When measuring the pelvis, the woman lies on her back with her stomach exposed, her legs extended and pushed together. The doctor stands to the right of the pregnant woman, facing her. The branches of the tazomer are picked up in such a way that the large and index fingers held buttons. points, the distance between which is measured by pressing buttons on them to push apart the branches of the pelvis gauge, and the value of the desired size is marked on the scale.
When measuring the pelvis, the woman lies on her back with her stomach exposed, her legs extended and pushed together. The doctor stands to the right of the pregnant woman, facing her. The branches of the tazomer are picked up in such a way that the large and index fingers held buttons. points, the distance between which is measured by pressing buttons on them to push apart the branches of the pelvis gauge, and the value of the desired size is marked on the scale.
 3. Conjugata, diameter conjugata is the distance between the promontory and the posterior surface of the pubic symphysis. 4. Distantia spinarum is the distance between the superior anterior iliac spines. (normally 25-26 cm) 5. Distantia trochanterica is the distance between the greater trochanters of the femurs. (normally 30-31 cm) 6. Distantia cristarum is the distance between the most distant points of the iliac crest. (normally 28-29 cm)
3. Conjugata, diameter conjugata is the distance between the promontory and the posterior surface of the pubic symphysis. 4. Distantia spinarum is the distance between the superior anterior iliac spines. (normally 25-26 cm) 5. Distantia trochanterica is the distance between the greater trochanters of the femurs. (normally 30-31 cm) 6. Distantia cristarum is the distance between the most distant points of the iliac crest. (normally 28-29 cm)
 Transverse diameter, diameter transversa, is the distance between the most distant points of both boundary lines. 2. Oblique diameter, diameter obliqua (dextra et sinistra) is measured from the right (left) sacroiliac joint to the left (right) iliopubic eminence.
Transverse diameter, diameter transversa, is the distance between the most distant points of both boundary lines. 2. Oblique diameter, diameter obliqua (dextra et sinistra) is measured from the right (left) sacroiliac joint to the left (right) iliopubic eminence.
 Diagonal conjugate measurement The diagonal conjugate (conjugata diagonalis) is the distance from the lower edge of the symphysis to the most prominent point of the sacral promontory. The diagonal conjugate is determined during a vaginal examination of a woman, which is performed in compliance with all the rules of asepsis and antiseptics. The II and III fingers are inserted into the vagina, the IV and V are bent, their back rests against the perineum
Diagonal conjugate measurement The diagonal conjugate (conjugata diagonalis) is the distance from the lower edge of the symphysis to the most prominent point of the sacral promontory. The diagonal conjugate is determined during a vaginal examination of a woman, which is performed in compliance with all the rules of asepsis and antiseptics. The II and III fingers are inserted into the vagina, the IV and V are bent, their back rests against the perineum
 Diagonal conjugate at normal pelvis equals on average 12.5-13 cm. To determine the true conjugate, 1.5-2 cm is subtracted from the size of the diagonal conjugate. It is not always possible to measure the diagonal conjugate, because with normal pelvic sizes the promontory is not reached or is difficult to palpate. If the cape cannot be reached with the end of an extended finger, the volume of this pelvis can be considered normal or close to normal.
Diagonal conjugate at normal pelvis equals on average 12.5-13 cm. To determine the true conjugate, 1.5-2 cm is subtracted from the size of the diagonal conjugate. It is not always possible to measure the diagonal conjugate, because with normal pelvic sizes the promontory is not reached or is difficult to palpate. If the cape cannot be reached with the end of an extended finger, the volume of this pelvis can be considered normal or close to normal.
 When determining the size of the pelvis, it is necessary to take into account the thickness of its bones; it is judged by the value of the so-called Solovyov index, the circumference of the wrist joint. The average index value is 14 cm. If the Solovyov index is more than 14 cm, it can be assumed that the pelvic bones are massive and the size of the small pelvis is smaller than expected.
When determining the size of the pelvis, it is necessary to take into account the thickness of its bones; it is judged by the value of the so-called Solovyov index, the circumference of the wrist joint. The average index value is 14 cm. If the Solovyov index is more than 14 cm, it can be assumed that the pelvic bones are massive and the size of the small pelvis is smaller than expected.


 a - head above the entrance to the pelvis; b - the head is a small segment at the entrance to the pelvis; c - the head is a large segment at the entrance to the pelvis; d - head in the wide part of the cavity of the small maz; d - head in the narrow part of the pelvic cavity; e - head at the pelvic outlet; I - plane of the entrance to the small pelvis, II - plane of the wide part of the pelvic cavity, III - plane of the exit of the small pelvis.
a - head above the entrance to the pelvis; b - the head is a small segment at the entrance to the pelvis; c - the head is a large segment at the entrance to the pelvis; d - head in the wide part of the cavity of the small maz; d - head in the narrow part of the pelvic cavity; e - head at the pelvic outlet; I - plane of the entrance to the small pelvis, II - plane of the wide part of the pelvic cavity, III - plane of the exit of the small pelvis.

