Methodological development No. 2
for a practical lesson on radiation diagnostics for 3rd year students of the Faculty of Medicine
Topic: Basic methods of radiation diagnostics
Completed by: intern Peksheva M.S.
Basic methods of radiation diagnostics:
1. X-ray based methods:
· Fluorography
Traditional radiography, fluoroscopy
· X-ray CT scan
· Angiography (x-ray contrast studies)
2. Ultrasound based methods:
General ultrasound examination
· Echocardiography
· Dopplerography
3. Methods based on the NMR effect:
MR spectroscopy
4. Methods based on the use of radionuclide preparations
Radionuclide diagnostics
Positron emission tomography
Radioimmunoassay in vitro
5. Invasive procedures in treatment and diagnosis, carried out under the control of radiation research methods:
· Interventional radiology.
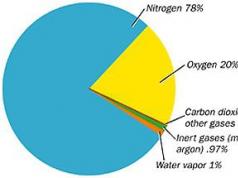
Properties of X-rays:
· Able to penetrate bodies and objects that absorb or reflect (i.e. do not transmit) visible light rays.
· Like visible light, they can create a latent image on a photosensitive material (photo or X-ray film), which becomes visible after development
· Cause fluorescence (glow) of a number of chemical compounds used in fluoroscopic screens
· They have high energy and are capable of causing the decay of neutral atoms into + and – charged particles (ionizing radiation).
Traditional radiography .
Radiography (x-ray photography) is a method of x-ray examination in which a fixed x-ray image of an object is obtained on a solid medium, in the vast majority of cases on x-ray film. In digital X-ray machines, this image can be recorded on paper, in magnetic or magnetic-optical memory, and obtained on a display screen.
An X-ray tube is a vacuum glass vessel, into the ends of which two electrodes are soldered - a cathode and an anode. The latter is made in the form of a thin tungsten spiral, around which, when heated, a cloud of free electrons is formed (thermionic emission). Under the influence of high voltage applied to the poles of the X-ray tube, they are accelerated and focused on the anode. The latter rotates at enormous speed - up to 10 thousand revolutions per minute, so that the flow of electrons does not hit one point and does not cause the anode to melt due to its overheating. As a result of electron braking at the anode, part of their kinetic energy is converted into electromagnetic radiation.
A typical X-ray diagnostic apparatus includes a power supply device, an emitter (X-ray tube), a device for beam collimation, an X-ray exposure meter and radiation receivers.
Radiographs can provide images of any part of the body. Some organs are clearly visible in the images due to natural contrast (bones, heart, lungs). Other organs are clearly visible only after artificial contrasting (bronchial tubes, blood vessels, bile ducts, heart cavities, stomach, intestines). In any case, the x-ray picture is formed from light and dark areas. Blackening of X-ray film, like photographic film, occurs due to the reduction of metallic silver in its exposed emulsion layer. To do this, the film is subjected to chemical and physical processing: developed, fixed, washed, dried. In modern X-ray rooms, the entire film processing process is automated thanks to the presence of developing machines. It should be remembered that an x-ray image is a negative in relation to the image visible on a fluorescent screen when transilluminated, therefore areas of the body that are transparent to x-rays on x-rays appear dark (“darkening”), and denser areas appear light (“clearance”).
Indications for radiography are very broad, but in each specific case they must be justified, since X-ray examination is associated with radiation exposure. Relative contraindications include an extremely serious condition or severe agitation of the patient, as well as acute conditions, which require emergency surgical care (for example, bleeding from a large vessel, open pneumothorax).
The radiography method has the following advantages:
· the method is quite simple to perform and is widely used;
· X-ray is an objective document that can be stored for a long time;
· comparison of image features on repeated images taken at different times makes it possible to study the dynamics of possible changes pathological process;
· relatively low radiation exposure (compared to the X-ray mode) on the patient.
Disadvantages of radiography
· difficulty assessing organ function.
· The presence of ionizing radiation that can have a harmful effect on the organism being studied.
· The information content of classical radiography is significantly lower than such modern medical imaging methods as CT, MRI, etc. Conventional X-ray images reflect the projection layering of complex anatomical structures, that is, their summation X-ray shadow, in contrast to the layer-by-layer series of images obtained by modern tomographic methods.
· Without the use of contrast agents, radiography is of little information for analyzing changes in soft tissues.
X-ray – a method of obtaining an X-ray image on a luminous screen.
IN modern conditions the use of a fluorescent screen is not justified due to its low luminosity, which forces research to be carried out in a well-darkened room and after long adaptation of the researcher to the dark (10-15 minutes) to distinguish a low-intensity image. Instead of classical fluoroscopy, X-ray television transillumination is used, in which X-rays fall on an X-ray image intensifier (X-ray image intensifier), which includes an image intensifier (electron-optical converter). The resulting image is displayed on the monitor screen. Displaying an image on a monitor screen does not require light adaptation of the researcher, nor does it require a darkened room. In addition, additional image processing and its recording on videotape or device memory is possible.
Advantages:
· The fluoroscopy technique is simple and economical, it allows you to examine the patient in various projections and positions (multi-axial and polypositional examination), evaluate the anatomical, morphological and functional features the organ being studied.
· The main advantage over radiography is the fact of research in real time. This allows you to evaluate not only the structure of the organ, but also its displacement, contractility or distensibility, passage of the contrast agent, and filling.
· Fluoroscopy allows you to monitor the implementation of some instrumental procedures - placement of catheters, angioplasty (see angiography), fistulography.
However, the method has certain disadvantages:
· significant radiation exposure to the patient, the magnitude of which is directly dependent on the size of the field being studied, the duration of the study and a number of other factors; relatively low resolution
· the need for special arrangement of the X-ray room (its location in relation to other departments, the street, etc.)
· the need to use protective devices (aprons, screens)
Digital technologies in fluoroscopy can be divided into:
Full frame method
This method is characterized by obtaining a projection of the entire area of the object under study onto an X-ray sensitive receiver (film or matrix) of a size close to the size of the area. The main disadvantage of the method is scattered X-ray radiation. During primary irradiation of an entire area of an object (for example, a human body), some of the rays are absorbed by the body, and some are scattered to the sides, which additionally illuminates the areas that were initially absorbed by the X-ray beam. This reduces the resolution and creates areas where the projected points are illuminated. The result is an X-ray image with a decrease in the range of brightness, contrast and image resolution. During a full-frame examination of a body area, the entire area is irradiated simultaneously. Attempts to reduce the amount of secondary scattered radiation by using a radiographic raster leads to partial absorption of X-rays, but also to an increase in the intensity of the source and an increase in the radiation dosage.[edit]
Scanning method
Single-line scanning method: The most promising is the scanning method of obtaining an x-ray image. That is, an X-ray image is obtained by a certain beam of X-rays moving at a constant speed. The image is recorded line by line (single line method) by a narrow linear X-ray sensitive matrix and transferred to a computer. At the same time, the irradiation dosage is reduced hundreds or more times, images are obtained with virtually no loss in the range of brightness, contrast and, most importantly, volumetric (spatial) resolution.
Multi-line scanning method: Unlike the single-line scanning method, the multi-line scanning method is the most effective. With the single-line scanning method, due to the minimum size of the X-ray beam (1-2mm), the width of the single-line matrix of 100 µm, the presence of various types of vibrations, equipment backlash, additional repeated irradiations are obtained. By using multi-line scanning technology, it was possible to reduce secondary scattered radiation by hundreds of times and reduce the intensity of the X-ray beam by the same amount. At the same time, all other indicators of the resulting X-ray image have been improved: brightness range, contrast and resolution.
X-ray fluorography - represents large-frame photographing of an image from an X-ray screen (frame format 70x70 mm, 100x100 mm, 110x110 mm). The method is intended for conducting mass preventive examinations of the chest organs. The sufficiently high image resolution of large-format fluorograms and lower cost also make it possible to use the method for studying patients in a clinic or hospital.
Digital radiography : (MCRU)
based on the direct conversion of the energy of X-ray photons into free electrons. A similar transformation occurs when an X-ray beam passing through an object acts on plates of amorphous selenium or amorphous semi-crystalline silicone. For a number of reasons, this X-ray method is currently used only for examining the chest. Regardless of the type of digital radiography, the final image is saved on various types of media, either as a hard copy (reproduced using a multi-format camera on special film) or using a laser printer on writing paper.
The advantages of digital radiography include
· high image quality,
· the ability to save images on magnetic media with all the ensuing consequences: ease of storage, the ability to create organized archives with quick access to data and transfer images over distances - both inside and outside the hospital.
In addition to general x-ray (room design and location), the disadvantages include the high cost of equipment.
Linear tomography:
Tomography (from the Greek tomos - layer) is a method of layer-by-layer x-ray examination.
