Recognizing signs of respiratory distress and providing timely assistance often prevents other serious complications, for example, anaphylactic shock. Respiratory problems require immediate attention or they can lead to death.
Signs of respiratory distress - superficial, rapid breathing. Despite trying to breathe, the victim cannot inhale enough air or begins to choke, signs of suffocation appear, accompanied by feelings of fear and confusion. The victim may feel dizzy and sometimes clutch his neck.
In any case, when providing assistance, you need to be sure of your own safety, since the victim may exhale toxic substances.
If the victim is breathing, albeit with difficulty, then the heart is beating.
You need to help him sit comfortably, open the window, unbutton his shirt collar, loosen his tie and belt. Ask someone to call an ambulance (if you cannot do it yourself) and make sure that it is called.
If there are witnesses to the incident, you need to interview them about what happened. The victim can confirm their story with a nod of the head or say “yes” or “no”. You need to try to reduce the victim’s anxiety, which also makes breathing difficult, find out what medicines help him in this condition (bronchodilators, etc.), while continuing to monitor for signs indicating breathing disorders. You should cover the victim if it is cold outside, move (help him leave) into the shade if it is hot outside.
If it is clear that rapid breathing is caused by emotional arousal, you should ask the victim to relax and breathe slowly. Often this is enough. When the victim stops breathing, he requires artificial lung ventilation (ALV) “mouth to mouth” or “mouth to nose”.
Artificial ventilation
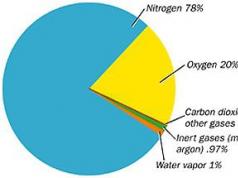
Remember! Without breathing (i.e. without oxygen supply), the brain can live for 4-6 minutes (Fig. 15.1). When conducting artificial ventilation lungs (ventilator), the exhaled air contains 16% oxygen, which is enough to maintain the life of the brain.
Rice. 15.1. Time is of the essence for starting resuscitation
If you do not see, hear, or feel any signs of breathing, immediately make two slow exhalations into the victim’s airway through a napkin (handkerchief). Then you need to check for a pulse.
If the victim is not breathing, but the pulse is carotid artery he has it, you should start mechanical ventilation: exhale, keep the airways open with your head thrown back and your chin raised (Fig. 15.2).

The thrown back head and raised chin not only open the airways, eliminating the retraction of the tongue, but also move the epiglottis, opening the entrance to the trachea. It is necessary to carefully squeeze the victim’s nostrils with your large and index fingers, pressing your palm on his forehead. Then, cover the victim’s mouth with your mouth and slowly exhale into it until it is visible that his chest rises (Fig. 15.3).

Rice. 15.3. Mouth-to-mouth breathing
Each breath should last about 1.5 seconds with pauses between your breaths. It is necessary to observe the chest with each breath to be sure that ventilation is actually being carried out. If the chest rise is not visible, the victim's head may not be tilted back enough. You need to throw your head back and try to breathe again. If the chest does not rise, then the airway is blocked foreign body, which needs to be deleted.
You need to check the pulse after the first two breaths: if there is a pulse, you can continue mechanical ventilation with a frequency of 1 breath every 5 s. When counting “one and”, “two and”, “three and”, “four and”, “five and” 5 seconds will pass. After this, the rescuer must inhale himself and then exhale into the victim. Then continue breathing at a frequency of 1 breath every 5 seconds. Each breath lasts 1.5 seconds. After one minute of mechanical ventilation (about 12 breaths), you need to check the pulse and make sure that the heart is beating. If breathing does not appear, continue mechanical ventilation. Check your pulse every minute.
- the victim began to breathe on his own;
- the victim’s pulse has disappeared (cardiopulmonary resuscitation must be started);
- other rescuers came to your aid;
- arrived " ambulance"and continues mechanical ventilation;
- you have exhausted your strength.
Remember! Stop mechanical ventilation if:
reduction of cyanosis (blueness of the skin);
pulsation of large arteries (primarily the carotid) according to the frequency of massage;
the appearance of independent respiratory movements.
The massage should be continued until spontaneous heart contractions are restored, ensuring sufficient blood circulation. The indicator will be determined on radial arteries pulse and increase in systolic blood pressure to 80-90 mm Hg. Art. The absence of independent heart activity with undoubted signs of the effectiveness of the massage is an indication for continued indirect cardiac massage.
1.5 Complications of cardiopulmonary resuscitation
Complications cardiopulmonary resuscitation are not an indication for termination resuscitation measures.
rib fractures;
sternum fracture;
rupture of the lungs or heart;
liver injury.
1.6 Criteria for stopping cardiopulmonary resuscitation
Resuscitation can only be stopped in the following cases:
if during CPR it turns out that it is not indicated for the patient;
if using all available CPR methods there are no signs of effectiveness within 30 minutes;
if there is (emergence) a danger to the health of those performing resuscitation;
when a situation arises that poses a threat to the lives of others.
1.7 Signs of biological death
If CPR fails, biological death occurs. The fact of the occurrence of biological death can be established by the presence reliable signs, and before their appearance - according to a set of signs. Reliable signs of biological death:
1. Cadaveric spots-begin to form 2-4 hours after cardiac arrest.
2. Rigor mortis - manifests itself 2-4 hours after circulatory arrest, reaches a maximum at the end of the first day and goes away spontaneously within 3-4 days.
A set of signs that allows one to ascertain biological death before the appearance of reliable signs:
Absence of cardiac activity (no pulse in the carotid arteries, heart sounds cannot be heard).
The time of absence of cardiac activity has been reliably established more than 30 minutes under normal (room) ambient temperature conditions.
Lack of breathing.
Maximum dilation of the pupils and their lack of reaction to light.
Absence of corneal reflex.
The presence of post-mortem hypostasis (dark blue spots) in sloping parts of the body.
These signs are not a basis for declaring biological death when they occur under conditions of deep cooling (body temperature + 32°C) or against the background of the action of drugs that depress the central nervous system.
Method of applying a hemostatic tourniquet for bleeding
The tourniquet is used only to stop arterial bleeding and only on the extremities. When applying a tourniquet, several rules must be impeccably followed, failure to comply with which can lead to serious consequences, from amputation of the damaged limb to the death of the victim.
The tourniquet is applied at the upper border of the wound, 5 cm higher. You cannot apply the tourniquet directly to the skin; be sure to place fabric under the tourniquet. Otherwise serious damage will occur skin at the site where the tourniquet is applied. A bandage should not be applied to the tourniquet; the tourniquet must be visible, especially if the victim is unconscious.
