It has now been proven that epileptic seizures can appear in people of any age, from all social classes and at any intellectual level, and that epilepsy is often not a disease, much less a mental illness in the usual sense of the word.
In the vast majority of cases, epileptic seizures can be controlled with medication, and sometimes they go away on their own.
People with epilepsy are practically no different from people without seizures. In an environment of emotional support from other people, they live a normal life full life. Despite this, problems may arise for the person with epileptic seizures and their family.
Personality problems:
Decreased level of self-esteem;
Depression;
Difficulties in finding one's place in society;
The need to come to terms with the diagnosis of epilepsy;
Possibility of side effects of drug treatment and complications of attacks.
Family problems:
Rejection by family members of the diagnosis of epilepsy;
The need for long-term emotional and material support for a person with seizures;
The need to try not to constantly think about the illness of a loved one;
The need to take reasonable precautions and avoid overprotection;
The need for genetic counseling;
The need to help a person with epilepsy live a full life outside the family;
Need to take into account age characteristics the psyche of a person with seizures;
The opportunity to have your own family and child;
The presence of side effects of drug therapy during pregnancy (danger of fetal hypoxia);
The risk of maternal seizures affecting the normal development of the fetus.
Problems between man and society:
Restrictions on certain types of work;
Discrimination in training and employment;
Limitation of certain forms of leisure and sports;
The need for self-control when drinking alcohol;
Prohibition of driving a car (you can drive a car if you have not had seizures for more than two years);
The need to overcome prejudice in society towards epilepsy and, especially, the idea of epilepsy as a mental illness. People with epilepsy and their families should have time to talk with each other about epilepsy, their problems, experiences and interests.
Epilepsy is not a mental illness!
Epilepsy is sometimes called a mental illness. This concept in relation to epilepsy should be avoided, as it is erroneous and causes prejudice among people.
Epilepsy is not a mental illness.
Mental illnesses include depression, psychosis with hallucinations and mania, as well as diseases accompanied by decreased intelligence and personality changes. Some patients with epilepsy experience periodic psychosis, but this should be considered as a temporary complication. A decrease in intelligence may also occur, but the cause is often not epilepsy, but an underlying brain disease.
People with epilepsy without additional causes, such as brain atrophy, are no more likely to have mental problems than other people. This applies to both children and adults. First of all, among these problems are the delay mental development and behavioral disorders. Such people must be aware that they may be different from those around them, that they are somewhat different.
Unfortunately, sometimes these people see alienation and ridicule from those around them, which aggravates their condition. If epilepsy is not based on brain pathology, patients have normal intelligence. If epilepsy is a consequence of severe brain pathology (trauma, atrophy, etc.), then it is the brain disease, and not the epilepsy itself, that contributes to a decrease in the patient’s intelligence. It has been proven that the attacks themselves, with sufficient treatment, do not lead to a decrease in intelligence. Problems with the risk of mental changes in a person with epilepsy are another argument for more early treatment attacks in order to reduce subsequent social difficulties as much as possible.
Personality disorder
People with epilepsy are usually attributed certain character traits. There is an opinion that these patients are slow, inactive, petty, distrustful and inflexible. Others claim that they are very frivolous, fickle, absent-minded and irresponsible. These opinions arose from individual observations of patients with epilepsy and contain unacceptable generalizations. There is no evidence that the personality traits described above are observed only in people with epileptic seizures. Therefore there are no distinctive features character of such people. However, one should not forget that long-term treatment anticonvulsants (barbiturates, benzodiazepines) could certainly have contributed to a change in character to a slower one with impaired concentration and memory, the appearance of irritability and fussiness.
It is possible that repeated attacks with falls and head injuries can lead to organic changes in the brain and a certain lethargy and slowness. It follows that treatment of attacks should begin as early as possible, since this gives a chance to stop them at an early stage of the disease. In addition, therapy should be carried out with an optimal number of drugs, preferably one drug and in the minimum effective doses.
Personality disorders are the most common symptom mental disorders found in people with epilepsy, and they appear most often in people with an epileptic focus in the temporal lobe.
IN general case these violations include:
Age-related desire disorders;
Changes in sexual behavior;
A feature commonly referred to as "viscosity";
Increased religiosity and emotional sensitivity.
Personality disorders in their entirety are rarely expressed even in those people who suffer from complex partial seizures caused by damage to the temporal lobe. Most people with epilepsy do not have a personality disorder, but some do have disorders that are very different from the personality changes described below.
It is possible that from the above personal characteristics The most difficult thing to describe is viscosity, rigidity. This personality trait turns out to be so typical that it is most noticeable in a conversation, which is usually slow, serious, boring, pedantic, oversaturated with details at the expense of unimportant details and circumstances. The listener begins to get bored, is afraid that the speaker will never get to the right question, wants to get away from this conversation, but talking man does not give him the opportunity to carefully and successfully extricate himself. This is where the term “viscosity” comes from. The same feature is found in a person with epilepsy when writing and drawing, and hypergraphia is considered by some as a cardinal manifestation of this syndrome. The tendency toward verbosity, circumstance, and excess that is evident in conversation is reflected in the writing of these people. Some people with epilepsy can improve their communication style if a sympathetic listener points out their weaknesses. However, many people lack criticism for their violations, or they do not perceive them as violations. The religiosity of people with epilepsy is often surprising and can manifest itself not only in external religious activity, but also in an unusual preoccupation with moral and ethical issues, reflection on what is good and what is bad, and an increased interest in global and philosophical problems.