 Normally, the vertical size of the rhombus is on average 11 cm, the transverse size is 10 cm. If the structure of the small pelvis is disturbed, the lumbosacral rhombus is not clearly expressed, its shape and size are changed. However, spinal diseases can lead to incorrect assessments of the pelvis
Normally, the vertical size of the rhombus is on average 11 cm, the transverse size is 10 cm. If the structure of the small pelvis is disturbed, the lumbosacral rhombus is not clearly expressed, its shape and size are changed. However, spinal diseases can lead to incorrect assessments of the pelvis
 The fetal skull consists of two frontal, two parietal, two temporal, one occipital, sphenoid and ethmoid bones. The following sutures are of greatest importance in obstetric practice: the sagittal (sagittal) suture connects the right and left parietal bones; in front the suture passes into the anterior (large) fontanel, in the back into the small (posterior); the frontal suture is located between the frontal bones (in a newborn, the frontal bones have not yet fused together); The coronal suture connects the frontal bones with the parietal bones and is located perpendicular to the sagittal and frontal sutures. The coronal suture connects the frontal bones with the parietal bones and runs perpendicular to the sagittal and frontal sutures; The lambdoid (occipital) suture connects the occipital bone to the parietal bone.
The fetal skull consists of two frontal, two parietal, two temporal, one occipital, sphenoid and ethmoid bones. The following sutures are of greatest importance in obstetric practice: the sagittal (sagittal) suture connects the right and left parietal bones; in front the suture passes into the anterior (large) fontanel, in the back into the small (posterior); the frontal suture is located between the frontal bones (in a newborn, the frontal bones have not yet fused together); The coronal suture connects the frontal bones with the parietal bones and is located perpendicular to the sagittal and frontal sutures. The coronal suture connects the frontal bones with the parietal bones and runs perpendicular to the sagittal and frontal sutures; The lambdoid (occipital) suture connects the occipital bone to the parietal bone.
 The fetus as an object of birth At the junction of the sutures there are fontanelles. The anterior and posterior fontanelles are of practical importance. The anterior (large) fontanel is located at the junction of the sagittal, frontal and coronal sutures. It has a diamond shape and four sutures extend from it: anteriorly - frontal, posteriorly - sagittal, to the right and left - coronal sutures. The posterior (small) fontanelle is a small depression in which the sagittal and lambdoid sutures converge. He has triangular shape. Three sutures extend from the posterior fontanel: anteriorly - sagittal, to the right and left - the corresponding sections of the lambdoid suture. For practical obstetrics, it is also important to know the tubercles that are located on the head: occipital, two parietal and two frontal. Knowledge of the topographic and anatomical features of the fetal bony head is very important for practical obstetrics, since the doctor is guided by these identification points when performing a vaginal examination during childbirth. No less important than sutures and fontanelles are the dimensions of the head of a mature and full-term fetus - each moment of the labor mechanism corresponds to a certain size of the fetal head at which it passes through the birth canal
The fetus as an object of birth At the junction of the sutures there are fontanelles. The anterior and posterior fontanelles are of practical importance. The anterior (large) fontanel is located at the junction of the sagittal, frontal and coronal sutures. It has a diamond shape and four sutures extend from it: anteriorly - frontal, posteriorly - sagittal, to the right and left - coronal sutures. The posterior (small) fontanelle is a small depression in which the sagittal and lambdoid sutures converge. He has triangular shape. Three sutures extend from the posterior fontanel: anteriorly - sagittal, to the right and left - the corresponding sections of the lambdoid suture. For practical obstetrics, it is also important to know the tubercles that are located on the head: occipital, two parietal and two frontal. Knowledge of the topographic and anatomical features of the fetal bony head is very important for practical obstetrics, since the doctor is guided by these identification points when performing a vaginal examination during childbirth. No less important than sutures and fontanelles are the dimensions of the head of a mature and full-term fetus - each moment of the labor mechanism corresponds to a certain size of the fetal head at which it passes through the birth canal

 On the fetal head two parts can be distinguished: a relatively small facial one: lower jaw (1), upper jaw(2) and very voluminous – brain. The latter consists of seven bones: two frontal (3), two parietal (4), one occipital (5), two temporal (6). Small transverse size (diameter bitemporalis) - the distance between the most distant points of the coronal suture, length - 8 cm. 8. Large transverse size (diameter biparietalis) - distance between the parietal tubercles, length - 9.5 cm
On the fetal head two parts can be distinguished: a relatively small facial one: lower jaw (1), upper jaw(2) and very voluminous – brain. The latter consists of seven bones: two frontal (3), two parietal (4), one occipital (5), two temporal (6). Small transverse size (diameter bitemporalis) - the distance between the most distant points of the coronal suture, length - 8 cm. 8. Large transverse size (diameter biparietalis) - distance between the parietal tubercles, length - 9.5 cm
 The following dimensions are distinguished on the fetal body: 1. The transverse size of the shoulders (distantia biacromialis) is 12 cm long and in circumference: for breech, leg and knee presentations - 34 cm (Fig. 18), for incomplete breech presentation - 39-41 cm 2. Transverse the size of the buttocks (distantia bisiliacalis) is 9.5 cm long and in circumference: with an incomplete breech presentation - 32 cm (see Fig. 19), with a full leg presentation - 28 cm (Fig. 20), with a complete breech presentation - 34 cm
The following dimensions are distinguished on the fetal body: 1. The transverse size of the shoulders (distantia biacromialis) is 12 cm long and in circumference: for breech, leg and knee presentations - 34 cm (Fig. 18), for incomplete breech presentation - 39-41 cm 2. Transverse the size of the buttocks (distantia bisiliacalis) is 9.5 cm long and in circumference: with an incomplete breech presentation - 32 cm (see Fig. 19), with a full leg presentation - 28 cm (Fig. 20), with a complete breech presentation - 34 cm
 The fetus as an object of labor Determination of the position of the fetal head relative to the interspinal line: – 3 – head above the entrance to the pelvis; – 2 – the head is pressed against the entrance to the pelvis; – 1 – head as a small segment in the plane of the entrance to the pelvis; 0 – head with a large segment in the plane of the entrance to the pelvis; +1 – the head is a large segment in the wide part of the small pelvis; +2 – head in the narrow part of the pelvis; +3 – head on the pelvic floor; +4 – the head cuts in and erupts.
The fetus as an object of labor Determination of the position of the fetal head relative to the interspinal line: – 3 – head above the entrance to the pelvis; – 2 – the head is pressed against the entrance to the pelvis; – 1 – head as a small segment in the plane of the entrance to the pelvis; 0 – head with a large segment in the plane of the entrance to the pelvis; +1 – the head is a large segment in the wide part of the small pelvis; +2 – head in the narrow part of the pelvis; +3 – head on the pelvic floor; +4 – the head cuts in and erupts.