The tomographic effect is achieved through continuous movement during imaging of two of the three components of the X-ray emitter-patient-film system. Most often, the emitter and film move while the patient remains motionless. In this case, the emitter and the film move in an arc, a straight line or a more complex trajectory, but always in opposite directions. With this movement, the image of most of the details on the x-ray image turns out to be unclear, smeared, and the image is sharp only of those formations that are located at the level of the center of rotation of the emitter-film system. Indications for tomography are quite wide, especially in institutions that do not have a CT scanner. Tomography is most widely used in pulmonology. Tomograms provide an image of the trachea and large bronchi without resorting to artificial contrast. Tomography of the lungs is very valuable for identifying cavities of decay in areas of infiltration or in tumors, as well as for detecting hyperplasia of the intrathoracic lymph nodes. It also makes it possible to study the structure of the paranasal sinuses and larynx, and to obtain an image of individual details of such a complex object as the spine.
Image quality is based on:
· Characteristics of X-ray radiation (mV, mA, time, dose (EDE), homogeneity)
Geometry (focal spot size, focal length, object size)
Type of device (screen-film device, memory phosphor, detector system)
Directly determine image quality:
Dynamic range
Contrast sensitivity
Signal-to-noise ratio
· Spatial resolution
Indirectly affect image quality:
· Physiology
· Psychology
· Imagination\fantasy
· Experience/awareness
Classification of X-ray detectors:
1. Screen-film
2. Digital
Based on memory phosphors
Based on URI
Based on gas discharge chambers
Based on semiconductors (matrix)
On phosphate plates: special cassettes on which many images can be taken (reading images from the plate to the monitor, the plate stores the image for up to 6 hours)
CT scan is a layer-by-layer x-ray study based on computer reconstruction of the image obtained by circular scanning of an object with a narrow beam of x-ray radiation.
A narrow beam of X-ray radiation scans the human body around the circumference. Passing through tissue, radiation is attenuated according to the density and atomic composition of these tissues. On the other side of the patient there is a circular system of X-ray sensors, each of which (and their number can reach several thousand) converts the radiation energy into electrical signals. After amplification, these signals are converted into a digital code, which is stored in the computer's memory. The recorded signals reflect the degree of attenuation of the X-ray beam (and, therefore, the degree of absorption of radiation) in any one direction. Rotating around the patient, the X-ray emitter “views” his body from different angles, for a total of 360°. By the end of the rotation of the emitter, all signals from all sensors are recorded in the computer memory. The duration of rotation of the emitter in modern tomographs is very short, only 1-3 s, which makes it possible to study moving objects. When using standard programs, the computer reconstructs the internal structure of the object. As a result, an image of a thin layer of the organ being studied is obtained, usually about a few millimeters, which is displayed on the display, and the doctor processes it in relation to the task assigned to him: he can scale the image (increase and decrease), highlight areas of interest (zones of interest), determine the size of the organ, the number or nature of pathological formations. Along the way, the tissue density in individual areas is determined, which is measured in conventional units - Hounsfield units (HU). The density of water is taken as zero. Bone density is +1000 HU, air density is -1000 HU. All other tissues of the human body occupy an intermediate position (usually from 0 to 200-300 HU). Naturally, such a range of densities cannot be displayed either on a display or on photographic film, so the doctor selects a limited range on the Hounsfield scale - a “window”, the dimensions of which usually do not exceed several tens of Hounsfield units. Window parameters (width and location on the entire Hounsfield scale) are always indicated on CT scans. After such processing, the image is placed in the long-term memory of a computer or dumped onto a solid medium - photographic film.
Spiral tomography is rapidly developing, in which the emitter moves in a spiral relative to the patient’s body and thus captures, in a short period of time, measured in a few seconds, a certain volume of the body, which can subsequently be represented by separate discrete layers.
Spiral tomography initiated the creation of new imaging methods - computed angiography, three-dimensional (volumetric) imaging of organs and, finally, virtual endoscopy.
Generations of computed tomographs: from the first to the fourth
The progress of CT tomographs is directly related to the increase in the number of detectors, that is, with an increase in the number of simultaneously collected projections.
1. The 1st generation device appeared in 1973. The first generation CT machines were step-by-step. There was one tube aimed at one detector. Scanning was carried out step by step, making one revolution per layer. One image layer was processed for about 4 minutes.
2. In the 2nd generation of CT devices, a fan type design was used. Several detectors were installed on the rotation ring opposite the X-ray tube. The image processing time was 20 seconds.
3. The 3rd generation of computed tomography scanners introduced the concept of spiral computed tomography. The tube and detectors synchronously performed full clockwise rotation in one step of the table, which significantly reduced the research time. The number of detectors has also increased. Processing and reconstruction times have decreased markedly.
4. The 4th generation has 1088 fluorescent sensors located throughout the gantry ring. Only the X-ray tube rotates. Thanks to this method, the rotation time was reduced to 0.7 seconds. But there is no significant difference in image quality with 3rd generation CT devices.
Spiral computed tomography
Spiral CT is used in clinical practice since 1988, when Siemens Medical Solutions introduced the first helical CT scanner. Spiral scanning consists of simultaneous performance of two actions: continuous rotation of the source - the X-ray tube generating radiation around the patient's body, and continuous translational movement of the table with the patient along longitudinal axis z scanning through the gantry aperture. In this case, the trajectory of the X-ray tube, relative to the z-axis - the direction of movement of the table with the patient's body, will take the shape of a spiral. Unlike sequential CT, the speed of movement of the table with the patient’s body can take arbitrary values, determined by the purposes of the study. The higher the table speed, the greater the extent of the scanning area. It is important that the table path length for one rotation of the X-ray tube can be 1.5-2 times greater than the thickness of the tomographic layer without deteriorating the spatial resolution of the image. Spiral scanning technology has made it possible to significantly reduce the time spent on CT examinations and significantly reduce the radiation dose to the patient.
Multilayer computed tomography (MSCT). Multilayer (“multislice”) computed tomography with intravenous contrast enhancement and three-dimensional image reconstruction. Multislice (“multislice”, “multi-slice” computed tomography - msCT) was first introduced by Elscint Co. in 1992. The fundamental difference between MSCT tomographs and spiral tomographs of previous generations is that not one, but two or more rows of detectors are located around the gantry circumference. In order for X-ray radiation to be simultaneously received by detectors located on different rows, a new one was developed - volumetric geometric shape beam. In 1992, the first two-slice (double-helix) MSCT tomographs with two rows of detectors appeared, and in 1998 - four-slice (four-helix) MSCT scanners, with four rows of detectors, respectively. In addition to the above-mentioned features, the number of rotations of the X-ray tube was increased from one to two per second. Thus, fifth-generation quad-slice MSCT scanners are currently eight times faster than conventional fourth-generation spiral CT scanners. In 2004-2005, 32-, 64- and 128-slice MSCT tomographs were introduced, including those with two X-ray tubes. Today, some hospitals already have 320-slice CT scanners. These tomographs, first introduced in 2007 by Toshiba, represent a new stage in the evolution of X-ray computed tomography. They allow not only to obtain images, but also make it possible to observe, almost in “real” time, the physiological processes occurring in the brain and heart. A feature of such a system is the ability to scan an entire organ (heart, joints, brain, etc.) in one revolution of the radiation tube, which significantly reduces the examination time, as well as the ability to scan the heart even in patients suffering from arrhythmias. Several 320 slice scanners have already been installed and are operating in Russia.
Preparation:
Special preparation of the patient for CT scanning of the head, neck, chest cavity and extremities is not required. When examining the aorta, inferior vena cava, liver, spleen, kidneys, the patient is recommended to limit himself to a light breakfast. The patient must appear for a gallbladder examination on an empty stomach. Before CT scanning of the pancreas and liver, measures must be taken to reduce flatulence. To more clearly differentiate the stomach and intestines during CT scanning of the abdominal cavity, they are contrasted by fractional ingestion by the patient before examination of about 500 ml of a 2.5% solution of a water-soluble iodide contrast agent. It should also be taken into account that if on the eve of the CT scan the patient underwent an X-ray examination of the stomach or intestines, then the barium accumulated in them will create artifacts in the image. In this regard, a CT scan should not be prescribed until the digestive canal is completely emptied of this contrast agent.
An additional CT technique has been developed - enhanced CT. It consists of performing tomography after intravenous administration of a water-soluble contrast agent to the patient (perfusion). This technique helps to increase the absorption of X-ray radiation due to the appearance of a contrast solution in the vascular system and parenchyma of the organ. At the same time, on the one hand, the contrast of the image increases, and on the other, highly vascularized formations are highlighted, for example, vascular tumors, metastases of some tumors. Naturally, against the background of an enhanced shadow image of the organ parenchyma, poorly vascular or completely avascular zones (cysts, tumors) are better identified.
Some CT scanner models are equipped with cardiac synchronizers. They turn on the emitter at precisely specified times - in systole and diastole. The cross-sections of the heart obtained as a result of such a study make it possible to visually assess the state of the heart in systole and diastole, calculate the volume of the heart chambers and ejection fraction, and analyze indicators of general and regional contractile function of the myocardium.
Computed tomography with two radiation sources . DSCT- Dual Source Computed Tomography.
