A. I. KIENIA
PHYSIOLOGY
BREATHING
Ministry of Health of the Republic of Belarus
Gomel State Medical Institute
Department of Human Physiology
A. I. KIENIA
doctor of biological sciences, professor
PHYSIOLOGY
BREATHING
Reviewers:
Ruzanov D.Yu., Candidate of Medical Sciences, Head of the Department of Phthisiopulmonology, Gomel State Medical Institute.
Kienya A.I.
K38 Physiology of respiration: Textbook.- Gomel.-2002.- p.
The manual is based on the material of lectures on the section "Physiology of Respiration" of normal physiology, read by the author to students of the medical faculty and the faculty for training specialists for foreign countries.
For students, teachers, graduate students of medical and biological universities and related specialties.
© A. I. Kienya
FOREWORD
This manual is a concise text of lectures on the section "Physiology of Respiration" of normal physiology, read by the author to students of the Gomel State Medical Institute. The material of the manual is presented in accordance with the Program on Normal Physiology for students of the Medical and Preventive Faculty of Higher Medical educational institutions No. 08-14/5941, approved by the Ministry of Health of the Republic of Belarus on September 3, 1997
The manual presents modern information about respiration as a system that serves metabolic processes in the body. The main stages of breathing, the mechanisms of respiratory movements (inhalation and exhalation), the role of negative pressure in pleural cavity, lung ventilation and lung volumes and capacities, anatomical and functional dead space, their physiological significance, processes of gas exchange in the lungs, transport of gases (O 2 and CO 2) by blood, factors affecting the formation of hemoglobin compounds with O 2 and CO 2 and their dissociation, gas exchange between blood and tissues. The neurohumoral mechanisms of respiration regulation are considered, the structural organization of the respiratory center, the role of the gas composition and various receptors in the regulation of respiration are analyzed. Describes the features of breathing in different conditions. The mechanism and theories of the emergence of the first breath of a newborn are outlined. Are being considered age features breathing.
The age-related features of the respiratory system are considered separately.
At the end of the manual, the main constants of the blood of a healthy person are presented.
At the same time, the author is aware that in this manual, due to its small volume, it was not possible to cover in detail all aspects of the physiology of respiration, therefore, some of them are presented in a concise form, more detailed information about which can be found in the literature sources cited at the end of the manual.
The author will be very grateful to everyone who considers it possible to express their critical comments about the proposed manual, which will be perceived as an expression of a desire to help improve it in a subsequent reprint.
EXTERNAL RESPIRATORY
The formation of energy necessary to ensure the vital activity of the human body occurs on the basis of oxidative processes. Their implementation requires a constant influx of O 2 from the external environment and the continuous removal of CO 2 from it, which is formed in the tissues as a result of metabolism.
The set of processes that ensure the entry of O 2 into the body, its delivery and consumption to tissues, and the release of the end product of respiration of CO 2 into external environment is called respiration. This is a physiological system.
A person can live without:
food for less than a month
water - 10 days,
Oxygen - 4-7 minutes (no stock). In this case, first of all, the death of nerve cells occurs.
The complex process of gas exchange with the environment consists of a number of successive processes.
External respiration (pulmonary):
1. Exchange of gases between lung air and atmospheric air (pulmonary ventilation).
2. The exchange of gases between the lung air and the blood of the capillaries of the pulmonary circulation.
Internal:
3. Transport of O 2 and CO 2 by blood.
4. The exchange of gases between blood and cells (tissue respiration), that is, the consumption of O 2 and the release of CO 2 in the process of metabolism.
Function external respiration and the renewal of the gas composition of the blood in humans is performed by the airways and lungs.
Respiratory tract: nasal and oral cavity, larynx, trachea, bronchi, bronchioles, alveolar passages. The human trachea is approximately 15 cm long and is divided into two bronchi: right and left. They branch into smaller bronchi, and the latter - into bronchioles (up to 0.3 - 0.5 mm in diameter). The total number of bronchioles is approximately 250 million. The bronchiole branches into alveolar passages, and they end in blind sacs - alveoli. The alveoli are internally lined with respiratory epithelium. The surface area of all alveoli in humans reaches 50-90 m 2 .
Each alveolus is surrounded by a dense network of blood capillaries.
There are two types of cells in the mucous membrane of the respiratory tract:
a) ciliated epithelial cells;
b) secretory cells.
Outside, the lungs are covered with a thin, serous membrane - the pleura.
IN right lung There are three lobes: upper (apical), middle (cardiac), lower (diaphragmatic). The left lung has two lobes (upper and lower).
For the implementation of gas exchange processes in the structure of the lungs, there are a number of adaptive features:
1. The presence of air and blood channels, separated from each other by the thinnest film, consisting of a double layer - the alveolus itself and the capillary (air and blood separation - thickness 0.004 mm). Diffusion of gases occurs through this air-blood barrier.