On the victim’s body, with a pen or felt-tip pen in two visible places, write down clearly and legibly, and do not remember or say, the time of application of the tourniquet. Inserting pieces of paper is highly undesirable - they get lost, get wet, etc. during transportation.
The tourniquet is applied on the upper extremities for up to 1.5 hours, on the lower extremities for up to 2 hours. In cold weather, the duration of application of the tourniquet is reduced by 30 minutes. When the time is up, remove the tourniquet for 15 seconds. Further application time is reduced by 2 times from the initial one. Compliance with this regime is strictly necessary. Longer application of a tourniquet threatens the development of ischemia and subsequent amputation of the limb.
When a tourniquet is applied, the patient experiences severe painful sensation. The victim will try to loosen the tourniquet - you need to be prepared for this. Signs of correct application of the tourniquet: there should be no pulsation below the wound. The fingers on the limbs turn white and become cold.
On the forearm and lower leg, applying a tourniquet may not be effective due to the radius bones, so in this case, if the first attempt is unsuccessful, the tourniquet can be applied in the lower third of the shoulder or in the lower third of the thigh.
When a tourniquet is applied, there is no stopping the bleeding as such, it is only delayed. In reality, it is possible to stop arterial bleeding only in a hospital setting. Therefore, after applying a tourniquet, urgent transportation of the victim to a medical facility is required.
General principles of first aid for fractures
Avoid any unnecessary movement around the fracture area.
For fractures of the lower extremities, move the victim only if his life is in danger. Check the pulse below the fracture site. If you feel like there is no pulse, consider it a very urgent matter.
You can position a person with a broken arm, hand, or collarbone more comfortably by placing a bandage over the fracture and hanging the arm from a scarf.
Open fractures require special attention.
Fractures of the neck and spine are especially dangerous and should be handled with great care.
If you are forced to apply temporary splints, remember to immobilize at least two joints closest to the injured area, otherwise the fracture site will not be immobilized.
Always carefully protect the area with cotton or gauze and avoid unnecessary pressure unless you need to stop heavy bleeding. For fractures of the lower extremities, immobilization can be achieved when the affected limb is connected to the healthy one using soft pads.
Rib fractures may be accompanied by pneumothorax. In such cases, the wound should be closed immediately and carefully using an occlusive dressing.
Educational question No. 2 Medical triage, the principles of its organization and implementation at the prehospital stage, the forces and means involved.
When considering issues of organizing the provision of assistance to victims during the liquidation of the consequences of disasters and natural disasters, the first place is traditionally given to medical triage of victims as one of the most important medical and organizational activities.
Nowadays, under medical triage understand the method of dividing victims into groups based on the principle of need for homogeneous treatment, preventive and evacuation measures, depending on medical indications and specific conditions of the situation.
Medical triage- one of the most important methods of organizing medical care for victims when they are massively admitted to medical institutions.
Purpose of sorting is to ensure that victims receive timely assistance medical care and rational further evacuation. This becomes especially important in situations where the number of people in need of medical care (or evacuation) exceeds the capacity of local (territorial) healthcare.
During the process of medical triage, the volume of medical care and the number of victims to whom it should be provided and the order of care are determined.
First of all, children who are injured with unstoppable external or internal bleeding, in a state of shock, asphyxia, with prolonged pressure syndrome, in a convulsive state, unconscious, with a penetrating wound of the chest or abdominal area need help in the center of mass destruction and in removal from it. cavities that are exposed to damaging factors that aggravate the damage (burning clothing, the presence of SDYA in open parts of the body, etc.).
Medical triage is a specific, continuous, repeating and successive process in providing victims of all types of medical care. It is carried out starting from the moment of provision of first medical aid (primary triage) on site (in the disaster zone) or outside the affected area - the first stage of medical evacuation, as well as when victims are admitted to medical institutions- second stage of medical evacuation.
Depending on the tasks being solved, it is customary to distinguish two types of medical triage: intra-point (intra-stage) And evacuation and transport.
Intra-point sorting victims is carried out in order to distribute them into groups depending on the degree of danger to others, as well as to establish the priority of medical care and determine the functional department of a given stage of medical evacuation or a medical institution where assistance should be provided.
Evacuation and transport sorting is carried out with the aim of distributing victims into homogeneous groups according to the order of evacuation and type of transport (railway, road, etc.), to determine the position of the injured in transport (lying, sitting) and resolving the issue of the place of evacuation (determination of the destination) taking into account localization, the nature and severity of the injury.
Sorting is based on three main sorting criteria:
danger to others;
medicinal sign;
evacuation sign.
TOdangerous for others relate:
those in need of special (sanitary) treatment (partial or complete) - those arriving with contamination of the skin and clothing with RV, SDYAV, BA, are sent to the special treatment site;
subject to temporary isolation - infectious patients and those suspected of having infectious disease, are sent to the infectious diseases isolation ward;
persons with severe mental disorders who are sent to a psychoisolator.
Depending on the degree of need victims in medical care, the priority and place of its provision, they can be divided into the following groups:
those in need of emergency medical care;
not needing this moment in medical care, i.e. assistance can be delayed until they are admitted to a medical institution;
those affected in a terminal state (agoning), requiring symptomatic therapy to reduce suffering.
Based evacuation sign (necessity and priority of evacuation, type of transport, position on transport where evacuated) victims are divided into groups:
those subject to evacuation to other medical institutions or centers of the republic, taking into account the evacuation purpose, priority, method of evacuation (lying, sitting), type of transport;
subject to stay in a given medical institution (due to the severity of the condition) temporarily or until the final outcome;
subject to return to their place of residence (resettlement) for outpatient treatment or medical observation.
To carry out medical triage most effectively, it is advisable to create triage medical teams from the most experienced doctors of the appropriate profile.
When carrying out triage, medical personnel must first identify those affected who are dangerous to others, and then, through a cursory examination of the victims who are most in need of medical care (the presence of external bleeding, asphyxia, women in labor, children, etc.). After selective sorting, they move on to sequential (“conveyor”) examination of the victims. Medical triage is usually carried out on the basis of data from an external examination of victims (patients), their questioning, familiarization with medical documentation (if available), the use of simple research methods and simple diagnostic equipment.
Based on the data obtained, a diagnosis is established and a prognosis is given for the injury, the degree of threat to the life of the affected person at the time of triage, the urgency, priority of provision and type of medical care at the moment and at the subsequent stage of evacuation, the need to create special conditions (isolation from others, etc.) are determined. and the procedure for further evacuation.
