The degree of skin response to radiation largely depends on the source and dose of ionizing radiation, and on the size of the area of skin irradiation of a cancer patient.
Manifestations of radiation skin reaction: itching, slight burning and redness of the skin.
Changes in the skin of a cancer patient after radiation can vary: from slight redness, discoloration (pigmentation) and peeling to swelling and the development of dry or wet inflammation with detachment of the upper layer (epidermis). Recent changes may resemble appearance burn from boiling water. Very deep burns cancer treatment are rarely observed.
In order to minimize the damaging effects of radiation on the skin, you need to remember the following.
1. During the period of radiation therapy for cancer, you should not use body creams and other perfumes for the skin, as they can increase the sensitivity of the skin to radiation that destroys cancer;
2. From the moment redness of the skin of a cancer patient appears, the damaged area of the skin must be lubricated with a rich cream. Well suited for this purpose fish fat, sea buckthorn oil or Fleur-enzyme cream. Fleur-enzyme cream contains the antioxidant (anti-oxidant) enzyme superoxide dismutase, the latter which provides a reduction in the degree inflammatory reactions in the skin after cancer therapy;
3. For radiation dermatitis, accompanied by swelling and pain, textile napkins “Coletex” with propolis, urea, chlorhexidine or dimexide can be applied to the area affected during cancer treatment. The material from which the napkin is made is designed in such a way that the medicine contained in it gradually moves into the skin over the course of two days. cancer patient, providing therapeutic effect. And if there is a wound that is devoid of the upper epithelial layer, the napkin also absorbs tissue breakdown products, helping to cleanse and heal the damaged surface.
Propolis effectively promotes the healing of irradiated skin surfaces and stimulates the restoration of the skin of a patient treating cancer.
Urea is good at relieving swelling and pain at the radiation site effects on cancer.
Dimexide not only relieves pain and swelling, but also promotes fast healing damaged skin and recovery of cancer patients.
Chlorhexidine disinfects and promotes healing.
The napkins are very easy to use. You need to open the sterile packaging and moisten plain water the top (working) layer of the napkin, and then fix it (wet layer to the skin) on the affected area. The napkin can remain in the affected area for up to 3 days. During this time, the healing process takes place.
It is necessary to inform your cancer doctor about any changes that occur on the skin during radiation exposure. The doctor treating your cancer will tell you what measures will help avoid unpleasant consequences.
In addition to the skin, the mucous membranes of organs entering the area are also involved in radiation reactions. cancer radiation.
How to reduce the radiation reaction of mucous membranes
The sensitivity of mucous membranes to cancer-killing radiation varies. The most vulnerable is the mucous membrane small intestine, and the most stable ones are the rectum and uterus.
Manifestations of a radiation reaction of the mucous membrane during radiation therapy for cancer: swelling and redness, increasing with increasing dose of radiation exposure to cancer. In the future, a filmy coating and erosion may appear on the mucous membrane (areas without an upper protective layer).
Typically, restoration of damaged mucous membrane after radiation cancer therapy takes 10-15 days, but redness and swelling can be observed for a longer time, since ionizing radiation damages the germinal layer of the mucous epithelium. This significantly slows down its update.
Radiation reactions of the mucous membranes during cancer treatment can be prevented or significantly reduced.
If you are to undergo irradiation of the abdominal area, you may experience frequent loose stools, often mixed with mucus, and the urge to defecate. These unpleasant consequences Radiation treatment of cancer is caused by damage to the mucous membrane of the small intestine and the death of intestinal microflora.
A number of measures can help reduce the severity of these manifestations: cancer patient can independently undertake other than the treatment prescribed by the cancer doctor. These measures are as follows.
1. It is necessary to significantly reduce the amount of carbohydrates in the food of a cancer survivor. Food should be high-calorie, rich in protein (for example, soy, boiled fish or meat, eggs). In addition, during periods of severe diarrhea in a cancer patient (frequent loose stools), it is necessary to limit the intake of fresh vegetables and fruits (with the exception of bananas);
2. The locking effect can be achieved using enveloping agents, which have anti-inflammatory and protective effect on the intestinal mucosa cancer survivor. Such agents include attapulgite (kaopectate, neointestopan, reabagg) and smecta (diosmectite). These drugs envelop the intestinal wall and form a protective barrier, precipitate and remove microbes, viruses, toxic substances (including bile acids) and gases from the intestine. The drugs are not absorbed from the digestive tract and have no side effects. The antidiarrheal effect manifests itself quite quickly - already within 24 hours and lasts for several hours. Intestinal bloating and associated pain are eliminated.
Attapulgite cancer patients take 1.5 grams after the first bowel movement, and then in the same dose after each subsequent one. The daily dose is no more than 9 grams. Smecta is a natural preparation obtained from clay. Diosmectite is pre-diluted in water until a homogeneous suspension is obtained. The contents of one sachet are used for one dose. Diosmectite is taken 2-3 times a day.
It must be remembered that when taking these drugs, the absorption of other drugs taken after cancer therapy is significantly impaired. Therefore, after taking adsorbents, other drugs cancer survivor can be taken no earlier than 1.5-2 hours later.
Dies when the abdominal area is irradiated normal microflora intestines, which is one of the reasons for the development intestinal problems in a cancer patient. Therefore, after a decrease in stool frequency, it is necessary to begin restoring the intestinal flora of a cancer patient. You need to start a week before the end of the course of radiation therapy for cancer. The main drug is bifidumbacterin or bificol. Bifidumbacterin is a dried mass of living bifidobacteria. Bifikol is a dried mass of living bifidobacteria and E. coli. If there is a deficiency or absence of bifid flora in the patient’s intestines, cancer survivor, taking these drugs normalizes its microbial composition, prevents the development of harmful microbes, promotes the synthesis of a number of vitamins, restores the function of the gastrointestinal tract, increases local intestinal immunity and the general defenses of the body of a cancer survivor. Any of the drugs (bifidumbacterin or bificol) for radiation treatment of cancer must be taken for 30-45 days, 5 doses three times a day. The combination of taking bifidumbacterin (or bificol) with food additive Fervital (analogues of BioSorb, Recizen-RD) promotes better engraftment of bacteria and also regulates stool well. Fervital for cancer radiation therapy is added to food (soup, porridge, kefir) 1 tablespoon 3 times a day.
Sometimes it is necessary to short term Add another drug - Lactobacterin - to the food of a cancer survivor. This is a dried mass of live lactobacilli, which play an equally important role in the normal functioning of the intestines and are also sensitive to radiation exposure, destroying cancer. It is advisable for cancer patients to take Lactobacterin 5 doses 2-3 times a day for 14 days. If you are taking bifidumbacterin, lactobacterin can be taken after or during meals on the days you are taking the bifid drug. If bificol is used to restore the intestinal microflora of a person suffering from cancer, then Lactobacterin should be taken only after finishing taking it, i.e. after a month and a half.
Skin cancer
Skin cancer is a malignant tumor with a relatively favorable course, since, due to its localization, it is available for radical treatment - radiation and surgery. It is detected in relatively early stages of its development, which is explained by its slow growth rate, as well as ease of detection.
Based on the histological structure, they mainly distinguish between squamous cell keratinizing, squamous cell non-keratinizing and basal cell skin cancer. The most common is basal cell carcinoma or so-called cutaneous basal cell carcinoma.
When treating skin tumors in the early stages, localized on the trunk and extremities, where the cosmetic side is of less importance, a lasting clinical effect is achieved using surgery or cryodestruction (freezing the tumor with liquid nitrogen). For tumors of the scalp and especially the face, short-distance radiotherapy is mainly used.
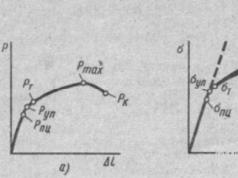
Short-distance radiotherapy is carried out taking into account the size and depth of tumor spread. The magnitude of the focal dose is planned so that the relative depth dose in the area of the tumor bed is 80%.
The latter is achieved by varying the radiation energy in the range of 30 - 100 keV and using various filters.
Short-distance radiotherapy for skin cancer.
Basalioma of the left corner of the mouth
a - before treatment; b - 2 1/2 years after radiation therapy;
c - isodose distribution under different irradiation conditions depending on the depth.
Irradiation is carried out, as a rule, from one field, and the surrounding area must be included in the irradiation zone. healthy tissue at a distance of at least 5 mm from the edge of the tumor. During irradiation, as the tumor is reabsorbed, the field size may be slightly reduced.
A single exposure dose is 400 R with an irradiation rhythm of 5 fractions per week, the total focal dose for basal cell carcinoma is increased to 50 - 55 Gy, for squamous cell skin cancer - up to 65 - 70 Gy.
A good clinical effect in the form of complete resorption of the tumor and its replacement with a cosmetically satisfactory scar, and sometimes complete epithelialization is observed mainly in superficially located skin tumors (95%), while in infiltrative forms the percentage of permanent cure is noticeably reduced.
When the tumor is localized on the skin of the eyelids, in the area of the inner corner of the eye, certain difficulties are created due to the risk of damage to the eye and the unevenness of the irradiated surface. In these cases, it is sometimes advisable to use interstitial gama therapy, and for very superficially located neoplasms (basal cell carcinoma) - applications with beta-emitting nuclides (32РХ, 90Y, etc.).
On the skin of the scalp, auricle, forehead, and bridge of the nose, radiation treatment is complicated by the proximity of bone and cartilage tissue. However, if the tumor is small and there is no infiltration of the underlying tissues, short-distance radiotherapy can be quite effective for skin cancer in these localizations.
For more common malignant skin tumors that deeply infiltrate the underlying tissue (stages III - IV), the use of remote gamma therapy is indicated.
Directories, encyclopedias, scientific works, public books.
Radiation therapy for skin cancer
Skin cancer is one of the most common cancer diseases. There are several varieties malignant tumors skin:
Basalioma or basal cell carcinoma (develops from the basal cells of the skin epithelium),
Cancer developing from skin appendages.
Popular foreign oncology clinics and centers
Cancer Center Nord, operating as part of German clinic Vivantes Clinicum Spandau is one of the largest centers in Berlin providing services in the field of oncology and hematology. Along with good technical equipment, the center is known for its team of well-trained oncologists. Go to page >>
The German outpatient clinic “Munich Oncology” is classified as a day hospital medical institution. The priority area of activity is the diagnosis and treatment of a wide range of malignant tumors, various forms of leukemia, as well as diseases of the autoimmune system. Go to page >>
The multidisciplinary cancer center of the University of Münster in Germany offers its patients highly accurate diagnosis and treatment of almost all oncological diseases. The main areas of focus are the treatment of breast cancer, gastrointestinal tract cancer, lung cancer, leukemia and lymphoma. Go to page >>
The Oncology Center at the University Hospital Hamburg-Eppendorf in Germany diagnoses and treats almost all known oncological diseases, having an excellent diagnostic and treatment base that allows for fast and highly accurate examination of patients. Go to page >>
The Oncology Center operating at the University Hospital of Ulm in Germany is rightfully considered by the medical community as one of the most advanced. The center is part of the International Society for the Treatment of Cancer, and is also a member of the Unified Cancer Center of the city of Ulm. Go to page >>
The Eastern Hospital of the National Cancer Research Center in Japan carries out diagnosis and effective treatment of cancer using the most modern equipment; it is here that the cyclotron accelerator is located, the only one in the country at the moment. Go to page >>
The Central Vienna Clinical Hospital in Austria has an Oncology Department in its division, which successfully treats many oncological diseases. The department has the most modern equipment and technology at its disposal, and is staffed by experienced oncologists. Go to page >>
Clinic named after Johann Wolfgang Goethe in Germany, among other services, provides its patients with highly accurate diagnostics and effective treatment of oncological diseases. The Clinic successfully operates one of the largest oncology centers in Europe, Rhein-Main, headed by Professor Mitrou. Go to page >>
Nutrition for cancer
What should nutrition be like for cancer patients? What foods are absolutely contraindicated for this or that form of cancer?
Herbal medicine in oncology
Herbal medicine can provide significant assistance not only in the treatment of cancer, but also in their prevention.
Heredity and cancer
Many people who have cancer in themselves or in their relatives are interested in the question: is cancer inherited?
Cancer during pregnancy
Treatment of cancer during pregnancy is quite difficult, because most medicines has toxicity.
Pregnancy after cancer
What are the prospects for pregnancy after cancer? Should you wait until after cancer treatment?
Cancer Prevention
Prevention is an important part common struggle with cancer. How to reduce the likelihood of cancer?
Palliative treatment of cancer
What is palliative cancer treatment? How can it affect the quality of life of a cancer patient and change it for the better?
New cancer treatments
Scientists have developed quite a lot of promising methods for treating cancer, which have not yet been recognized by official medicine. But everything can change!
Cancer statistics
Cancer incidence statistics, unfortunately, are disappointing: there is an increase in the number of cases, while the disease is getting younger.
About “folk” medicine
Sometimes it is possible to defeat cancer using “folk” methods, but there are many more of those who relied only on them and ended up leaving this world ahead of time.
How to fight cancer?
How to find strength to fight cancer? How not to fall into despair over possible disability? What can serve as hope and meaning in life?
How to help your loved ones?
How to help to a loved one living with a cancer diagnosis? Is a “white lie” necessary? How to behave so that loved ones suffer less?
Stress and cancer
There is an opinion that constant stressful situations can lead to the development of cancer. Is it so?
Fighting cachexia
Many cancer patients often suffer from sudden weight loss. What causes this and is there any way to deal with this problem?
Caring for bedridden patients
The rules for caring for patients who are forced to constantly remain in bed have their own characteristics and must be known.
Radiation therapy for skin cancer
Of all the existing treatments for skin cancer, radiation therapy provides the best results. This primarily applies to facial skin tumors. Considering that there are basal cell cancers on the skin of the face, radiation therapy provides a high percentage of cures with a good cosmetic effect.
Indications for radiation therapy for skin cancer