2. An extensive respiratory area of the lungs of 50-90 m 2 is approximately equal to an increase in the surface of the body (1.7 m 2 0) by several tens of times.
3. The presence of a special - a small circle of blood circulation, specifically performing an oxidative function (functional circle). A small circle of a blood particle passes in 5 seconds, and the time of its contact with the wall of the alveoli is only 0.25 - 0.7 seconds.
4. The presence of elastic tissue in the lungs, which contributes to the expansion and collapse of the lungs during inhalation and exhalation. The lungs are in a state of elastic tension.
5. The presence in the airways of the supporting cartilaginous tissue in the form of cartilaginous bronchi. This prevents the airways from collapsing and promotes quick and easy air passage.
Breathing movements
The ventilation of the alveoli, necessary for gas exchange, is carried out due to the alternation of inhalation (inspiration), exhalation (expiration). When you inhale, air saturated with O 2 enters the alveoli. When exhaling, air is removed from them, poor in O 2, but richer in CO 2. The inspiratory phase followed by the expiratory phase is respiratory cycle.
The movement of air is due to the alternate increase and decrease in volume chest.
The mechanism of inhalation (inspiration).
Enlargement of the chest cavity in the vertical, sagittal, frontal planes. This is ensured by: raising the ribs and flattening (lowering) the diaphragm.
Rib movement. The ribs form mobile connections with the bodies and transverse processes of the vertebrae. The axis of rotation of the ribs passes through these two points. The axis of rotation of the upper ribs is located almost horizontally, therefore, when the ribs are raised, the size of the chest increases in the anteroposterior direction. The axis of rotation of the lower ribs is more sagittal. Therefore, when the ribs are raised, the volume of the chest increases laterally.
Since the movement of the lower ribs has a greater effect on the volume of the chest, the lower lobes of the lung are better ventilated than the tops.
Raising the ribs occurs due to the contraction of the inspiratory muscles. These include: external intercostal, internal intercartilaginous muscles. Their muscle fibers are oriented in such a way that their point of attachment to the lower rib is located further from the center of rotation than the point of attachment to the overlying rib. Their direction: behind, above, forward and down.
As a result, the chest increases in volume.
In a healthy young man, the difference between the circumference of the chest in the position of inhalation and exhalation is 7-10 cm, in women it is 5-8 cm. With forced breathing, auxiliary inspiratory muscles are connected:
- large and small chest;
· - stairs;
- sternocleidomastoid;
- (partially) serrated;
- trapezoidal, etc.
Auxiliary devices are connected when pulmonary ventilation exceeds 50 l / min.
Diaphragm movement. The diaphragm consists of a tendon center and muscle fibers extending from this center in all directions and are attached to the opening of the chest. It has the shape of a dome, protruding into the chest cavity. When exhaling, it is adjacent to the inner wall of the chest for approximately 3 ribs. When you inhale, the diaphragm flattens as a result of contraction of its muscle fibers. At the same time, it moves away from the inner surface of the chest and the costophrenic sinuses open.
Innervation of the diaphragm - phrenic nerves from C 3 -C 5. Unilateral transection of the phrenic nerve on the same side, the diaphragm is strongly pulled into the chest cavity under the pressure of the viscera and the traction of the lungs. The movement of the lower parts of the lungs is limited. So inspiration is active Act.
Mechanism of exhalation (expiration) provided through:
Heaviness of the chest.
Elasticity of costal cartilages.
lung elasticity.
The pressure of the abdominal organs on the diaphragm.
At rest, exhalation occurs passively.
In forced breathing, expiratory muscles are taken: internal intercostal muscles (their direction is from above, back, front, down) and auxiliary expiratory muscles: muscles that flex the spine, abdominal muscles (oblique, straight, transverse). When the latter contract, the abdominal organs put pressure on the relaxed diaphragm and it protrudes into the chest cavity.
Breath types. Depending mainly due to which component (raising the ribs or the diaphragm) the volume of the chest increases, 3 types of breathing are distinguished:
- thoracic (costal);
- abdominal;
- mixed.
To a greater extent, the type of breathing depends on age (the mobility of the chest increases), clothing (tight corsets, swaddling), profession (for people engaged in physical labor, the abdominal type of breathing increases). Abdominal breathing is difficult recent months pregnancy, and then breastfeeding is additionally included.
The most effective abdominal type of breathing:
- deeper lung ventilation;
- facilitates the return of venous blood to the heart.
The abdominal type of breathing prevails among manual workers, climbers, singers, etc. After birth, the child first establishes the abdominal type of breathing, and later - by the age of 7 - chest.
Pressure in the pleural cavity and its change during breathing.
The lungs are covered with a visceral pleura, and the film of the chest cavity is covered with a parietal pleura. Between them contains a serous fluid. They fit tightly to each other (slit 5-10 microns) and slide relative to each other. This sliding is necessary so that the lungs can follow the complex changes in the chest without deforming. With inflammation (pleurisy, adhesions), the ventilation of the corresponding sections of the lungs decreases.