When providing medical care in a disaster zone by medical and nursing teams and emergency medical teams, the following groups of victims can be identified:
those in need of medical care in the disaster zone first or second;
those in need of removal or removal first or second (lying or sitting);
walking (slightly affected), which can follow from the lesion independently or with assistance.
Immediately upon arrival of victims at the first stage of medical evacuation, medical triage is carried out in order to:
identifying victims who pose a danger to others and need special measures (sanitary treatment);
identifying those in need of emergency first aid medical care to direct them to the appropriate functional departments;
preparations for further evacuation.
In this regard, medical triage begins at the sorting site (distribution post), where victims who need sanitary treatment (with contamination of the skin and clothing with radioactive substances, SDYV) are identified and subject to referral to a special treatment site, and also infectious patients and persons in state of strong psychomotor agitation, which are subject to isolation. All other victims are sent to the emergency department.
In the reception and triage department, among the delivered victims, the following triage groups are distinguished based on an assessment of the general condition, the nature of the injury, and the complications that have arisen:
victims in serious condition who need medical care for life-saving (urgent) reasons. Their number may account for 20% of all admissions;
victims of moderate severity, for whom medical care is provided in second priority or may be delayed. The number of such victims may be 20%;
lightly wounded, medical care for which may be significantly delayed. They may account for 40% of all affected;
victims who have lost prospects for survival (agoning) and need symptomatic therapy - 20% of all affected.
Study question No. 3 Medical evacuation. Pre-evacuation preparation activities, their organization and implementation, attracted forces and means.
An integral part of treatment and evacuation support for victims is medical evacuation. It combines treatment and preventive measures dispersed in place and time into a single process of providing medical care.
Medical evacuation begins with the organized removal, withdrawal and removal of victims from the disaster zone, providing them with first aid and ends with the delivery of victims to a medical facility.
Depending on the situation, special, adapted and unadapted road, rail, water and air transport can be used to evacuate victims. Due to the lack of special vehicles, national transport is used, which is equipped with special or improvised devices for the evacuation of seriously injured people (equipment with a universal sanitary device for installing USP-G stretchers, adding ballast to the vehicle body to soften shaking, covering the vehicle bodies with awnings, etc.).
The most convenient for evacuating victims are buses equipped standard sanitary equipment (TSO) for installing a stretcher. However, as the experience of the service in disaster zones shows, the most difficult is the evacuation (removal, removal) of those affected through rubble, fires, etc. If it is not possible to move vehicles to the locations of the affected people, their removal on stretchers or improvised means is organized to places of possible loading onto transport.
When evacuating victims by rail (water) transport, access roads are equipped at loading (unloading) points. Piers, platforms, and gangways can also be used for these purposes. In case of bad weather conditions, measures are taken to protect victims from their effects.
Victims in a state of mental agitation during evacuation are secured with straps to the stretcher to prevent them from falling from the vehicle. For the same purpose, they are given sedative drugs, and sometimes accompanying persons are provided.
Medical evacuation is carried out mainly on the “self-guided” principle - by ambulances, medical institutions, etc., but the possibility (if transport is available) of evacuation on the “self-directed” principle is not excluded - by transport of the affected facility, rescue teams and etc.
Evacuation of victims to the first stage of medical evacuation is carried out in the form of a single flow in one direction. This type of evacuation was called “directional”.
Evacuation of victims from the first stage to the second is carried out to a strictly designated hospital, depending on the location of the injury or the nature of the lesion. It is called “destination” evacuation.
In conditions where for medical evacuation it is necessary to widely use various types of adapted and unadapted vehicles, evacuation and transport triage of victims with the preparation of medical documents for evacuees is of particular importance.
The evacuation of victims from sources of chemical, bacterial and radiation damage is organized in accordance with general principles, although it also has a number of features.
Thus, the majority of severely affected patients will require first aid in the immediate vicinity of the lesion until they are removed from a non-transportable state, followed by evacuation to the nearest medical facility. At the same time, priority remains with evacuation and transport sorting.
The evacuation of patients from hotbeds of dangerous infectious diseases is sharply limited or should not be carried out at all. If necessary, it must strictly comply with the requirements of the anti-epidemic regime in order to prevent the spread of infection along evacuation routes. For this purpose, special routes for traffic are determined, stops in populated areas when moving through them. In addition, vehicles transporting infectious patients must have a supply of disinfectants, containers for collecting secretions from patients, and they must be accompanied by medical personnel.
Certain difficulties may also arise during the evacuation of victims from sources of radioactive contamination (accidents at nuclear power plants, during the transportation of radioactive substances, etc.). In such cases, timely and high-quality triage of victims, provision of emergency care sick (vomiting, collapse), carrying out sanitary treatment, subsequent evacuation to specialized hospitals.
Thus, medical evacuation provides timely provision of medical care to victims and combines medical and evacuation measures scattered in place and time into one whole. In addition, evacuation frees up some medical personnel for emergency work in the disaster zone. On the other hand, any transportation negatively affects the health of the victim and the course of the pathological process, therefore evacuation activities require careful preparation and organization.
Preparation of victims for evacuation begins immediately from the beginning of providing them with medical care, because Competently provided full medical care is, to a certain extent, a guarantee that the victim will be delivered to the hospital with minimal problems. hospital stage. Even the most gentle transportation conditions will contribute to a certain deterioration of the victim’s condition.
To prevent deterioration of the victim’s condition during transportation, it is necessary to monitor his vital functions during preparation for medical evacuation and the evacuation itself.
For this purpose, immediately before loading into the ambulance transport, the victim is examined again and the pulse is assessed. Blood pressure, respiratory rate and, if necessary, corrective therapy (additional analgesia, infusion therapy, symptomatic medications), as well as transportation accompanied by a medical worker equipped with an emergency aid kit.
Study question No. 5 Features of organizing the provision of medical care during various types natural disasters (hurricanes, floods, fires).
Providing medical care in various natural emergencies has its own characteristics. The most common natural disasters that occur in our country are floods, fires and hurricanes, and much less often - tectonic processes (earthquakes).
Flood- temporary flooding of a significant part of the land adjacent to a river, lake or reservoir.
Healthcare tactics have their own characteristics. What matters in this case is the fact that a large number of people are homeless, drinking water and food, exposed to cold, wind and other meteorological factors, and neuropsychic stress.