1) for primary skin cancers;
2) for metastatic skin cancers;
3) for prophylactic purposes after surgery;
4) in case of relapses.
Radiation therapy methods for skin cancer
Fractionated irradiation method. Its essence is this. that over 10-12 days treatment is carried out in relatively fractional doses, and the total dose is brought to 4000 rads.
The fractionated irradiation method has the advantage that tumor tissues are more damaged and healthy tissues are spared more than with older methods; on the other hand, the reactive ability of the tissues surrounding the tumor is preserved, which largely determines the therapeutic effect.
The positive features of the fractionated irradiation method include the influence of the time factor. Extending treatment to 12-15 days ensures that all cancer cells are exposed to x-rays, since during this period all cells go through the mitosis phase and, therefore, are exposed to radiation.
In the literature we have collected on the treatment of skin cancer, a common thread is the idea that all efforts should be aimed at achieving a cure after one course of radiotherapy.
The currently accepted principle for the treatment of malignant neoplasms is to give in one course the maximum dose compatible with the need to spare healthy tissue. Repeated irradiations due to the cumulative effect of X-rays are dangerous - they entail changes in vascularization, damage to surrounding healthy tissue, and cause necrotic changes.
Based on this, fractionated irradiation using a high total dose is recognized as the most effective method that guarantees the elimination of a cancer focus in one course of treatment.
Concentrated short-focus irradiation method according to Shaul. The short-focus irradiation method is based on the principle of creating conditions for the distribution of X-ray energy similar to those found when using radium, despite the fact that the wavelength of these two types of radiation is not the same. From the point of view of modern X-ray biology, the therapeutic and biological effect depends only on the amount of energy absorbed, be it the energy of y-rays or the energy of X-rays. The qualitative side of radiation is not given significant importance.
Based on the equivalence of y- and x-rays, Shaul believes that the greater effectiveness of radium therapy is due only to a more appropriate distribution of 7-rays. It is appropriate to note here that the issue of spatial dose distribution during radiation therapy is extremely relevant, especially when treating malignant neoplasms. The relationship between the energy absorbed by the tumor and adjacent tissues becomes extremely important.
The difficulty with radiation therapy for skin cancer is that the sensitivity differences between tumor cells and surrounding tissue cells are often insufficient. That is why the currently accepted principle of using radiation therapy for malignant neoplasms is based on the desire not only to destroy the tumor as much as possible, but also to spare the surrounding tissue as much as possible.
When radium is applied directly to the affected area, the greatest impact of rays on the site of application of radium and minimal impact on surrounding tissues is achieved, since the intensity of the radiation action to the depth and to the periphery sharply decreases.
In this regard, the method of concentrated close-focus irradiation is aimed at creating the same conditions.
According to Shaul, the method he proposed should be an imitation of radium therapy; and indeed it began to be successfully used instead of radiation therapy for some localizations of skin cancer, cancer of the lower lip, oral cavity, as well as for malignant melanomas and hemangiomas. Treatment is carried out using a special X-ray tube, in which the anode in the form of a hollow cylinder is brought out.
Radiation therapy for skin cancer with this method is carried out with a single dose of 400 - 800 rads, and a total dose of 6000 - 8000 rads.
Results of radiation therapy for skin cancer
Results depend on:
1) morphological picture;
2) localization and soil on which cancer develops;
3) treatment methods.
Basal cell carcinoma is most successfully treated with radiotherapy. The mixed form is more resistant than the purely basocellular form. Squamous cell carcinoma is the most dangerous form skin cancer. The success of treatment for this form depends on the timeliness of diagnosis.
In some locations (corner of the eye, ear), the effectiveness of radiation therapy for skin cancer is reduced.
The prognosis sharply worsens with damage to bone and cartilage tissue. This is explained by the fact that bone and cartilage tissue, due to their anatomical and physiological properties, cannot respond to X-ray irradiation with an appropriate reaction.
The soil on which the neoplasm developed also matters. The reason for the worse treatment results for cancer caused by lupus and scars is that the surrounding tissue, being weakened by the underlying disease, is unable to respond the right reaction to x-ray irradiation.
The reason radiation therapy for skin cancer fails is that sometimes the proliferation of epithelial tissue in the deeper parts of the tumor stops for a very short time and then resumes again. This may be a result of inappropriate selection of beam quality, inappropriate filtration and dose. To select a carcinicidal dose in relation to deep-lying cells, it is necessary to use filtered beams, appropriate voltage and cross-irradiation. Large doses should be used without damaging normal tissue.
Failure is rare due to the presence of resistant cells, especially in basocellular epitheliomas. It is also necessary to remember that not all cells that make up a malignant neoplasm have the same degree of sensitivity; some cells in the same tumor may be very resistant.
Patients after radiation therapy for skin cancer should be monitored every six months for 5 years. Failure to comply with this rule often leads to serious consequences.
For stages 1 and 2, radiation therapy for skin cancer is carried out under short-focus radiotherapy conditions. A single dose is 300 - 400 rad, the total dose is 5000 - 7000 rad. Doses of 500 - 600 rads per session significantly reduce the treatment time, but leave large changes on the skin, which gives worse results from a cosmetic point of view. Cure in stage 1 is observed in 95-98%, and in stage 2 - in 85-87% of cases.
At stage 3, radiation therapy should be carried out under conditions of deep radiotherapy, on a cesium installation, and in some cases, on a telegamma installation. A single dose should not exceed 250 rads. The question of the total dose is decided in each individual case, depending on the size of the lesion. If radiation therapy alone raises doubts about the possibility of achieving good results, then after the radiation reaction has subsided, surgical or electrosurgical treatment methods may be recommended. At stage 4, treatment (if it can be carried out) must begin with radiation (deep radiotherapy or telegammatherapy).
After radiation therapy, in some cases it is possible to excise the tumor with or without plastic surgery, depending on the condition and location of the pathological process. For x-ray cancer that has developed due to scars and relapses of skin cancer after radiation treatment, it is indicated surgical treatment. The scope of the operation should not confuse the surgeon, since tumor growth does not spare the patient and leads to severe disability.
Healthy:
Related articles:
Add a comment Cancel reply
Related articles:
Medical website Surgeryzone
The information does not constitute an indication for treatment. For all questions, consultation with a doctor is required.
Related articles:
What you should not and should be afraid of after irradiation of basal cell carcinoma
The treatment method for one of the most common forms of skin cancer, basal cell carcinoma, is determined by several factors. This is the location of the tumor, its size and the extent of spread to the tissues of cartilage, muscles, tendons and bones located under the epidermis. Radiation therapy is suitable for older people, patients with contraindications to removing the tumor by other means, or its size is too large. The disadvantages of this method of therapy include side effects and complications that arise after irradiation.
Indications for testing
Basalioma belongs to the so-called borderline types of cancer. The growth of the tumor occurs due to its growth deep into the skin. Initially, the neoplasm forms on the lowest layer of the epidermis - the basal layer. However, over time, it affects the subcutaneous tissue, and then cartilage or even bones. The “favorite” place for localization of basal cell carcinoma is the face, neck, and less often other open areas of the body. Considering the peculiarities of the course of this type of cancer, tumors located on the wings of the nose, near the eyes or ears are especially dangerous.
Radiation therapy for basal cell carcinoma is possible at almost any stage of the disease. However, with the development of laser and radio wave techniques for tumor removal, this method of treatment faded into the background. In addition, doctors emphasize that basal cell carcinoma grows slowly, so if you undergo regular preventive examinations, there is a high chance of detecting the disease at an early stage. In the initial stages of basal cell skin cancer, you can do without drug treatment or minimally invasive surgery. But oncologists recommend radiation therapy in such cases:
- large size of basal cell carcinoma;
- spread of malignant cells deep under the skin;
- patient age over 65 years;
- the presence of diseases that serve as contraindications to other treatments;
- features of the localization of basal cell carcinoma that prevent its surgical removal.
Irradiation is also widely used as part of complex therapy. For example, sessions of ionizing exposure are necessary after surgery if complete elimination of pathological cells is impossible. In addition, radiation exposure is an option for so-called palliative treatment. This means that therapy sessions help relieve pain and other symptoms of the disease in inoperable cases.
Methods of radiation therapy for basal cell carcinoma, their advantages and disadvantages
The effectiveness of ionizing radiation lies in its effect on cellular DNA. Under the influence of γ-irradiation, it begins to collapse, which makes further proliferation of malignant structures impossible. First of all, therapeutic radiation is aimed at rapidly dividing cells, and this is the main property of malignant neoplasms. But healthy tissue is also exposed to radiation, which causes the effects of therapy.
When contact γ-irradiation with isotopes of cobalt Co60, radium Ra226, iridium Ir192, the dose must be selected so as to achieve the death of malignant cells or a permanent cessation of their division. The procedure is carried out using special applicators, made individually for each patient from plastic material. The plate is 1 cm thick; it is dipped in boiling water and then applied to the skin of the nose or other area of the face, neck and body. The applicator is then molded to follow each curve. Radioactive elements and protective lead plates are applied to it. The advantage of this method is that the radiation intensity decreases as it passes through the tissue. This is why it is widely used to treat skin cancer.
The effect of close-focus X-ray therapy from a distance of up to 7.5 cm is achieved by irradiation with a power of 10 to 250 W. Depending on this, the depth of exposure changes - from a few millimeters to 7 - 8 cm. To focus the rays, a special tube is put on the device, and the area of influence is limited using filters made of aluminum or brass up to 3 mm thick. The degree of radiation absorption by tissues depends on the stage of basal cell carcinoma and general condition sick. Therefore, the dosage and frequency of sessions is calculated individually for each patient.
How does basal cell carcinoma differ from papilloma? Basalioma is
In this episode of the TV show "Live Healthy!" with El�
This video has How to treat and cure skin cancer - This video has How to t
Interstitial β-irradiation is carried out using radioactive isotopes of phosphorus P32 or thallium Tl204. Before this, colloidal solutions of gold Au188, silver Ag111 in the form of granules, treated with catgut threads are injected into the basal cell carcinoma tissue. According to oncologists, this method of radiation therapy is more complex than others, and the equipment for its implementation is not available in every clinic due to its high cost. It is used to treat forms of basal cell skin cancer that are resistant to other methods of radiation exposure.
Side effects that develop directly during therapy
Radiation treatment of basal cell carcinoma is always accompanied by damage to the surrounding tissues. This cannot be avoided even if you follow the rules of this method of therapy. The sensitivity of the skin to radiation depends on many factors. This:
- localization of the tumor, the anterior surface of the neck is more susceptible to radiation exposure than the skin of the wings of the nose and other areas of the face and back of the head;
- air temperature, in hot weather the blood supply to the epidermis improves, which increases the risk of developing the consequences of treatment; in cold weather this probability decreases;
- excess weight, it has been proven that the skin of obese people is more susceptible to the effects of radiation;
- cracks and scratches increase the permeability of the epidermis;
- age-related changes.
In most cases, radiation treatment of basal cell carcinoma does not cause systemic consequences. Most of the side effects are due to a skin reaction, which manifests itself in the form of epidermatitis. First, during each session, swelling, redness, and itching occur. As treatment continues, symptoms become more pronounced and reach a maximum by the third week of therapy and disappear 1 - 1.5 months after its completion.
Blisters filled with exudate form on the affected area of the skin. They burst, revealing an inflamed, bright red epidermis. This serves as a gateway for pathogenic flora, and if the doctor’s recommendations are not followed, a bacterial infection can develop. The appearance of wounds covered with crusts is also noted.
A dangerous consequence of such treatment for basal cell carcinoma is a radiation ulcer. Under the influence of radioactive isotopes, microcirculation in the blood vessels located under the skin. The risk of complications increases in proportion to the depth of penetration of the pathological process and the strength of radiation. The onset of ulcerative changes in the skin is indicated by the following symptoms:
- dryness and flaking;
- disappearance of the surface pattern of the epidermis;
- the appearance of spider veins;
- pigmentation disorder.
If basal cell carcinoma is located near the mucous membranes of the nose or mouth, inflammation may occur - mucositis. It is characterized by dry epithelium, burning and pain when touched. However, such consequences are rare. During radiation treatment of a tumor in the eye area, recurrent conjunctivitis is noted.
Long-term complications of radiation therapy
Over time, the skin exposed to radiation becomes thinner, and the vascular network is visible underneath. A year to a year and a half after the end of treatment, lighter or, conversely, darker areas of the epidermis may appear. The severity of these signs depends on the duration of treatment, the radiation dose received as a result of therapy, and the area of exposure. It is worth noting that the radiation ulcer discussed above may also appear several months after the end of treatment.
The most dangerous consequence There is a high risk of developing a more severe, malignant form of skin cancer – squamous cell cancer. For this reason, irradiation of basal cell carcinoma is not advisable for patients under 50 years of age. Also, due to the risk of complications, this method of treatment is not used for relapses of basal cell carcinoma. After exposure to radiation on the scalp, hair loss is observed. Over time, they grow back, but become brittle, dull, and their color becomes more faded.
When treating tumors located on the facial skin near the eyes, cataracts may occur. How high the risk of such a disease is is unknown, since today the threshold dose of radiation to the lens has not been established. Due to tissue scarring after the destruction of neoplasm cells, their mobility is limited, which affects facial expressions. There are also changes in the functioning of the sebaceous and sweat glands in the area of radiation exposure.