 Special methods of obstetric examination. At the initial visit of a pregnant woman in the first and second trimesters of pregnancy, an examination of the external genitalia, examination of the vagina and cervix using vaginal speculum, vaginal (internal) and bimanual (externally internal) examinations are carried out (see Gynecological examination). First, examine the external genitalia, the perineum (its height is the distance from the posterior commissure to anus- normally 4-5 cm), anus area. Using vaginal speculum, examine the vagina and cervix. During a two-handed examination, the length and width of the vagina, the condition of its walls, the severity of the vault, the shape, size, and consistency of the cervix and the condition of its external os are determined. Then the position, shape, size, consistency, mobility of the uterus, condition fallopian tubes, ovaries, parametrial tissue, inner surface of the pelvic bones.
Special methods of obstetric examination. At the initial visit of a pregnant woman in the first and second trimesters of pregnancy, an examination of the external genitalia, examination of the vagina and cervix using vaginal speculum, vaginal (internal) and bimanual (externally internal) examinations are carried out (see Gynecological examination). First, examine the external genitalia, the perineum (its height is the distance from the posterior commissure to anus- normally 4-5 cm), anus area. Using vaginal speculum, examine the vagina and cervix. During a two-handed examination, the length and width of the vagina, the condition of its walls, the severity of the vault, the shape, size, and consistency of the cervix and the condition of its external os are determined. Then the position, shape, size, consistency, mobility of the uterus, condition fallopian tubes, ovaries, parametrial tissue, inner surface of the pelvic bones.
 Schematic representation of external obstetric examination techniques (Leopold's techniques): first appointment (determining the level of the uterine fundus, the shape of the uterus and the part of the fetus located in the area of the uterine fundus
Schematic representation of external obstetric examination techniques (Leopold's techniques): first appointment (determining the level of the uterine fundus, the shape of the uterus and the part of the fetus located in the area of the uterine fundus
 Schematic representation of external obstetric examination techniques (Leopold's techniques): second technique (determining the position, position and type of fetal position).
Schematic representation of external obstetric examination techniques (Leopold's techniques): second technique (determining the position, position and type of fetal position).

 Schematic representation of external obstetric examination techniques (Leopold's techniques): fourth technique (determination of the presenting part, its insertion and advancement).
Schematic representation of external obstetric examination techniques (Leopold's techniques): fourth technique (determination of the presenting part, its insertion and advancement).
 Places where heart sounds can be heard most clearly various positions fetus: 1 - anterior view, first position, cephalic presentation; 2 - posterior view, first position, cephalic presentation; 3 - anterior view, second position, cephalic presentation; 4 - posterior view, second position, cephalic presentation;
Places where heart sounds can be heard most clearly various positions fetus: 1 - anterior view, first position, cephalic presentation; 2 - posterior view, first position, cephalic presentation; 3 - anterior view, second position, cephalic presentation; 4 - posterior view, second position, cephalic presentation;
 Places of the clearest listening to heart sounds in different positions of the fetus 5 - anterior view, first position, breech presentation; 6 - posterior view, first position, breech presentation, 7 - anterior view, second position, breech presentation; 8 - posterior view, second position, breech presentation.
Places of the clearest listening to heart sounds in different positions of the fetus 5 - anterior view, first position, breech presentation; 6 - posterior view, first position, breech presentation, 7 - anterior view, second position, breech presentation; 8 - posterior view, second position, breech presentation.
 A significant part of prenatal invasive studies is cytogenetic diagnosis of chromosomal diseases. In these cases, the indications for its implementation are: the mother’s age is 35 years and older; the birth of a child in a family with chromosomal pathology; carriage of a familial chromosomal abnormality; suspicion of the presence of congenital malformations in the fetus; In the first trimester of pregnancy, transcervical or transabdominal chorionic villus aspiration is most often performed. In the second trimester, amniocentesis, transabdominal aspiration of placental villi and transabdominal cordocentesis (puncture of umbilical cord vessels) are performed
A significant part of prenatal invasive studies is cytogenetic diagnosis of chromosomal diseases. In these cases, the indications for its implementation are: the mother’s age is 35 years and older; the birth of a child in a family with chromosomal pathology; carriage of a familial chromosomal abnormality; suspicion of the presence of congenital malformations in the fetus; In the first trimester of pregnancy, transcervical or transabdominal chorionic villus aspiration is most often performed. In the second trimester, amniocentesis, transabdominal aspiration of placental villi and transabdominal cordocentesis (puncture of umbilical cord vessels) are performed
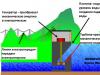
 Indications for this diagnostic procedure most often include the need for cytogenetic diagnosis of chromosomal diseases. In more rare cases, amniocentesis is performed in case of fetal hypoxia, isoserological incompatibility of the blood of mother and fetus, to assess the degree of fetal maturity (by the ratio of the concentration of lecithin and sphingomyelin or by the number of anucleate lipid-containing “orange” cells), the need microbiological research amniotic fluid. Contraindications: threat of miscarriage and infection of the genital tract. The procedure is performed under ultrasound guidance, choosing access depending on the location of the placenta and fetus. In this case, both transabdominal (Fig. 4. 42) and transcervical amniocentesis are performed.
Indications for this diagnostic procedure most often include the need for cytogenetic diagnosis of chromosomal diseases. In more rare cases, amniocentesis is performed in case of fetal hypoxia, isoserological incompatibility of the blood of mother and fetus, to assess the degree of fetal maturity (by the ratio of the concentration of lecithin and sphingomyelin or by the number of anucleate lipid-containing “orange” cells), the need microbiological research amniotic fluid. Contraindications: threat of miscarriage and infection of the genital tract. The procedure is performed under ultrasound guidance, choosing access depending on the location of the placenta and fetus. In this case, both transabdominal (Fig. 4. 42) and transcervical amniocentesis are performed.
When measuring the pelvis, the woman lies on her back with her stomach exposed, her legs extended and pushed together. The doctor stands to the right of the pregnant woman, facing her. The branches of the tazomer are picked up in such a way that the thumbs and forefingers hold the buttons. points, the distance between which is measured by pressing buttons on them to push apart the branches of the pelvis gauge, and the value of the desired size is marked on the scale.
3. Conjugata, diameter conjugata - the distance between the promontory and the posterior surface of the pubic symphysis. 4. Distantia spinarum - the distance between the upper anterior iliac spines. (normally cm) 5. Distantia trochanterica - the distance between the greater trochanters of the femurs. (normally cm) 6. Distantia cristarum - the distance between the most distant points of the iliac crest. (normal cm)

Transverse diameter, diameter transversa - the distance between the most distant points of both boundary lines. 2. Oblique diameter, diameter obliqua (dextra et sinistra) - measured from the right (left) sacroiliac joint to the left (right) iliopubic eminence.