In 2005, Siemens Medical Solutions introduced the first device with two X-ray sources. The theoretical prerequisites for its creation were already in 1979, but technically its implementation was impossible at that moment. In fact, it is one of the logical continuations of MSCT technology. The fact is that when examining the heart (CT coronary angiography), it is necessary to obtain images of objects that are in constant and rapid motion, which requires a very short scanning period. In MSCT, this was achieved by synchronizing the ECG and conventional examination with rapid rotation of the tube. But the minimum period of time required to register a relatively stationary slice for MSCT with a tube rotation time of 0.33 s (≈3 revolutions per second) is 173 ms, that is, the time of half a rotation of the tube. This temporal resolution is quite sufficient for normal heart rates (studies have shown effectiveness at rates less than 65 beats per minute and around 80, with an interval of low effectiveness between these indicators and at higher values). For some time they tried to increase the rotation speed of the tube in the gantry tomograph. Currently, the limit of technical possibilities for its increase has been reached, since with a tube rotation of 0.33 s its weight increases 28 times (overload 28 g). To obtain a temporal resolution of less than 100 ms, overloads of more than 75 g are required. The use of two X-ray tubes located at an angle of 90° gives a time resolution equal to a quarter of the tube's rotation period (83 ms with a rotation of 0.33 s). This made it possible to obtain images of the heart regardless of the frequency of contractions. Also, such a device has another significant advantage: each tube can operate in its own mode (at different voltage and current values, kV and mA, respectively). This allows you to better differentiate closely located objects of different densities in the image. This is especially important when contrasting vessels and formations located close to bones or metal structures. This effect is based on different absorption of radiation when its parameters change in a mixture of blood + iodine-containing contrast agent, while this parameter remains unchanged in hydroxyapatite (bone base) or metals. Otherwise, the devices are conventional MSCT devices and have all their advantages.
Indications:
· Headache
Head injury not accompanied by loss of consciousness
· Fainting
· Exclusion of lung cancer. If computed tomography is used for screening, the study is done as planned.
· Severe injuries
Suspicion of cerebral hemorrhage
Suspicion of vessel injury (eg, dissecting aortic aneurysm)
· Suspicion of some other acute injuries of hollow and parenchymal organs (complications of both the underlying disease and as a result of the treatment)
· Most CT scans are done routinely, upon the direction of a doctor, to finally confirm the diagnosis. As a rule, before performing a computed tomography, simpler studies are done - x-rays, ultrasound, tests, etc.
· To monitor treatment results.
· For carrying out therapeutic and diagnostic procedures, for example, puncture under the control of computed tomography, etc.
Advantages:
· Availability of a machine operator’s computer, which replaces the control room. This improves control over the progress of the study, because the operator is located directly in front of the lead-lined viewing window; the operator can also monitor the patient’s vital parameters directly during the examination.
· There was no longer a need to equip a darkroom due to the introduction of a developing machine. There is no longer any need to manually develop photographs in tanks with developer and fixer. Also, dark vision adaptation is not required to work in a darkroom. A supply of film is loaded into the developing machine in advance (like a regular printer). Accordingly, the characteristics of the air circulating in the room have improved, and the work comfort for personnel has increased. The process of developing photographs and their quality have accelerated.
· The quality of the image has improved significantly, making it possible to process it on a computer and store it in memory. There was no need for X-ray film or archives. It became possible to transmit images over cable networks and process them on a monitor. Methods of volumetric visualization have appeared.
High spatial resolution
· Speed of examination
Possibility of 3-dimensional and multi-planar image reconstruction
Low operator-dependency of the method
Possibility of standardization of research
· Relative availability of equipment (in terms of number of devices and cost of examination)
Advantages of MSCT over conventional spiral CT
o improved time resolution
o improved spatial resolution along the longitudinal z axis
o increased scanning speed
o improved contrast resolution
o increasing the signal-to-noise ratio
o efficient use of the X-ray tube
o large anatomical coverage area
o reducing radiation exposure to the patient
Flaws:
· The relative disadvantage of CT is the high cost of the study compared to conventional ones X-ray methods. This limits the widespread use of CT to strict indications.
· Presence of ionizing radiation and use of radiocontrast agents
Some absolute and relative contraindications :
No contrast
· Pregnancy
With contrast
· Allergy to contrast agent
· Kidney failure
· Severe diabetes mellitus
· Pregnancy (teratogenic effects of X-ray radiation)
· Severe general condition of the patient
Body weight greater than maximum for the device
· Thyroid diseases
Myeloma
Angiography is an X-ray examination of blood vessels performed using contrast agents. For artificial contrast, a solution of an organic iodine compound intended for this purpose is injected into the blood and lymphatic channels. Depending on which part of the vascular system is contrasted, arteriography, venography (phlebography) and lymphography are distinguished. Angiography is performed only after a general clinical examination and only in cases where it is not possible to diagnose the disease using non-invasive methods and it is assumed that, based on the picture of the vessels or the study of blood flow, it is possible to identify damage to the vessels themselves or their changes in diseases of other organs.
Indications:
· to study hemodynamics and identify vascular pathology itself,
· diagnosis of damage and malformations of organs,
· recognition of inflammatory, dystrophic and tumor lesions that cause
· their dysfunction and vascular morphology.
· Angiography is a necessary step when performing endovascular operations.
Contraindications:
· extremely serious condition of the patient,
acute infectious, inflammatory and mental diseases,
· severe cardiac, hepatic and renal failure,
· hypersensitivity to iodine preparations.
Preparation:
· Before the study, the doctor must explain to the patient the need and nature of the procedure and obtain his consent to perform it.
· The evening before the angiography, tranquilizers are prescribed.
· Breakfast is canceled in the morning.
· The hair in the puncture area is shaved.
· 30 minutes before the examination, premedication is performed (antihistamines,
tranquilizers, analgesics).
The favorite place for catheterization is the area of the femoral artery. The patient is placed on his back. The surgical field is treated and delimited with sterile sheets. The pulsating femoral artery is palpated. After local paravasal anesthesia with a 0.5% novocaine solution, a skin incision 0.3-0.4 cm long is made. A narrow passage is made from it bluntly to the artery. A special needle with a wide lumen is inserted into the stroke made with a slight inclination. The wall of the artery is pierced with it, after which the stabbing stylet is removed. By pulling the needle, its end is localized in the lumen of the artery. At this moment, a strong stream of blood appears from the needle pavilion. A metal guide is inserted into the artery through a needle, which is then advanced into the internal and common iliac arteries and the aorta to the selected level. The needle is removed, and along the guidewire to the required point arterial system a radiopaque catheter is inserted. Its progress is monitored on a display. After removing the guidewire, the free (outer) end of the catheter is connected to the adapter and the catheter is immediately washed with isotonic sodium chloride solution with heparin. All manipulations during angiography are carried out under X-ray television control. Catheterization participants wear protective aprons over which sterile gowns are worn. During angiography, the patient's condition is constantly monitored. A contrast agent is injected under pressure through a catheter into the artery being examined using an automatic syringe (injector). At the same moment, high-speed X-ray imaging begins. Its program - the number and time of taking pictures - is installed on the device's control panel. The photographs are developed immediately. Once the test is successful, the catheter is removed. The puncture site is pressed for 8-10 minutes to stop bleeding. A pressure bandage is applied to the puncture area for a day. The patient is prescribed bed rest for the same period. A day later, the bandage is replaced with an aseptic sticker. The attending physician constantly monitors the patient's condition. Measurement of body temperature and inspection of the surgical site are mandatory.
A new technique for x-ray examination of blood vessels is digital subtraction angiography (DSA). It is based on the principle of computer subtraction (subtraction) of two images recorded in the computer memory - images before and after the introduction of a contrast agent into the vessel. Thanks to computer processing, the final X-ray picture of the heart and blood vessels is different high quality, but the main thing is that it is possible to isolate the image of blood vessels from the general image of the part of the body being studied, in particular, to remove interfering shadows of soft tissues and skeleton and to quantitatively assess hemodynamics. A significant advantage of DSA compared to other techniques is the reduction in the required amount of radiopaque contrast agent, so it is possible to obtain images of blood vessels with a large dilution of the contrast agent. This means (attention!) that you can inject a contrast agent intravenously and obtain a shadow of the arteries on a subsequent series of images without resorting to catheterization. Currently, conventional angiography is almost universally replaced by DSA.
Radionuclide method is a method of studying the functional and morphological state of organs and systems using radionuclides and indicators labeled with them. These indicators - they are called radiopharmaceuticals (RP) - are introduced into the patient’s body, and then, using various instruments, the speed and nature of their movement, fixation and removal from organs and tissues are determined.
A radiopharmaceutical is a drug that is approved for administration to humans for diagnostic purposes. chemical compound, the molecule of which contains a radionuclide. The radionuclide must have a radiation spectrum of a certain energy, cause a minimum radiation dose and reflect the state of the organ being studied.