Prevention of complications
The basic rule of radiation treatment for basal cell carcinoma is a preliminary examination of the patient, collection of anamnesis, and identification of concomitant pathologies. This information will help you correctly calculate the dose, frequency and duration of therapy. Depending on the size of the tumor, the procedure involves 1–2 cm of surrounding healthy tissue. This is done to prevent relapse of the disease.
Lead plates are used to protect other nearby cells. A hole is cut out in them, which exactly follows the shape of the basal cell carcinoma, and is applied during each radiation therapy session. The patient is warned that before starting the course of treatment (as well as during it) the skin should be protected from damage. In addition, doctors recommend adhering to the following rules:
- protect yourself from direct sunlight, do not visit the solarium, go outside in long sleeves, cover your face with a wide-brimmed hat, apply a special cream to exposed skin;
- You cannot rub the skin that has been exposed to irradiation, massage it, apply cupping, apply mustard plasters, treat it with antiseptics and alcohol solutions (iodine, brilliant green, peroxide) without a doctor’s prescription;
- hygienic procedures should be carried out with care so as not to wash off the marks made by the doctor that define the area of radiation exposure;
- It is forbidden to make compresses or use a heating pad;
- before using scented soap or shower gel, bath foam, deodorant, cream, you should definitely consult a doctor; decorative cosmetics (if allowed) should be washed off 4 hours before the radiation treatment session for basal cell carcinoma;
- To prevent bacterial infection, it is worth limiting visits to public places such as swimming pools or baths.
Doctors emphasize that radiation therapy is a serious burden on the body. Therefore, if any disturbing symptoms appear, you should seek advice from your doctor or nurse. It is also better to coordinate changes in diet and climate with them. It is worth remembering that the danger of the consequences of radiation treatment for basal cell carcinoma remains for the rest of your life.
Medicines used to relieve side effects
To prevent radiation dermatitis, the skin around the basal cell carcinoma is regularly lubricated with Vaseline, metacil emulsion, or treated with a cotton swab moistened with a mixture of Shostakovsky Balsam and vegetable oil (prepared in a ratio of 1:4). Moreover, this should be done from the first irradiation session. If, despite the measures taken, ulcers form, it is necessary to prevent bacterial inflammation. To do this, lotions with solutions of silver or dioxidine are applied to the affected areas of the skin; gels Solcoseryl, Actovegin, Iruksol, and methyluracil ointment are used for speedy healing.
To prevent damage to the mucous membrane, rinsing or washing with chlorhexidine, chamomile or sage decoction is prescribed. Antibacterial drops are indicated for the treatment of conjunctivitis. If it is not possible to avoid exposure to sunlight on the skin of the face or other area of the body where the basal cell carcinoma is located, so-called indurative edema may appear. Its treatment consists of prescribing antibiotics, anti-inflammatory prednisolone and drugs to strengthen vascular wall. To prevent pigmentation, vitamin P (100 mg daily) and ascorbic acid are prescribed.
It is worth noting that with radiation treatment of basal cell carcinomas located on the face, the risk of relapse is higher than in other areas of the skin. According to oncology clinics in Russia and foreign countries, this probability is up to 30%. It is particularly difficult to target tumors localized on a textured surface, since radiation is unevenly absorbed by cells. Severe consequences of radiation therapy are noted in almost 17% of cases. Therefore, a timely visit to the clinic is of great importance, when the area and depth of the lesion allows for the removal of basal cell carcinoma without significant complications.
Good afternoon Please tell me that my friend was prescribed 12 radiation treatments for basal cell carcinoma. But she can't drive every day. Is it possible to carry out this procedure 2 days after 2 days? Is this so important?
All information on the site is presented for informational purposes. Before using any recommendations, be sure to consult your doctor.
Doctor of Medical Sciences, Professor Afanasyev Maxim Stanislavovich, oncologist, surgeon, expert in photodynamic therapy of basal cell carcinoma.
Basalioma, or basal cell skin cancer, is a complex disease. Medicine offers many treatment methods, but all of them are traumatic, fraught with the formation of serious cosmetic defects, the development of long-term complications, and none of them eliminates relapses in the future.
Even Hollywood stars, who have access to the most high-tech and expensive treatments, have to undergo treatment for basal cell skin cancer for years. Most famous example- Hugh Jackman. The actor has been fighting the disease since 2013 to save his nose. And so far he has succeeded. But against the backdrop of his sixth relapse, Jackman has a serious risk of losing it.
Unfortunately, they do not guarantee getting rid of basal cell carcinoma forever.
And even if Hugh Jackman, who has access to the most modern medical care, cannot get rid of the problem, then a logical question arises: is this disease treatable? Is it possible to cure basal cell carcinoma?
Is it necessary to remove basal cell carcinoma?, if she doesn't bother?
Many people treat basal cell carcinoma treatment too leniently. Because this form of cancer grows slowly and almost never metastasizes, doctors rarely insist on treatment and usually do not warn about the consequences of failure.
And if for elderly patients such tactics can be considered justified with a stretch, then for young people - and over the past 10 years basal cell carcinoma has become very “younger” - it does not stand up to criticism.
With this approach, the patient does not take his seemingly insignificant disease seriously and decides not to do anything about it. Very often, treatment is limited to the use of so-called “green stuff”.
But I believe that Hugh Jackman is right in his persistent desire to get rid of basal cell carcinoma. And not only because of an aesthetic defect.
Treatment is necessary. Basalioma is a tumor that, although slowly, is constantly growing. It never goes away on its own. Sooner or later, it overcomes the skin, grows into muscles and nerves, penetrates cartilage and irreversibly disrupts the functioning of organs. If basal cell carcinoma is located on the face, it literally destroys it. Basalioma in the area of the eye or nose, growing, can lead to their loss. Over time, basalioma of the head can destroy the skull and grow to the brain.
Need I say that these processes are also extremely painful?
In this stage basal cell carcinoma It is practically impossible to treat, because along with basal cell carcinoma it will be necessary to remove part of the organ or the entire organ.
You need to know the enemy by sight
Before continuing our conversation, I must tell you about one type of basal cell carcinoma that cannot be recognized at the diagnostic stage.
In approximately 6% of cases, treatment of basal cell carcinoma does not have any effect - removal of the basal cell carcinoma ends in relapse, and it reappears in the same place. And after the next removal, the whole process repeats... This form of basal cell carcinoma is called persistently recurrent basal cell carcinoma.
Unfortunately, modern medicine does not have a single effective means of combating stubbornly recurrent basal cell carcinoma. The mechanism why it returns has not yet been figured out.
However, even for such a head start on basal cell carcinoma, the founder of PDT in Russia, Professor Evgeniy Fillipovich Stranadko, recommends using exclusively photodynamic therapy as the method of choice. Indeed, in case of manifestation of persistently recurrent basal cell carcinoma, it is necessary to repeated treatment, the cosmetic effect of which will depend entirely on the method of its removal chosen at an early stage.
We must understand that any surgical treatment is always a “minus tissue” treatment, a mutilating treatment. Only PDT allows for effective treatment without removing healthy tissue and obtaining an aesthetic result even against the background of persistently recurrent basal cell carcinoma.
Surgery for basal cell carcinoma
Surgical removal of basal cell carcinoma usually performed with a laser, scalpel or radio wave scalpel with the obligatory capture of 5 mm of healthy tissue. Surgical techniques also include the cryodestruction method - removal of basal cell carcinoma with nitrogen, and the Mohs method.
I strongly advise you not to agree to remove basal cell carcinoma with a scalpel - this method usually leaves behind a rough scar.
In the early stages, removal of basal cell carcinoma surgically gives a good effect. Therefore, it makes sense to remove very small and accessible formations up to 2-3 millimeters surgically. I myself prefer this method: the procedure is simple, quick and does not require special rehabilitation.
Disadvantages of the surgical method:
- High percentage of basal cell carcinoma recurrence after excision. Advanced basal cell carcinomas, which have managed to grow beyond the skin, recur especially often.
You should not trust information that surgery to remove basal cell carcinoma has a low recurrence rate. This figure is relevant only for small entities. When basaliomas larger than 2-3 mm are removed, usually more than half of them recur.
- Difficulty and impossibility re-treatment due to severe tissue loss.
Recurrence of basal cell carcinoma requires repeated surgery. But after the second or third relapse, surgery is usually impossible: imagine what happens to the area in which, with each removal of the basal cell carcinoma, an additional 6 mm of healthy tissue is removed.
- Relapse after surgery occurs in the scar area. This area is almost impossible to treat with PDT. Therefore, in case of relapse of basal cell carcinoma after surgical treatment, you will have practically no alternative method left - only repeat surgery or irradiation.
- If the tumor is located on the wings of the nose, on the auricle or in the corners of the lips, if multiple basal cell carcinoma is to be treated, then the surgical method literally turns into a mutilating operation. In these areas, every millimeter of tissue is important, but often, along with the tumor, it may be necessary to remove up to half of the nose or ear, and the lack of tissue cannot be compensated for by plastic surgery methods.
- A contraindication to surgery is the location of the basal cell carcinoma in close proximity to the eye - there is a high risk of its loss.
Laser removal of basal cell carcinoma: features of the method and its disadvantages
Laser treatment of basal cell carcinoma is a surgical operation.
Laser removal of basal cell carcinoma has one significant drawback. The fact is that laser ray does not cut tissue, but evaporates it, layer by layer. After the laser, only a charred crust remains from the tumor. Thus, “cauterization” with a laser does not make it possible to send the removed tumor for histological examination. Only histology allows one to assess the completeness of basal cell carcinoma removal and exclude a more serious form of cancer, which in rare cases is hidden or adjacent to basal cell carcinoma.
This method also has one more drawback. Laser treatment of basal cell carcinoma thermally damages tissue, and such a wound heals with the formation of a scar.
Removal of basal cell carcinoma using Surgitron: features of the method and its disadvantages
Radio wave removal of basal cell carcinoma, or electrocoagulation, or treatment with electric knife,
- another surgical method. In this case, a tip with a thin wire is used to remove the formation. When an electric current of a certain frequency is passed through a wire, it acquires the properties of a scalpel.
Most often, treatment of basal cell carcinoma with radio waves is performed using medical equipment from the American company Surgitron, which gave the method its second name.
This method is good because after its use, tissue remains for biopsy - the pathologist will be able to assess the completeness of basal cell carcinoma removal and rule out a more aggressive form of cancer. The disadvantage of electrocoagulation is the same as everyone else's surgical techniques– high percentage of relapses for all tumors exceeding 2 mm.
You also need to be mentally prepared for the fact that excision of skin basal cell carcinoma using radio waves leaves behind a scar.
Cryodestruction of basalioma: features of the method and its disadvantages
Cryodestruction, or cryotherapy, is the cauterization of basal cell carcinoma with liquid nitrogen.
The method is cheap and quite widespread. However, you shouldn’t count on a miracle. Removing basal cell carcinoma by cryodestruction has a very serious drawback: the depth of exposure of liquid nitrogen to tissue cannot be controlled. That is, after treating basal cell carcinoma with nitrogen, there is a risk of both leaving lesions in the skin and, conversely, affecting too large areas of healthy tissue. In the latter case, after cauterization of basal cell carcinoma, there is a high probability of developing an extensive scar.
Treatment of basal cell carcinoma with cryodestruction has another drawback. Since the method does not make it possible to assess whether the tumor has been completely removed or not, basal cell carcinoma after cryodestruction may well resume its growth and eventually require repeated removal.
Mohs method: features of the method and its disadvantages
This is a high-tech and expensive treatment method that requires special equipment, special training of the surgeon and the presence of the clinic’s own pathology laboratory. It is designed to achieve high aesthetic results in the treatment of tumors on the face, neck, legs and arms, and genitals.
This is probably the method used to treat Hugh Jackman.
The Mohs operation can be compared (very loosely, of course) to using a slicer: tissue is removed in thin layers, layer by layer, and immediately sent to the laboratory. The procedure is repeated until tumor cells are no longer detectable in the section.
Since the entire operation is carried out under the supervision of a pathologist, there is no need to remove the basal cell carcinoma “involving” 6 mm of healthy tissue.
The operation is highly aesthetic, and if there is a lack of skin in the operated area, it is replaced with implants.
Irradiation of basal cell carcinoma: features of the method and consequences after irradiation of basal cell carcinoma
Radiation, or radiation, treatment methods are used only if there are contraindications to alternative methods. This is the method of choice for complexly located (for example, on the face), deep or too large tumors up to 5 cm that cannot be treated surgically. They are also prescribed to elderly patients with contraindications to surgical treatment.
Since the use of the method is always accompanied by complications, it is used mainly for elderly people over 65 years of age.
Irradiation of skin basalioma is carried out:
- using close-focus X-ray therapy,
- using gamma rays,
- using beta rays (electrons).
The use of a particular method is not always determined by rationality. Close-focus X-ray therapy is presented in every oncology clinic, so most often patients are referred to it. Electronic installations are expensive and complex, so literally only a few clinics are equipped with them.
Let's look at how radiation therapy works on basalioma.
It is believed that treatment of basal cell carcinoma with radiation therapy negatively affects the DNA of tumor cells. Ionizing radiation makes their further division impossible; after radiation therapy, basal cell carcinoma stops growing and is destroyed over time.
There is often information that radiation treatment of basal cell carcinoma does not have any serious consequences. Unfortunately, this is not true. Irradiation of skin basalioma causes a lot of complications, which impossible to avoid. Therefore, treating basal cell carcinoma with radiation is often comparable to shooting sparrows with a cannon, since the side effects of such treatment often exceed the severity of the disease itself.