Change in sexual vision
Changes in sexual behavior can be expressed in the form of hypersexuality, disturbances sexual relations, for example, fetishism, transvestism and hyposexuality. Quite rare in epilepsy are increased sexual need - hypersexuality and disturbances in sexual relations. Cases of change in sexual orientation—homosexuality—are somewhat more common.
Hyposexuality is much more common and manifests itself both in a general decrease in interest in sexual issues and in a decrease in sexual activity. People whose complex partial seizures begin before puberty may not achieve normal level sexuality. Hyposexuality can lead to strong emotional experiences and difficulties in raising a family. Unilateral temporal lobectomy, which is sometimes successful in stopping seizures, can have a surprisingly strong positive effect on increasing libido. This operation, however, is rarely used. In addition, if hyposexuality is present, it should be taken into account that one of the main reasons for it may be anticonvulsants(barbiturates, benzodiazepines, etc.) taken long time. However, in people with epilepsy, as in other people, the cause of sexual dysfunction should be sought primarily in conflict situations with a partner.
Limitation of independence
Whether a person with epilepsy achieves independence or loses it depends not only on the form of epilepsy and its treatment, but mainly on his self-adaptation. If attacks occur frequently, loved ones will limit the person's mobility for fear of injury and avoid additional risk factors such as cycling or swimming. The fear is based on the fact that without supervision and care, an attack will occur, and there will be no one to help him. This gives rise, of course, with the best intentions, to an often exaggerated desire for the constant presence of an accompanying person. These concerns must be countered by the fact that most people with epilepsy are not exposed to trauma. It would also be worthwhile to weigh whether permanent care actually reduces the risk of deterioration of the condition of a person with epilepsy, or whether it itself causes more harm. It is doubtful that witnessing a seizure can prevent an accident. Often there is not enough strength to catch or hold a person in an attack. It is important that society is as informed as possible about the existence of people with epileptic seizures. This will help people become more compassionate and skilled in providing first aid during attacks.
The downside of constant guardianship is a person’s weakening sense of responsibility for himself. The awareness of constant supervision and the presence of another person reduces a person with epilepsy’s sense of responsibility for their actions, independence in decision-making and their correct assessment. Your own experience, even erroneous ones, strengthens your sense of self-confidence.
Therefore, you need to come to a compromise between fear for your condition and a certain freedom. It is impossible to find a rule for all occasions. Therefore, in each specific case, it would be necessary to determine, in a conversation with a doctor, the restrictions characteristic of this person with epilepsy.
Dementia (intellectual disability)
Epileptic dementia is characterized by a combination of intellectual failure (decreased level of generalization, lack of understanding of figurative and hidden meaning etc.) with peculiar personality changes in the form of extreme egocentrism, pronounced inertia, stiffness of mental processes, affective viscosity, i.e. a tendency to long-term fixation on emotionally charged, especially negative experiences, a combination of rancor, vindictiveness and cruelty towards peers and younger children with exaggerated obsequiousness, flattery, subservience to adults, especially doctors, medical personnel, teachers. Intellectual deficiency and low productivity in mental work are significantly enhanced by bradyphrenia, difficulty engaging in any new activity, switching from one activity to another, excessive thoroughness of thinking with “getting stuck” on trifles, which even in the case of a shallow defect abstract thinking create the impression of an inability to identify the main, essential features of objects and phenomena; as a rule, mechanical memory suffers, but events affecting the patient’s personal interests are remembered better. Children with epileptic dementia are often characterized by a gloomy mood background, a tendency to outbursts of affect and aggression when dissatisfied with something. In preschool and younger children school age in behavior, motor disinhibition often comes to the fore, combined with the “heaviness” and angularity of individual movements. Relatively often, including in preschool children, there is a gross disinhibition of sexual desire, manifested in persistent and undisguised masturbation, the desire to cling to someone’s naked body, hug, and squeeze children. A sadistic perversion of sexual desire is possible, in which children take pleasure in causing pain (biting, pinching, scratching, etc.) to others. When a malignant ongoing epileptic process occurs in early age in the structure of dementia, as a rule, there is a pronounced oligophrenia-like component, and the depth of dementia itself may correspond to imbecility and even idiocy. Distinguishing such an oligophrenia-like variant of epileptic dementia from oligophrenic dementia is possible only by analyzing the entire clinical picture(including epileptic paroxysms) and the course of the disease. More or less typical epileptic dementia described above is present at the onset of the disease in children over 3-5 years of age.
