contraindicated.
To remove the absorbed poison from the body in the hospital, measures are taken to enhance the processes of cleansing the body of toxic products. Detoxification of the body can be started already at the pre-hospital stage, its main method is forced diuresis with the use of osmotic diuretics (urea, mannitol) or saluretics (lasix), which increase urination.
Strengthening the excretory function of the kidneys accelerates the excretion of poison circulating in the bloodstream with urine by 5-10 times. Direct indications for forced diuresis are poisoning with water-soluble substances that are excreted from the body mainly through the kidneys. Forced diuresis includes three successive stages: preliminary water load, intravenous administration of diuretics and replacement administration of electrolyte solutions.
At the same time, monitoring of hourly diuresis is established by placing a urinary catheter, the concentration of a toxic substance in the blood and urine, the content of electrolytes in the blood, and hematocrit (the ratio of formed elements and blood plasma) are determined. These parameters are controlled both during forced diuresis and after its completion; if necessary, carry out the correction of water and electrolyte disorders.
Preliminary water load in mild cases is usually 1.5-2 liters of water orally for 1 hour; severe poisoning with the development of exotoxic shock (decrease in the volume of circulating fluid, dehydration) require intravenous administration of plasma-substituting solutions (polyglucin, hemodez) and 5% glucose solution, Ringer's solution in a volume of at least 1-1.5 liters. Patients in an unconscious state or with severe dyspeptic symptoms, frequent vomiting increase the amount of fluid administered (under the control of diuresis) to 3-5 liters.
The absence of spontaneous diuresis is regulated by intravenous administration of furosemide at a dose of 80 to 200 mg. Osmotic diuretics (30% urea solution or 15% mannitol solution) are injected intravenously over 10-15 minutes, at the rate of 1 g/kg. A side effect of furosemide, especially with repeated administration, is a significant loss of potassium and other electrolytes, which requires appropriate correction.
The replacement administration of electrolyte solutions begins immediately after the end of the administration of the osmotic diuretic, continuing the water load with an electrolyte solution (4.5 g of potassium chloride, 6 g of sodium chloride and 10 g of glucose per 1 liter of solution), at a rate of intravenous administration corresponding to diuresis rate (not less than 800-1200 ml/h).
If necessary, forced diuresis is repeated every 4-5 hours, until the complete removal of the toxic substance from the bloodstream. Its implementation is contraindicated in acute heart or vascular insufficiency (persistent collapse, stage II-III circulatory failure), impaired renal function (anuria, oliguria, azotemia, increased blood creatinine content of more than 5 mg%). A decrease in the effectiveness of this method in patients older than 50 years was noted.
An increase in diuresis and an increase in the release of poison (along with a water load) also contributes to alkalization of the blood, which is indicated for poisoning with hemolytic and other poisons that cause severe metabolic acidosis, as well as for the treatment of acute poisoning with drugs whose solutions are acidic (barbiturates, salicylates, etc.).
In addition, a change in the reaction of the blood to the alkaline side accelerates the release of poison from the cells of the body into the extracellular fluid. Under the control of the acid-base state, in order to maintain a constant alkaline reaction of urine (pH over 8.0), a 4% solution of sodium bicarbonate is injected intravenously - 500-1500 ml per day. The alkaline reaction of urine is maintained for several days.
Contraindications to alkalization of the blood are the same as for the water load with forced diuresis. In the absence of impaired consciousness and vomiting, sodium bicarbonate can be given orally 4-5 g every 15 minutes during the first hour, then 2 g every 2 hours; also recommend a plentiful alkaline drink (up to 3-5 liters per day). The fight against acidosis is carried out very carefully due to the risk of developing alkalosis, a more severe and difficult to correct condition.
In a hospital, in case of poisoning with water-soluble poisons that can penetrate the semi-permeable membrane of the dialyzer, extracorporeal detoxification methods (hemodialysis, hemofiltration and hemodiafiltration, ultrafiltration) are used, which are 2-3 times superior to forced diuresis in terms of clearance (poison release per unit time - blood purification rate) 2-3 times.