This is what a radiation ulcer looks like
If at the beginning of treatment the skin in the training area only turns red and itches, then by the third week of therapy a non-healing bright red ulcer develops. It becomes very easily infected, has an extremely unpleasant odor, and heals with great difficulty only 1.5 months after the end of treatment.
2. A radiation ulcer always heals with the formation of a scar. This creates not only a defect in facial expressions, but also makes it very difficult to treat basal cell carcinoma in case of relapse.
3. It is impossible to predict in advance how radioactive particles will act. On the one hand, therapeutic radiation is aimed at rapidly dividing cells, and this is the main property of malignant neoplasms: radiation damages basal cell carcinoma cells and makes them non-viable.
But on the other hand, radiation exposure itself has high mutagenic properties. Healthy tissue is also exposed to radiation, and the DNA of healthy cells is damaged.
Thus, an initially safe basal cell carcinoma is highly likely to “degenerate” into metastatic forms of cancer - for example, squamous cell carcinoma skin.
The risk of developing this complication persists for the rest of your life after basal cell carcinoma irradiation. It is for this reason that radiation treatment is not given to patients under 50 years of age. Due to the high risks of complications, radiation treatment is not used for recurrent basal cell carcinoma.
4. If basal cell carcinoma occurs on the head, irradiation leads to hair loss in the affected area, which grows brittle and dull after treatment.
5. The risk of complications increases in proportion to the depth of penetration of basal cell carcinoma and the intensity of irradiation.
6. When treating tumors located near the eyes, cataracts may occur.
7. Treatment of basal cell carcinoma with radiation leads to changes in the functioning of the sebaceous and sweat glands in the area of radiation exposure.
8. Anatomically difficult areas are not treated with any of the methods of radiation therapy.
9. With radiation treatment of basal cell carcinomas on the face, the risk of relapse is higher than on other areas of the skin.