The amount of sanitary losses during floods can vary widely depending on population density, timeliness of warning, height of the flood wave, temperature and speed of movement of water and air, and other situational conditions. In case of sudden flooding, the total losses on average can amount to 20–35% of the number of residents in the flood zone. In cold weather, they usually increase by 10–20%, depending on the length of time the victims remain in the water.
The structure of sanitary losses during floods is dominated by victims with symptoms of asphyxia, acute dysfunction of the respiratory and cardiovascular systems, concussion, general cooling, as well as soft tissue injuries, etc. There may also be victims with mental disorders.
The sanitary-hygienic and sanitary-epidemiological condition of the affected region is deteriorating. In this case, what matters, first of all, is the scale of the flooded area and the fact that a large number of people find themselves without shelter, drinking water and food, and are exposed to cold, wind and other meteorological factors.
Medical and sanitary provision of the population is carried out in order to reduce the severity of damage to people by timely provision of first medical, first aid, qualified and specialized medical care to victims and their referral, if necessary, to medical institutions, as well as ensuring sanitary and epidemiological well-being in the flood zone.
Medical support measures are carried out in two stages:
at the first stage, during the immediate evacuation of the population or sheltering it in non-flooded areas, medical support for evacuation measures is organized, and people are sent to places of temporary accommodation medical workers with means of providing medical care;
at the second stage, after the arrival and deployment of appropriate medical forces and equipment, measures are taken to provide first medical, first aid, qualified and specialized medical care to the affected population in accordance with the specific situation.
The main consequences of floods can be drowning of people, mechanical injuries, the appearance of neuropsychic overstrain (a state of psycho-emotional disorder) in a significant part of the population, and exacerbation of various chronic diseases. The incidence of pneumonia with high mortality is increasing. Frostbite occurs due to hypothermia. In the structure of sanitary losses, those affected by asphyxia, acute impairment of respiratory and cardiac activity, and chills will prevail.
To eliminate the medical consequences, formations of the EMF service, other forces and means, including medical units of units and formations of the Armed Forces, are involved if they are involved in eliminating the consequences of the flood.
Personnel involved in flood rescue operations must be trained in the rules of conduct on water and techniques for rescuing people from half-flooded buildings, structures and other structures, as well as techniques for rescuing drowning people and providing them with first aid.
After removing victims from the water (rescue) and providing first aid, they are delivered to shore in temporary collection points for the affected.
At collection points, first aid continues to be provided to those affected if necessary and they are prepared for evacuation to medical institutions.
The situation in large areas of the flood-affected region may be complicated by a sharp deterioration in the sanitary and epidemiological situation and the associated risk of the emergence and spread of infectious (mainly intestinal) diseases. Sanitary, hygienic and anti-epidemic measures are organized and carried out by sanitary supervisory authorities and include:
control of the sanitary and epidemiological condition of the surrounding territory, buildings for temporary accommodation of evacuees, as well as isolation wards for infectious patients;
control of compliance with sanitary and hygienic standards and supply rules drinking water(providing the population with individual means of water disinfection) and food storage;
organizing epidemiological surveillance, identifying infectious patients and their hospitalization;
control over the organization of bath and laundry services for the population in places of temporary settlement;
control of insects and rodents, control over the organization of removal and disinfection of sewage and food waste along travel routes and in areas of temporary settlement.
Upon admission of the affected population, specialists from treatment and preventive health care institutions Special attention for patients in need of emergency medical care and for identifying infectious diseases.
To organize sanitary-hygienic and anti-epidemic measures in flood zones, sanitary-epidemiological teams and emergency sanitary-preventive assistance teams are sent, which are created on the basis of the centers of hygiene and epidemiology (H&E).
Fires- spontaneous spread of fire out of human control. They often result in death, cause burns and injuries, carbon monoxide (CO) poisoning, have a psychologically traumatic effect on the population and cause great material damage.
The organization of medical care has a number of features:
a thorough search for victims in smoke-filled areas and inside burning premises (carried out by fire and rescue units);
providing first aid and emergency evacuation from a smoke-filled area;
maximum approach and provision of first medical aid;
the need to provide medical care to a large number of burnt victims, as well as victims of CO poisoning.
This will require strengthening medical institutions with intensive care and resuscitation teams, as well as specialized combustiological (burn) teams and additionally providing them with the necessary medicines, equipment and equipment.
Study question No. 6 Features of organizing the provision of medical care in various types of major industrial and transport accidents.
Road transportincidents
In road accidents, a significant proportion of victims die from untimely provision of medical care, although the injuries in some cases are not fatal in severity. According to WHO, 20 out of 100 victims could have been saved if medical assistance had been provided to them in a timely manner.
As a result of road accidents, the most common injuries are traumatic brain injuries, injuries to the chest and abdomen, and fractures of long tubular bones limbs, extensive soft tissue wounds. The wounds are usually lacerated, deep, and often contaminated with soil.
First aid is the basis for saving lives before medical workers arrive. It is provided by traffic police officers, passers-by, drivers, as well as in the form of self- and mutual assistance.
Pre-medical and first aid is provided by emergency medical teams at the scene of an accident and on the way to a medical facility.
Emergency qualified care is provided in a medical institution, and specialized medical care is provided in specialized medical institutions (departments).
Train accidents
Train accidents are accompanied by the loss of a large number of people. Up to 50% of the total number of passengers may be injured.
Most of them receive mechanical injuries - up to 90%, thermal - up to 20%. High specific gravity combined lesions - up to 60%.
Before the arrival of emergency medical services, victims are provided with assistance in the form of self- and mutual assistance.
Ambulance and emergency medical services teams arriving at the scene of the disaster provide pre-hospital and first aid to the victims, and also triage them based on the severity of their condition.
The ambulance team that arrived first in the disaster area is the senior one before the arrival of the responsible medical worker or senior medical commander, is responsible for and manages the medical triage, determines the priority of providing medical care to the injured and preparing them for transportation, and remains at the scene until the rescue work is completed. .
Evacuation is carried out to medical institutions by sanitary transport, always accompanied by a medical worker. In this case, it is necessary to take into account the even distribution of victims among medical institutions (the responsibility of the dispatcher).
Plane crashes
The transportation of passengers and cargo by air has acquired enormous proportions in all developed countries. According to world statistics, almost half plane crashes occurs on the airfield and half occurs in the air at various altitudes.
As the capacity of passenger airliners has increased significantly, the number of victims of air crashes has increased accordingly. When a crashed plane crashes to the ground, residential buildings, industrial buildings, etc. can be destroyed. In this case, there can be victims both on board and on the ground. A particular danger is posed by airplane crashes at nuclear power plants and chemical industry facilities.