Indications for extracorporeal detoxification methods are the early toxigenic stage of poisoning with a lethal level of the concentration of a toxic substance in the blood, a progressive deterioration in the background of maintenance therapy, and the somatogenic stage with the threat of life-threatening complications, the development of acute renal or hepatic insufficiency with a slowdown in the elimination of toxic substances from the body. , hyperhydration of the body.
The most effective method of removing water-insoluble toxic substances from the body is detoxification hemosorption, during which the patient's blood is passed through a detoxifier (a special column with activated carbon or another type of sorbent).
To remove toxic substances deposited in adipose tissues or capable of firmly binding to plasma proteins, peritoneal dialysis is used, which, in terms of clearance of toxic substances, is not inferior to forced diuresis and is often used simultaneously with it.
To double the rate of excretion of toxic substances (especially psychotropic action) by enhancing the processes of biotransformation of toxic substances and correcting violations of homeostasis indicators allows physiohemotherapy - magnetic, ultraviolet, laser, chemohemotherapy (intravenous injection of 400 ml of 0.06% sodium hypochlorite solution).
In case of acute poisoning with chemicals that cause toxic damage to the blood (with massive hemolysis, the formation of methemoglobin, a prolonged decrease in plasma cholinesterase activity, etc.), a blood replacement operation is indicated (in the amount of 2-3 liters of donor individually selected single-group Rh-compatible blood).
To improve the rheological properties of blood, 15-20% of the volume of the transfused liquid should be plasma-substituting solutions (polyglucin, reopoliglyukin). The effectiveness of the blood replacement operation in terms of the clearance of toxic substances is significantly inferior to other methods of active detoxification; upon completion, it requires monitoring and correction of the electrolyte and acid-base composition of the blood; it is most often used in pediatrics.
Symptomatic treatment of acute poisoning, including resuscitation, is the main one, especially at the prehospital stage; its volume is determined by the clinical manifestations of intoxication.
Most toxic substances cause oxygen deficiency in the body - hypoxia. In severe poisoning in patients in a deep coma, the respiratory and vasomotor centers of the medulla oblongata are inhibited, which leads to respiratory failure. At the same time, the rhythm of breathing is disturbed, it slows down until it stops. Cells of the central nervous system, primarily the cerebral cortex, are most sensitive to oxygen deficiency.
Most often, respiratory problems develop as a result of airway obstruction due to retraction of the tongue, spasm of the larynx, aspiration of vomit, increased bronchial secretions or severe salivation. Violation of airway patency is evidenced by frequent noisy breathing with the participation of auxiliary respiratory muscles, cough, cyanosis.
In these cases, first of all, it is necessary to remove mucus, vomit from the pharynx and oral cavity using an electric suction or “pear”, remove and strengthen the tongue with a tongue holder, insert an air tube or intubate the trachea. With severe bronchorrhea and salivation, s / c atropine is administered 1 ml of 0.1% (if necessary, repeatedly). All patients with respiratory disorders are shown inhalation of oxygen.
After restoration of airway patency, in case of respiratory disorders due to impaired innervation of the respiratory muscles with insufficiency or absence of independent respiratory movements, artificial ventilation of the lungs is performed, better - apparatus breathing with preliminary tracheal intubation. Artificial respiration is the best method of dealing with acute respiratory failure in case of poisoning. Laryngeal edema in case of poisoning with cauterizing poisons, it dictates the need for immediate lower tracheostomy.
Pulmonary edema, which occurs with burns of the upper respiratory tract with chlorine, ammonia, strong acids, phosgene and nitrogen oxide poisoning (having a selective pulmonotoxic effect), is stopped by intravenous administration of 30-60 mg of prednisolone or 100-150 mg of hydrocortisone per 20 ml of 40% glucose solution (if necessary - again), 100-150 ml of a 30% urea solution or 80-100 mg of furosemide (lasix); with unstable hemodynamics, vasopressors (dopamine, dobutamine, norepinephrine) are used. In addition, the secret is sucked from the upper respiratory tract, oxygen is inhaled with alcohol vapor (through a nasal catheter). The amount of fluid injected is limited.
To prevent the development of a late complication - pneumonia, which often occurs after burns of the upper respiratory tract with caustic chemicals or in patients in a coma, early antibiotic therapy is necessary. Antibiotics are administered intramuscularly (for example, penicillin at a dose of at least 12 million units per day), with an insufficient effect, the dose is increased.