The psychotic state occurs more often in the interictal period, but personality disorders are observed even more often in the interictal state. Psychoses that resemble schizophrenia have been described, and there is evidence that psychoses are more often observed in individuals with temporal lobe epilepsy than in epilepsy without a local focus or with a focus located outside the temporal lobe. These chronic schizophrenia-like psychoses can manifest acutely, subacutely, or have a gradual onset. They usually occur only in patients who have suffered for many years from complex partial seizures, the source of which is disturbances in the temporal lobe. Thus, the duration of epilepsy becomes an important causative factor in psychosis. The onset of psychosis is often preceded by personality changes. The most common symptoms of such psychoses are paranoid delusion and hallucinations (especially auditory hallucinations) with clear consciousness. Emotional flattening may occur, but patients often retain emotional warmth and adequate affective experiences. Despite the fact that a typical feature of schizophrenic psychoses is thinking disorders, when organic type thinking disorders are dominated by such disorders as insufficiency of generalizations or thoroughness. The nature of the connection between such psychoses and attacks often remains unclear; in some patients, exacerbation of psychosis is observed when the attacks are successfully stopped, but such a perverted nature of the connection between these phenomena is not necessary. Responses to treatment with antipsychotics are unpredictable. In most patients, these psychoses differ from classic schizophrenic psychoses in several important respects. The affect is less pronounced, and the personality suffers less than in chronic schizophrenia. Some data indicate the enormous importance of organic factors in the occurrence of such psychoses. They occur, as a rule, only in those patients who have suffered from epilepsy for many years, and are much more common in epilepsy with a dominant focus in the temporal lobe, especially if the epileptic focus includes the deep temporal structures of the dominant (usually left) hemisphere. Over time, these people begin to be much more like patients with organic brain damage than patients with chronic schizophrenia, that is, their cognitive impairments predominate over thinking disorders. Affective psychoses or mood disorders, such as depression or manic-depressive illness, are not observed as often as schizophrenia-like psychoses. In contrast, however, affective psychoses occur episodically and are more common when the epileptic focus is in the temporal lobe of the non-dominant cerebral hemisphere. ABOUT important role Mood disorders in epilepsy can be judged based on the large number of suicide attempts in people with epilepsy.
Depression
May occur in people with epileptic seizures due to:
Excessive concern about their unusual condition;
Hypochondria;
Excessive sensitivity.
It is necessary to distinguish between simple (reactive) depression and depression as an independent disease: reactive depression is a reaction to circumstances; depression as a disease is depression associated with individual characteristics, endogenous depression.
Causes of depression in people with epileptic seizures:
Diagnosis of epilepsy;
Social, family, emotional problems associated with epilepsy;
Prodromal symptoms of a depressive nature before an attack (aura in the form of depression);
Depression accompanying an attack;
Depression after an attack;
Constant depression during long period after an attack.
Aggression
Aggressive behavior generally occurs with equal frequency in people with epilepsy and in the general population. People with epilepsy are just as capable of violence as others. Sometimes these patients are attributed to increased irritability. Although quite often you can meet people without epilepsy who are quite cocky. And for people with epilepsy with their difficult life situation, with scant social contacts, loneliness, restrictions, and also deeply offended by others, with their prejudice and ignorance, it is understandable that sometimes they can be irritable and angry with the whole world.
In addition, a person with epileptic seizures may have additional reasons become aggressive:
If you force him or hold him during an attack; as a result of a negative attitude towards this person from society;
In the pre-attack or post-attack period;
During an attack of ambulatory automatism or during an aura;
When brain function is disrupted after severe attacks leading to personality changes or mental illness; when he has a negative attitude towards treatment.
Pseudo-seizures
These conditions are intentionally caused by a person and look like seizures. They may appear to attract additional attention or to avoid some activity. It is often difficult to distinguish a true epileptic seizure from a pseudoseizure.
Pseudo-attacks occur:
More common in women than men;
People who have relatives with mental illness in their family;
In some forms of hysteria; in families where there are difficulties in relationships;
For women with problems in the sexual area;
In people with a burdened neurological history.
Clinical manifestations of pseudo-attacks:
Behavior during an attack is simple and stereotypical;
The movements are asymmetrical;
Excessive grimacing;
Trembling instead of convulsions;
Sometimes there may be shortness of breath;
Emotional explosion, state of panic;
Sometimes screaming; complaints about headache, nausea, abdominal pain, redness of the face.
But unlike epileptic seizures, pseudo-seizures do not have a characteristic post-seizure phase, there is a very rapid return to normal, the person smiles often, there is rarely damage to the body, there is rarely irritability, there is rarely more than one attack in a short period of time. Electroencephalography (EEG) is the main examination method used to identify pseudoseizures.
In addition to a variety of paroxysmal-convulsive disorders, epilepsy is characterized by mental disorders, manifested by changes in the entire personality structure of the patient, as well as various psychotic states.
Personality changes in epilepsy are characterized by irritability, pickiness, a tendency to quarrel, outbursts of rage, often accompanied by dangerous aggressive actions.