Diagonal conjugate measurement The diagonal conjugate (conjugata diagonalis) is the distance from the lower edge of the symphysis to the most prominent point of the sacral promontory. The diagonal conjugate is determined during a vaginal examination of a woman, which is performed in compliance with all the rules of asepsis and antiseptics. The II and III fingers are inserted into the vagina, the IV and V are bent, their back rests against the perineum

The diagonal conjugate with a normal pelvis is on average 12.513 cm. To determine the true conjugate, 1.52 cm is subtracted from the size of the diagonal conjugate. It is not always possible to measure the diagonal conjugate, because with normal pelvic sizes the promontory is not reached or is difficult to palpate. If the promontory cannot be reached with the end of an extended finger, the volume of this pelvis can be considered normal or close to normal.

When determining the size of the pelvis, it is necessary to take into account the thickness of its bones; it is judged by the value of the so-called Solovyov index - the circumference of the wrist joint. The average index value is 14 cm. If the Solovyov index is more than 14 cm, it can be assumed that the pelvic bones are massive and the size of the small pelvis is smaller than expected.



And the head is above the entrance to the small pelvis; b the head is a small segment at the entrance to the pelvis; in the head with a large segment at the entrance to the small pelvis; d head in the wide part of the cavity of the small maz; e head in the narrow part of the pelvic cavity; e head at the pelvic outlet; I plane of the entrance to the small pelvis, II plane of the wide part of the pelvic cavity, III plane of the exit of the small pelvis.


Normally, the vertical size of the rhombus is on average 11 cm, the transverse size is 10 cm. If the structure of the pelvis is disturbed lumbosacral The rhombus is not clearly expressed, its shape and size are changed. However, spinal diseases can lead to incorrect assessments of the pelvis

The fetal skull consists of two frontal, two parietal, two temporal, one occipital, sphenoid and ethmoid bones. The following sutures are of greatest importance in obstetric practice: - sagittal (sagittal) suture connects the right and left parietal bones; in front the suture passes into the anterior (large) fontanel, in the back into the small (posterior); - the frontal suture is located between the frontal bones (in a newborn, the frontal bones have not yet fused together); - the coronal suture connects the frontal bones with the parietal bones and is located perpendicular to the sagittal and frontal sutures. The coronal suture connects the frontal bones with the parietal bones and runs perpendicular to the sagittal and frontal sutures; - the lambdoid (occipital) suture connects the occipital bone with the parietal bones.

The fetus as an object of birth At the junction of the sutures there are fontanelles. The anterior and posterior fontanelles are of practical importance. The anterior (large) fontanel is located at the junction of the sagittal, frontal and coronal sutures. It has a diamond shape and four sutures extend from it: frontal sutures anteriorly, sagittal sutures posteriorly, and coronal sutures to the right and left. The posterior (small) fontanelle is a small depression in which the sagittal and lambdoid sutures converge. It has a triangular shape. Three sutures extend from the posterior fontanel: anteriorly the sagittal suture, and to the right and left the corresponding sections of the lambdoid suture. For practical obstetrics, it is also important to know the tubercles that are located on the head: occipital, two parietal and two frontal. Knowledge of the topographic and anatomical features of the fetal bony head is very important for practical obstetrics, since the doctor is guided by these identification points when performing a vaginal examination during childbirth. The size of the head of a mature and full-term fetus is no less important than the sutures and fontanels; each moment of the labor mechanism corresponds to a certain size of the fetal head at which it passes through the birth canal


On the fetal head, two parts can be distinguished: a relatively small facial one: the lower jaw (1), the upper jaw (2) and a very voluminous one - the brain. The latter consists of seven bones: two frontal (3), two parietal (4), one occipital (5), two temporal (6). Small transverse size (diameter bitemporalis) – the distance between the most distant points of the coronal suture, length – 8 cm. 8. Large transverse size (diameter biparietalis) – distance between the parietal tubercles, length – 9.5 cm

The following dimensions are distinguished on the fetal body: 1. Transverse size of the shoulders (distantia biacromialis) 12 cm long and in circumference: for breech, leg and knee presentations - 34 cm (Fig. 18), for incomplete breech presentation - cm 2. Transverse size of the buttocks (distantia bisiliacalis) 9.5 cm long and in circumference: with incomplete breech presentation - 32 cm (see Fig. 19), with full leg presentation - 28 cm (Fig. 20), with complete breech presentation - 34 cm

The fetus as an object of labor Determination of the position of the fetal head relative to the interspinal line: –3 – head above the entrance to the pelvis; –2 – the head is pressed to the entrance to the pelvis; –1 – head as a small segment in the plane of the entrance to the pelvis; 0 – head with a large segment in the plane of the entrance to the pelvis; +1 – the head is a large segment in the wide part of the small pelvis; +2 – head in the narrow part of the pelvis; +3 – head on the pelvic floor; +4 – the head cuts in and erupts.



Special methods of obstetric examination. At the initial visit of a pregnant woman in the first and second trimesters of pregnancy, an examination of the external genitalia, examination of the vagina and cervix using vaginal speculum, vaginal (internal) and bimanual (external-internal) examinations are carried out (see Gynecological examination). First, the external genitalia, the perineum (its height, the distance from the posterior commissure to the anus is normally 45 cm), and the anus area are examined. Using vaginal speculum, examine the vagina and cervix. During a two-handed examination, the length and width of the vagina, the condition of its walls, the severity of the vault, the shape, size, and consistency of the cervix and the condition of its external os are determined. Then the position, shape, size, consistency, mobility of the uterus, the condition of the fallopian tubes, ovaries, parametric tissue, and the inner surface of the pelvic bones are assessed. Gynecological examination of the perineum-vagina





Places for the clearest hearing of heart sounds in different positions of the fetus: 1 anterior view, first position, cephalic presentation; 2 posterior view, first position, cephalic presentation; 3 anterior view, second position, cephalic presentation; 4 posterior view, second position, cephalic presentation;

Places of the clearest listening to heart sounds in different positions of the fetus 5 anterior view, first position, breech presentation; 6 posterior view, first position, breech presentation, 7 anterior view, second position, breech presentation; 8 posterior view, second position, breech presentation.