With hemic hypoxia(as a result of hemolysis), methemoglobinemia, carboxyhemoglobinemia and tissue hypoxia (due to blockade of respiratory tissue enzymes, for example, in case of cyanide poisoning), oxygen therapy and specific antidote therapy are considered the main methods of treatment.
Selective cardiotoxic effect(in case of poisoning with cardiac glycosides, tricyclic antidepressants, potassium salts, nicotine, quinine, pachycarpine) is manifested by a decrease in cardiac output, which can be due to both the direct toxic effect of the poison on the myocardium and cardiac arrhythmias.
Vascular insufficiency develops due to the direct toxic effect of poisons on the vascular wall (in case of poisoning with nitrites, amidopyrine), as well as due to the inhibitory effect of the poison on the vasomotor center of the medulla oblongata (in case of poisoning with barbiturates, phenothiazines, benzodiazepine derivatives).
The most common and early occurring dysfunction of the cardiovascular system in acute poisoning is exotoxic shock, manifested by a drop in blood pressure, pallor of the skin, cold sweat, frequent weak pulse, shortness of breath; against the background of respiratory failure, metabolic acidosis occurs.
The volume of circulating blood and plasma decreases, the central venous pressure falls, the stroke and minute volume of the heart decreases (i.e., hypovolemia develops). Dehydration of the body with the subsequent development of shock is possible in case of poisoning with acids, alkalis, metal salts, mushrooms, etc. The patient is given a horizontal position with a raised foot end, heating pads are applied to the legs and arms.
Plasma substituting fluids are injected intravenously until the volume of circulating blood is restored and arterial and central venous pressure is normalized (sometimes up to 10-15 l / day). Usually, 400-1200 ml of polyglucin or gemodez are used, in their absence - isotonic sodium chloride solution and 10-15% glucose solution with insulin, hormone therapy is simultaneously carried out (prednisolone IV up to 500-800 mg per day). With the ineffectiveness of infusion therapy, vasopressors (dopamine, dobutamine, norepinephrine) are used.
Intracardiac conduction disorders and bradycardia are stopped in / in the introduction of 1-2 ml of a 0.1% solution of atropine, in the presence of contraindications to its use, it is possible to use sympathomimetics (alupent, novodrin). In case of violations of intraventricular conduction, the administration of hydrocortisone (250 mg intravenously), unithiol (10 ml of a 5% solution intramuscularly), alpha-tocopherol (300 mg intramuscularly) is also indicated.
Toxic Nephropathy develops in case of poisoning not only with purely nephrotoxic poisons (antifreeze-ethylene glycol, heavy metal salts - sublimate, dichloroethane, carbon tetrachloride, oxalic acid, etc.), but also with hemolytic poisons (acetic acid, copper sulfate), as well as with prolonged toxic shock, deep trophic disorders with myoglobinuria (the appearance of muscle protein in the urine) and the development of myorenal syndrome (necrosis of the skeletal muscles that develops with arterial hypotension and forced position, followed by the development of myoglobinuric nephrosis and acute renal failure).
Treatment of acute renal failure carried out under the control of the electrolyte composition, the content of urea and creatinine in the blood. The complex of therapeutic measures includes carrying out a pararenal novocaine blockade, intravenous drip of a glucosone-vocaine mixture (300 ml of a 10% glucose solution, 30 ml of a 2% novocaine solution) and alkalization of the blood.
Prevention of kidney damage in the early period of acute poisoning with nephrotoxic poisons allows the use of hemodialysis, the indications for which are hyperkalemia (over 5.5 mmol / l), high levels of urea in the blood (over 2 g / l or mol / l), significant fluid retention in body.
Toxic hepatopathy develops in acute poisoning with "liver", hepatotoxic poisons (chlorinated hydrocarbons - dichloroethane, carbon tetrachloride; phenols and aldehydes), plant forms (male fern, mushrooms) and some drugs (akrikhin).
Clinically acute liver failure, in addition to an increase and soreness of the liver, hysteria of the sclera and skin, it is accompanied by cerebral disorders (motor restlessness, alternating with drowsiness, apathy, delirium, coma), hemorrhagic diathesis (nosebleeds, hemorrhages in the conjunctiva, sclera, skin and mucous membranes).