Along with these explosive traits in epilepsy, there are also diametrically opposed character traits - timidity, timidity, a tendency to self-humiliation, emphatically exaggerated courtesy, reaching the point of flattery and servility, exaggerated deference and affection in treatment. The mood of patients is subject to frequent fluctuations - from gloomy-depressed with a feeling of irritation, hostility and hopelessness to increased carelessness or simply somewhat excited without noticeable cheerfulness. The intellectual abilities of patients with epilepsy are also variable. They complain of sluggish thoughts, the inability to concentrate their attention, decreased performance, or, on the contrary, they become overly active, talkative, and capable of doing work that until recently seemed insurmountable to them. Intermittency psychic phenomena in the sphere of mood and mental abilities is one of the most important traits in the character of patients with epilepsy. Patients with epilepsy are characterized by slowness and stiffness thought processes(“heaviness of thinking”, in the words of P. B. Gannushkin). This is manifested in the thoroughness and verbosity of their speech, the tendency in conversation to detail, getting stuck on the unimportant and the inability to highlight the main thing, the difficulty of moving from one circle of ideas to another. Characterized by poverty of speech, frequent repetition of what has already been said, the use of formulaic ornate phrases, diminutive words, definitions containing an affective assessment - “good, beautiful, bad, disgusting”, as well as words and expressions of a religious nature (the so-called divine nomenclature). The speech of patients with epilepsy is melodious. Patients with epilepsy pay attention to their own “I” Special attention. Therefore, in the foreground of their interests and statements is always the personality of the patient himself and his illness, as well as relatives, about whom the patient speaks with emphasized respect and praises at every opportunity. Patients with epilepsy are always supporters of truth, justice, order, especially when it comes to everyday trifles. They are characterized by a love for treatment, belief in the possibility of recovery, and an optimistic attitude towards the future (epileptic optimism).
In cases where the listed signs are only partially expressed, not sharply, and there is no disruption of the patient’s adaptation to usual living conditions, they speak of an epileptic character. Their distinct manifestation, accompanied by memory changes of varying depth, suggests the presence of epileptic dementia. The rate of increase in personality changes, as well as memory changes, depends on many reasons, including the duration of the disease itself, the nature of paroxysmal disorders and their frequency.
Against the background of the described personality changes, in some cases due to seizure states (before their onset or after them), in others without visible external cause With epilepsy, a variety of psychotic disorders develop. They are characterized by the following general signs: as a rule, the suddenness of the beginning and end, the same type of clinical picture (like a “cliché”), short duration or transience (from several minutes to several days).
What epilepsy is is still not clear, although it has been known for thousands of years. Hippocrates also studied this disease. But still here today more questions than answers.
Orthodox psychologist Tatyana Shishova talks about epilepsy with a famous psychiatrist, Doctor of Medical Sciences, Professor Galina Vyacheslavovna KOZLOVSKAYA.
T.Sh.: – The ancient Greeks called it Hercules disease, believing that it was a sign of intervention from above. In Russia, a more down-to-earth and accurate name has taken root: “epileptic”. This is formidable serious disease, which affects people of all ages. Moreover, children suffer from it more often than people of other ages. And the consequences of epilepsy in children can be especially dangerous.
G.K.: – The main manifestation of epilepsy is a seizure. Epileptic seizures are very diverse, but they have basic properties that unite them. This is suddenness, short duration and a memory disorder that occurs after a seizure, when the patient does not remember what happened to him before. A classic seizure looks like this. Suddenly, loss of consciousness occurs when a person cannot keep the body in balance and falls. Moreover, he falls suddenly, without having time to group himself, he falls backward, or, conversely, prone, or on his side. A motor storm arises... This is the kind of discharge when a person freezes in some very tense tonic pose, gritting his teeth. His arms and legs tense, his head throws back. This lasts for several seconds, after which another phase of the seizure begins: the whole body is shaken by convulsions. There is vigorous flexion and extension of the muscles of the arms and legs, contraction of the muscles of the neck and face, as a result of which the person bites his tongue, bites his cheek, breathes very violently and heavily because the muscles are contracting chest. All this lasts about two minutes, and then the person comes to his senses, but remains in a state of some kind of stunned state. For many people with epilepsy, a classic seizure occurs rarely, up to once or twice a year, or even less often. In other patients, on the contrary, seizures occur very often.
T.Sh.: – Are there any other forms of manifestation of epilepsy, besides seizures?
G.K.: – Of course, there are, and they are very diverse. These include mood disorders, sleepwalking, and ambulatory automatism.
T.Sh.: – Let’s talk about each such manifestation in more detail.
G.K.: – Mood disorders occur in children, perhaps even more often than in adults. Suddenly, without any reason, the so-called melancholy with anger rolls in, increased irritability, pickiness towards everyone and everything, a state of dissatisfaction. It can be so unbearably difficult for a person that adults look for an outlet in the use of alcohol or drugs. And in children, the release from this state most often manifests itself in aggression, protest behavior, and hysterics. An attack of dysphoria passes as suddenly as it appears. It can last for hours, days, and sometimes weeks. In such attacks there is no classic sign of epilepsy - loss of memory for what is happening. Although for some actions, especially in a state of passion, memory is lost or reduced in detail. The patient does not remember the details of his angry outbursts.
T.Sh.: – Are people of different ages also susceptible to sleepwalking?
G.K.: – Yes. This is the most well-known form of epilepsy in the literature, when a person gets up during sleep, begins to wander, performs any actions, can go out into the street and go somewhere. Outwardly, he differs from others only in the increased pallor of his face. If you ask him a question, he, as a rule, does not react to the speech addressed to him. A person in a state of sleepwalking should under no circumstances be called out or woken up: having suddenly woken up, he loses the balance of his movements. This can also provoke a violent outburst of aggression.