In the event of an aircraft crash, the following types of injuries to passengers and crew are noted: injuries and thermal burns, oxygen starvation(in case of depressurization of the aircraft cabin or cabin). Sanitary losses can reach 80-90%.
If an airplane crash occurred on the airport premises, the communications officer on duty immediately reports this to the emergency medical service station and to the medical institution that serves the airport. The EMT teams arriving at the airport provide medical assistance to the victims at the scene of the incident, and also triage them, taking into account the severity of their condition. Then the victims are evacuated by the transport of EMP teams to the airport medical center (lightly injured people are evacuated on their own), where the medical team examines them, provides emergency first aid to those in need, registers patients and determines the order of their evacuation to medical institutions. Evacuation is carried out by ambulance transport, always accompanied by a medical worker (paramedic, nurse).
If the plane crash occurred outside the airport area, then in this case the organization of assistance to the victims will largely depend on local conditions.
However, in any case, after providing first medical aid, the victims must be immediately evacuated from the accident area in order to avoid repeated exposure to damaging factors (fire, explosion, fuel spill, etc.).
The principles of providing medical care to victims outside the airport area are the same as in case of a plane crash in the airport area.
In case of aviation accidents occurring over a sparsely populated (hard-to-reach) territory or over a vast water area, the survival of people largely depends on the preparedness of the crew for such situations, as well as on the speed of search and proper organization help them, since in a deserted area the external environment can be life-threatening (lack of water, food, cold, heat, etc.).
Accidents at fire and explosion hazardous facilities
The main damaging factors of accidents at air defense facilities are:
air shock wave;
fragmentation fields;
thermal radiation from fires;
the effect of toxic substances as combustion products.
The main reasons determining the number of sanitary losses in fires and explosions are:
the size of the fire or the power of the explosion;
character and density of development;
fire resistance of buildings and structures;
weather conditions;
Times of Day;
population density.
As a result of the explosion of gas condensate on the main product pipeline near the Ulu-Telyak railway station in 1989, more than 1000 people were injured - passengers on two trains, which amounted to more than 97% of the number of people on these trains. Moreover, in 38.3% of those affected, the area of burns was from 41 to 60%, and in 10.8% it exceeded 60% of the body surface. Skin burns in combination with burns of the upper respiratory tract noted in 33% of victims. Thermal injuries to the skin, upper respiratory tract and mechanical injuries occurred in almost 17%. Mildly affected people accounted for 3%, moderately severely affected - 16.4%, severely affected - 61.6% and extremely severely affected - 19% of the total number of victims.
With explosions in confined spaces (mines, industrial buildings, etc.), almost all people there may suffer burns, the area of which, in about half, will be from 20 to 60% of the body surface. Thermal lesions of the skin can be combined with burns of the upper respiratory tract in 25%, and in 12% - with mechanical injuries. In addition, approximately 60% of those affected may be poisoned by combustion products.
It can save a person who has fallen into a state of clinical (reversible) death medical intervention. The patient will have only a few minutes before death, so those nearby are obliged to provide him with emergency first aid. Cardiopulmonary resuscitation (CPR) is ideal in this situation. It is a set of measures to restore respiratory function and circulatory systems. Not only rescuers, but also ordinary people nearby can provide assistance. The reason for carrying out resuscitation measures is the inherent clinical death manifestations.
Cardiopulmonary resuscitation is a combination of primary methods saving the patient. Its founder is the famous doctor Peter Safar. He was the first to create the correct algorithm for emergency aid to a victim, which is used by most modern resuscitators.
The implementation of the basic complex for saving a person is necessary when identifying clinical picture characteristic of reversible death. Its symptoms are primary and secondary. The first group refers to the main criteria. This:
- disappearance of the pulse in large vessels (asystole);
- loss of consciousness (coma);
- complete lack of breathing (apnea);
- dilated pupils (mydriasis).
The voiced indicators can be identified by examining the patient:

There are secondary signs varying degrees expressiveness. They help ensure the need for pulmonary-cardiac resuscitation. Acquainted with additional symptoms clinical death can be found below:
- pale skin;
- loss of muscle tone;
- lack of reflexes.
Contraindications
Basic form of cardiopulmonary resuscitation is performed by nearby people in order to save the patient’s life. An extended version of assistance is provided by resuscitators. If the victim has fallen into a state of reversible death due to a long course of pathologies that have depleted the body and cannot be treated, then the effectiveness and expediency of rescue methods will be in question. Usually leads to this terminal stage development oncological diseases, severe deficiency internal organs and other ailments.
There is no point in resuscitating a person if there are visible injuries that are incomparable to life against the background of a clinical picture of characteristic biological death. You can see its signs below:
- post-mortem cooling of the body;
- the appearance of spots on the skin;
- clouding and drying of the cornea;
- the emergence of the phenomenon cat eye»;
- hardening of muscle tissue.
Drying and noticeable clouding of the cornea after death is called the “floating ice” symptom due to appearance. This sign is clearly visible. The "cat's eye" phenomenon is determined by light pressure on the sides eyeball. The pupil contracts sharply and takes the shape of a slit.
The rate at which the body cools depends on the ambient temperature. Indoors, the decrease occurs slowly (no more than 1° per hour), but in a cool environment everything happens much faster.
Cadaveric spots are a consequence of the redistribution of blood after biological death. Initially, they appear on the neck from the side on which the deceased was lying (front on the stomach, back on the back).
Rigor mortis is the hardening of muscles after death. The process begins with the jaw and gradually covers the entire body.
Thus, it makes sense to perform cardiopulmonary resuscitation only in the case of clinical death, which was not provoked by serious degenerative changes. Its biological form is irreversible and has characteristic symptoms, so people nearby will only have to call an ambulance for the team to pick up the body.
Correct procedure
 The American Heart Association regularly provides advice on how to help better effective assistance sick people. Cardiopulmonary resuscitation according to new standards consists of the following stages:
The American Heart Association regularly provides advice on how to help better effective assistance sick people. Cardiopulmonary resuscitation according to new standards consists of the following stages:
- identifying symptoms and calling an ambulance;
- implementation of CPR according to generally accepted standards with an emphasis on indirect massage heart muscle;
- timely implementation of defibrillation;
- use of intensive care methods;
- carrying out complex treatment asystole.