To obtain images of organs, only radionuclides emitting γ-rays or characteristic X-ray radiation are used, since these radiations can be recorded with external detection. The more γ-quanta or X-ray quanta are formed during radioactive decay, the more effective a given radiopharmaceutical is in diagnostic terms. At the same time, the radionuclide should emit as little as possible corpuscular radiation - electrons that are absorbed in the patient’s body and do not participate in obtaining images of organs. From this point of view, radionuclides with nuclear transformation according to the type of isomeric transition - Tc, In - are preferable. The optimal range of quantum energy in radionuclide diagnostics is considered to be 70-200 keV. The time during which the activity of a radiopharmaceutical introduced into the body is reduced by half due to physical breakdown and elimination is called the effective half-life (Tm.)
A variety of diagnostic instruments have been developed to perform radionuclide studies. Regardless of their specific purpose, all these devices are designed according to the same principle: they have a detector that converts ionizing radiation into electrical pulses, an electronic processing unit, and a data presentation unit. Many radiodiagnostic devices are equipped with computers and microprocessors. The detector is usually scintillators or, less commonly, gas meters. A scintillator is a substance in which, under the influence of rapidly charged particles or photons, light flashes - scintillations - occur. These scintillations are picked up by photomultiplier tubes (PMTs), which convert the flashes of light into electrical signals. The scintillation crystal and photomultiplier are placed in a protective metal casing - a collimator, which limits the “field of vision” of the crystal to the size of the organ or part of the patient’s body being studied. The collimator has one large or several small holes through which radioactive radiation enters the detector.
In devices designed to determine the radioactivity of biological samples (in vitro), scintillation detectors are used in the form of so-called well counters. Inside the crystal there is a cylindrical channel into which a test tube with the test material is placed. This detector design significantly increases its ability to detect weak radiation from biological samples. To measure radioactivity biological fluids containing radionuclides with soft β-radiation, liquid scintillators are used.
No special preparation of the patient is required.
Indications for radionuclide testing are determined by the attending physician after consultation with a radiologist. As a rule, it is performed after other clinical, laboratory and non-invasive radiation procedures, when the need for radionuclide data on the function and morphology of a particular organ becomes clear.
There are no contraindications to radionuclide diagnostics; there are only restrictions provided for by the instructions of the Ministry of Health of the Russian Federation.
The term “visualization” is derived from the English word vision. It refers to the acquisition of an image, in in this case using radioactive nuclides. Radionuclide imaging is the creation of a picture of the spatial distribution of a radiopharmaceutical in organs and tissues when it is introduced into the patient’s body. The main method of radionuclide imaging is gamma scintigraphy(or simply scintigraphy), which is performed on a machine called a gamma camera. A variant of scintigraphy performed on a special gamma camera (with a moving detector) is layer-by-layer radionuclide imaging - single-photon emission tomography. Rarely, mainly due to the technical difficulty of obtaining ultra-short-lived positron-emitting radionuclides, two-photon emission tomography is also performed on a special gamma camera. Sometimes an outdated method of radionuclide imaging is used - scanning; it is performed on a machine called a scanner.
Scintigraphy is the process of obtaining an image of a patient's organs and tissues by recording on a gamma camera the radiation emitted by an incorporated radionuclide. Gamma camera: A scintillation crystal (usually sodium iodide) is used as a radioactive radiation detector. large sizes– with a diameter of up to 50 cm. This ensures that radiation is recorded simultaneously over the entire part of the body being examined. Gamma rays emanating from the organ cause light flashes in the crystal. These flashes are recorded by several photomultipliers, which are evenly located above the surface of the crystal. Electrical pulses from the photomultiplier are transmitted through an amplifier and discriminator to the analyzer unit, which generates a signal on the display screen. In this case, the coordinates of the point glowing on the screen exactly correspond to the coordinates of the light flash in the scintillator and, consequently, the location of the radionuclide in the organ. At the same time, using electronics, the moment of occurrence of each scintillation is analyzed, which makes it possible to determine the time of passage of the radionuclide through the organ. The most important component of a gamma camera is, of course, a specialized computer, which allows for a variety of computer processing of the image: identifying fields worthy of attention on it - the so-called zones of interest - and conducting various procedures: measurement of radioactivity (general and local), determination of the size of an organ or its parts, study of the rate of passage of radiopharmaceuticals in this field. Using a computer, you can improve the quality of the image and highlight details of interest, for example, the vessels feeding the organ.
A scintigram is a functional anatomical image. This is the uniqueness of radionuclide images, which distinguishes them from those obtained during X-ray and ultrasound examinations, and magnetic resonance imaging. This implies the main condition for prescribing scintigraphy - the organ being studied must be functionally active, at least to a limited extent. Otherwise, the scintigraphic image will not be obtained.
When analyzing scintigrams, mainly static ones, along with the topography of the organ, its size and shape, the degree of homogeneity of its image is determined. Areas with increased accumulation of radiopharmaceuticals are called hot spots, or hot nodes. Usually they correspond to overly actively functioning areas of the organ - inflammatory tissues, some types of tumors, zones of hyperplasia. If the syntigram reveals an area of reduced accumulation of radiopharmaceuticals, then it means that we are talking about some kind of volumetric formation that has replaced the normally functioning parenchyma of the organ - the so-called cold nodes. They are observed in cysts, metastases, focal sclerosis, and some tumors.
Single photon emission tomography (SPET) is gradually replacing conventional static scintigraphy, since it allows one to achieve better spatial resolution with the same amount of the same radiopharmaceutical, i.e. identify significantly smaller areas of organ damage - hot and cold nodes. To perform SPET, special gamma cameras are used. They differ from ordinary ones in that the detectors (usually two) of the camera rotate around the patient’s body. During the rotation process, scintillation signals are sent to the computer from different shooting angles, which makes it possible to construct a layer-by-layer image of the organ on the display screen.
SPET differs from scintigraphy in higher image quality. It allows you to identify smaller details and, therefore, recognize the disease at a more advanced stage. early stages and with greater reliability. If there is a sufficient number of transverse “slices” obtained in a short period of time, using a computer, it is possible to construct a three-dimensional volumetric image of an organ on the display screen, allowing one to obtain a more accurate idea of its structure and function.
There is another type of layer-by-layer radionuclide imaging - positron two-photon emission tomography (PET). Radionuclides that emit positrons are used as radiopharmaceuticals, mainly ultra-short-lived nuclides with a half-life of several minutes - C (20.4 min), N (10 min), O (2.03 min), F (10 min). The positrons emitted by these radionuclides annihilate near atoms with electrons, resulting in the appearance of two gamma quanta - photons (hence the name of the method), scattering from the annihilation point in strictly opposite directions. Scattering quanta are recorded by several gamma camera detectors located around the subject. The main advantage of PET is that the radionuclides used in it can label very physiologically important drugs, for example glucose, which is known to be actively involved in many metabolic processes. When labeled glucose is introduced into the patient’s body, it is actively involved in the tissue metabolism of the brain and heart muscle.
The spread of this important and very promising method in the clinic is hampered by the fact that ultra-short-lived radionuclides are produced in nuclear particle accelerators - cyclotrons.
Advantages:
Obtaining data on organ function
· Obtaining data on the presence of a tumor and metastases with high reliability in the early stages
Flaws:
· All medical studies related to the use of radionuclides are carried out in special radioimmune diagnostic laboratories.
· Laboratories are equipped with means and equipment to protect personnel from radiation and prevent contamination by radioactive substances.
· Radiodiagnostic procedures are regulated by radiation safety standards for patients when using radioactive substances for diagnostic purposes.
· In accordance with these standards, 3 groups of subjects were identified - AD, BD and VD. The AD category includes persons for whom a radionuclide diagnostic procedure is prescribed in connection with an oncological disease or suspicion of it, the BD category includes persons for whom a diagnostic procedure is performed in connection with non-oncological diseases, and the VD category includes persons. subject to examination, for example, for prophylactic purposes, using special tables of radiation exposure, the radiologist determines the admissibility, from the point of view of radiation safety, of performing one or another radionuclide diagnostic study.
Ultrasonic method - a method for remotely determining the position, shape, size, structure and movement of organs and tissues, as well as pathological foci using ultrasound radiation.
There are no contraindications for use.
Advantages:
· are classified as non-ionizing radiation and in the range used in diagnostics do not cause pronounced biological effects.
· The ultrasound diagnostic procedure is short, painless, and can be repeated many times.
· The ultrasound machine takes up little space and can be used to examine both inpatients and outpatients.
· Low cost of research and equipment.
· There is no need to protect the doctor and patient or special arrangement of the office.
· safety in terms of dose load (examination of pregnant and lactating women);
· high resolution,
· differential diagnosis of solid and cavitary formations
· visualization of regional lymph nodes;
· conducting targeted puncture biopsies of palpable and non-palpable formations under objective visual control, multiple dynamic studies during the treatment process.