If you insert a needle into the pleural cavity and connect it to a water pressure gauge, it turns out that the pressure in it:
when inhaling - by 6-8 cm H 2 O
· when exhaling - 3-5 cm H 2 O below atmospheric.
This difference between intrapleural and atmospheric pressure is commonly referred to as pleural pressure.
Negative pressure in the pleural cavity is due to the elastic recoil of the lungs, i.e. the tendency of the lungs to collapse.
When inhaling, an increase in the chest cavity leads to an increase in negative pressure in the pleural cavity, i.e. transpulmonary pressure increases, leading to the expansion of the lungs (demonstration using the Donders apparatus).
When the inspiratory muscles relax, the transpulmonary pressure decreases and the lungs collapse due to elasticity.
If a small amount of air is introduced into the pleural cavity, it will be absorbed, because in the blood of small veins of the pulmonary circulation, the tension of dissolved gases is less than in the atmosphere.
The accumulation of fluid in the pleural cavity is prevented by the lower oncotic pressure of the pleural fluid (less proteins) than in plasma. The decrease in hydrostatic pressure in the pulmonary circulation is also important.
The change in pressure in the pleural cavity can be measured directly (but can be damaged lung tissue). Therefore, it is better to measure it by introducing a 10 cm long canister into the esophagus (into the chest part). The walls of the esophagus are very pliable.
The elastic recoil of the lungs is due to 3 factors:
1. Surface tension of the liquid film covering the inner surface of the alveoli.
2. The elasticity of the tissue of the walls of the alveoli (they contain elastic fibers).
3. The tone of the bronchial muscles.
On any interface between air and liquid, intermolecular cohesion forces act, tending to reduce the size of this surface (surface tension forces). Under the influence of these forces, the alveoli tend to shrink. Surface tension forces create 2/3 of the elastic recoil of the lungs. The surface tension of the alveoli is 10 times less than theoretically calculated for the corresponding water surface.
If the inner surface of the alveolus were covered aqueous solution, then the surface tension should have been 5-8 times greater. Under these conditions, there would be a collapse of the alveoli (atelectasis). But that doesn't happen.
This means that in the alveolar fluid on the inner surface of the alveoli there are substances that reduce surface tension, i.e., surfactants. Their molecules are strongly attracted to each other, but have a weak relationship with the liquid, as a result of which they gather on the surface and thereby reduce the surface tension.
Such substances are called surface active substances(surfactants), whose role in this case perform the so-called surfactants. They are lipids and proteins. Formed by special cells of the alveoli - type II pneumocytes. The lining has a thickness of 20-100 nm. But lecithin derivatives have the highest surface activity of the components of this mixture.
With a decrease in the size of the alveoli. surfactant molecules approach each other, their density per unit surface is greater and the surface tension decreases - the alveolus does not collapse.
With an increase (expansion) of the alveoli, their surface tension increases, since the density of the surfactant per unit surface decreases. This enhances the elastic recoil of the lungs.
In the process of breathing amplification respiratory muscles is spent on overcoming not only the elastic resistance of the lungs and chest tissues, but also on overcoming the inelastic resistance to gas flow in the airways, which depends on their lumen.
Violation of the formation of surfactants leads to the collapse of a large number of alveoli - atelectasis - lack of ventilation of large areas of the lungs.
In newborns, surfactants are needed to expand the lungs during the first breaths.
There is a disease of newborns, in which the surface of the alveoli is covered with fibrin precipitate (healin membranes), which reduces the activity of surfactants - reduced. This leads to incomplete expansion of the lungs and severe violation gas exchange.
When air enters (pneumothorax) into the pleural cavity (through the damaged chest wall or lungs) due to the elasticity of the lungs - they collapse and are pressed to the root, occupying 1/3 of their volume.
With unilateral pneumothorax, the lung on the uninjured side can provide sufficient blood saturation with O 2 and removal of CO 2 (at rest). With double-sided - if not produced artificial ventilation lungs, or sealing of the pleural cavity - to death.
Unilateral pneumothorax is sometimes used for therapeutic purposes: the introduction of air into the pleural cavity to treat tuberculosis (cavities).
The lungs and walls of the chest cavity are covered with a serous membrane - the pleura, consisting of visceral and parietal sheets. Between the sheets of the pleura there is a closed slit-like space containing serous fluid - the pleural cavity.
Atmospheric pressure, acting on the inner walls of the alveoli through the airways, stretches the tissue of the lungs and presses the visceral sheet to the parietal, i.e. the lungs are constantly in a stretched state. With an increase in the volume of the chest as a result of contraction of the inspiratory muscles, the parietal sheet will follow the chest, this will lead to a decrease in pressure in the pleural space, so the visceral sheet, and with it the lungs, will follow the parietal sheet. The pressure in the lungs will become lower than atmospheric pressure, and air will flow into the lungs - inhalation occurs.