This is what a device for close-focus X-ray therapy looks like.
Since the depth of exposure to this radiation ranges from a few millimeters to 7–8 cm, the dosage and number of sessions are calculated individually.
Close-focus X-ray therapy is effective only in the initial stages of basal cell carcinoma and is used only on accessible areas of the skin. For example, the corner of the nose is considered difficult to treat.
This method also has its drawback. X-ray radiation is well absorbed dense fabrics- for example, bones. Therefore, when basal cell carcinoma is located close to the bone - in the area of the ears and on the head - electron radiation therapy is recommended.
Electronic therapy for basal cell carcinoma: features of the method and its disadvantages
Beta rays are called electrons. Accordingly, beta ray treatment is called electron therapy.
Compared to X-rays, electron radiation is considered more gentle, selective and highly targeted. Electrons are absorbed by tissues equally and regardless of their density. Unlike X-rays, whose energy is lost with increasing depth, uh The energy of the electron beam increases to a peak at a certain depth and then drops sharply.
All this means that with the correct dose calculation, radiation minimally injures healthy tissue around the tumor. Electronic therapy also allows irradiation of large areas of skin for multiple basal cell carcinomas.
But electronic therapy treatment also has limitations. On the one hand, this is the high cost of equipment. On the other hand, the technique is indicated in advanced stages - the size of the basal cell carcinoma should be no less than 4 cm2, since the device is quite labor-intensive to set up and does not allow focusing the flow onto a smaller area.
Electron irradiation is also not used to treat basal cell carcinoma in the eye area: modern radiology does not effectively protect the organ of vision.
The main disadvantage of all existing treatment methods is the high risk of relapse. As a result, you have to cut or irradiate again and again. Moreover, each stage of treatment is accompanied by significant loss of healthy tissue and scarring.
The need for deep tissue excision is a critical moment in the treatment of basal cell carcinomas on the face - especially on the nose, ears and corners of the lips, when each recurrence of basal cell carcinoma is accompanied by irreversible loss of a significant part of the organ.
Relapsebasal cell carcinomasin the rumen - perhaps the most terrible consequence treatment of basal cell carcinoma using classical methods
You need to understand that almost all existing treatment methods lead to the formation of a scar, which is a dense connective tissue, poorly penetrated by blood vessels and poorly supplied with blood. In this case, relapse of basal cell carcinoma occurs in the area of its original localization - that is, always in the scar area.
Unfortunately, in this case, PDT loses its effectiveness - the microcirculation of the rumen does not allow the photosensitizer to accumulate in sufficient concentration. Accordingly, recurrence of basal cell carcinoma in the scar is poorly amenable to any alternative treatment methods other than surgery.
So, having performed an operation to remove basal cell carcinoma just once, you become a hostage to the surgical method.
How to treat basaliomato cure. Treatment of basal cell carcinoma using PDT
PDT is an effective method of relapse-free treatment of basal cell carcinoma in one procedure.
Big personal experience treatment of basal cell carcinoma using PDT allows me to confidently say that:
- PDT in 96% of cases forever eliminates basal cell carcinoma in one procedure,
- Photodynamic treatment of basal cell carcinoma shows the highest efficiency among all existing techniques. The method targets cancer cells and fully eliminates them. The risk of recurrence of even large basal cell carcinoma after correct and fully performed PDT is several times lower than from other treatment methods and is only a few percent.
- Only the photodynamic method of treating basal cell carcinoma provides the highest aesthetic result: either no scar remains or it is almost invisible.
- The method is suitable for the most complex basal cell carcinomas in the nose and eyelids.
- PDT shows very good results in the treatment of large basal cell carcinomas.
- It has almost no side effects, since healthy cells are not harmed during PDT.
What is the essence of the technique
Photodynamic removal of skin basalioma begins with a dropper - a photosensitizer drug is injected into the patient’s blood, which increases the photosensitivity of tissues. The photosensitizer has the special property of being retained only in old, atypical, damaged and cancer cells.
2-3 hours after injection, the tissues are irradiated with a laser according to a special scheme. The photosensitizer is activated by light and enters into a complex photochemical reaction, which results in the release of toxic compounds and reactive oxygen species that destroy cancer cells.
The duration of the procedure depends on the size and number of tumors and takes from 20 minutes to 2.5 hours.
It is this targeted effect on cancer cells that ensures complete tumor removal and an excellent aesthetic result after the procedure.
Is it that simple?
Of course, the PDT procedure is not at all as simple as it might seem at first glance. To obtain a guaranteed result, it requires very high-quality equipment, the highest craftsmanship, jewelry precision and strictly individual developed treatment plan.
For every patient I I am developing my own treatment protocol, which depends on age, medical history, size and location of the tumor, and concomitant diseases.
I make sure to diagnose and differentiate the tumor:
- visual examination with dermatoscopy;
- collection of material for cytological evaluation;
- taking a fingerprint-smear in the case of an ulcerated form;
- taking a biopsy for tumors larger than 5 cm2.
This procedure allows you to accurately diagnose basal cell skin cancer and exclude the more aggressive squamous cell cancer.
Before the procedure, I carefully calculate the dosage of the photosensitizer, as well as the intensity and time laser exposure. I carefully control the power of laser radiation during the procedure.
Compliance with the PDT protocol and individual approach allows me to achieve good treatment results of 96% the first time.
By the way, not all specialists trained in PDT are able to trigger the necessary photochemical reaction and achieve a cure.