Flaws:
· lack of visualization of the organ as a whole (only tomographic section);
· low information content during fatty involution (ultrasound contrast between tumor and fatty tissues is weak);
· subjectivity of interpretation of the resulting image (operator-dependent method);
An ultrasound examination apparatus is a complex and fairly portable device, available in a stationary or portable version. The device's sensor, also called a transducer, includes an ultrasonic transducer. the main part of which is a piezoceramic crystal. Short electrical pulses coming from the electronic unit of the device excite ultrasonic vibrations in it - the inverse piezoelectric effect. The vibrations used for diagnostics are characterized by a short wavelength, which allows them to be formed into a narrow beam directed at the part of the body being examined. Reflected waves (“echoes”) are perceived by the same piezoelectric element and converted into electrical signals - a direct piezoelectric effect. The latter enter a high-frequency amplifier, are processed in the electronic unit of the device and are presented to the user in the form of a one-dimensional (in the form of a curve) or two-dimensional (in the form of a picture) image. The first is called an echogram, and the second is a sonogram (synonyms: ultrasonogram, ultrasound scanogram). Depending on the shape of the resulting image, sector, linear and convex (convex) sensors are distinguished.
According to the principle of operation, all ultrasonic sensors are divided into two groups: pulse echo and Doppler. Devices of the first group are used to determine anatomical structures, their visualization and measurement. Doppler sensors make it possible to obtain kinematic characteristics of rapidly occurring processes - blood flow in the vessels, heart contractions. However, this division is conditional. Many installations make it possible to simultaneously study both anatomical and functional parameters.
Preparation:
· For examination of the brain, eyes, thyroid, salivary and mammary glands, heart, kidneys, examination of pregnant women with a term of more than 20 weeks, no special preparation is required.
· When examining the abdominal organs, especially the pancreas, the intestines should be carefully prepared so that there is no accumulation of gas.
· The patient must come to the ultrasound room on an empty stomach.
Three methods of ultrasound diagnostics are most widespread in facial practice: one-dimensional examination (echography), two-dimensional examination (sonography, scanning) and Dopplerography. All of them are based on recording echo signals reflected from an object.
There are two options for one-dimensional ultrasound examination: A- and M-methods.
Principle A-method: The sensor is in a fixed position to record the echo in the direction of emission. Echo signals are represented in one-dimensional form as amplitude marks on the time axis. Hence, by the way, the name of the method (from the English amplitude - amplitude). In other words, the reflected signal forms a figure on the indicator screen in the form of a peak on a straight line. The number and location of peaks on a horizontal line correspond to the location of the object’s ultrasound-reflecting elements. Consequently, the one-dimensional Α-method makes it possible to determine the distance between tissue layers along the path of the ultrasonic pulse. The main clinical application of the A-method is ophthalmology and neurology. The Α-method of ultrasonic dowsing is still quite widely used in the clinic, as it is characterized by simplicity, low cost and mobility of the study.
M-method(from English motion - movement) also refers to one-dimensional ultrasound examinations. It is designed to study a moving object - the heart. The sensor is also in a fixed position. The frequency of sending ultrasonic pulses is very high - about 1000 per 1 s, and the pulse duration is very short, only 1 μs. The echo signals reflected from the moving walls of the heart are recorded on chart paper. Based on the shape and location of the recorded curves, one can get an idea of the nature of heart contractions. This method of ultrasonic dowsing is also called “echocardiography” and, as follows from its description, is used in cardiological practice.
Ultrasound scanning allows you to obtain a two-dimensional image of organs (sonography). This method is also known as B-method(from the English bright - brightness). The essence of the method is to move the ultrasound beam along the surface of the body during the study. This ensures registration of signals simultaneously or sequentially from many objects. The resulting series of signals serves to form an image. It appears on the display and can be recorded on paper. This image can be subjected to mathematical processing, determining the dimensions (area, perimeter, surface and volume) of the organ under study. During ultrasonic scanning, the brightness of each luminous point on the indicator screen is directly dependent on the intensity of the echo signal. Signals of different strengths cause dark areas on the screen varying degrees(from white to black). On devices with such indicators, dense stones appear bright white, and formations containing liquid appear black.
Dopplerography-based on the Doppler effect, the effect consists of a change in wavelength (or frequency) when the source of the waves moves relative to the device receiving them.
There are two types of Doppler studies - continuous (constant wave) and pulsed. In the first case, ultrasonic waves are generated continuously by one piezo-crystal element, and reflected waves are recorded by another. In the electronic unit of the device, two frequencies of ultrasonic vibrations are compared: those directed at the patient and those reflected from him. By the shift in the frequencies of these oscillations, the speed of movement of anatomical structures is judged. Frequency shift analysis can be done acoustically or using recorders.
Continuous Dopplerography- a simple and accessible research method. It is most effective at high blood flow rates, for example in areas of vasoconstriction. However, this method has a significant drawback: the frequency of the reflected signal changes not only due to the movement of blood in the vessel under study, but also due to any other moving structures that occur in the path of the incident ultrasonic wave. Thus, with continuous Doppler ultrasound, the total speed of movement of these objects is determined.
Free from this disadvantage pulsed dopplerography. It allows you to measure speed in prescribed by the doctor control volume area (up to 10 points)
Ultrasound angiography, or color Doppler mapping. The method is based on color coding of the average Doppler shift of the emitted frequency. In this case, the blood moving towards the sensor is colored red, and from the sensor - blue. The color intensity increases with increasing blood flow speed.
Further development Doppler mapping has become power doppler. With this method, it is not the average value of the Doppler shift that is encoded in color, as with conventional Doppler mapping, but the integral of the amplitudes of all echo signals of the Doppler spectrum. This makes it possible to obtain an image of a blood vessel over a much larger extent and to visualize vessels of even a very small diameter (ultrasound angiography). Angiograms obtained using power Doppler do not reflect the speed of movement of red blood cells, as with conventional color mapping, but the density of red blood cells in a given volume.
Another type of Doppler mapping is tissue doppler. It is based on imaging of native tissue harmonics. They arise as additional frequencies during the propagation of a wave signal in a material environment, are an integral part of this signal and are multiples of its main (fundamental) frequency. By registering only tissue harmonics (without the main signal), it is possible to obtain an isolated image of the heart muscle without an image of the blood contained in the cavities of the heart.
MRI based on the phenomenon of nuclear magnetic resonance. If a body located in a constant magnetic field is irradiated by an external alternating magnetic field, the frequency of which is exactly equal to the frequency of transition between energy levels of atomic nuclei, then the nuclei will begin to transform into higher-energy quantum states. In other words, selective (resonant) absorption of energy is observed electromagnetic field. When the influence of an alternating electromagnetic field ceases, a resonant release of energy occurs.
Modern MRI scanners are “tuned” to hydrogen nuclei, i.e. to protons. The proton is constantly spinning. Consequently, a magnetic field is also formed around it, which has a magnetic moment, or spin. When a rotating proton is placed in a magnetic field, precession of the proton occurs. Precession is the movement of the proton's rotation axis, in which it describes a circular conical surface like the axis of a rotating top. Typically, an additional radio frequency field acts in the form of a pulse, and in two versions: a shorter one, which rotates the proton by 90°, and a longer one, which rotates the proton by 180°. When the radio frequency pulse ends, the proton returns to its original position (its relaxation occurs), which is accompanied by the emission of a portion of energy. Each element of the volume of the object under study (i.e., each voxel - from the English volume - volume, cell - cell), due to the relaxation of protons distributed in it, excites an electric current (“MR signals”) in a receiving coil located outside the object. The magnetic resonance characteristics of an object are 3 parameters: proton density, time Tι and time T2. T1 is called spin-lattice, or longitudinal, relaxation, and T2 is called spin-spin, or transverse. The amplitude of the recorded signal characterizes the proton density or, which is the same, the concentration of the element in the medium under study.
The MRI system consists of a strong magnet that creates a static magnetic field. The magnet is hollow and has a tunnel in which the patient is located. The patient table has an automatic movement control system in the longitudinal and vertical directions. For radio wave excitation of hydrogen nuclei, a high-frequency coil is additionally installed, which simultaneously serves to receive a relaxation signal. Using special gradient coils, an additional magnetic field is applied which serves to encode the MR signal from the patient; in particular, it sets the level and thickness of the selected layer.
In MRI, artificial tissue contrast can be used. For this purpose, chemical substances that have magnetic properties and contain nuclei with an odd number of protons and neutrons are used, for example fluorine compounds, or paramagnetic substances that change the relaxation time of water and thereby enhance the image contrast on MRI scans. One of the most common contrast agents used in MRI is the gadolinium compound Gd-DTPA.
Flaws:
· very strict requirements are imposed on the placement of an MRI scanner in a medical institution. Separate rooms are required, carefully shielded from external magnetic and radio frequency fields.
· the treatment room where the MRI scanner is located is enclosed in a metal mesh cage (Faraday cage), on top of which finishing material is applied (floor, ceiling, walls).
Difficulty in visualizing hollow organs and chest organs
· A large amount of time is spent on the study (compared to MSCT)
· In children aged from the neonatal period to 5–6 years, the examination can usually only be carried out under sedation under the supervision of an anesthesiologist.
· An additional limitation may be waist circumference, which is incompatible with the diameter of the tomograph tunnel (each type of MRI scanner has its own patient weight limit).
· The main diagnostic limitations of MRI are the inability to reliably detect calcifications and assess the mineral structure of bone tissue (flat bones, cortical plate).
· MRI is also much more susceptible to motion artifacts than CT.