The pressure in the pleural cavity is lower than atmospheric pressure, so pleural pressure is called negative, conditionally accepting Atmosphere pressure for zero. The more the lungs are stretched, the higher their elastic recoil becomes and the lower the pressure in the pleural cavity drops. The value of negative pressure in the pleural cavity is equal to: by the end of a quiet breath - 5-7 mm Hg; by the end of a maximum breath - 15-20 mm Hg; by the end of a quiet exhalation - 2-3 mm Hg, by the end of maximum exhalation - 1-2 mm Hg.
Negative pressure in the pleural cavity is due to the so-called elastic recoil of the lungs- the force with which the lungs constantly strive to reduce their volume.
The elastic recoil of the lungs is due to three factors:
1) the presence in the walls of the alveoli of a large number of elastic fibers;
2) the tone of the bronchial muscles;
3) surface tension of the liquid film covering the walls of the alveoli.
The substance that covers the inner surface of the alveoli is called a surfactant (Fig. 5).
Rice. 5. Surfactant. Section of the alveolar septum with accumulation of surfactant.
Surfactant- this is a surfactant (a film that consists of phospholipids (90-95%), four proteins specific to it, as well as a small amount of carbon hydrate), is formed by special type II alveolar-pneumocyte cells. Its half-life is 12-16 hours.
Surfactant Functions:
when inhaling, it protects the alveoli from overstretching due to the fact that the surfactant molecules are located far from each other, which is accompanied by an increase in the surface tension;
when exhaling, it protects the alveoli from falling: the surfactant molecules are located close to each other, as a result of which the surface tension decreases;
creates the possibility of straightening the lungs at the first breath of the newborn;
influences the rate of diffusion of gases between alveolar air and blood;
regulates the intensity of evaporation of water from the alveolar surface;
Has bacteriostatic activity;
It has anti-edematous (reduces sweating of fluid from the blood into the alveoli) and antioxidant effect (protects the walls of the alveoli from the damaging effects of oxidants and peroxides).
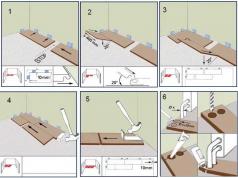
Studying the mechanism of lung volume change using the Donders model
Physiological experiment
The change in lung volume occurs passively, due to changes in the volume of the chest cavity and pressure fluctuations in the pleural space and inside the lungs. The mechanism of change in lung volume during respiration can be demonstrated using the Donders model (Fig. 6), which is a glass tank with a rubber bottom. The top opening of the tank is closed with a cork through which a glass tube is passed. At the end of the tube placed inside the tank, the lungs are attached to the trachea. Through the outer end of the tube, the lung cavity communicates with atmospheric air. When the rubber bottom is pulled down, the volume of the reservoir increases, and the pressure in the reservoir becomes lower than atmospheric pressure, which leads to an increase in lung volume.
The lungs are located in a geometrically closed cavity formed by the chest wall and the diaphragm. From the inside, the chest cavity is lined with a pleura, consisting of two sheets. One sheet is adjacent to the chest, the other - to the lungs. Between the sheets there is a slit-like space, or pleural cavity, filled with pleural fluid.
The chest in the womb and after birth grows faster than the lungs. In addition, the pleural sheets have a large suction capacity. Therefore, a negative pressure is established in the pleural cavity. So, in the alveoli of the lungs, the pressure is equal to atmospheric - 760, and in the pleural cavity - 745-754 mm Hg. Art. These 10-30 mm provide the expansion of the lungs. If the chest wall is pierced so that air enters the pleural cavity, the lungs immediately collapse (atelectasis). This will happen because the pressure atmospheric air on the outer and inner surface of the lungs will be equal.
The lungs in the pleural cavity are always in a somewhat stretched state, but during inhalation their stretch increases sharply, and decreases during exhalation. This phenomenon is well demonstrated by the model proposed by Donders. If you pick up a bottle that corresponds in volume to the size of the lungs, after placing them in this bottle, and instead of the bottom, stretch the rubber film that acts as a diaphragm, then the lungs will expand with each retraction of the rubber bottom. Accordingly, the value of the negative pressure inside the bottle will change.
Negative pressure can be measured by inserting an injection needle connected to a mercury manometer into the pleural space. In large animals, it reaches 30-35 mm Hg during inspiration, and decreases to 8-12 mm Hg during exhalation. Art. Pressure fluctuations during inhalation and exhalation affect the movement of blood through the veins located in the chest cavity. Since the walls of the veins are easily extensible, the negative pressure is transmitted to them, which contributes to the expansion of the veins, their blood filling and the return of venous blood to the right atrium, while inhaling blood flow to the heart increases.