The most effective ways to treat acute liver failure are extracorporeal detoxification methods. Bioantioxidants are used as emergency therapy - a 5% solution of unitiol up to 40 ml / day, alpha-tocopherol, selenium preparations, alpha-lipoic acid. As lyotropic preparations, B vitamins (2 ml of a 5% thiamine solution, 2 ml of a 2.5% nicotinamide solution, 100 μg of cyanocobalamin) and 200 mg of cocarboxylase are administered intramuscularly.
To restore glycogen stores, 20-40 ml of a 1% solution of glutamic acid, 4 ml of a 0.5% solution of lipoic acid are injected intravenously. Intravenous drip twice a day, 750 ml of a 5-10% glucose solution is administered with 8-16 IU / day of insulin. To stabilize the membranes of hepatocytes, Essentiale and Heptral are used.
Often liver damage is combined with kidney damage (hepatic-renal failure). In this case, plasmapheresis is performed (up to 1.5-2 liters of plasma are removed, making up for the loss with fresh frozen plasma and saline solutions in the same amount), hemodialysis or blood replacement.
Selective neurotoxic effect with impaired mental activity (including the development of psychosis), toxic coma, toxic hyperkinesis and paralysis is typical for poisoning with alcohol and its surrogates, benzene, isoniazid derivatives, amidopyrine, atropine, carbon monoxide, organophosphorus compounds, psychotropic drugs (antidepressants, narcotic analgesics, tranquilizers, including barbiturates).
Emerging intoxication psychoses usually stopped by psychotropic drugs of a wide spectrum of action (chlorpromazine, haloperidol, viadryl, sodium hydroxybutyrate), regardless of the type of poisoning, while toxic coma requires strictly differentiated measures.
With toxic cerebral edema repeated spinal punctures are performed with the removal of 10-15 ml of cerebrospinal fluid, depending on the cerebrospinal fluid pressure. Osmotic diuretics are administered intravenously, without prior fluid loading. The use of mannitol is preferable to urea due to the lesser severity of the recoil phenomenon (repeated increase in intracranial pressure).
Glycerol is injected into the stomach through a probe or it is administered intravenously in the form of a 30% solution at the rate of 1 g/kg of body weight in a 20% solution of sodium ascorbate. Arising metabolic disorders are stopped by the introduction of a 10-20% glucose solution with insulin, potassium preparations, ATP, cocarboxylase and vitamins.
In case of development of a convulsive syndrome in case of poisoning with strychnine, amidopyrine, tubazide, organophosphorus insecticides, etc. or due to brain hypoxia (after restoration of airway patency), 4-5 ml of a 0.5% solution of diazepam (seduxen, relanium) is injected intravenously. The introduction of diazepam is repeated at the same dose (but not more than 20 ml in total) every 20-30 seconds until the seizures stop. In extremely severe cases, tracheal intubation, ether-oxygen anesthesia and the introduction of muscle relaxants are indicated.
Hyperthermia in acute poisoning often accompanies convulsive conditions and toxic cerebral edema. The differential diagnosis is carried out with febrile conditions (for example, with pneumonia). Showing craniocerebral hypothermia (cooling the head - ice and with the help of special devices), intramuscular injection of a lyric mixture (1 ml of a 2.5% solution of chlorpromazine, 2 ml of a 2.5% solution of diprazine and 10 ml of a 4% - amidopyrine solution); if necessary, repeat spinal punctures are performed.
Pain syndrome in case of poisoning with caustic acids and alkalis stop in / in the introduction of 500 ml of a 5% glucose solution with 50 ml of a 2% solution of novocaine, narcotic analgesics or using neuroleptanalgesia.
Use antidotes (antidotes) recommended as early as possible, since they directly affect the action and metabolism of the toxic substance that has entered the body, its deposition or excretion, and thereby weaken the effect of the poison. There are 4 groups of specific antidotes: chemical (toxicotropic), biochemical (toxic-kinetic), pharmacological (symptomatic), antitoxic immunopreparations.