Advantages:
· allows you to obtain an image of thin layers of the human body in any section - frontal, sagittal, axial (as is known, with X-ray computed tomography, with the exception of spiral CT, only the axial section can be used).
· The examination is not burdensome for the patient, is absolutely harmless, and does not cause complications.
· MRI scans display soft tissues better than X-ray computed tomograms: muscles, cartilage, fat layers.
· MRI makes it possible to detect infiltration and destruction of bone tissue, bone marrow replacement long before the appearance of radiological (including CT) signs.
· With MRI, you can obtain images of blood vessels without injecting a contrast agent into them.
· Using special algorithms and selection of radiofrequency pulses, modern high-field MR tomographs make it possible to obtain two-dimensional and three-dimensional (volumetric) images of the vascular bed - magnetic resonance angiography.
· Large vessels and their branches of medium caliber can be quite clearly visualized on MR tomograms without additional administration of a contrast agent.
· To obtain images of small vessels, gadolinium preparations are additionally administered.
· Ultra-high-speed MRI scanners have been developed that make it possible to observe the movement of the heart and blood in its cavities and vessels and obtain matrices of increased resolution for visualizing very thin layers.
· In order to prevent the development of claustrophobia in patients, the production of open MRI scanners has been developed. They do not have a long magnetic tunnel, and a constant magnetic field is created by placing magnets on the side of the patient. Such a constructive solution not only saved the patient from the need long time being in a relatively confined space, but also created the prerequisites for instrumental interventions under MRI control.
Contraindications:
· Claustrophobia and closed-type tomograph
· The presence of metal (ferromagnetic) implants and foreign bodies in cavities and tissues. In particular, intracranial ferromagnetic hemostatic clips (if displaced, vessel damage and bleeding may occur), periorbital ferromagnetic foreign bodies (if displaced, damage to the eyeball may occur)
· Presence of pacemakers
· Pregnant women in the 1st trimester.
MR spectroscopy , like MRI, is based on the phenomenon of nuclear magnetic resonance. Usually the resonance of hydrogen nuclei is studied, less often - carbon, phosphorus and other elements.
The essence of the method is as follows. The tissue or liquid sample being tested is placed in a stable magnetic field with a strength of about 10 T. The sample is exposed to pulsed radio frequency oscillations. By changing the magnetic field strength, resonant conditions are created for different elements in the magnetic resonance spectrum. The MR signals arising in the sample are captured by the radiation receiver coil, amplified and transmitted to a computer for analysis. The final spectrogram has the form of a curve, to obtain which fractions (usually millionths) of the voltage of the applied magnetic field are plotted along the abscissa axis, and the signal amplitude values are plotted along the ordinate axis. The intensity and shape of the response signal depend on the proton density and relaxation time. The latter is determined by the location and relationship of hydrogen nuclei and other elements in macromolecules. Different nuclei have different resonance frequencies, so MR spectroscopy allows us to get an idea of the chemical and spatial structure of a substance. It can be used to determine the structure of biopolymers, the lipid composition of membranes and their phase state, and the permeability of membranes. Based on the appearance of the MR spectrum, it is possible to differentiate mature
State Institution "Ufa Research Institute of Eye Diseases" of the Academy of Sciences of the Republic of Belarus, Ufa
The discovery of X-rays marked the beginning new era in medical diagnostics - the era of radiology. Modern methods of radiation diagnostics are divided into X-ray, radionuclide, magnetic resonance, and ultrasound.
X-ray method is a way of studying the structure and function of various organs and systems, based on qualitative and quantitative analysis a beam of X-ray radiation passing through the human body. X-ray examination can be carried out under conditions of natural contrast or artificial contrast.
Radiography is simple and not burdensome for the patient. A radiograph is a document that can be stored for a long time, used for comparison with repeated radiographs, and presented for discussion to an unlimited number of specialists. Indications for radiography must be justified, since X-ray radiation is associated with radiation exposure.
Computed tomography (CT) is a layer-by-layer x-ray examination based on computer reconstruction of the image obtained by circularly scanning an object with a narrow beam of x-ray radiation. A CT scanner can distinguish between tissues that differ in density by only half a percent. Therefore, a CT scanner provides approximately 1000 times more information than a regular X-ray. With spiral CT, the emitter moves in a spiral relative to the patient’s body and captures a certain volume of the body in a few seconds, which can subsequently be represented in separate discrete layers. Spiral CT initiated the creation of new promising imaging methods - computed angiography, three-dimensional (volumetric) imaging of organs, and, finally, the so-called virtual endoscopy, which became the crown of modern medical imaging.
The radionuclide method is a method of studying the functional and morphological state of organs and systems using radionuclides and indicators labeled with them. Indicators—radiopharmaceuticals (RPs)—are introduced into the patient’s body, and then, using instruments, the speed and nature of their movement, fixation, and removal from organs and tissues are determined. Modern methods of radionuclide diagnostics are scintigraphy, single photon emission tomography (SPET) and positron emission tomography (PET), radiography and radiometry. The methods are based on the introduction of radiopharmaceuticals, which emit positrons or photons. These substances, when introduced into the human body, accumulate in areas of increased metabolism and increased blood flow.
Ultrasound method is a method for remotely determining the position, shape, size, structure and movement of organs and tissues, as well as pathological foci using ultrasound radiation. It can register even minor changes in the density of biological media. Thanks to this, the ultrasound method has become one of the most popular and accessible studies in clinical medicine. Three methods are most widespread: one-dimensional examination (echography), two-dimensional examination (sonography, scanning) and Dopplerography. All of them are based on recording echo signals reflected from an object. With the one-dimensional A-method, the reflected signal forms a figure on the indicator screen in the form of a peak on a straight line. The number and location of peaks on a horizontal line corresponds to the location of the object’s ultrasound-reflecting elements. Ultrasound scanning (B-method) allows you to obtain a two-dimensional image of organs. The essence of the method is to move the ultrasound beam along the surface of the body during the study. The resulting series of signals serves to form an image. It appears on the display and can be recorded on paper. This image can be subjected to mathematical processing, determining the dimensions (area, perimeter, surface and volume) of the organ under study. Dopplerography allows you to non-invasively, painlessly and informatively record and evaluate the blood flow of an organ. Color Doppler mapping, which is used in the clinic to study the shape, contours and lumen of blood vessels, has been proven to be highly informative.
Magnetic resonance imaging (MRI) is an extremely valuable research method. Instead of ionizing radiation, a magnetic field and radio frequency pulses are used. The operating principle is based on the phenomenon of nuclear magnetic resonance. By manipulating gradient coils that create small additional fields, it is possible to record signals from a thin layer of tissue (up to 1 mm) and easily change the direction of the slice - transverse, coronal and sagittal, obtaining a three-dimensional image. The main advantages of the MRI method include: the absence of radiation exposure, the ability to obtain images in any plane and perform three-dimensional (spatial) reconstructions, the absence of artifacts from bone structures, high resolution visualization of various tissues, and the almost complete safety of the method. Contraindications to MRI are the presence of metal foreign bodies in the body, claustrophobia, convulsive syndrome, serious condition of the patient, pregnancy and lactation.
The development of radiation diagnostics also plays an important role in practical ophthalmology. It can be argued that the organ of vision is an ideal object for CT due to pronounced differences in the absorption of radiation in the tissues of the eye, muscles, nerves, blood vessels and retrobulbar fatty tissue. CT allows us to better study the bone walls of the orbits and identify pathological changes in them. CT is used for suspected orbital tumors, exophthalmos of unknown origin, trauma, or orbital foreign bodies. MRI makes it possible to examine the orbit in different projections and allows a better understanding of the structure of neoplasms inside the orbit. But this technique is contraindicated if metal foreign bodies get into the eye.
The main indications for ultrasound are: damage to the eyeball, a sharp decrease in the transparency of light-conducting structures, detachment of the choroid and retina, the presence of foreign intraocular bodies, tumors, damage to the optic nerve, the presence of areas of calcification in the membranes of the eye and the area of the optic nerve, dynamic monitoring of the treatment , study of the characteristics of blood flow in the orbital vessels, studies before MRI or CT.
Radiography is used as a screening method for injuries to the orbit and lesions of its bone walls to identify dense foreign bodies and determine their location, and diagnose diseases of the lacrimal ducts. The method of x-ray examination of the paranasal sinuses adjacent to the orbit is of great importance.
Thus, at the Ufa Research Institute of Eye Diseases in 2010, 3116 x-ray examinations were carried out, including 935 (34%) for patients from the clinic, 1059 (30%) from the hospital, and from the office emergency care— 1122 (36%). 699 (22.4%) special studies were performed, which included examination of the lacrimal ducts with contrast (321), non-skeletal radiography (334), and identification of the localization of foreign bodies in the orbit (39). X-ray of the chest organs in inflammatory diseases of the orbit and eyeball was 18.3% (213), and of the paranasal sinuses - 36.3% (1132).
conclusions. Radiation diagnostics is a necessary component of the clinical examination of patients in ophthalmology clinics. Many achievements of traditional X-ray examination are increasingly retreating before the improving capabilities of CT, ultrasound, and MRI.