Types of respiration. In animals, three types of respiration are distinguished: costal, or thoracic, - when inhaling, contraction of the external intercostal muscles predominates; diaphragmatic, or abdominal, - the expansion of the chest occurs mainly due to the contraction of the diaphragm; eebero-abdominal - inspiration is provided equally by the intercostal muscles, diaphragm and abdominal muscles. The last type of breathing is characteristic of farm animals. A change in the type of breathing may indicate a disease of the chest or abdominal organs. For example, in case of diseases of the abdominal organs, the costal type of breathing predominates, since the animal protects diseased organs.
Vital and total lung capacity. At rest large dogs and sheep exhale an average of 0.3-0.5, horses
5-6 liters of air. This volume is called breathing air. In excess of this volume, dogs and sheep can inhale another 0.5-1, and horses - 10-12 liters - extra air. After a normal exhalation, animals can exhale approximately the same amount of air - reserve air. Thus, during normal, shallow breathing in animals, the chest does not expand to maximum limit, but is at some optimal level, if necessary, its volume can be increased due to the maximum contraction of the muscles of the inspirators. Respiratory, additional and reserve air volumes are vital capacity of the lungs. In dogs it is 1.5 -3 l, in horses - 26-30, in large cattle- 30-35 liters of air. At maximum exhalation, there is still some air left in the lungs, this volume is called residual air. The vital capacity of the lungs and the residual air are total lung capacity. Value vital capacity lungs can significantly decrease in some diseases, which leads to disruption of gas exchange.
The determination of the vital capacity of the lungs has great importance to clarify physiological state body in normal and pathological conditions. It can be determined using a special apparatus called a water spirometer (Spiro 1-B apparatus). Unfortunately, these methods are difficult to apply in a production environment. In laboratory animals, the vital capacity is determined under anesthesia, by inhaling a mixture with a high content of CO2. The maximum exhalation approximately corresponds to the vital capacity of the lungs. Vital capacity varies depending on age, productivity, breed and other factors.
Pulmonary ventilation. After a quiet expiration, reserve, or residual, air remains in the lungs, also called alveolar air. About 70% of the inhaled air directly enters the lungs, the remaining 25-30% do not take part in gas exchange, since it remains in the upper respiratory tract. The volume of alveolar air in horses is 22 liters. Since, during calm breathing, the horse inhales 5 liters of air, of which only 70%, or 3.5 liters, enters the alveoli, then with each breath in the alveoli, only one-half of the air is ventilated (3.5:22). The ratio of inhaled air to alveolar called coefficient of pulmonary ventilation, and the amount of air passing through the lungs in 1 minute - minute volume of lung ventilation. Minute volume is a variable value, depending on the respiratory rate, vital capacity of the lungs, the intensity of work, the nature of the diet, pathological condition lungs and other factors.
Airways (larynx, trachea, bronchi, bronchioles) are not directly involved in gas exchange, so they are called harmful space. However, they are of great importance in the process of respiration. In the mucous membrane of the nasal passages and upper respiratory tract there are serous-mucous cells and ciliated epithelium. The mucus traps dust and moistens the airways. Ciliated epithelium with the movements of its hairs, it helps to remove mucus with particles of dust, sand and other mechanical impurities into the nasopharynx, from where it is ejected. In the upper respiratory tract there are many sensitive receptors, the irritation of which causes protective reflexes, such as coughing, sneezing, snorting. These reflexes contribute to the removal of particles of dust, food, microbes, toxic substances from the bronchi that are dangerous to the body. In addition, due to the abundant blood supply to the mucous membrane of the nasal passages, larynx, trachea, the inhaled air is warmed.
The volume of pulmonary ventilation is slightly less than the amount of blood flowing through the pulmonary circulation per unit time. In the region of the tops of the lungs, the alveoli are ventilated less efficiently than at the base adjacent to the diaphragm. Therefore, in the region of the tops of the lungs, ventilation relatively predominates over blood flow. The presence of veno-arterial anastomoses and a reduced ratio of ventilation to blood flow in certain parts of the lungs are the main cause of lower oxygen tension and higher carbon dioxide tension in arterial blood compared to the partial pressure of these gases in the alveolar air.
The composition of inhaled, exhaled and alveolar air. Atmospheric air contains 20.82% oxygen, 0.03% carbon dioxide and 79.03% nitrogen. The air in livestock buildings usually contains more carbon dioxide, water vapor, ammonia, hydrogen sulfide, etc. The amount of oxygen may be less than in atmospheric air.
Exhaled air contains an average of 16.3% oxygen, 4% carbon dioxide, 79.7% nitrogen (these figures are given in terms of dry air, that is, excluding water vapor, which saturated the exhaled air). The composition of the exhaled air is not constant and depends on the intensity of metabolism, the volume of pulmonary ventilation, ambient air temperature, etc.