Chemical antidotes are given orally (for example, a metal antidote) or administered parenterally (thiol compounds that form non-toxic compounds when combined - unithiol, mecaptide; chelating agents - EDTA salts, tetanine). The action of toxicotropic antidotes administered orally is based on the "binding" reaction of toxic substances in the gastrointestinal tract; parenteral antidotes neutralize poisons in the humoral environment of the body.
To precipitate poison in the gastrointestinal tract in case of poisoning with heavy metal salts, sorbents are used: egg white, activated charcoal, etc. The use of unitiol contributes to the formation of soluble compounds and their acceleration with the help of forced diuresis.
Biochemical antidotes alter the metabolism of toxic substances or biochemical reactions. In case of poisoning with organophosphorus compounds, cholinesterase reactivators - oximes (dipiroxime, diethixime and alloxime) are used, in case of poisoning with methemoglobin-forming poisons - methylene blue (chromosmon). The use of antimetabolites makes it possible to delay the formation of toxic metabolites of these poisons in the liver. For example, the appointment of ethyl alcohol in case of poisoning with ethylene glycol and methyl alcohol inhibits the accumulation of formaldehyde, formic or oxalic acid.
The action of pharmacological antidotes is based on pharmacological antagonism between substances (for example, atropine-acetylcholine, prozerin-pachycarpine, physostigmine-atropine, naloxone-opiates, flumazenil-benzodiazepines). Antitoxic immunopreparations (anti-snake immune sera, etc.) are used in medical institutions, taking into account the special conditions for their storage and a short shelf life. These drugs are generally ineffective when used late and may cause anaphylactic shock.
- Target: formation of knowledge of the general patterns of pharmacokinetics and pharmacodynamics of drugs used in acute drug poisoning to ensure the choice of drugs for appropriate pathological conditions in dental practice.
- Learning objectives:
Cognitive competencies
1. To form knowledge on modern principles of detoxification therapy for acute drug poisoning.
2. To form knowledge on the classification, general characteristics, mechanisms of action and the main pharmacological and side effects of drugs used in acute drug poisoning.
3. To form knowledge on the choice of antidotes and antagonists of various drugs for acute poisoning.
4. To form knowledge of choosing a combination of drugs in acute drug poisoning for detoxification activities.
5. To study the routes of administration, the principles of the dosing regimen for drugs used in acute drug poisoning, depending on the individual characteristics and properties of the drug, including in dentistry
Operational Competence
1. To form the skills of prescribing medicines in prescriptions with analysis.
2. To form the ability to calculate single doses of drugs
Communicative competence:
1. Possession of competent and developed speech.
2. Ability to prevent and resolve conflict situations.
3. The use of questions of motivation, stimulation to influence the relationship between members of the team.
4. Statement of an independent point of view.
5. Logical thinking, possession of a free discussion on the problems of pharmacology.
Self-development (lifelong learning and education):
1. Independent search for information, its processing and analysis using modern research methods, computer technologies.
2. Performing various forms of SIW (writing essays, test tasks, presentations, abstracts, etc.)
4. Main questions of the topic:
1. Classification of poisoning depending on the conditions of occurrence, the rate of development.
2. Principles of detoxification therapy for acute drug poisoning.
3. Features of pharmacokinetics, pharmacodynamics of various toxic substances and antidotes.
4. Delayed absorption of a toxic substance into the blood in case of poisoning with gaseous substances, when poison gets on the skin, mucous membranes, and in the gastrointestinal tract.
5. Removal of a toxic substance from the body. The concept of hemodialysis, hemosorption, forced diuresis, peritoneal dialysis, plasmapheresis, lymphodilysis, lymphosorption.
6. Neutralization of the poison during its resorptive action (antidotes, functional antagonists).
7. Symptomatic and pathogenetic therapy for various rav poisonings (stimulants of vital functions, drugs for normalizing acid-base balance, blood substitutes).
8. Long-term effects of exposure to poisonous substances.
5. Teaching methods: consultations of the teacher on issues of the topic, solving test tasks, situational tasks and assignments for guidance with conclusions, prescribing receptors with analysis and calculation of doses, discussions, work in small groups, work with illustrative material.
Literature:
Main:
1. Kharkevich D.A. Pharmacology: Textbook. - 10th ed., revised, additional. and correct. –M.: GEOTAR-Media, 2008 - С 327-331, 418-435, 396-406.