T.Sh.: – Are such manifestations characteristic only of epilepsy?
G.K.: – There is an opinion that this also happens with neuroses. But with neuroses, the matter is usually limited to sleep talking or mild somnambulism, when a person moves around his bed.
T.Sh.: – A Sopor– manifestation of epilepsy?
G.K.: – Yes, but lethargic sleep and somnambulism occur in adults, and children often have petit epileptic seizures, when the child’s gaze suddenly stops, the child suddenly turns pale, moves something with his hands, and performs some habitual actions. All this lasts for a few seconds and then stops, and the child does not remember what happened to him. With such seizures there is no motor storm or convulsions. There is only a slight loss of consciousness.
T.Sh.: – You mentioned ambulatory automatism. What is he?
G.K.: – Outpatient – from the Latin word ambulo- "walk around". A person can wander involuntarily for a long time, go somewhere, even, for example, to another city. This condition is very dangerous. It can be long lasting, lasting several days. The patient briefly, monosyllabically answers questions, but at the same time his consciousness is turned off. The body operates automatically. Coming out of it, a person does not remember what happened to him.
There are other manifestations of epilepsy that it is also advisable to talk about. Seizures usually start suddenly. However, in some patients, a so-called aura, a harbinger, first appears. In fact, this is already the beginning of a seizure, but the person can still control himself and, for example, does not fall into a fire or a river, but manages to catch on to something, avoiding serious injury or even death.
T.Sh.: – Yes, indeed, very diverse manifestations...
G.K.: – However, the disease is characterized by amazing constancy. If, for example, a patient has minor seizures, then he is no longer threatened with major ones. The same movements are repeated time after time: someone straightens their hair, someone smacks their lips, chews, grinds their teeth... And the aura flows unchanged for each person. It can be visual, when a person sees, say, some balls in front of him, or auditory, olfactory, tactile. In the latter case, the patient feels tingling and twisting. As a rule, with epilepsy all these sensations are unpleasant. The smells are disgusting, the visual visions are terrible, the sounds are loud and irritating, the tingling sensations in the body are also very unpleasant.
T.Sh.: – What are the consequences of epilepsy?
G.K.: – Again, very different. The disease itself usually leads to personality changes. An epileptoid character is a combination of incompatible things: sweetness and cruelty, pedantry and sloppiness, hypocrisy and licentiousness, pickiness towards others and permissiveness for oneself. A person with such a character is very difficult in everyday life, unkind, greedy, picky, always dissatisfied, constantly lecturing everyone, demanding compliance with the established order once and for all. In these demands, he can reach the point of fanaticism and show incredible cruelty towards others if they do not fulfill his demands. In addition to this, if seizures last a long time and are not treated, the patient develops specific epileptic dementia: memory and mental combinatorics weaken, and mental clarity is lost. And character traits, on the contrary, become sharper. Self-esteem becomes very high, and pettiness, demandingness and greed reach the point of absurdity.
And the exact opposite also happens. Some patients are unusually kind, selfless, selfless, compassionate, and reverent. Typically, these are patients who rarely have seizures. Although they are also characterized by stubbornness and adherence to certain attitudes, which they will never, under any circumstances, even sometimes under the threat of death, change. These attitudes are usually humanistic, friendly towards other people.
T.Sh.: – The character of Prince Myshkin?
G.K.: – Yes, Prince Myshkin of Dostoevsky is exactly such an image. Of course, a rare event with epilepsy, but it does occur. And I would like to say separately about the rare - once or twice a year - seizures of epilepsy, characteristic of great people. For example, Alexander the Great, Michelangelo, Peter the Great, Ivan the Terrible and a number of other people who created an entire era in the development of mankind suffered from such attacks. These attacks reveal the tension of their entire personality and nervous system.
T.Sh.: – Why do people get epilepsy?
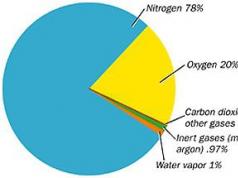
G.K.: – There is an opinion that the cause of epilepsy is auto-intoxication, the accumulation in the body of toxic substances, excess amounts of amino acids that should normally be broken down - urea, nitrogenous compounds. With the help of a seizure, the body is detoxified.
T.Sh.: – Why does intoxication occur?
G.K.: – This is not completely clear, but most often epilepsy is associated with birth injuries in children, with asphyxia during childbirth, with damage to the child’s central nervous system during the mother’s pregnancy or in the first months of the child’s life. But on the other hand, if this were the case, then there would be many cases of epilepsy. And it, unlike, say, borderline states, is quite rare. So there are, apparently, some other factors influencing the occurrence of this disease.
T.Sh.: – Can epilepsy begin in infancy?
G.K.: – Yes. And here too there are some peculiarities. Sometimes it can be easily treated, but if treatment does not work positive results, early-onset epilepsy quickly leads to dementia.
T.Sh.: – How does epilepsy manifest in infants?