The alveolar air differs from the exhaled air by a high content of carbon dioxide - 5.62% and less oxygen - an average of 14.2-14.6, nitrogen - 80.48%. Exhaled air contains air not only from the alveoli, but also from the “harmful space”, where it has the same composition as atmospheric air.
Nitrogen does not participate in gas exchange, but its percentage in inhaled air is somewhat lower than in exhaled and alveolar air. This is because the volume of exhaled air is slightly less than that of inhaled air.
Maximum allowable concentration of carbon dioxide in barnyards, stables, calves - 0.25%; but already 1% C 0 2 causes noticeable shortness of breath, and pulmonary ventilation increases by 20%. The content of carbon dioxide above 10% leads to death.
BREATHING - a set of processes that ensure the consumption of oxygen (O2) by the body and the release of carbon dioxide (CO2)
STAGES OF BREATHING:
1. External respiration or ventilation of the lungs - the exchange of gases between atmospheric and alveolar air
2. The exchange of gases between the alveolar air and the blood of the capillaries of the pulmonary circulation
3. Transport of gases by blood (O 2 and CO 2)
4. The exchange of gases in tissues between the blood of the capillaries of the systemic circulation and tissue cells
5. Tissue, or internal, respiration - the process of absorption of O 2 by tissues and the release of CO 2 (redox reactions in mitochondria with the formation of ATP)
RESPIRATORY SYSTEM
A set of organs that supply the body with oxygen, remove carbon dioxide and release the energy necessary for all forms of life
FUNCTIONS OF THE RESPIRATORY SYSTEM:
Ø Providing the body with oxygen and using it in redox processes
Ø Formation and excretion of excess carbon dioxide from the body
Ø Oxidation (decomposition) organic compounds with energy release
Ø Isolation of volatile metabolic products (water vapor (500 ml per day), alcohol, ammonia, etc.)
Processes underlying the execution of functions:
a) ventilation (ventilation)
b) gas exchange
STRUCTURE OF THE RESPIRATORY SYSTEM

Rice. 12.1. Structure respiratory system
1 - Nasal passage
2 - Concha
3 - Frontal sinus
4 - Sphenoid sinus
5 - Throat
6 - Larynx
7 - Trachea
8 - Left bronchus
9 - Right bronchus
10 - Left bronchial tree
11 - Right bronchial tree
12 - Left lung
13 - Right lung
14 - Diaphragm
16 - Esophagus
17 - Ribs
18 - Sternum
19 - Clavicle
the organ of smell, as well as the external opening of the respiratory tract: serves to warm and purify the inhaled air
NOSE CAVITY
The initial section of the respiratory tract and at the same time the organ of smell. It stretches from the nostrils to the pharynx, divided by a partition into two halves, which are in front through nostrils communicate with the atmosphere, and behind with the help of choan- with nasopharynx

Rice. 12.2. The structure of the nasal cavity
Larynx
a piece of breathing tube that connects the pharynx to the trachea. Located at the level of IV-VI cervical vertebrae. It is an inlet that protects the lungs. The vocal cords are located in the larynx. Behind the larynx is the pharynx, with which it communicates with its top hole. Below the larynx passes into the trachea

Rice. 12.3. The structure of the larynx
Glottis- the gap between the right and left vocal folds. When the position of the cartilage changes, under the action of the muscles of the larynx, the width of the glottis and the tension of the vocal cords can change. Exhaled air vibrates the vocal cords ® sounds occur
Trachea
a tube that communicates with the larynx at the top and ends at the bottom with a division ( bifurcation ) on the two main bronchi

Rice. 12.4. Main airways
The inhaled air passes through the larynx into the trachea. From here it is divided into two streams, each of which goes to its own lung through an extensive bronchial system.
BRONCHI
tubular formations representing the branches of the trachea. Depart from the trachea almost at a right angle and go to the gates of the lungs
Right bronchus wider but shorter left and is, as it were, a continuation of the trachea
The bronchi are similar in structure to the trachea; they are very flexible due to the cartilaginous rings in the walls and are lined with respiratory epithelium. The connective tissue base is rich in elastic fibers that can change the diameter of the bronchus
main bronchi(first order) are divided into equity (second order): three in the right lung and two in the left - each goes to its share. Then they are divided into smaller ones, going into their segments - segmental (third order) that continue to divide, forming "bronchial tree" lung
BRONCHIAL TREE- the bronchial system, through which air from the trachea enters the lungs; includes main, lobar, segmental, subsegmental (9-10 generations) bronchi, as well as bronchioles (lobular, terminal and respiratory)
Inside the bronchopulmonary segments, the bronchi sequentially divide up to 23 times until they end in a dead end of the alveolar sacs.

Bronchioles(airway diameter less than 1 mm) divide to form terminal (terminal) bronchioles, which are divided into the thinnest short airways - respiratory bronchioles, passing into alveolar passages, on the walls of which there are bubbles - alveoli (air sacs). The main part of the alveoli is concentrated in clusters at the ends of the alveolar ducts, which are formed during the division of the respiratory bronchioles.