A significant part of prenatal invasive studies is cytogenetic diagnosis of chromosomal diseases. In these cases, the indications for its implementation are: the mother’s age is 35 years and older; the birth of a child with a chromosomal pathology in a family; carriage of a familial chromosomal abnormality; suspicion of the presence of congenital malformations in the fetus; In the first trimester of pregnancy, transcervical or transabdominal chorionic villus aspiration is most often performed. In the second trimester, amniocentesis, transabdominal aspiration of placental villi and transabdominal cordocentesis (puncture of umbilical cord vessels) are performed

Indications for this diagnostic procedure most often include the need for cytogenetic diagnosis of chromosomal diseases. In more rare cases, amniocentesis is performed in case of fetal hypoxia, isoserological incompatibility of the blood of mother and fetus, to assess the degree of fetal maturity (by the ratio of lecithin and sphingomyelin concentrations or by the number of anucleate lipid-containing “orange” cells), and the need for microbiological examination of amniotic fluid. Contraindications: threat of miscarriage and infection of the genital tract. The procedure is performed under ultrasound guidance, choosing access depending on the location of the placenta and fetus. In this case, both transabdominal (Fig. 4.42) and transcervical amniocentesis are performed.

Reasons for measuring/examining the head:
1. The head is the first to pass through the birth canal, making a series of sequential movements.
2. Yavl. voluminous and densest part.
3. The fontanelles, clearly palpable during childbirth, make it possible to clarify the nature of the insertion of the head in the small pelvis.
4. The degree of density of the bones of the skull and their mobility determines the ability of the head to compress in one direction and in the other.
the fetal head is bean-shaped. Consists of 2 parts: the face and the brain (volumetric) part. Skull - consists of 7 bones connected to each other by sutures.
SEAMS: 1. Frontal - between the 2 frontal bones. 2. Sagittal - between 2 parietal bones. 3. Lambdavid - between both parietal and occipital bones. 4. Coronoid - between both parietal and frontal bones.
fontanelles: fibrous plates at the junction of sutures. The main ones:
1. Large (anterior) - between the posterior parts of both frontals and the anterior parts of both parietals. Represents the connection. tk. plate, in the form of a rhombus (3O3 cm). Place of intersection of 3 seams: 1,2,4.
2. Small (rear) – has a pump function. Between the posterior parts of both parietals and the occipital bone.
Large and small fontanelle conn. arrow-shaped seam.
3. Lateral (secondary): anterolateral, posterolateral.
7 head sizes: 1) Straight - S from the bridge of the nose to the occipital protuberance. L=12 cm, d=34–35 cm.
2) Large oblique - S from the chin to the most distant point of the back of the head. L=13.5 cm, d=39–41 cm.
3) Small oblique - S from the suboccipital fossa to the middle of the large fontanel. L=9.5 cm, d=32 cm.
4) Middle oblique - S from the suboccipital fossa to the anterior corner of the large fontanel (scalp). L=10 cm, d=33 cm.
5) Large transverse - S between the most distant points of the parietal sutures. L=9.5 cm.
6) Small transverse - between the most distant points of the coronal suture. L = 8 cm.
7) Vertical (steep) – S from the middle of the large fontanel to the hyoid bone. L=9 cm, d=32–34 cm.
The pelvis from an obstetric point of view
Taz: The female pelvis is wider and shorter, wings iliac bones turned to the sides, the entrance to the small pelvis has the shape of a transverse oval, the shape of the pelvic cavity is cylindrical, the angle between the lower branches of the pubic bones is obtuse or straight.
In obstetric practice, the small pelvis is divided into 4 sections by conventional planes, which fan out from the pubic symphysis to the sacrum. IN clinical practice The following sizes are most commonly used female pelvis: distantia spinarum – the distance between the anterior superior iliac spines is 25–26 cm; distantia cristarum – the distance between the iliac crests is 28–29 cm; distantia trochanterica – the distance between the greater trochanters is 30–31 cm; true, or obstetric, conjugate - the distance between the posterior edge of the pubic symphysis and the promontory is 11 cm. To determine the obstetric conjugate, it is necessary to subtract 9 cm from the external direct size of 20–21 cm - a distance equal to the thickness of the tissues and the spinal column.
Normal sizes pelvis Definition of true conjugates
Full external pelvic measurement:
1.Distantia spinarum is the distance between the two anterior superior iliac spines (in N = 25 – 26 cm)
2. Distantia cristarum is the distance between the most distant points of the ridges (in N = 28 – 29 cm)
3.Distantia trochanterica is the distance between two trochanters (in N = 30 – 31 cm)
4.Conjugata externa is the distance between the anterior top part pubic symphysis and suprasacral fossa (in N = 20 – 21 cm)
If all 4 sizes are N, you can deliver through the vaginal birth canal.
5.Conjugata diagonalis – S from the lower edge of the promontory to the symphysis (in N = 13 cm).
6. Conjugata vera - to determine it - 9 cm is subtracted from Conjugata externa (N = 20–9 = 11 cm).
7. Solovyov index – wrist circumference (in N = 13 – 18 cm). If the Solovyov index is less than 16 cm, then the bones of the skeleton are considered thin and Conjugata vera = Conjugata diagonalis - 1.5 cm. If the Solovyov index is 16 cm or more, then the pelvic capacity will be less (Conjugata vera = Conjugata diagonalis - 2 cm).
8. Lateral Kerner conjugate is the distance between the anterior superior and posterior superior awns of the same side (in N = 15 cm)
9.Height of the pubis – in N = 5 cm
10. Pelvic height – the distance between the ischial tuberosity and the pubic tubercle (in N = 9 cm)
11. Michaelis rhombus is a rhombus whose vertices are the points: above - the suprasacral fossa, below - top edge gluteal fold, from the sides - the posterior superior iliac spines. Vertical size – 11 cm. Transverse size (Tridandani distance) – 10 cm.
12. Pelvic circumference – hip circumference in a non-pregnant state (at least 85 cm in N).
Objective methods for assessing fetal viability
Periods of fetal viability. From 28 to 37 weeks - the antenatal period - the period of fetal life during pregnancy.
The intranatal period is the period of life of the fetus during childbirth.
The postnatal period is divided into:
· Early – neonatal (first 7 days)