G.K.: – They have minor epileptic seizures in the form of head shaking, smacking, so-called Salaam seizures, when the child bows and spreads his arms, makes “nods” and “pecks” (twitching of the head). These minor attacks are especially malignant and quickly lead to mental retardation.
T.Sh.: – At what age does this happen?
G.K.: – About a year. It is these attacks that are difficult to eliminate. Neurologists are now actively involved in the treatment of epilepsy. But in cases where epileptic dementia sets in, they give up, and this contingent comes under the supervision of psychiatrists.
T.Sh.: – Can epilepsy develop from a blow to the head, resulting in a concussion?
G.K.: – Yes. There is so-called symptomatic epilepsy, which occurs after severe head trauma, with head wounds, severe infections, and encephalitis. But it does not lead to epileptic personality changes. If any changes occur, they are insignificant.
T.Sh.: – Can epilepsy occur against the background of severe stress?
G.K.: – No. Against the background of severe stress, a hysterical attack occurs, which is similar to an epileptic one, but this is a phenomenon of a completely different genesis and of a different type.
T.Sh.: – Can a person who did not have epilepsy in childhood develop it at a later age?
G.K.: – Unfortunately, yes. This can be caused, for example, by an altered metabolism or a head injury, especially if the person was genetically predisposed to epilepsy.
T.Sh.: – Does it happen that a person had epileptic seizures in childhood, and then they went away?
G.K.: – Of course! This is very common. If childhood epilepsy is properly treated, it goes away. Especially if epilepsy is not congenital, but arises due to some kind of brain damage.
T.Sh.: – When should parents be wary? What should you pay attention to?
G.K.: – If at least one attack occurs, you must definitely show the child to a doctor. It is best to see an epileptologist. And under no circumstances should you be embarrassed by the prescription of medications. In such cases, as a rule, large doses are prescribed to relieve epileptic seizures and prevent the development of dementia, since in childhood epilepsy is often accompanied by dementia. Avoid drug treatment, using any auxiliary means is very dangerous. You can miss time and irreparably harm your child.
T.Sh.: – By attack, do we mean not only severe seizures, but also manifestations of somnambulism?
G.K.: – Yes, and also dream-speaking. Nocturnal enuresis can also sometimes be a manifestation of a seizure. And since seizures in children often occur in their sleep and are not developed, parents may not notice them. Therefore, manifestations of nocturnal enuresis require investigation for epilepsy. Now there are wonderful ways, allowing to determine the presence of epileptic discharges in the brain.
T.Sh.: – Do you mean an encephalogram?
G.K.: – Yes, it is a good diagnostic indicator.
T.Sh. – You said that epilepsy is treated with large doses of drugs. And some parents are afraid that such doses will harm their child.
G.K.: – Nevertheless, epilepsy is treated in exactly this way, and for years. And treatment should under no circumstances be interrupted. Competent treatment, lasting two to three years, as a rule, the attacks stop, after which the dosage of the drugs is gradually reduced and, finally, they are canceled altogether. The person becomes virtually healthy. A sudden interruption of medication can provoke an epileptic condition in which seizures do not stop, and this can lead to death.
T.Sh.: – What other instructions must be carefully followed?
G.K.: – If you have epilepsy, you cannot engage in sports that have a high risk of head injury. You should not swim, because a seizure may occur while in the water and the person will drown. Abrupt climate change and dousing are contraindicated. cold water, bath and other similar shocks to the body. Of course, you need a calm environment, an appropriate diet: no salt, no fatty meat, limited sweets.
T.Sh.: – How should you treat a child who has an epileptoid character? As you rightly noted, this is a difficult character, and parents do not always cope with such children.
G.K.: – We must use positive sides character: clarity, pedantry, accuracy, diligence, dedication, conscientiousness. Such a child can be assigned something both in kindergarten and at school, and he will carefully complete the task. Just don't force him to watch other children. The role of an overseer is categorically contraindicated for him. It will contribute to the aggravation of the unpleasant traits of his character. It is important to recognize the child’s merits and increase his authority in the eyes of others.
T.Sh.: – In what areas can an epileptoid succeed?
G.K.: – They are often good musicians, virtuoso performers. Natural pedantry helps them master technology music game. They are not lazy to spend a long time learning scales and other exercises. If they have the data, they make good vocalists, because producing a voice also requires a lot of work. They are good accountants and do well with any work that requires systematic, painstaking work. But they are usually not distinguished by flights of creative thought or any breakthrough discoveries. The intellect is still not brilliant. We are, of course, not talking about outstanding people with rare attacks of epilepsy, whose brains work for ten. However, they essentially do not have epilepsy as such.
T.Sh.: – What professions should you not choose?
G.K.: – It is quite difficult for them to establish good relationships with people, so professions that require communication should be approached with caution. Epileptoids should not be teachers, because they are big bores. It is not recommended to work as a high-altitude climber, driver, pilot, or sailor. Even if epileptic seizures only occurred in childhood and then stopped, such professions are contraindicated for them. You shouldn’t work as a surgeon either, since surgery requires a lot of effort, intelligence, and attention, and this can provoke an attack. But a therapist - please! Unless, of course, there is a tendency towards anger. If, on the contrary, a person of an epileptoid type has a tendency toward complacency, then he will become an excellent, caring doctor or veterinarian.