2. Kharkevich D.A. Pharmacology: Textbook. - 8th ed., revised, add. and correct. -M.: GEOTAR-Media, 2005 - C 320-327, 399-415, 377-387.
3. Guide to laboratory studies /Ed. YES. Kharkevich, Medicine, 2005.– 212-216, 276-287, 231-238 p.
Additional:
1. Mashkovsky M.D. Medicines. Fifteenth edition. - M.: New wave, 2007. vol. 1-2. - 1206 p.
2. Alyautdin R.N. Pharmacology. Textbook. Moscow. Ed. House "GEOTAR-MED". 2004.-591 p.
3. Goodman G., Gilman G. Clinical pharmacology. Translation of the 10th edition. M. "Practice". 2006. - 1648 p.
4. Lectures on pharmacology for doctors and pharmacists / Vengerovsky A.I. - 3rd edition, revised and supplemented: textbook - M.: IF "Physical and Mathematical Literature", 2006. - 704 p.
5. Clinical pharmacology. / Ed. V.G. Kukes. - GEOTAR.: Medicine, 2004. - 517 p.
6. Directory of a general practitioner. Edition Moscow EKSMO - PRESS, 2002. v. 1-2. – 926 p.
7. Lawrence D.R., Benett P.N. Clinical pharmacology. - M .: Medicine, 2002, vol. 1-2. – 669 p.
8. L.V. Derimedved, I.M. Pertsev, E.V. Shuvanova, I.A. Zupanets, V.N. Khomenko "Interaction of drugs and the effectiveness of pharmacotherapy" - Publishing house "Megapolis" Kharkov 2002.-p.782
9. Bertram G. Katzung. Basic and clinical pharmacology (translated by Doctor of Medical Sciences, Prof. E.E. Zvartau.) - St. Petersburg, 1998.- 1043 p.
10. Belousov Yu.B., Moiseev V.S., Lepakhin V.K. Clinical pharmacology and pharmacotherapy. - M: Universum Publishing, 1997. - 529 p.
Drugs according to the program: unithiol, sodium thiosulfate, calcium thetacin, methylene blue
apomorphine hydrochloride, magnesium sulfate, furosemide, mannitol, urea, inducers and inhibitors of microsomal enzymes (phenobarbital, levomycetin, cimetidine), atropine sulfate, physostigmine salicylate, prozerin, naloxone, naltrexone, activated charcoal, dipyroxime, isonitrosine, pyridoxine hydrochloride, chromosmon, bemegride .
Prescription drugs: furosemide (in amp.), atropine sulfate (in amp.), activated charcoal, unithiol.
Tests for self-control.
Test No. 1 (1 answer)
Used to remove toxic substances from the body
1. "loop" diuretics
2.analeptics
3.antidotes
4. sleeping pills
5.glycosides
Test No. 2 (1 answer)
Pharmacological antagonist in case of poisoning with narcotic analgesics
1. naloxone
2.atropine
3.platifillin
4.unithiol
5. bemegrid
Test No. 3 (1 answer)
In order to delay the absorption of a toxic substance,
1.adsorbents
2. antihypertensive drugs
3.diuretics
4.glycosides
5.analeptics
Test No. 4 (1 answer)
Competitive antagonist of antidepolarizing muscle relaxants
1. atropine sulfate
2. pilocarpine
3. acetylcholine
4. aceclidine
5. pirenzepine
Test No. 5 (1 answer)
Dipyroxime - an antidote for poisoning
1. organophosphorus compounds
2. salts of heavy metals
3. ethyl alcohol
4. benzodiazepine derivatives
5. narcotic analgesics
Test No. 6 (1 answer)
In case of poisoning with M-cholinergic blockers,
1. prozerin
2. unitiol
3. methylene blue
4. digoxin
5. aceclidine
Test No. 7 (1 answer)
1. Donor of sulfhydryl groups
2. Laxative
3. Cholinesterase reactivator
4. Adsorbent
5. Opioid receptor antagonist
Test No. 8 (3 answers)
Measures aimed at removing a toxic substance from the body
1. Introduction of antidotes
2. Hemodialysis
3. Forced diuresis
4. gastric lavage
5. hemosorption
Test No. 9 (2 answers)
Used for forced diuresis
1. furosemide
2. hydrochlorothiazide
3. indapamide
5. triamterene
Test No. 10 (2 answers)
In case of an overdose of cardiac glycosides,
1. naloxone
2. dipyroxime
3. unitiol
4. potassium chloride
5. methylene blue
Answers to test tasks for self-control
| Test #1 | |
| Test #2 | |
| Test #3 | |
| Test #4 | |
| Test #5 | |
| Test #6 | |
| Test #7 | |
| Test #8 | 2,3,5 |
| Test #9 | 1,4 |
| Test #10 | 3,4 |
Lesson number 29.