· Late – up to a month of life.
Childbirth. Premature - occurs from 28 to 37 weeks inclusive.
Urgent birth – 37 – 42 weeks.
Late birth – 43 weeks or more.
New criteria for live birth.
· Gestation period 22 – 27 weeks.
· Fruit weight 500 – 1000 g.
· Fruit length – 25 cm or more.
· There is one of the following signs: “heartbeat”, “spontaneous breathing”, “reflexes”, “pulsation of the umbilical cord”.
· If you lived 7 days of life.
Evaluation methods: 1) Non-invasive: determination of the level of α-fetoprotein. The study is carried out at 15–18 weeks. The level of fetoprotein in developmental defects is pathological. during pregnancy.
Ultrasound – 3 times – first visit ♀ – pregnancy diagnosis. 2 – at 16-
18 weeks assessment of growth rates, identifying development anomalies. 3 – 32–35 weeks. – condition, growth rate, term, position, weight of the fetus.
CTG, hysterography – continuous. simultaneous registering fetal heart rate and uterine tone.
2) Invasive: amniocentesis - puncture of amniotic fluid. The goal is cultivation, karyotyping. Chorionic biopsy – performed for karyotyping. Cordocentesis is a puncture of the fetal umbilical cord vessels to obtain its blood.
Hormonal function placenta
Placenta (P.) – “child’s place”, endocrine gland, cat. combines the function. system ♀and fetus. By the end of pregnancy, M = 500 g, d = 15–18 cm. The placenta is divided into the child's place, the maternal side, and the fetal side. Pl. – lobular organ (50–70 lobules). Functions: gas exchange, endocrine function, protective, excretory. Maternal and fetal. blood flows do not communicate with each other.
Hormonal function: Pl. together with the fruit the image. single endocrine system(fetoplacental system). In Pl. implementation etc. synthesis, secretion, transformation of hormones of protein and steroid nature. Hormone production occurs in the trophoblast syncytium, decidual tissue. Hormones Pl.:
– placental lactogen (PL) – synthesized only in the placenta, enters the mother’s blood, maintains the function of the placenta.
– human chorionic gonadotropin (CG) – synthesized by the placenta, enters the mother’s blood, and participates in the mechanisms of fetal sex differentiation.
– prolactin – synthesis. placenta and decidular tissue. – plays a role in the image and surfactant.
From cholesterol, containing. in the mother's blood, in the placenta the image. pregnenolone and progesterone. Steroid hormones also include estrogens (estradiol, estrone, estriol). They cause hyperplasia and hypertrophy of the endometrium and myometrium.
Besides these, Pl. capable of production testosterone, CS, thyroxine, parathyroid hormone, calcitonin, serotonin, etc.
Intrapartum fetal protection
The influence of childbirth on the condition of the fetus: the fetus experiences increasing e hypoxia, hypercapnia, acidosis. Scrum accompanied. decreased uterine hemodynamics. Complicated labor aggravates intrauterine hypoxia. During childbirth, the condition of the fetus worsens in parallel with the pharmacological load, and some problems occur. not directly toxic. e-e, but indirect.
The meaning of the body position of a woman in labor: the position of pregnant women. presented on the back additional load on the cardiovascular system, and breathe. woman's system. For the outcome of labor and fetal condition, and then for n/r. The mother's position is of no small importance. The most physiological at time pushing - semi-sitting or sitting position, as well as positioning on the side. Childbirth in horizontal positive and more often accompanied. traumatization of the fetus and greater physiological blood loss.
Surgical delivery: All operations are characterized by traumatic for the fetus. At the same time, they help ↓ perinatal mortality. Application of A. forceps - can lead to birth trauma n/r. C-section- allows noun ↓ perinatal mortality. The timeliness of the operation is of decisive importance when it is possible to avoid protracted labor, a long anhydrous interval and the onset of fetal hypoxia. Incorrectly chosen anesthesia and technical errors can have a negative impact on the fetus.
Features of care: after removal from the uterus, the baby is given the usual circle resuscitation measures, aerosol therapy is prescribed, often respiratory stimulants. and heart activities The frequency of complications reaches 10.9% (surgery during childbirth) and 1.7% (planned). The prognosis depends on the nature of A. pathology. The prognosis improves if the operation was performed as planned.
Birth trauma: a distinction is made between birth trauma, birth injuries and obstetric trauma. The first ones arose. under the doctor of physics. loads, properties. complicated giving birth The latter often more easily arose where there is an unfavorable background in the womb. development, aggravated by hypoxia during childbirth. For acute or chronic oblivion ♀, poisoning, pathological. during pregnancy, polyhydramnios, multiple pregnancies, post-term/premature pregnancy, rapid/ protracted labor, conditions are created for the occurrence of birth trauma.
Causes of intrauterine hypoxia and fetal death during childbirth: There are acute and chronic. fetal hypoxia: Chronic – 1. Maternal obstetrics (decompensated heart defects, diabetes, anemia, bronchopulmonary pathology, intoxication, infections). 2. Complications of pregnancy: late gestosis, postmaturity, polyhydramnios. 3. Fetal obstetrics: hemolytic. illness, generalization. IUI, developmental defects.
Acute – 1. Inadequate blood perfusion to the fetus from the maternal part of the placenta. 2. Placental abruption. 3. Clamping of the umbilical cord. 4. Inability to tolerate changes in oxygenation, connection. with contraction of the uterus.
Causes of fetal death during childbirth: 1. Fetal asphyxia. 2. Hemolytic. disease. 2. Birth injuries. 3. VUI. 4. Malformations of the fetus.
18. Perinatology, definitions, tasks
Perinatology (antenatal – from 28 weeks before the start of regular labor; intranatal – childbirth; postnatal – 7 days after birth). Objectives: 1. Prevention of pathology during childbirth.
2. Prevention of developmental defects.
3. Diagnosis of developmental defects.
4. Diagnosis and treatment of fetal distress.
AND