When choosing a profession for a person suffering from epilepsy, it is important to follow his inclinations. Let's say he has a penchant for drawing - and not just for drawing, but for sketching, making copies - wonderful! He can become a very good copyist, will repeat great masters, meticulously reproducing their writing style.
Embroidery, knitting, beading, painting on wood, ceramics are suitable for them... There are many ways to succeed professionally, using your epileptic character for good.
PERSONALITY CHANGES IN EPILEPSY.
According to various assumptions, the formation of personality changes is influenced by: 1) in which lobe the epileptic focus is located; 2) changes depend on the frequency of large convulsive paroxysms (lead to secondary necrosis of ganglion cells); 3) an important role is given to antiepileptic drugs, which contribute to the development of irritability and dysphoric states in patients; 4) the influence of biological (premorbid characteristics, level of intelligence and degree of brain maturity at the time of the onset of the disease) and social factors (environmental, microenvironmental) - patients with epilepsy often develop reactive and neurotic states associated with the dismissive and sometimes aggressive attitude of others; 5) the result of the combined influence of various factors; 6) changes in character (manifestation of “epileptic radicals” of the personality) increase as the disease progresses.
The range of personality changes in epilepsy ranges from relatively mild characterological features to disorders indicating deep dementia specific to this disease. Epileptic personality changes are quite typical. The main features of the psyche of patients with epilepsy are stiffness, slowness of all mental processes, a tendency to get stuck on details, thoroughness, the inability to distinguish the main from the unimportant, and difficulty switching. All this makes it difficult to accumulate new experience, weakens combinatorial abilities, impairs reproduction and ultimately makes it difficult to adapt to the surrounding reality.
A significant place in the picture of personality changes is occupied by the polarity of affect in the form of a combination of affective viscosity, the tendency to get stuck on certain, especially negative, affective experiences, on the one hand, and explosiveness (explosiveness) on the other. These features of affect are expressed in such characterological features as rancor, vindictiveness, egocentrism, malice, brutality.
Patients are characterized by emphasized, often caricatured pedantry in relation to both their clothing and the special scrupulous order in their home and workplace. An essential feature of epileptic personality changes is infantilism. It is expressed by immaturity of judgment, a special overvalued attitude towards relatives, as well as the religiosity characteristic of some patients with epilepsy.
Relatively often there are also exaggerated sanctimonious sweetness, emphasized servility, affectionate behavior and a combination hypersensitivity, vulnerability (defensive traits) with brutality, malice, hostility, explosiveness. The combination of defensive and explosive traits in patients with epilepsy is indicated by an old but true figurative expression: “With a prayer on your lips and a stone in your bosom.”
Noteworthy and special appearance patients suffering from epilepsy for a long time. They are, as a rule, slow, stingy and restrained in gestures, their face is inactive and inexpressive, and their facial reactions are very poor. A special, cold, “steel” shine in the eyes (Chizh’s symptom) is often striking.
Patients with epilepsy may experience hysterical and asthenic disorders.
Hysterical disorders can manifest themselves both in individual hysterical features and in hysterical seizures that occasionally occur along with typical epileptic paroxysms.
Asthenic disorders in the form of symptoms of general hyperesthesia, increased excitability, rapid exhaustion, sleep disturbances, and headaches. In some cases, asthenic disorders may be associated with repeated traumatic brain injuries when patients fall during seizures or with chronic intoxication with barbiturates.
The characteristics of final epileptic states are directly related to the issue of personality changes in patients with epilepsy. The most successful definition of epileptic dementia is visco-apathetic. Along with pronounced stiffness of mental processes, patients with epileptic dementia experience lethargy, passivity, indifference to the environment, lack of spontaneity, and dull reconciliation with the disease. Thinking becomes viscous, concretely descriptive, the ability to separate the main from the secondary is lost, the patient gets bogged down in trifles. At the same time, memory decreases, vocabulary becomes impoverished, and oligophasia appears. At the same time, with epileptic dementia there is no affective tension, malice, or explosiveness characteristic of the epileptic psyche, although traits of servility, flattery, and hypocrisy often remain.
With a long course of the disease, patients often develop certain features that were previously not characteristic of them; a so-called epileptic character arises. The patient’s thinking also changes in a peculiar way, with an unfavorable course of the disease reaching typical epileptic dementia.
The range of interests of patients narrows, they become more and more selfish, they “lose the richness of colors and their feelings dry up” (V. Griesinger). One's own health, one's own petty interests - this is what is increasingly becoming the focus of the patient's attention. Internal coldness towards others is often masked by ostentatious tenderness and courtesy. Patients become picky, petty, pedantic, love to teach, declare themselves champions of justice, usually understanding justice in a very one-sided way. A peculiar polarity appears in the character of patients, an easy transition from one extreme to another. They are either very friendly, good-natured, frank, sometimes even sugary and obsessively flattering, or unusually angry and aggressive. The tendency to sudden violent attacks of anger is generally one of the most bright features epileptic character. The affects of rage, which easily, often without any reason, arise in patients with epilepsy, are so demonstrative that Charles Darwin, in his work on the emotions of animals and humans, took as one of the examples the angry reaction of a patient with epilepsy. At the same time, patients with epilepsy are characterized by inertia and immobility of emotional reactions, which is outwardly expressed in rancor, “getting stuck” on grievances, often imaginary, and vindictiveness.