1. Theme: « Drugs affecting the oral mucosa and dental pulp».
2. Purpose: formation of knowledge of the general patterns of pharmacokinetics and pharmacodynamics of drugs that affect the oral mucosa and dental pulp to ensure the choice of drugs for appropriate pathological conditions in dental practice, the ability to write prescriptions.
3. Learning objectives:
1. Familiarize yourself with the classification of drugs that affect the oral mucosa and dental pulp
2. To study the general patterns of pharmacokinetics and pharmacodynamics of drugs that affect the oral mucosa and dental pulp.
3. To study the main indications for the use of agents that affect the oral mucosa and dental pulp
4. Learn to prescribe in prescriptions the main drugs that affect the oral mucosa and dental pulp, calculate single and daily doses.
5. To study the routes of administration, the principles of the dosing regimen of drugs that affect the oral mucosa and dental pulp, depending on the individual characteristics and properties of the drug, including in dentistry
6. To study the possibility of a combination of agents that affect the oral mucosa and dental pulp
7. Study the side effects and their prevention.
4. Main questions of the topic:
1. Anti-inflammatory drugs:
local action: astringents (organic and inorganic),
enveloping agents, enzyme preparations,
Preparations of glucocorticosteroids for local use.
resorptive action: steroid and non-steroidal anti-inflammatory
· facilities; calcium salts.
2. Antiallergic drugs:
antihistamines.
glucocorticosteroids.
3. Means for the treatment of infectious and fungal diseases of the mucosa
membranes of the oral cavity:
Antiseptics (compound of chlorine, iodine, oxidizing agents and dyes;
derivatives of nitrofuran;
topical antibiotics;
Antibiotics for resorptive action;
sulfa drugs;
antifungal agents (nystatin, levorin, dekamin).
4. Means used to relieve pain in case of inflammation of the mucous membrane
oral cavity, pulpitis:
5. local anesthetics;
6. non-narcotic analgesics.
5. Means that promote the rejection of necrotic tissues:
Enzyme preparations
proteases - trypsin, chymotrypsin.
nucleases - ribonuclease, deoxyribonuclease.
The principle of their action, application.
6. Means that improve the regeneration of oral tissues and remineralization of tooth tissues:
Vitamin preparations, preparations of calcium, phosphorus, fluorine.
Leukopoiesis stimulants - pentoxyl, sodium nucleinate.
biogenic stimulants: preparations from plants - aloe extract, preparations from animal tissues - the vitreous body, firth mud - FIBS, bee glue - propolis, prosol.
anabolic steroids.
13. Dehydration and cauterizing agents - ethyl alcohol
14. Means for pulp necrosis: arsenic acid, paraformaldehyde.
15. Deodorants: hydrogen peroxide, potassium permanganate, boric acid.
Sodium borate, sodium bicarbonate.
5. Methods of learning and teaching: oral survey on the main issues of the topic, solution of test tasks and situational problems, work in small groups, analysis of tables, figures, diagrams, summing up, writing prescriptions with analysis, calculation of single doses.
Literature
Main:
1. Kharkevich D.A. Pharmacology. Eighth edition - M .: Medicine GEOTAR, 2008. -. pp. 529-558.
2. Kharkevich D.A. Pharmacology. Eighth edition - M .: Medicine GEOTAR, 2005. - S. 241-247.
3. Guide to laboratory studies / Ed. D.A. Kharkevich. Medicine, S. 2005. S. 129-136, 331-334.
Additional:
1. Mashkovsky M.D. Medicines. Fifteenth edition - M.: Medicine, 2007.– 1200 p.
2. Lectures on pharmacology for doctors and pharmacists / Vengerovsky A.I. - 3rd edition, revised and supplemented: textbook - M .: IF "Physical and Mathematical Literature", 2006. - 704 p.