hAll parts of a full-term mature fetus require special study of the head. This is due to a number of reasons. Firstly, the fetal head is the most voluminous part and, as a rule, moving first along the birth canal, experiences the greatest difficulties. Secondly, the ability of the head to shrink in one direction and expand in the other largely depends on the degree of density of the bones of the skull and their mobility. Thanks to this, the fetal head can adapt to the size of the pelvis and overcome existing obstacles. In addition, the likelihood of injury to a woman’s soft birth canal and, to a certain extent, the occurrence of intracranial injury to the fetus depends on the density of the skull bones, their mobility and the size of the head. Thirdly, the sutures and fontanelles on the fetal head that are clearly palpated during childbirth make it possible to clarify the nature of the insertion of the head and its position in the small pelvis.
According to S. A. Mikhnov, the fetal head is bean-shaped. On the head of a newborn, 2 unequal parts are distinguished: the face (a relatively small part) and the brain skull (a bulky part). The skull of a newborn consists of 7 bones: two frontal, two parietal, two temporal and one occipital. All bones of the brain skull are connected to each other by fibrous plates that have a linear shape. These fibrous plates are called sutures. Thanks to them, the bones of the skull become mobile relative to each other. There are several sutures on the fetal head that are of practical importance in obstetrics (see color chart, Fig. 9). The frontal suture (sut. frontalis) connects the two frontal bones. Coronal suture(sut. coronaria) connects the frontal and parietal bones on each side of the skull and runs in the frontal direction. Sagittal, or sagittal, suture (sut.
sagittalis) connects the two parietal bones. Lambdoid, or occipital, suture (sut. lambdoidea) in the form of a Greek letter )S and pass extends between both parietal bones on one side and the occipital bone on the other. Temporal suture (sut. temporalis) connects on each side temporal bones with parietal, frontal, basal and occipital.
The fibrous plates at the junction of the sutures are called fontanelles. There are 2 main fontanelles and 2 pairs of secondary (lateral) ones. The main fontanelles include (large and small fontanelles. The anterior, large fontanel (fonticulus anterior, fonticulus magnus, s. Bregmaticus) is located at the intersection of the vendinal, frontal and frontal sutures. It lies in the center between four parts (two frontal and two parietal) and has the shape of a diamond. The acute angle of this diamond is directed anteriorly (towards the forehead), and the obtuse angle is directed posteriorly (towards the back of the head). The size of the anterior fontanel is usually 2-3 cm at the time of birth. Small fontanel (fonticulus posterior, s. fonticulus minor, parvus) located "n" at the intersection of the sagittal and lambdoid sutures. By the time of birth, it is closed and is determined by the finger as the place where 3 sutures converge, and the sagittal suture ends in the fontanelle itself and does not go beyond it limits where the smooth (occipital) bone is determined. In the anterior fontanel, 4 sutures converge, each of which, being continued through the fontanel, again leads to a suture. The same type of rollers is called a suture (fonticulus lateralis). They are located in two on the right and left sides of the skull, have a triangular or quadrangular shape. At the junction of the parietal, sphenoid, frontal and temporal bones) there is a wedge-shaped (roof-shaped) fontanel (fonticulus spEEliQldalisTsTptenon). At the junction of the parietal, temporal and occipital bones there is a mastoid and supero-posterior fontanel (fonticulus mastoideus, s. asterion). Lateral fontanelles acquire diagnostic value with significant disruption of the biomechanism of childbirth. In these cases, they occupy a central position in the small pelvis and can be mistaken for one of the main fontanelles.
On the head of a mature fetus, there are a number of sizes that need to be known to understand the biomechanism of labor (see color plate, Fig. 9).
1. Straight size(diametr frontooccipitalis recta) - from the bridge of the nose to the occipital protuberance - is 12 cm. The circumference of the head, measured through these points (circumferentia frontooccipitalis), is 34 cm.
2. Large oblique size(diametr mentooccipitalis, obliqus major) - from the chin to the most distant point on the back of the head - is 13.5 cm. The circumference of the head corresponding to this size (circumferentia mentooccipitalis) is 39-40 cm.
3. Small oblique size(diametr suboccipitobregmaticus, s. obliqus minor) - from the suboccipital fossa to the middle of the anterior fontanel - is 9.5 cm. The circumference of the head corresponding to this size (circumferentia suboccipitobregmatica) is 32 cm.
4. Medium oblique size(diametr suboccipitofrontalis, s. obliqus media) - from the suboccipital fossa to the anterior angle of the anterior fontanel (border of the scalp) - equal to 10.5 cm. The circumference of the head corresponding to this size (circumferentia suboccipitofrontalis) is 33 cm.
5. Vertical or plumb dimension(diametr sublinguobregmaticus, s. tracheobregmaticus, s. verticalis) - this is the distance from the hyoid bone to the middle of the anterior fontanel - is equal to 9.5 cm. The circumference of the head corresponding to this size (circumferentia tracheobregmatica, s. sublinguobregmatica) is - measures 32-33 cm.
6. Large transverse size(diametr biparietalis) - the greatest distance between the parietal tuberosities - is 9.5 cm.
7. Small transverse size(diametr bitemporalis) - the distance between the most distant points of the coronal suture is 8 cm.
The size of the shoulders and buttocks is also determined on the body of a mature fetus. The transverse size of the shoulders (distantia biacromialis) is 12-12.5 cm (circumference is 34-35 cm). The transverse size of the buttocks (distantia biiliacus) is 9-9.5 cm (circumference is 27-28 cm).
Lecture 3. The fetus as an object of birth. Obstetric terminology.
The maturity of the fetus is determined by its morphofunctional characteristics physical development. Term of the fetus is determined by the length of its stay in the uterus from the moment of conception to birth. Maturity and full term - different concepts. A mature and full-term fetus has a body weight of more than 2000 g (the current average is 3500 g) and a body length of 45 cm (and an average of 50-52 cm). He shows great activity, moves his limbs, screams loudly. Has a fairly developed subcutaneous fat layer, pink color skin, dense cartilage ears and nose, hair on the head is 2-3 cm long. The fluff is preserved only on shoulder girdle and in the upper back. The umbilical cord is located midway between the pubis and the xiphoid process. In boys, the testicles are lowered into the scrotum; in girls, the clitoris and labia minora are covered by the labia majora.