The photograph shows hyperthermia - a tissue burn that should not occur after a correctly performed PDT procedure. From the reaction of the tissues, I understand that no photochemical reaction occurred in this case, even if before the procedure the patient was injected with a photosensitizer and a laser was used. The treatment result shown in the photograph does not give the right to call it PDT. Therefore, after completion of treatment, the patient will not receive the benefits of the technique that I spoke about above.

The photochemical reaction may be accompanied by whitening of the tissue in the affected area, as shown in the photograph.

On days 14-20, a crust forms, under which epithelization occurs.
Rehabilitation
After the procedure, cyanosis appears at the site of treatment, which becomes covered with a black crust on days 14-20.
If the patient carefully follows the doctor’s requirements in the postoperative period for 4–6 weeks, after the PDT procedure a small and almost invisible scar remains on the skin. If a small basal cell carcinoma is removed, the tumor often disappears without a trace after PDT.
Why is the PDT method poorly represented in Europe and the USA?
According to statistics, in last years The number of people with skin cancer is rapidly increasing, regardless of their age and gender. Despite the use best practices diagnosis and treatment of oncological pathologies, to answer the question that worries everyone: “is it possible to cure skin cancer?” There is still no clear answer.
The concept of “skin cancer” includes a group of cancer neoplasms that develop from cells of various layers of the epidermis and are localized on the surface of the skin.
Depending on the structure of the affected cells, several forms of this disease are distinguished.
- All information on the site is for informational purposes only and is NOT a guide to action!
- Can give you an ACCURATE DIAGNOSIS only DOCTOR!
- We kindly ask you NOT to self-medicate, but make an appointment with a specialist!
- Health to you and your loved ones! Do not give up
Basalioma or basal cell carcinoma, develops from the upper layer of the epidermis, is the most common form of cancer pathology. Characterized by tissue germination and absence of metastases.
Squamous cell carcinoma originates from the cells of the spinous layer of the epidermis, develops against the background of skin pathology, and is diagnosed less frequently than basal cell carcinoma. This form is characterized by an aggressive course and metastasis in the early stages of development. With the development of this form, facial skin is damaged.
Metatypical cancer It has clinical manifestations, similar to the symptoms of basal cell carcinoma, but the features of the course are similar to the nature of the development of squamous cell carcinoma. This form occupies an intermediate position between these two types.
Melanoma develops from melanocytes - pigment cells of the epidermis. It is characterized by rapid development and extreme malignancy. May occur as a result of pathological changes in nevi (birthmarks).
Kaposi's sarcoma develops from the vascular endothelium, and is characterized by multifocal malignant lesions of the dermis and a variety of clinical forms. There are red, nodular, infiltrative, disseminated (lymphadenopathic) forms of the tumor. Kaposi's sarcoma is characterized by multiple bluish-red spots that gradually transform into tumor formations up to 5 cm in size.

The choice of the most effective treatment tactics depends on the form of the tumor, its location, degree of differentiation, extent of the process, and the age of the patient.
Video: Skin cancer. Types, symptoms, treatment
Surgical treatment (operation)
The main goal in the treatment of skin cancer is radical removal of the tumor, which is carried out by excision of the primary tumor to healthy tissue. Currently, there are several methods of surgical treatment.
Classic excision . This method is applicable to any form of tumor in the early stages of development. The surgeon removes the tumor, capturing 1-2 cm of the adjacent healthy skin. It is subsequently examined under a microscope for the presence cancer cells in intact tissue.
Microsurgery MOHS . This method is most effective in the development of basal cell carcinoma or squamous cell carcinoma. The peculiarity of this operation is the layer-by-layer removal of the tumor and instant microscopic examination of each layer for the presence of cancer cells. Sections are made until healthy tissue without cancer appears under the microscope. Microsurgery is performed to minimize the removal of healthy tissue and preserve the cosmetic effect.
Fulguration (electrocoagulation) and curettage . This simple method is also suitable for removing small squamous or basal forms. The operation is performed using a curette, a small spoon-shaped instrument. When damaged tissue is removed, an electrical current is applied to the area to destroy any remaining cancer cells and prevent bleeding. For complete removal it is necessary to carry out several stages of treatment.
Cryotherapy . This method is used to remove Kaposi's sarcoma, melanoma, basal cell carcinoma or squamous cell carcinoma when the tumor is small. The essence of the operation is to remove cancerous tumor liquid nitrogen, which is applied directly to the affected area.
As a result of shock freezing of a tumor, cancer cells are destroyed, but along with them, nerve damage can occur, which often leads to loss of sensitivity in this area.
Laser therapy . Removing cancer cells with a laser is a modern and highly effective method, since during layer-by-layer removal of affected tissue, which is carried out with high precision, healthy tissue is not injured. Laser therapy is performed quickly and under local anesthesia.
Radiation therapy
Very often, skin cancer is treated using laser therapy. At stages 1-2 of basal cell carcinoma development, with its small size, close-focus radiotherapy is indicated. In case of extensive damage, combined treatment using remote gamma therapy is prescribed.
This treatment method is indicated in the early stages tumor process, or after surgical removal squamous cell and metatypical cancer in case of relapse. It shows a good effect, since with the help of a powerful stream of radio rays the structure of cancer cells is destroyed, as a result of which they stop multiplying and die. In some situations, radiotherapy is prescribed in combination with the drug Prospidin.
Radiation therapy is prescribed to elderly people if primary tumor reaches a diameter of up to 20 mm. In this case, a tolerable radiation dose is selected, which is calculated individually for each patient. The advantage of radiation therapy is the destruction of cancer cells and the preservation of healthy, undamaged ones. However, after it is carried out, local complications may develop in the form of perichondritis, dermatitis, conjunctivitis.
If a patient is diagnosed with melanoma, radiation therapy is prescribed at the stage when the tumor begins to progress, and only in combination with chemotherapy or immunotherapy, since melanoma very often shows resistance to the effects of radiation.
If a patient develops Kaposi's sarcoma, namely when large painful lesions are identified, local exposure to radiation is carried out. However, this is only true for HIV-infected patients. For patients in the AIDS stage desired result almost impossible to achieve.
Chemotherapy
The chemotherapy method is the most effective field of surgical intervention. It is appointed in front of everyone possible forms skin cancer. Chemotherapy is especially effective when the tumor recurs or when the size of the tumor is critical, which prevents surgery. In this case, chemotherapy drugs are prescribed that destroy tumor cells.
For basal cell tumors, local chemotherapy is prescribed using external ointment for cancer (prospidin or 5-fluorouracil), which should be applied locally twice a day for several weeks.
Most often, chemotherapy involves the use of local applications using cytostatics (Fluorouracil, Doxorubicin, Metatrixate, etc.)
To know how to cure squamous cell skin cancer with chemotherapy, you should determine the stage of development of the process, since this method is effective only for small tumors or when relapses occur. The patient is prescribed local chemotherapy using 0.5% omain or 5-fluorouracil ointment. Otherwise, highly effective chemotherapy drugs are prescribed.
Metastatic epidermal cancer, which can cause lesions on the skin of the nose, cheeks, forehead and face in general, is treated in the same way as squamous cell carcinoma, since the clinical manifestations of both forms are almost similar.
For the treatment of melanoma, as a rule, chemotherapy is not indicated, or is indicated at the last stage of the disease, when extensive metastasis occurs and the primary tumor reaches a critical size. The destruction of cancer cells in both the primary and secondary tumors occurs when chemotherapy drugs are applied directly to the tumor.
When Kaposi's sarcoma is diagnosed, the patient is prescribed chemotherapy along with other treatment methods: antiretroviral therapy, interferon therapy. For a course of chemotherapy, Vinblastine, Vincristine, Prospidin, Taxol, Etoposide and other drugs of the latest generation are prescribed.
|
|
|
Modern methods allow you to expand your capabilities complete cure oncological diseases. But only depending on the form of skin cancer with a timely start and correctly chosen treatment protocol can one reliably determine whether skin cancer is curable and whether a recurrence is possible.
A large number of skin diseases are now known. Some of them are quite harmless, but there are also those that require special attention. This includes skin cancer. This pathology can develop in absolutely anyone; age and gender do not affect this in any way, but this disease is most often diagnosed in old age.
What is the disease
This pathology begins its development from squamous epithelial cells and is a cancerous tumor. Quite often such neoplasms can be seen on open areas of the body; on the limbs and trunk they form in only 10% of cases.
According to statistics, skin cancer on the face or other areas is often diagnosed; it ranks 3rd among cancer diseases.
Who is at risk
No one is immune from cancer pathologies, but there are categories of people whose risk of developing skin cancer is much greater. These include:
- Patients with fair skin are genetically designed to synthesize less melanin.
- Elderly people.
- Having a hereditary predisposition to the appearance various kinds neoplasms.
- Having precancerous diseases.
- Smokers.