The procedure for performing cardiopulmonary resuscitation is compiled according to the recommendations of the American Heart Association. For convenience, it has been divided into specific phases entitled in English letters"ABCDE". You can see them in the table below:
| Name | Decoding | Meaning | Goals |
|---|---|---|---|
| A | Airway | Restore | Use the Safar method. Try to eliminate life threatening violations. |
| B | Breathing | Carry out artificial ventilation of the lungs | Do artificial respiration. Preferably using an Ambu bag to prevent infection. |
| C | Circulation | Ensuring blood circulation | Perform an indirect massage of the heart muscle. |
| D | Disability | Neurological status | Assess vegetative-trophic, motor and brain functions, as well as sensitivity and meningeal syndrome. Eliminate life-threatening failures. |
| E | Exposure | Appearance | Assess the condition of the skin and mucous membranes. Stop life-threatening disorders. |
The voiced stages of cardiopulmonary resuscitation are compiled for doctors. To ordinary people If you are near the patient, it is enough to carry out the first three procedures while waiting for an ambulance. WITH correct technique implementation can be found in this article. Additionally, pictures and videos found on the Internet or consultations with doctors will help.
For the safety of the victim and the resuscitator, experts have compiled a list of rules and advice regarding the duration of resuscitation measures, their location and other nuances. You can find them below:

Time to make a decision is limited. Brain cells are rapidly dying, so pulmonary-cardiac resuscitation must be carried out immediately. There is only no more than 1 minute to make a diagnosis of “clinical death”. Next, you need to use the standard sequence of actions.
Resuscitation procedures
To a common man without medical education There are only 3 methods available to save the patient’s life. This:
- precordial stroke;
- indirect form of cardiac muscle massage;
- artificial ventilation.
Specialists will have access to defibrillation and direct cardiac massage. The first remedy can be applied by a visiting team of doctors if they have the appropriate equipment, and the second only by doctors intensive care unit. The sound methods are combined with the administration of medications.
 Precordial shock is used as a replacement for a defibrillator. Usually it is used if the incident happened literally before our eyes and no more than 20-30 seconds passed. Algorithm of actions this method next:
Precordial shock is used as a replacement for a defibrillator. Usually it is used if the incident happened literally before our eyes and no more than 20-30 seconds passed. Algorithm of actions this method next:
- If possible, pull the patient onto a stable and durable surface and check for the presence of a pulse wave. If it is absent, you must immediately proceed to the procedure.
- Place two fingers in the center of the chest in the area of the xiphoid process. The blow must be applied slightly above their location with the edge of the other hand, gathered into a fist.
If the pulse cannot be felt, then it is necessary to move on to massage the heart muscle. The method is contraindicated for children whose age does not exceed 8 years, since the child may suffer even more from such a radical method.
Indirect cardiac massage
The indirect form of cardiac muscle massage is compression (squeezing) of the chest. This can be done using the following algorithm:
- Place the patient on a hard surface so that the body does not move during the massage.
- The side where the person performing resuscitation measures will stand is not important. You need to pay attention to the placement of your hands. They should be in the middle of the chest in its lower third.
- Hands should be placed one on top of the other, 3-4 cm above the xiphoid process. Press only with the palm of your hand (fingers do not touch the chest).
- Compression is carried out mainly due to the rescuer’s body weight. It is different for each person, so you need to make sure that the chest sag no deeper than 5 cm. Otherwise, fractures are possible.
- pressure duration 0.5 seconds;
- the interval between presses does not exceed 1 second;
- the number of movements per minute is about 60.
 When performing cardiac massage in children, it is necessary to take into account the following nuances:
When performing cardiac massage in children, it is necessary to take into account the following nuances:
- in newborns, compression is performed with 1 finger;
- in infants, 2 fingers;
- in older children, 1 palm.
If the procedure turns out to be effective, the patient will develop a pulse, the skin will turn pink and the pupillary effect will return. It must be turned on its side to avoid tongue sticking or suffocation by vomit.
Before carrying out the main part of the procedure, you must try the Safar method. It is performed as follows:
- First, you should lay the victim on his back. Then tilt his head back. The maximum result can be achieved by placing one hand under the victim’s neck and the other on the forehead.
- Next, open the patient’s mouth and take a test breath of air. If there is no effect, push his lower jaw forward and down. If in oral cavity If there are objects that cause blockage of the respiratory tract, they should be removed using improvised means (handkerchief, napkin).
If there is no result, you must immediately proceed to artificial ventilation. Without the use of special devices, it is performed according to the instructions below:

To avoid infection of the rescuer or patient, it is advisable to carry out the procedure through a mask or using special devices. Its effectiveness can be increased by combining it with indirect cardiac massage:
- When performing resuscitation measures alone, you should apply 15 pressures on the sternum, and then 2 breaths of air to the patient.
- If two people are involved in the process, then air is injected once every 5 presses.
Direct cardiac massage
The heart muscle is massaged directly only in a hospital setting. Often resort to this method in case of sudden cardiac arrest during surgical intervention. The technique for performing the procedure is given below:
- Doctor opening chest in the region of the heart and begins to rhythmically compress it.
- Blood will begin to flow into the vessels, due to which the functioning of the organ can be restored.
 The essence of defibrillation is the use of a special device (defibrillator), with which doctors apply current to the heart muscle. This radical method is indicated for severe forms arrhythmias (supreventricular and ventricular tachycardias, ventricular fibrillation). They provoke life-threatening disruptions in hemodynamics, which often lead to fatal outcome. If the heart stops, using a defibrillator will not bring any benefit. In this case, other resuscitation methods are used.
The essence of defibrillation is the use of a special device (defibrillator), with which doctors apply current to the heart muscle. This radical method is indicated for severe forms arrhythmias (supreventricular and ventricular tachycardias, ventricular fibrillation). They provoke life-threatening disruptions in hemodynamics, which often lead to fatal outcome. If the heart stops, using a defibrillator will not bring any benefit. In this case, other resuscitation methods are used.
Drug therapy
Doctors administer special medications intravenously or directly into the trachea. Intramuscular injections are ineffective, so they are not carried out. The following medications are most commonly used:
- Adrenaline is the main drug for asystole. It helps start the heart by stimulating the myocardium.
- "Atropine" represents a group of M-cholinergic receptor blockers. The drug helps to release catecholamines from the adrenal glands, which is especially useful in cardiac arrest and severe bradysystole.
- "Sodium bicarbonate" is used if asystole is a consequence of hyperkalemia ( high level potassium) and metabolic acidosis (acid-base imbalance). Especially during a prolonged resuscitation process (over 15 minutes).