The influence of the fetal head on the course of labor is explained by for the following reasons:
1. The fetal head is its most voluminous formation, least susceptible to deformations necessary during childbirth.
2. During childbirth, it is the head, due to its volume and density, that experiences the greatest difficulties from the birth canal, preventing its progress:
3. The possibility of birth trauma to the mother (damage to the birth canal) and fetus (intracranial hemorrhage) largely depends on the degree of density and mobility of the bones of the skull;
4. Identification points on the head (sagittal suture, large and small fontanelles) allow them to be used during childbirth for diagnostic purposes,
5. About 96% of all births occur in cephalic presentations.
Brain part of the skull. The bones of the brain part of the skull are connected by fibrous membranes - sutures. The following seams are distinguished:
1. sagittal, located between the edges of the parietal bones and two fontanelles
2. frontal located between the two frontal bones;
3. occipital, located between the posterior edges of the parietal bones and the occipital bone
4. coronal suture, located between the frontal and parietal bones. The intersections of the sutures are called fontanelles. There are two main fontanelles - large and small. The large fontanelle (bregma) has a diamond shape and is located at the intersection of the coronal, frontal and sagittal sutures, connecting four bones - two frontal and two parietal. The small fontanel (lambda) has a triangular shape and is located at the intersection of the sagittal and occipital sutures.
Dimensions of the head of a mature, full-term fetus.
1. Small oblique size - from the center of the large fontanel to the suboccipital fossa It is 5 cm; its corresponding circumference is 32 cm.
2. The average oblique size - from the suboccipital fossa to the border of the scalp, is 10 cm; the circumference corresponding to it is 33 cm;
3. large oblique size - from the chin to the occipital protuberance - 13 cm and 38-42 cm
4. direct size - from the glabella to the occipital protuberance, equal to 12 cm; the circumference corresponding to it is 35 cm;
5. vertical - from the hyoid bone to the center of the large fontanelle, -9.5. cm-circumference-- 32cm;
6. large transverse dimension is the distance between the most distant points of the parietal tubercles, 9.5 cm.
7. small transverse size) - this is the distance between the most distant points of the coronal suture, that is, the temporal fossae, equal to 8 cm.
Dimensions on the body of a mature, full-term fetus.
1) the transverse size of the hanger is 12 cm, the circumference is 35 cm;
2) the transverse size of the buttocks is 9 cm, the circumference is 28 cm.
Obstetric terms for determining the location of the fetus in the uterus.
Habitus - the relationship of the limbs and head to the body of the fetus. Physiologically, the fetal position is bent: the head is bent and the chin is pressed to the chest, the back is curved outward; the arms are bent at the elbow joints and crossed on the chest; the legs are bent at the knee and hip joints, extended at the ankles, crossed and pressed to the stomach. With this arrangement, the fetus has an ovoid shape and occupies the smallest space in the uterine cavity. Extended articulation is a deviation from the physiological one and in some cases leads to a pathological course of labor.
Position- the ratio of the axis of the fetus to the vertical axis of the uterus. The fetal axis is a line running along the back of the fetus, from the back of the head to the tailbone. There are three options for the position of the fetus in the uterus: longitudinal, transverse and oblique. Longitudinal position-axis the fetus coincides with the vertical axis of the uterus. This position is physiological. Transverse position - the axis of the fetus and the axis of the uterus intersect at a right angle, and the head and buttocks of the fetus are at the level of the border of the large pelvis or slightly higher. Oblique position - the axis of the fetus and the axis of the uterus intersect at an acute angle, with the head or pelvic end of the fetus located in one of the iliac regions.
Position (rositio)-relation of the fetal back to the right or left side of the uterus. The first position is the back of the fetus facing the left side of the uterus. The second position is the back of the fetus facing right side uterus. In transverse and oblique positions of the fetus, the position is determined by the fetal head; the head is located on the left side of the uterus - the first position; the head is located on the right side of the uterus - the second position.
View(visus) position; - the relationship of the back of the fetus to the anterior or posterior side of the uterus. The fetal back is directed not only to one of the sides of the uterus, but also somewhat anteriorly or posteriorly. Anterior view - the back of the fetus is facing slightly anteriorly. Posterior view - the back of the fetus is turned slightly posteriorly.
Presentation (prgaesentatio) It is customary to call the ratio of the large part of the fetus to the plane of entry into the pelvic cavity.
Presenting part of the fetus (para praeua) It is customary to call that part of the fetus that during childbirth is the first to descend into the pelvic cavity.
Insertion- formation of tight contact between the fetal head and the entrance to the small pelvis, in which a belt of contact is formed (i.e. soft fabrics The birth canal tightly covers the head in its small or large size, and the head itself is fixed at the entrance to the small pelvis. Correct (axial or synclitic insertion - one in which the head is not tilted and the sagittal suture is at the same distance from the pubis and sacrum
Classification of fetal positions and presentations
1.Longitudinal position
1) Head presentation
A Flexion presentations
▪ anterior view of occipital presentation - physiological labor,
▪ posterior view of occipital presentation.
B extension presentation:
▪ anterior cephalic presentation,
▪ frontal presentation,
▪ facial presentation.
2) Breech presentation - when the pelvic end of the fetus is located above the entrance to the pelvic cavity:
A Flexion presentations:
▪ pure breech presentation,
▪ mixed breech presentation
B Extensor presentation;
▪ full leg presentation,
▪ incomplete leg.
II Transverse position.
III Oblique position
Lecture 3. The fetus as an object of birth. Obstetric terminology. - concept and types. Classification and features of the category "Lecture 3. The fetus as an object of childbirth. Obstetric terminology." 2017, 2018.