PREFACE
Medical radiology (radiation diagnostics) is a little over 100 years old. During this historically short period of time, she wrote many bright pages in the chronicle of the development of science - from the discovery of V.K. Roentgen (1895) to the rapid computer processing of medical radiation images.
At the origins of domestic X-ray radiology were M.K. Nemenov, E.S. London, D.G. Rokhlin, D.S. Lindenbraten - outstanding organizers of science and practical healthcare. Such outstanding personalities as S.A. Reinberg, G.A. Zedgenizde, V.Ya. Dyachenko, Yu.N. Sokolov, L.D. Lindenbraten and others made a great contribution to the development of radiation diagnostics.
The main goal of the discipline is to study theoretical and practical issues of general radiation diagnostics (x-ray, radionuclide,
ultrasound, computed tomography, magnetic resonance imaging, etc.) necessary in the future for students to successfully master clinical disciplines.
Today, radiation diagnostics, taking into account clinical and laboratory data, allows 80-85% to recognize the disease.
This guide to radiation diagnostics is compiled in accordance with the State Educational Standard (2000) and the Curriculum approved by VUNMC (1997).
Today, the most common method of radiological diagnosis is traditional x-ray examination. Therefore, when studying radiology, the main attention is paid to methods for studying human organs and systems (fluoroscopy, radiography, ERG, fluorography, etc.), methods for analyzing radiographs and general x-ray semiotics of the most common diseases.
Currently, digital radiography with high image quality is successfully developing. It is distinguished by its speed, the ability to transmit images over a distance, and the convenience of storing information on magnetic media (disks, tapes). An example is X-ray computed tomography (XCT).
The ultrasound method of examination (ultrasound) deserves attention. Due to its simplicity, harmlessness and effectiveness, the method is becoming one of the most common.
CURRENT STATE AND PROSPECTS FOR THE DEVELOPMENT OF RADIOLOGICAL DIAGNOSTICS
Radiation diagnostics (diagnostic radiology) is an independent branch of medicine that combines various methods of obtaining images for diagnostic purposes based on the use of various types of radiation.
Currently, the activities of radiation diagnostics are regulated by the following regulatory documents:
1. Order of the Ministry of Health of the Russian Federation No. 132 dated August 2, 1991 “On improving the radiology diagnostic service.”
2. Order of the Ministry of Health of the Russian Federation No. 253 dated June 18, 1996 “On further improvement of work to reduce radiation doses during medical procedures”
3. Order No. 360 of September 14, 2001. “On approval of the list of radiation research methods.”
Radiation diagnostics includes:
1. Methods based on the use of X-rays.
1). Fluorography
2). Traditional X-ray examination
4). Angiography
2. Methods based on the use of ultrasound radiation 1).Ultrasound
2). Echocardiography
3). Dopplerography
3. Methods based on nuclear magnetic resonance. 1).MRI
2). MP spectroscopy
4. Methods based on the use of radiopharmaceuticals (radiopharmacological drugs):
1). Radionuclide diagnostics
2). Positron emission tomography - PET
3). Radioimmune studies
5.Methods based on infrared radiation (thermophafia)
6.Interventional radiology
Common to all research methods is the use of various radiations (X-rays, gamma rays, ultrasound, radio waves).
The main components of radiation diagnostics are: 1) radiation source, 2) sensing device.
The diagnostic image is usually a combination of different shades of gray color, proportional to the intensity of the radiation hitting the receiving device.
A picture of the internal structure of the study of an object can be:
1) analog (on film or screen)
2) digital (radiation intensity is expressed in the form of numerical values).
All these methods are combined into a common specialty - radiation diagnostics (medical radiology, diagnostic radiology), and the doctors are radiologists (abroad), but for now we have an unofficial “radiology diagnostician”
In the Russian Federation, the term radiology diagnostics is official only to designate a medical specialty (14.00.19); departments also have a similar name. In practical healthcare, the name is conditional and combines 3 independent specialties: radiology, ultrasound diagnostics and radiology (radionuclide diagnostics and radiation therapy).
Medical thermography is a method of recording natural thermal (infrared) radiation. The main factors determining body temperature are: the intensity of blood circulation and the intensity of metabolic processes. Each region has its own “thermal relief”. Using special equipment (thermal imagers), infrared radiation is captured and converted into a visible image.
Patient preparation: discontinuation of medications that affect blood circulation and the level of metabolic processes, prohibition of smoking 4 hours before the examination. There should be no ointments, creams, etc. on the skin.
Hyperthermia is characteristic of inflammatory processes, malignant tumors, thrombophlebitis; hypothermia is observed in case of vasospasms, circulatory disorders in occupational diseases (vibration disease, cerebrovascular accident, etc.).
The method is simple and harmless. However, the diagnostic capabilities of the method are limited.
One of the widely used modern methods is ultrasound (ultrasound dowsing). The method has become widespread due to its simplicity, accessibility, and high information content. In this case, the frequency of sound vibrations is used from 1 to 20 megahertz (a person hears sound within frequencies from 20 to 20,000 hertz). A beam of ultrasonic vibrations is directed to the area under study, which is partially or completely reflected from all surfaces and inclusions that differ in sound conductivity. The reflected waves are captured by a sensor, processed by an electronic device and converted into a one-dimensional (echography) or two-dimensional (sonography) image.
Based on the difference in the sound density of the picture, one or another diagnostic decision is made. From the scanograms one can judge the topography, shape, size of the organ being studied, as well as pathological changes in it. Being harmless to the body and staff, the method has found wide application in obstetric and gynecological practice, in the study of the liver and biliary tract, retroperitoneal organs and other organs and systems.
Radionuclide methods for imaging various human organs and tissues are rapidly developing. The essence of the method is that radionuclides or radioactive compounds labeled with them are introduced into the body, which selectively accumulate in the corresponding organs. In this case, radionuclides emit gamma quanta, which are detected by sensors and then recorded by special devices (scanners, gamma camera, etc.), which makes it possible to judge the position, shape, size of the organ, distribution of the drug, the speed of its elimination, etc.
Within the framework of radiation diagnostics, a new promising direction is emerging - radiological biochemistry (radioimmune method). At the same time, hormones, enzymes, tumor markers, drugs, etc. are studied. Today, more than 400 biologically active substances are determined in vitro; Methods of activation analysis are being successfully developed - determining the concentration of stable nuclides in biological samples or in the body as a whole (irradiated with fast neutrons).
The leading role in obtaining images of human organs and systems belongs to X-ray examination.
With the discovery of X-rays (1895), the age-old dream of a doctor came true - to look inside a living organism, study its structure, work, and recognize a disease.
Currently, there are a large number of X-ray examination methods (non-contrast and using artificial contrast), which make it possible to examine almost all human organs and systems.
Recently, digital imaging technologies (low-dose digital radiography), flat panels - detectors for REOP, X-ray image detectors based on amorphous silicon, etc. - have been increasingly introduced into practice.
The advantages of digital technologies in radiology: reduction of the radiation dose by 50-100 times, high resolution (objects 0.3 mm in size are visualized), film technology is eliminated, office throughput increases, an electronic archive is formed with quick access, and the ability to transmit images over a distance.
Interventional radiology is closely related to radiology - a combination of diagnostic and therapeutic measures in one procedure.
Main directions: 1) X-ray vascular interventions (expansion of narrowed arteries, blockage of blood vessels with hemangiomas, vascular prosthetics, stopping bleeding, removal of foreign bodies, medicinal substances to the tumor), 2) extravasal interventions (catheterization of the bronchial tree, puncture of the lung, mediastinum, decompression for obstructive jaundice, administration of drugs that dissolve stones, etc.).
CT scan. Until recently, it seemed that the methodological arsenal of radiology was exhausted. However, computed tomography (CT) was born, revolutionizing X-ray diagnostics. Almost 80 years after the Nobel Prize received by Roentgen (1901), in 1979 the same prize was awarded to Hounsfield and Cormack on the same part of the scientific front - for the creation of a computed tomograph. Nobel Prize for creating the device! The phenomenon is quite rare in science. And the whole point is that the capabilities of the method are quite comparable to the revolutionary discovery of Roentgen.
The disadvantage of the x-ray method is the flat image and the overall effect. With CT, the image of an object is mathematically reconstructed from a countless set of its projections. Such an object is a thin slice. At the same time, it is illuminated from all sides and its image is recorded by a huge number of highly sensitive sensors (several hundred). The received information is processed on a computer. CT detectors are very sensitive. They detect differences in the density of structures of less than one percent (with conventional radiography - 15-20%). From here, you can get images of various structures of the brain, liver, pancreas and a number of other organs.
Advantages of CT: 1) high resolution, 2) examination of the thinnest section - 3-5 mm, 3) the ability to quantify density from -1000 to + 1000 Hounsfield units.
Currently, spiral computed tomographs have appeared that provide examination of the entire body and obtain tomograms in normal operating mode in one second and image reconstruction time from 3 to 4 seconds. For the creation of these devices, scientists were awarded the Nobel Prize. Mobile CT scanners have also appeared.