Other medications, including antiarrhythmic drugs, are used as appropriate. After the patient’s condition improves, they will be kept under observation in the intensive care unit for a certain period of time.
Consequently, cardiopulmonary resuscitation is a set of measures to recover from the state of clinical death. Among the main methods of providing assistance are artificial respiration and indirect cardiac massage. They can be performed by anyone with minimal training.
Recognizing the signs of respiratory distress and providing timely assistance often prevents other serious complications, such as anaphylactic shock. Respiratory problems require immediate attention or they can lead to death.
Signs of respiratory disorders are shallow, rapid breathing. Despite trying to breathe, the victim cannot inhale enough air or begins to choke, signs of suffocation appear, accompanied by feelings of fear and confusion. The victim may feel dizzy and sometimes clutch his neck.
In any case, when providing assistance, you need to be sure of your own safety, since the victim may exhale toxic substances.
If the victim is breathing, albeit with difficulty, then the heart is beating.
You need to help him sit comfortably, open the window, unbutton his shirt collar, loosen his tie and belt. Ask someone to call an ambulance (if you cannot do it yourself) and make sure that it is called.
If there are witnesses to the incident, you need to interview them about what happened. The victim can confirm their story with a nod of the head or say “yes” or “no”. You need to try to reduce the victim’s anxiety, which also makes breathing difficult, find out what medications help him in this condition (bronchodilators, etc.), while continuing to monitor the signs indicating breathing disorders. You should cover the victim if it is cold outside, move (help him leave) into the shade if it is hot outside.
If it is clear that rapid breathing is caused by emotional arousal, you should ask the victim to relax and breathe slowly. Often this is enough. When the victim stops breathing, he requires artificial lung ventilation (ALV) “mouth to mouth” or “mouth to nose”.
Artificial ventilation.
Remember! Without breathing (i.e. without oxygen supply), the brain can live for 4-6 minutes (Fig. 15.1). When performing artificial pulmonary ventilation (ALV), the exhaled air contains 16% oxygen, which is enough to maintain brain life.
If you don't see, don't hear, don't feel There are no signs of breathing, immediately make two slow exhalations into the victim’s airway through a napkin (handkerchief). Then you need to check for a pulse.
If the victim is not breathing, but has a pulse in the carotid artery, mechanical ventilation should be started: exhale, keep the airways open with the head thrown back and the chin raised (Fig. 15.2). The thrown back head and raised chin not only open the airways, eliminating the retraction of the tongue, but also move the epiglottis, opening the entrance to the trachea.
Rice. 15.1. Time is of the essence for starting resuscitation.
You need to carefully squeeze the victim’s nostrils with your thumb and forefinger, pressing your palm on his forehead. Then, cover the victim’s mouth with your mouth and slowly exhale into it until it is visible that his chest rises (Fig. 15.3). Each breath should last about 1.5 seconds with pauses between your breaths. It is necessary to observe the chest with each breath to be sure that ventilation is actually being carried out. If the chest rise is not visible, the victim's head may not be tilted back enough. You need to throw your head back and try to breathe again. If the chest does not rise, then the airways are blocked by a foreign body that must be removed.


chin lift.
You need to check the pulse after the first two breaths: if there is a pulse, you can continue mechanical ventilation with a frequency of 1 breath every 5 s. When counting “one and”, “two and”, “three and”, “four and”, “five and” 5 seconds will pass. After this, the rescuer must inhale himself and then exhale into the victim. Then continue breathing at a frequency of 1 breath every 5 seconds. Each breath lasts 1.5 seconds. After one minute of mechanical ventilation (about 12 breaths), you need to check the pulse and make sure that the heart is beating. If breathing does not appear, continue mechanical ventilation. Check your pulse every minute.
Remember! Stop mechanical ventilation if:
The victim began to breathe on his own;
The victim’s pulse has disappeared (cardiopulmonary resuscitation must be started);
Other rescuers came to your aid;
An ambulance has arrived and continues mechanical ventilation;
You have exhausted your strength.
A combination of cardiac massage and mechanical ventilation.
Since indirect cardiac massage must be combined with mechanical ventilation, resuscitation measures are best carried out together. One person performs the massage, and the other performs mechanical ventilation, the ventilation ratio (massage should be 1:5. If one person provides assistance, he has to alternate 2 blows of air into the lungs with 15 quick (interval - no more than 1 second) sternum thrusts. Every 1- 2 minutes, it is necessary to interrupt resuscitation for a few seconds (no more than 4-5) to determine the spontaneous pulse that has arisen.
One person performing mechanical ventilation should monitor the effectiveness of resuscitation.
The effectiveness of cardiopulmonary resuscitation is assessed using following criteria:
1. First of all, by the narrowing of the pupils and the appearance of their reaction to light. Constriction of the pupils indicates the flow of oxygenated blood into the patient’s brain. If the pupils remain wide and do not respond to light, with properly performed CPR, one can think of brain death.
2. The appearance of pulse transmission waves on the carotid and femoral arteries with each push, and then spontaneous pulsation.
3. Skin pallor and cyanosis are reduced.
4. Restoration of spontaneous breathing.
In case of successful resuscitation, cardiac massage is carried out until recovery heart rate, mechanical ventilation (minimal) until spontaneous breathing is restored, throwing back the head with opening the mouth and extending lower jaw(or presence of the air duct in the respiratory tract) - until consciousness is restored.
If the pupils remain wide for 30-40 minutes, independent cardiac and respiratory activity is not restored, resuscitation measures are stopped.