Rice. 12.5. lower respiratory tract

Rice. 12.6. Airway, gas exchange area and their volumes after a quiet exhalation
Functions of the airways:
1. Gas exchange - delivery of atmospheric air to gas exchange area and conduction of the gas mixture from the lungs to the atmosphere
2. Non-gas exchange:
§ Purification of air from dust, microorganisms. Protective respiratory reflexes(coughing, sneezing).
§ Humidification of the inhaled air
§ Warming of the inhaled air (at the level of the 10th generation up to 37 0 С
§ Reception (perception) of olfactory, temperature, mechanical stimuli
§ Participation in the processes of thermoregulation of the body (heat production, heat evaporation, convection)
§ They are a peripheral apparatus for generating sounds
acinus
structural unit lung (up to 300 thousand), in which gas exchange occurs between the blood in the capillaries of the lung and the air filling the pulmonary alveoli. It is a complex from the beginning of the respiratory bronchiole, in appearance resembling a bunch of grapes
The acinus includes 15-20 alveoli, in the pulmonary lobule - 12-18 acini. Lobes of the lung are made up of lobules

Rice. 12.7. Pulmonary acinus
Alveoli(in the lungs of an adult 300 million, their total surface area is 140 m 2) - open vesicles with very thin walls, the inner surface of which is lined with a single-layer squamous epithelium lying on the main membrane, to which the entwining alveoli are adjacent blood capillaries which, together with epithelial cells, form a barrier between blood and air (air barrier) 0.5 µm thick, which does not interfere with the exchange of gases and the release of water vapor
found in the alveoli:
§ macrophages(protective cells) that absorb foreign particles that enter the respiratory tract
§ pneumocytes-cells that secrete surfactant

Rice. 12.8. Ultrastructure of the alveoli
SURFACTANT- a lung surfactant containing phospholipids (in particular lecithin), triglycerides, cholesterol, proteins and carbohydrates and forming a 50 nm thick layer inside the alveoli, alveolar ducts, sacs, bronchioles
Surfactant value:
§ Reduces the surface tension of the liquid covering the alveoli (almost 10 times) ® facilitates inhalation and prevents atelectasis (sticking together) of the alveoli during exhalation.
§ Facilitates the diffusion of oxygen from the alveoli into the blood due to the good solubility of oxygen in it.
§ Performs a protective role: 1) has bacteriostatic activity; 2) protects the walls of the alveoli from the damaging effects of oxidizing agents and peroxides; 3) provides return transport of dust and microbes along the airway; 4) reduces the permeability of the lung membrane, which is the prevention of the development of pulmonary edema due to a decrease in the sweating of fluid from the blood into the alveoli
LUNGS
The right and left lungs are two separate objects located in the chest cavity on either side of the heart; covered with a serous membrane pleura, which forms around them two closed pleural sac. They have an irregular conical shape with a base facing the diaphragm and an apex protruding 2-3 cm above the collarbone in the neck

Rice. 12.10. Segmental structure of the lungs.
1 - apical segment; 2 - posterior segment; 3 - anterior segment; 4 - lateral segment ( right lung) and upper reed segment (left lung); 5 - medial segment (right lung) and lower reed segment (left lung); 6 - apical segment of the lower lobe; 7 - basal medial segment; 8 - basal anterior segment; 9 - basal lateral segment; 10 - basal posterior segment
ELASTICITY OF THE LUNGS
the ability to respond to a load with an increase in voltage, which includes:
§ elasticity- the ability to restore its shape and volume after the termination of action external forces causing deformation
§ rigidity– the ability to resist further deformation when the elastic limit is exceeded
Reasons for the elastic properties of the lungs:
§ elastic fiber tension lung parenchyma
§ surface tension fluid lining the alveoli - created by surfactant
§ blood filling of the lungs (the higher the blood filling, the less elasticity
Extensibility- the property is the opposite of elasticity, associated with the presence of elastic and collagen fibers that form a spiral network around the alveoli
Plastic- property opposite to rigidity
LUNG FUNCTIONS
gas exchange- enrichment of the blood with oxygen used by the tissues of the body, and the removal of carbon dioxide from it: achieved through pulmonary circulation. Blood from body organs returns to right side hearts and pulmonary arteries goes to the lungs
Non-gas exchange:
Ø Z protective - the formation of antibodies, phagocytosis by alveolar phagocytes, the production of lysozyme, interferon, lactoferrin, immunoglobulins; microbes, aggregates of fat cells, thromboemboli are retained and destroyed in the capillaries
Ø Participation in the processes of thermoregulation
Ø Participation in the selection processes - removal of CO 2 , water (about 0.5 l / day) and some volatile substances: ethanol, ether, acetone nitrous oxide, ethyl mercaptan
Ø BAS inactivation - more than 80% of bradykinin introduced into the pulmonary circulation is destroyed during a single passage of blood through the lung, angiotensin I is converted into angiotensin II under the influence of angiotensinase; 90-95% of prostaglandins of groups E and P are inactivated
Ø Participation in the development of biologically active substances -heparin, thromboxane B2, prostaglandins, thromboplastin, coagulation factors VII and VIII, histamine, serotonin
Ø They act as an air reservoir for vocalization
EXTERNAL BREATHING
The process of ventilation of the lungs, providing gas exchange between the body and the environment. It is carried out due to the presence of the respiratory center, its afferent and efferent systems, respiratory muscles. Estimated by the ratio alveolar ventilation to minute volume. To characterize external respiration, static and dynamic indicators of external respiration are used.