- Bowen disease can also cause skin cancer.
- Patients diagnosed with xeroderma pigmentosum.
- Having inflammatory skin pathologies.
- Long-term exposure to ultraviolet rays.
Important. Visiting a solarium increases the risk of developing cancer several times.
A predisposition to a disease does not always mean that it will definitely develop. But often some factors become strong provocateurs and act as a trigger.
Causes of skin cancer
There are some causes that cause skin cancer:
- Constant contact with harmful substances, which have a carcinogenic effect on the body. These include: cigarette components, lubricants, arsenic compounds.
- Long-term impact on skin radioactive radiation.
- Constant exposure to thermal radiation.
- Mechanical injuries, damage to moles.
- Mechanical damage to old scars.
- Eating large amounts of foods that contain chemical additives, many of which may be carcinogenic.

The development of oncology is not always provoked by a single cause; most often, a complex influence of negative factors is observed.
Types of skin cancer
The skin contains a large number of cells belonging to various tissues. This is why developing tumors can differ from each other. Experts recognize several types of skin cancer:
- Squamous. It can form in different places, but usually on exposed areas and lips. The causes are often mechanical damage and scarring of tissue after a burn.
Important. In 30% of cases, old scars subsequently become the cause of the development of cancer.
- Basal skin cancer characterized by a tendency to relapse; the cause is most often a hereditary predisposition and problems in the functioning of the immune system. But experts also assign an important role in the development of pathology to the effects of carcinogens and ultraviolet radiation. Basalioma, as this type of cancer is also called, is often located on the head and can form single tumors or entire clusters.
- Cell cancer has a similar course to basal cell carcinoma, but can produce “sprouts”, which significantly worsens the prognosis for the patient.
- develops from pigment cells.
Skin cancer symptoms
Skin cancer symptoms can vary depending on the type of pathology, but there are general signs that always appear:
- Fatigue and rapid fatigue during any type of activity.
- Sudden weight loss for no apparent reason.

- Poor appetite.
- The temperature remains at 37 °C for a long time.
- The lymph nodes become enlarged and can be easily palpated.
- Moles can change their shape, color and size.
- If it is already a late stage of the disease, then pain also becomes a sign.
But each type of cancer has its own distinctive signs that allow specialists to diagnose them.
Manifestations of various types of cancer
When visiting an oncologist, the first thing the doctor examines is the patient and pays attention to his tumors. Often, just by external signs, the type of cancer can be preliminarily determined, and then the diagnosis can be confirmed by other studies.. It is the different manifestations that help doctors distinguish one type of tumor from another.
Important. Depending on the type of cancer, the signs of pathology will differ.
For ease of study, the information is presented in the table.
|
Type of skin cancer |
Symptoms |
|
|
Squamous cell carcinoma |
The neoplasm of this variety is often red in color, has a dense consistency, is lumpy and bleeds. The tumor grows rapidly and may appear as a plaque, ulcer or nodule. Sometimes the formation resembles cauliflower. This variety is different rapid growth and easily spreads in width and depth. |
|
|
Basal cell carcinoma |
Unlike the previous form, it grows slowly and can develop over many years, but is distinguished by the presence of a variety of external forms. It can be: nodular-ulcerative, warty, flat, pigmented. It usually begins with the appearance of a small gray or pinkish nodule with a pearlescent sheen. The neoplasm has a smooth surface, and there are scales in the center. The favorite place of education is the face. |
|
|
Melanoma |
This is a pigmented tumor that is dark in color, ranging from brown to black. During development, it can increase in different directions, so there are horizontal and vertical forms. This variety is considered the most dangerous, as it metastasizes and spreads quickly. It does not appear on its own, but necessarily occurs at the site of a mole, freckles or other heavily pigmented areas. The affected area often itches and swelling appears, which forces patients to consult a doctor. |
|
|
Adenocarcinoma |
It is less common than other varieties. Favorite places are areas with a high content of sweat and sebaceous glands. In appearance it resembles a small nodule or tubercle. It grows slowly, but during development it affects muscle tissue. |
|
Stages of development of skin cancer
All oncological pathologies They go through several stages in their development. The earlier the disease is diagnosed, the easier it is to treat. To recognize the extent of skin cancer, doctors may use computed tomography, blood tests, biopsies. Lymph nodes must be examined. Malignant skin tumors are characterized by the following stages of development:
- First. If skin cancer is at an early stage, then the tumor does not exceed 2 centimeters. Metastasis does not form, but the lower layers of the epidermis are affected. If therapy is started at this stage, then almost complete recovery occurs.

- Stage 2 cancer characterized by an increase in formation up to 4 centimeters. Sometimes, already at this stage, metastases can be detected in a neighboring lymph node. The site of injury causes discomfort and sometimes pain to the patient. The tumor grows into all layers of the skin. Therapy at this stage leads to recovery in 50% of cases.

- Stage 3 cancer affects the lymph nodes, but metastases have not yet penetrated the organs. The neoplasm takes on a lumpy appearance, and the patient experiences discomfort. The prognosis is favorable for only 30% of patients.
Need to know. At this stage of the disease, patients often experience elevated temperature bodies.
- Stage 4. The tumor is more than 5 centimeters in diameter. It has uneven outlines, the top is covered with crusts and bleeding ulcers. Patients lose a lot of weight, constantly feel weak, headache. Metastases appear in the lungs, liver and bones. Even after treatment, only 20% of patients survive.

You should know it. Basal cell cancer does not have stages in its development; the tumor simply gradually increases and negatively affects neighboring tissues.
Skin cancer treatment
The choice of therapy method is influenced by several factors:
- Stage of development of the neoplasm.
- The presence of concomitant diseases in the patient.
- General condition of the body.
- Patient's age.
- Location and type of cancer.
Important. Oncological diseases of the skin respond quite well to therapy if it is started in a timely manner.
TO modern methods treatments include:
- Radiation therapy.
- Laser treatment.
- Surgical removal of the tumor.
- Cryodestruction.
- Drug therapy.
Sometimes, to achieve a complete cure, you have to resort to several types of therapy at once..
Getting rid of cancer with radiation therapy
Irradiation of skin cancer is a fairly effective method, since malignant cells are quite sensitive to radiation. The latest treatment regimens have now been developed that allow minimal impact on healthy cells.
Radiation therapy is often prescribed:
- If there are contraindications to surgery or general anesthesia.
- There is a relapse of the disease.
- A good cosmetic effect is important.
- The tumor is large.
- Located away from important organs.

Important. For each patient, the radiation dose is selected strictly individually, as well as the duration of treatment and the number of procedures. If such therapy is carried out at the first stage of cancer, the effectiveness reaches 95%.
Chemotherapy
This type of therapy involves introducing substances into the body that are harmful to cancer cells.. Indications for such treatment are:
- Recurrence of basal cell carcinoma.
- Large tumors that cannot be operated on.
- Stages 3 and 4 cancer.
Medicines can be used externally, or do intravenous injections. The effectiveness of this method is good when it is an addition to radiation therapy or surgical removal of the tumor.