TECHNIQUE OF EXTERNAL HEART MASSAGEThe heart is located in the chest cavity between two bone formations: the vertebral bodies at the back and the sternum at the front. When the chest is compressed in a horizontal position of the body to a depth of 4–5 cm, the heart is compressed, while performing its pumping function: it pushes blood into the aorta and pulmonary artery when the chest is compressed and sucks in venous blood when it expands. The effectiveness of external cardiac massage has been proven for a long time. Currently, this method is generally accepted.1. The victim is placed on his back on a hard and level base (floor, ground). 2. The person providing assistance takes a position on the side of the patient, feels the end of the sternum in the epigastric region, and at a distance of 2 transversely located fingers upward along the midline, places the palm of the hand with its widest part. The second palm is placed crosswise on top.3. Without bending your arms, makes strong pressure on the sternum towards the spine to a depth of 4 - 5 cm and releases after a short pause, without lifting your hands from the surface of the chest. It is necessary to repeat these movements with a frequency of at least 60 per 1 min (1 compression per 1 s), since less frequent exposures do not provide sufficient blood circulation. The chest should be compressed with vigorously dosed pressure to cause a pulse wave in the carotid artery. 4. When performing a massage on adults, it is necessary to use not only the strength of the hands, but also apply pressure with the entire body. In children over 5 years old, external cardiac massage is performed with one hand, in infants and newborns - with the tips of the index and middle fingers. The frequency of compression is 100 - 110 per minute. The effectiveness of the massage is judged by the change in color of the skin of the face, the appearance of a pulse in the carotid artery, and the constriction of the pupils. You can stop external heart massage every 2 minutes for only 3 –
5 s to ensure that cardiac activity is restored. If, after stopping the massage, the pulse is not detected and the pupils dilate again, the massage should be continued. Practice shows that external massage even when cardiac activity stops, it restores blood circulation in vital organs (brain, heart). However, the effectiveness of such a massage is ensured only in combination with artificial respiration. The following optimal combinations of the frequency of artificial respiration and cardiac massage are proposed, depending on the number of persons providing assistance.  If assistance is provided by 1 person (Fig. 6), then the ratio of manipulations performed should be 2; 15. For every 2 quick blows of air into the lungs, there should be 15 massage compressions of the sternum. The person providing assistance takes the most comfortable position in relation to the patient, which allows him to perform both revival techniques without changing his position. A roll of rolled up clothing should be placed under the patient’s shoulders so that the head is thrown back and the airways are open. If assistance is provided by 2 people (Fig. 7), then the ratio of techniques should be 1:5. One performs external cardiac massage, the other performs artificial respiration after every 5th compression of the sternum, at the moment of expansion of the chest. If cardiac activity has recovered, the pulse has become clear, the face has turned pink, cardiac massage is stopped, and artificial respiration is continued in the same rhythm until spontaneous breathing is restored. If the victim develops full breathing Constant monitoring should be established for him (until he regains consciousness). It should be remembered that in the absence of consciousness, repeated breathing disorders are possible due to retraction of the tongue and lower jaw.
If assistance is provided by 1 person (Fig. 6), then the ratio of manipulations performed should be 2; 15. For every 2 quick blows of air into the lungs, there should be 15 massage compressions of the sternum. The person providing assistance takes the most comfortable position in relation to the patient, which allows him to perform both revival techniques without changing his position. A roll of rolled up clothing should be placed under the patient’s shoulders so that the head is thrown back and the airways are open. If assistance is provided by 2 people (Fig. 7), then the ratio of techniques should be 1:5. One performs external cardiac massage, the other performs artificial respiration after every 5th compression of the sternum, at the moment of expansion of the chest. If cardiac activity has recovered, the pulse has become clear, the face has turned pink, cardiac massage is stopped, and artificial respiration is continued in the same rhythm until spontaneous breathing is restored. If the victim develops full breathing Constant monitoring should be established for him (until he regains consciousness). It should be remembered that in the absence of consciousness, repeated breathing disorders are possible due to retraction of the tongue and lower jaw.  The issue of stopping resuscitation measures if they are ineffective should be decided by the doctor called to the scene of the incident, or the one providing assistance himself, taking into account precise definition time of cardiac arrest and duration of resuscitation not exceeding the limits of possible revival (until the appearance of obvious signs of death). Errors Observations show that first aid teachers often do not fully demonstrate the technique of maximum extension of the head and do not ensure free passage of the airways. If this mistake is made during the provision of assistance, the blown air may enter the stomach, and the technique used will not give the desired effect. By blowing air it is not always possible to achieve a tightness when covering the mouth or nose of the victim, and part of the volume of the blown air is lost and comes out. Therefore, covering the circumference of the mouth or the nose should be full when blowing air. When performing external cardiac massage, you should correctly choose the location of the palm on the sternum. Displacement of compression (squeezing) upward often leads to a fracture of the sternum, downwards - to a rupture of the stomach, downwards and to the right - to damage to the liver, downwards and to the left - to damage to the spleen, to the left or to the right of the sternum - to a fracture of the ribs. When providing assistance from two persons, performing an external cardiac massage and artificial respiration should be carried out synchronously so that air is blown into the lungs at the moment of relaxation of the chest. When performing external cardiac massage, one should monitor the dynamics of signs of life, especially the pulse in the carotid artery and the size of the pupils. Thus, promptly started artificial respiration and external cardiac massage can not only restore cardiac activity and other temporarily lost functions of the body, but also prolong human life. Currently, many examples of successful cardiopulmonary resuscitation have accumulated, when rescued people regained the ability to enjoy life.
The issue of stopping resuscitation measures if they are ineffective should be decided by the doctor called to the scene of the incident, or the one providing assistance himself, taking into account precise definition time of cardiac arrest and duration of resuscitation not exceeding the limits of possible revival (until the appearance of obvious signs of death). Errors Observations show that first aid teachers often do not fully demonstrate the technique of maximum extension of the head and do not ensure free passage of the airways. If this mistake is made during the provision of assistance, the blown air may enter the stomach, and the technique used will not give the desired effect. By blowing air it is not always possible to achieve a tightness when covering the mouth or nose of the victim, and part of the volume of the blown air is lost and comes out. Therefore, covering the circumference of the mouth or the nose should be full when blowing air. When performing external cardiac massage, you should correctly choose the location of the palm on the sternum. Displacement of compression (squeezing) upward often leads to a fracture of the sternum, downwards - to a rupture of the stomach, downwards and to the right - to damage to the liver, downwards and to the left - to damage to the spleen, to the left or to the right of the sternum - to a fracture of the ribs. When providing assistance from two persons, performing an external cardiac massage and artificial respiration should be carried out synchronously so that air is blown into the lungs at the moment of relaxation of the chest. When performing external cardiac massage, one should monitor the dynamics of signs of life, especially the pulse in the carotid artery and the size of the pupils. Thus, promptly started artificial respiration and external cardiac massage can not only restore cardiac activity and other temporarily lost functions of the body, but also prolong human life. Currently, many examples of successful cardiopulmonary resuscitation have accumulated, when rescued people regained the ability to enjoy life.
Literature:
1. “Fundamentals of resuscitation”, edited by V.A. Negovsky, “Medicine”, Tashkent, 1974.
2. “Basics of resuscitation for nurses", I.V. Remizov, “Phoenix”, 2005.
3. “Disaster Medicine” edited by H.A. Musalatova, Moscow, 2002
4. “Handbook of resuscitation”, edited by I.Z. Klyavzunika, Minsk, 1978