Typically, the thinking of patients with epilepsy changes: it becomes viscous, with a tendency to detail. With a long and unfavorable course of the disease, the features of thinking become more and more distinct: a kind of epileptic dementia increases. The patient loses the ability to separate the main thing, the essential from the secondary, from small details, everything seems important and necessary to him, he gets bogged down in trifles, with great difficulty switching from one topic to another. The patient’s thinking becomes more and more concretely descriptive, memory decreases, vocabulary becomes impoverished, and so-called oligophasia appears. The patient usually operates with a very small number of words, standard expressions. Some patients have a tendency to use diminutive words - “little eyes”, “little hands”, “doctor, dear, look how I cleaned up my little bed.” The unproductive thinking of patients with epilepsy is sometimes called labyrinthine.
A patient with epilepsy, wanting to inform the doctor about another seizure, describes her condition as follows: “So, when I got up, I went to wash, there was no towel yet, Ninka, the viper, probably took it, I’ll remember that to her. While I was looking for a towel, I had to go to breakfast, and I hadn’t brushed my teeth yet, the nanny told me to go quickly, and I told her about the towel, and then I just fell, and I don’t remember what happened next.”
All of the listed symptoms do not necessarily have to be fully present in every patient. Much more typical is the presence of only some specific symptoms, which naturally always appear in the same form.
The most common symptom is a seizure. However, there are cases of epilepsy without grand mal seizures. This is the so-called masked, or hidden, epilepsy (epilepsia larvata). In addition, epileptic seizures are not always typical. There are also various kinds of atypical seizures, as well as rudimentary and abortive ones, when a seizure that has begun can stop at any stage (for example, everything can be limited to just an aura, etc.).
There are cases when epileptic seizures occur reflexively, like centripetal impulses. The so-called photogenic epilepsy is characterized by the fact that seizures (major and minor) occur only when exposed to intermittent light (flickering light), for example, when walking along an infrequently illuminated fence, under intermittent light from a ramp, when watching programs on a faulty TV, etc. d.
Late-onset epilepsy (epilepsia tarda) occurs after the age of 30 years. A feature of late-onset epilepsy is, as a rule, the faster establishment of a certain rhythm of seizures, the relative rarity of the transition of seizures to other forms, i.e., they are characterized by greater monomorphism epileptic seizures compared with early-onset epilepsy (V. A. Karlov).
The results of the disease are difficulties in using new experience, weakness of combinatorial abilities, and deterioration in the reproduction of past experience. It should be noted the polarity of affect - a combination of affective viscosity and explosiveness (explosiveness). Patients remember the insult for a long time and take revenge for it. There is pedantry emphasized to the point of caricature in relation to clothing, order in the house, etc. An essential feature of epileptics is infantilism, expressed in immaturity of judgment, and inadequate religiosity characteristic of some patients. Often there is politeness exaggerated to the point of sweetness, to the point of servility; a combination of increased sensitivity, vulnerability with brutality and malice. The face of these patients is inactive, inexpressive, facial reactions are poor, the patients are stingy and restrained in gestures.
During a pathopsychological examination of patients with epilepsy, thinking (dynamics, operations), memory, attention, processing ability, and switching are studied. The thinking of patients with epilepsy is stiff and viscous. Patients find it difficult to perform any switching tests. Using Schulte tables reveals a slowdown in tempo mental activity(bradycardia). The time to find numbers on one table increases to 1.5-2.5 minutes or more. At the same time, exhaustion is not noted if there is no somatization. Difficulties in working with the modified Gorbov table are especially pronounced. In the methods of “excluding objects,” “classification,” and “analogies,” patients find it difficult to differentiate the main and secondary signs. There is a fixation of attention on specific unimportant details. As a result, subjects find it difficult to establish similarities based on gender. When describing drawings, retelling texts, establishing the sequence of events in a series of plot paintings, excessive detail of associations and thoroughness of judgments are noted. In an associative experiment, an increase in the latent period, frequent echolalic reactions, monotonous repetition of the names of the same objects, and inertia of the attitude are noted (for example, when the patient answers, it is only with adjectives). As a result of impoverishment vocabulary patients form antonyms by adding the particle “not”. The difficulty is especially pronounced when presenting abstract concepts. Often the speech of patients is replete with diminutive suffixes, and the rate of speech is slow. Reasoning in this disease is distinguished by pathos, instructiveness, overestimation of one’s life experience, banality of associations, and patterns in thinking. Patients often involve themselves in situations (for example, when drawing pictograms, etc.), do not understand humor (a series of drawings by H. Bidstrup), which indicates egocentrism, insufficient understanding of figurative meaning, subtext. Patients experience a decrease in memory; the curve for memorizing “10 words” has a “plateau” character. The decrease in the level of generalization is proportional to the decrease in memory.