3. V.R. Weber, B.T. Freezing. Clinical pharmacology for dentists.-S-P.:2003.-p.351
4. Clinical pharmacology./Ed. V.G. Kukes. - GEOTAR.: Medicine, 2004. - 517 p.
5. Derimedved L.V., Pertsev I.M., Shuvanova E.V., Zupanets I.A., Khomenko V.N. "Interaction of drugs and the effectiveness of pharmacotherapy" - Publishing house "Megapolis" Kharkov 2002.- 782 p.
6. Lawrence D.R., Benitt P.N. – Clinical pharmacology. - M.: Medicine, 2002, v.1-2.- 669. p.
7. Oxford Handbook of Clinical Pharmacology and Pharmacotherapy. - M.: Medicine, 2000-740 p.
8. Krylov Yu.F., Bobyrev V.M. Pharmacology: Textbook for students of the Faculty of Dentistry. –M., 1999
9. Basic and clinical pharmacology. / Ed. Bertram G. Katzung. - M .: S-P .: Nevsky dialect, 1998.-t. 1 - 669. p.
10. Komendantova M.V., Zoryan E.V. Pharmacology. Textbook.-M.: 1988. p-206.
Drugs according to the program: ascorbic acid, ergocalciferol, vikasol, thrombin, acetylsalicylic acid, pentoxyl, sodium nucleinate, anabolic steroids, phosphorus, fluorine preparations, prednisolone
Prescription drugs: ascorbic acid, ergocalciferol, vikasol, thrombin, acetylsalicylic acid
Control
1. Oral survey on the main issues of the topic.
2. Writing prescriptions with analysis of fixed assets. In the analysis, indicate the group affiliation, the main pharmacological effects, indications for use, side effects.
3. Performing tasks in a test form.
Test questions
Test #1
Mechanism of action of diclofenac sodium:
1. Blocking COX-1
2. Blocking COX-2
3. Blocking COX-1 and COX-2
4. Blocking of phosphodiesterase, COX-1
5. Blocking of phosphodiesterase, COX-2
Test #2
Diphenhydramine has all of the following effects EXCEPT:
1. Anti-inflammatory
2. Antipyretic
3. Antihistamine
4. Sleeping pills
5. Antiemetic
Test #3
Withdrawal syndrome is possible with a sharp discontinuation of the reception:
1. Acetylsalicylic acid
2. Cromolyn sodium
3. Prednisolone
5. Ibuprofen
Test #4
For an immediate allergic reaction, use:
1. Adrenaline hydrochloride
2. Prednisolone
4. Ibuprofen
5. Diclofenac sodium
Test #5
The most effective and safe non-steroidal anti-inflammatory agent used for arthritis of the maxillary joint:
1. Indomethacin
2. Diclofenac sodium
3. Diphenhydramine
4. Acetylsalicylic acid
5. Prednisolone
Test #6
A drug that stimulates the synthesis of prothrombin in the liver:
1. Heparin
2. Acetylsalicylic acid
3. Neodicumarin
4. Vikasol
5. Aminocaproic acid
Test #7
For allergic reactions of immediate and delayed types, apply:
1. Glucocorticoids
2. H1 blockers of histamine receptors
3. COX1 and COX2 blockers
4. Beta-blockers
5. COX-1 blockers
Test #8
Pharmacological effects of non-steroidal anti-inflammatory drugs:
1. Antipyretic, antihistamine
2. Antihistamine, anti-inflammatory
3. Anti-inflammatory, pain relief
4. Pain reliever, antihistamine
5. Immunosuppressive, anti-inflammatory
Test #9
The main side effect of acetylsalicylic acid:
1. Ulcerogenic action
2. Hypotensive
3. Antiarrhythmic
4.Sedative
5.Immunosuppressive
Test #10
Mechanism of action of cromolyn sodium:
1. Blocks histamine receptors
2. Blocks serotonin receptors
3. Stabilizes mast cell membranes
4. Stabilizes lysosomal membranes
5. Stabilizes leukocyte membranes