Respiratory cycle- rhythmically repeating change in the state of the respiratory center and executive bodies breathing

Rice. 12.11. respiratory muscles
Diaphragm- a flat muscle that separates the thoracic cavity from the abdominal cavity. It forms two domes, left and right, directed upwards with bulges, between which there is a small cavity for the heart. It has several holes through which very important structures of the body pass from the chest region to the abdominal region. By contracting, it increases the volume of the chest cavity and provides air flow to the lungs.

Rice. 12.12. Diaphragm position during inhalation and exhalation
pressure in the pleural cavity
physical quantity characterizing the state of the contents of the pleural cavity. This is the amount by which the pressure in the pleural cavity is below atmospheric ( negative pressure); with calm breathing, it is 4 mm Hg. Art. at the end of exhalation and 8 mm Hg. Art. at the end of the breath. Created by surface tension forces and elastic recoil of the lung

Rice. 12.13. Pressure changes during inhalation and exhalation
INHALE(inspiration) - the physiological act of filling the lungs with atmospheric air. It is carried out due to the active activity of the respiratory center and the respiratory muscles, which increases the volume of the chest, resulting in a decrease in pressure in the pleural cavity and in the alveoli, which leads to the flow of air environment in the trachea, bronchi and respiratory zones of the lung. Occurs without the active participation of the lungs, since there are no contractile elements in them
EXHALATION(expiration) - the physiological act of removing from the lung part of the air that takes part in gas exchange. First, the air of the anatomical and physiological dead space, which differs little from atmospheric air, is removed, then the alveolar air enriched with CO 2 and poor with O 2 as a result of gas exchange. At rest, the process is passive. It is carried out without the expenditure of muscle energy, due to the elastic traction of the lung, chest, gravitational forces and relaxation of the respiratory muscles
During forced breathing, the depth of exhalation is increased by abdominal muscles and internal intercostal. The abdominal muscles are squeezing abdominal cavity in front and increase the rise of the diaphragm. The internal intercostal muscles move the ribs down and thereby reduce the cross section of the chest cavity, and hence its volume.
At the birth of a child, the lungs do not yet contain air and their own volume coincides with the volume of the chest cavity. Contracted on first breath skeletal muscles inspiration, the volume of the chest cavity increases.
The pressure on the lungs outside from the side of the ore cage decreases compared to atmospheric pressure. Due to this difference, air freely enters the lungs, stretching them and pressing outer surface lungs to the inner surface of the chest and to the diaphragm. At the same time, the lungs are stretched, having elasticity, counteracting stretching. As a result, at the height of inhalation, the lungs exert on the chest from the inside no longer atmospheric pressure, but less by the amount of elastic recoil of the lungs.
After the baby is born, the chest grows faster than lung tissue. Because
the lungs are under the action of the same forces that stretched them during the first breath, they completely fill the chest both during inhalation and during exhalation, being constantly in a stretched state. As a result, the pressure of the lungs on the inner surface of the chest is always less than the air pressure in the lungs (by the amount of elastic recoil of the lungs). When breathing stops at any moment of inhalation or exhalation, atmospheric pressure is immediately established in the lungs. When the chest and parietal pleura of an adult are punctured for diagnostic purposes with a hollow needle connected to a manometer, and the end of the needle enters the pleural cavity, the pressure in the manometer immediately decreases below atmospheric pressure. The manometer registers negative pressure in the pleural cavity relative to atmospheric pressure, taken as zero. This difference between the pressure in the alveoli and the pressure of the lungs on the inner surface of the chest, i.e. pressure in the pleural cavity, is called transpulmonary pressure.
More on the topic PRESSURE IN THE PLEURAL CAVITY. THE MECHANISM OF ITS APPEARANCE.:
- PRESSURE OSCILLATIONS IN THE PLEURAL CAVITY DURING BREATHING. THEIR MECHANISM.
- RESPIRATORY EXERCISE № I. MECHANISMS OF ITS HEALTH IMPACT. "STRENGTHS" AND "WEAK" SIDES OF THE EXERCISE.