Safe treatments
They are also called gentle and include:
- Cryotherapy- freeze the tumor and cut it off.
- Laser treatment carried out using a laser, which burns out the tumor.
- Local therapy. It involves the use of drugs administered using electrophoresis, they stop the growth of malignant cells.
It is important to know. Skin cancer treatment should be carried out only in an oncology clinic. Folk remedies To get rid of the disease, you can use it at your own peril and risk.
How to prevent the development of the disease
How skin cancer manifests itself is now clear, but the question arises: is it possible to prevent the development of pathology? Everyone knows that preventing any disease is much easier than treating it later. This also applies to cancer. Preventing skin cancer involves following these recommendations:
- Everyone is looking forward to a vacation to go closer to the sea and soak up the warm rays of the sun, but this is not at all safe for health. It is necessary to protect your skin from prolonged exposure to ultraviolet radiation.
Important. Tanning is harmful to health and has serious consequences.
- Every time you go outside in the summer, use sunglasses and protective creams.

A tanned body is beautiful, but prolonged exposure to direct sunlight does not have the best effect on our skin.
- If there are long-term non-healing wounds or ulcers on the skin, then you need to see a doctor.
- If there are old scars, they should be protected from mechanical irritation.
- Pay attention to moles; if their shape or color changes, visit an oncologist.
- Lead a healthy lifestyle.
- Limit consumption of foods containing carcinogens.
- When working with household chemicals, be sure to use gloves.
- Any skin diseases treat in a timely manner.
Among all cancer pathologies, skin cancer is considered highly treatable. It is easy to diagnose, and can be cured in one day if you contact a specialist at the very beginning of the development of the disease.
It is important not to waste time, and for this you just need to be more attentive to yourself and your health.
All methods treatment of squamous cell skin cancer are aimed at radical removal of the tumor focus and obtaining a lasting clinical cure. The choice of treatment method depends on the shape of the tumor, stage, localization, extent of the process, the presence of metastases, age and general condition of the patient. Thus, solar-induced squamous cell carcinoma of the skin has a lower level of metastasis compared to squamous cell carcinoma that developed against the background of foci of chronic inflammation, scars or chronic radiation dermatitis, which should be taken into account when performing surgery. Tumors of the lips, ears and nose have a higher level of metastasis, however, such localization does not allow for wide excision of the formations, so they must be treated with methods that allow microscopic control of the marginal zone of the removed tumor. Recurrent tumors are also aggressive and often localized. Regarding the size of the tumor, it is known that squamous cell skin cancer, the diameter of which exceeds 2 cm, recurs and metastasizes more often and therefore requires treatment with more radical methods.
To histological features that determine tactics treatment of patients with squamous cell skin cancer, include the degree of differentiation, depth of invasion and the presence of perineural spread of the tumor. Patients with well-differentiated squamous cell carcinoma have a better prognosis than with poorly differentiated ones, because low-grade cancer is more aggressive and has a higher rate of recurrence and metastasis. Tumors with a lower level of invasion, growing only into the papillary layer of the dermis, have a significantly lower frequency of recurrence and metastasis than tumors that deeply invade the dermis, subcutaneous fatty tissue or having perineural invasion. Squamous cell skin cancer also occurs more aggressively in patients with immunosuppression (recipients of internal organ transplants, patients with lymphoma, AIDS, etc.), with a higher risk of recurrence, metastasis and fatal outcome. Their treatment should be carried out with radical methods, as well as patients with palpable lymph nodes, since this may be a sign of metastasis.
The oldest, but which has not lost its significance up to the present time, is surgical treatment for squamous cell skin cancer, which for small tumors is based on excision of the tumor within healthy skin, retreating 1-2 cm from the edge of the tumor, with or without subsequent plastic surgery. This gives not only a good cosmetic result, but also the opportunity to obtain adequate material for pathomorphological examination. Larger and more aggressive tumors are removed more widely. Large tumors require the removal of a significant amount of tissue and sometimes amputation, for example of a finger or penis. If tumor removal is performed adequately, the cure rate within 5 years is 98%.
Exclusively important at surgical treatment squamous cell skin cancer has the Mohs method with microscopic control of the marginal zone of the removed tumor at the moment surgical intervention, which allows you to achieve a high cure rate (up to 99%) and preserve a maximum of normal skin around the lesion. The lowest level of recurrence while maintaining a good cosmetic effect is achieved by removing tumors within a 4 mm zone of apparently healthy skin. This method is also advisable to use for poorly differentiated and metastatic skin cancers.
TO surgical methods Treatments also include electrocoagulation and juoretage, which are used for small tumor diameters (up to 2 cm) and minor invasion. More often, electrocoagulation is used for squamous cell skin cancer with a diameter of less than 1 cm, located on smooth surfaces of the skin (forehead, cheek, torso) and having a depth of invasion within the dermis or upper subcutaneous tissue. Electrocoagulation is also indicated for the treatment of small-diameter squamous cell skin cancer that develops against the background of foci of chronic radiation dermatitis. When performing electrocoagulation, it is necessary to capture 5-6 mm of healthy skin adjacent to the tumor. Sometimes electrocoagulation and curettage are combined with cryotherapy. The advantages of the method include a high cure rate, simplicity of the method, as well as the formation of a cosmetically satisfactory scar due to the rapid and complete subsequent healing of the skin. The method does not allow obtaining adequate material for histological control of the edges of the removed tumor and therefore requires careful monitoring of patients over a long period of time.
Cryodestruction of squamous cell skin cancer It is performed only for small superficial and highly differentiated tumors located on the body. It is carried out using a cryoprobe (but in no case with a cotton swab) or using the aerosol method; exposure time - 5 minutes with repeated thawing from 2 to 5 times and capturing healthy skin by 2-2.5 cm. Due to the fact that with this method histological control of the edges of the removed tumor is impossible, the procedure must be preceded by a biopsy confirming that the tumor is superficial and highly differentiated. In hand experienced doctor If you carefully observe the indications and contraindications for cryodestruction, treatment with this method can be very effective, providing a cure in 95% of cases. However, it should be taken into account that the healing period during cryodestruction ranges from 2 to 4 weeks, and after treatment an atrophic hypopigmented scar is formed.
Application of laser radiation in the treatment of squamous cell skin cancer carried out by two methods: by photothermal destruction (coagulation, excision) of the tumor and in the form of photodynamic therapy.
For excision of squamous cell skin cancer A carbon dioxide laser can be used in a focused mode, which reduces the likelihood of bleeding (due to coagulation of small vessels during treatment) and scar formation, thereby providing a good cosmetic result. The use of a focused laser beam to remove this tumor is especially indicated for patients receiving anticoagulant therapy or suffering from bleeding diseases.
In order to reduce the intensity of exposure laser coagulation, as a rule, use neodymium and carbon dioxide lasers in defocused mode. Laser coagulation is especially indicated for squamous cell cancer of the nail bed and penis.
Photodynamic therapy for squamous cell skin cancer is a combination of exposure to light radiation (wavelength from 454 to 514 nm) with drug therapy photosensitizers (for example, hematoporphyrins), which leads to necrosis of tumor cells. However, the effectiveness of its use in squamous cell skin cancer has not yet been studied sufficiently.
Squamous cell skin cancer small lesions can be successfully treated with close-focus X-rays, although, in general, radiation therapy is rarely used in the treatment of primary squamous cell carcinoma of the skin. She happens to be alternative method treatment, and with appropriate selection of patients ensures their cure in more than 90% of cases. The method is most effective in the treatment of deeply invasive skin tumors located along the closure lines of the embryonic ectoderm (nasolabial folds, parotid areas, etc.); when the tumor is localized near natural openings (eyes, nose, ears, etc.). Radiation therapy is also used to suppress metastases. It is indicated in some cases after surgery in patients with a high risk of metastasis; for recurrent tumors that have arisen after the use of other treatment methods, as well as as a palliative method of treatment in patients with inoperable tumors. It is the method of choice in the treatment of elderly patients and in the presence of severe concomitant pathology.
Usually for older people radiation therapy for squamous cell skin cancer carried out with a tumor diameter of up to 20 mm. One of the conditions that ensures the effectiveness of treatment is the preservation of the viability of healthy tissues located in the area of radiation exposure. In this regard, the dose of radiation exposure must be tolerable (tolerable). The irradiation regimen depends on the location and size of the tumor, as well as the degree of cellular differentiation. It should be taken into account that highly differentiated squamous cell skin cancer requires higher doses of radiation than poorly differentiated ones. The radiation dose varies from 3 to 5 Gy/day; per course - from 50 to 80 Gy. Before X-ray therapy, exophytic lesions are cut off using a scalpel or by electrodissection. An electron beam is used to treat large superficial skin tumors. A significant disadvantage of radiation therapy is the development local complications(radiation dermatitis, conjunctivitis, cataracts, perichondritis). which are observed in approximately 18% of cases. Although the immediate cosmetic outcome after radiation therapy may be good, it sometimes worsens over time, including the development of chronic radiation dermatitis. In this case, at the site of previous irradiation, the skin becomes atrophic, hypopigmented with the presence of telangiectasia. For recurrent tumors, repeated radiation therapy is not performed.