Magnetic resonance imaging is based on nuclear magnetic resonance. Unlike an X-ray machine, a magnetic tomograph does not “examine” the body with rays, but forces the organs themselves to send radio signals, which the computer processes to form an image.
Work principles. The object is placed in a constant magnetic field, which is created by a unique electromagnet in the form of 4 huge rings connected together. On the couch, the patient is moved into this tunnel. A powerful constant electromagnetic field is turned on. In this case, the protons of hydrogen atoms contained in the tissues are oriented strictly along the lines of force (under normal conditions they are randomly oriented in space). Then the high-frequency electromagnetic field is turned on. Now the nuclei, returning to their original state (position), emit tiny radio signals. This is the NMR effect. The computer registers these signals and the distribution of protons and forms an image on a television screen.
Radio signals are not the same and depend on the location of the atom and its environment. Atoms in painful areas emit a radio signal that differs from the radiation of neighboring healthy tissues. The resolution of the devices is extremely high. For example, individual structures of the brain are clearly visible (stem, hemisphere, gray, white matter, ventricular system, etc.). Advantages of MRI over CT:
1) MP tomography is not associated with the risk of tissue damage, unlike X-ray examination.
2) Scanning with radio waves allows you to change the location of the section being studied in the body”; without changing the patient's position.
3) The image is not only transverse, but also in any other sections.
4) Resolution is higher than with CT.
Obstacles to MRI are metal bodies (clips after surgery, cardiac pacemakers, electrical neurostimulators)
Current trends in the development of radiation diagnostics
1. Improving methods based on computer technology
2. Expanding the scope of application of new high-tech methods - ultrasound, MRI, X-ray CT, PET.
4. Replacement of labor-intensive and invasive methods with less dangerous ones.
5. Maximum reduction of radiation exposure to patients and staff.
Comprehensive development of interventional radiology, integration with other medical specialties.
The first direction is a breakthrough in the field of computer technology, which made it possible to create a wide range of devices for digital digital radiography, ultrasound, MRI to the use of three-dimensional images.
One laboratory per 200-300 thousand population. It should preferably be placed in therapeutic clinics.
1. It is necessary to place the laboratory in a separate building, built according to a standard design with a security sanitary zone around it. It is forbidden to build children's institutions and catering units on the territory of the latter.
2. The radionuclide laboratory must have a certain set of premises (radiopharmaceutical storage, packaging, generator, washing, treatment room, sanitary inspection room).
3. Special ventilation is provided (five air changes when using radioactive gases), sewerage with a number of settling tanks in which waste of at least ten half-lives is kept.
4. Daily wet cleaning of the premises must be carried out.
In the coming years, and sometimes even today, the main place of work of a doctor will be a personal computer, on the screen of which information with electronic medical history data will be displayed.
The second direction is associated with the widespread use of CT, MRI, PET, and the development of ever new areas of their use. Not from simple to complex, but the choice of the most effective techniques. For example, detection of tumors, brain metastases and spinal cord- MRI, metastases - PET; renal colic - spiral CT.
The third direction is the widespread elimination of invasive methods and methods associated with high radiation exposure. In this regard, today myelography, pneumomediastinography, intravenous cholegraphy, etc. have practically disappeared. Indications for angiography are being reduced.
The fourth direction is the maximum reduction of doses of ionizing radiation due to: I) replacing X-ray emitters MRI, ultrasound, for example, when examining the brain and spinal cord, biliary tract, etc. But this must be done deliberately so that a situation does not happen similar to an X-ray examination of the gastrointestinal tract, where everything shifted to FGS, although for endophytic cancers more information is obtained from X-ray examination. Today, ultrasound cannot replace mammography. 2) maximum reduction of doses during the X-ray examinations themselves by eliminating duplication of images, improving technology, film, etc.
The fifth direction is the rapid development of interventional radiology and the widespread involvement of radiation diagnosticians in this work (angiography, puncture of abscesses, tumors, etc.).
Features of individual diagnostic methods at the present stage
In traditional radiology, the layout of X-ray machines has fundamentally changed - installation on three workstations (images, translucency and tomography) is replaced by a remote-controlled one workstation. The number of special devices has increased (mammographs, angiography, dentistry, ward, etc.). Devices for digital radiography, URI, subtraction digital angiography, and photostimulating cassettes have become widespread. Digital and computer radiology has emerged and is developing, which leads to a reduction in examination time, the elimination of the darkroom process, the creation of compact digital archives, the development of teleradiology, and the creation of intra- and interhospital radiological networks.
Ultrasound technologies have been enriched with new programs for digital processing of echo signals, and Dopplerography for assessing blood flow is intensively developing. Ultrasound has become the main method in the study of the abdomen, heart, pelvis, and soft tissues of the extremities; the importance of the method in the study of the thyroid gland, mammary glands, and intracavitary studies is increasing.
In the field of angiography, interventional technologies are intensively developing (balloon dilatation, installation of stents, angioplasty, etc.)
In RCT, spiral scanning, multilayer CT, and CT angiography become dominant.
MRI has been enriched with open-type installations with a field strength of 0.3 - 0.5 T and with high intensity (1.7-3 OT), functional methods for studying the brain.
A number of new radiopharmaceuticals have appeared in radionuclide diagnostics, and PET (oncology and cardiology) has established itself in the clinic.
Telemedicine is emerging. Its task is electronic archiving and transmission of patient data over a distance.
The structure of radiation research methods is changing. Traditional X-ray examinations, testing and diagnostic fluorography, ultrasound are methods of primary diagnosis and are mainly focused on studying the organs of the thoracic and abdominal cavity, and the osteo-articular system. Specifying methods include MRI, CT, radionuclide studies, especially when examining bones, dentofacial area, head and spinal cord.
Currently, over 400 compounds of various chemical natures have been developed. The method is an order of magnitude more sensitive than laboratory biochemical studies. Today, radioimmunoassay is widely used in endocrinology (diabetes mellitus diagnosis), oncology (search for cancer markers), in cardiology (myocardial infarction diagnosis), in pediatrics (for child development disorders), in obstetrics and gynecology (infertility, fetal development disorders), in allergology, toxicology, etc.
In industrialized countries, the main emphasis is now on organizing positron emission tomography (PET) centers in large cities, which, in addition to a positron emission tomograph, also includes a small-sized cyclotron for the on-site production of positron-emitting ultrashort-lived radionuclides. Where there are no small-sized cyclotrons, the isotope (F-18 with a half-life of about 2 hours) is obtained from their regional radionuclide production centers or generators (Rb-82, Ga-68, Cu-62) are used.
Currently, radionuclide research methods are also used for preventive purposes to identify hidden diseases. Thus, any headache requires a brain study with pertechnetate-Tc-99sh. This type of screening allows us to exclude tumors and areas of hemorrhage. A reduced kidney detected in childhood by scintigraphy should be removed to prevent malignant hypertension. A drop of blood taken from the child's heel allows you to determine the amount of thyroid hormones.
Methods of radionuclide research are divided into: a) research of a living person; b) examination of blood, secretions, excreta and other biological samples.
In vivo methods include:
1. Radiometry (of the whole body or part of it) - determination of the activity of a part of the body or organ. Activity is recorded as numbers. An example is the study of the thyroid gland and its activity.
2. Radiography (gammachronography) - on a radiograph or gamma camera, the dynamics of radioactivity is determined in the form of curves (hepatoradiography, radiorenography).
3. Gammatopography (on a scanner or gamma camera) - the distribution of activity in an organ, which allows one to judge the position, shape, size, and uniformity of drug accumulation.
4. Radioimmunoassay (radiocompetitive) - hormones, enzymes, drugs, etc. are determined in a test tube. In this case, the radiopharmaceutical is introduced into a test tube, for example, with the patient’s blood plasma. The method is based on competition between a substance labeled with a radionuclide and its analogue in a test tube for complexing (combining) with a specific antibody. An antigen is a biochemical substance that needs to be determined (hormone, enzyme, drug). For analysis you must have: 1) the substance under study (hormone, enzyme); 2) its labeled analogue: the label is usually 1-125 with a half-life of 60 days or tritium with a half-life of 12 years; 3) a specific perceptive system, which is the subject of “competition” between the desired substance and its labeled analogue (antibody); 4) a separation system that separates bound radioactive substances from unbound ones (activated carbon, ion exchange resins, etc.).
RADIATION STUDY OF THE LUNG
The lungs are one of the most common objects of radiation research. The important role of x-ray examination in the study of the morphology of the respiratory organs and the recognition of various diseases is evidenced by the fact that the accepted classifications of many pathological processes are based on x-ray data (pneumonia, tuberculosis, lung cancer, sarcoidosis, etc.). Often hidden diseases such as tuberculosis, cancer, etc. are detected during screening fluorographic examinations. With the advent of computed tomography, the importance of X-ray examination of the lungs has increased. An important place in the study of pulmonary blood flow belongs to radionuclide research. Indications for radiation examination of the lungs are very wide (cough, sputum production, shortness of breath, fever, etc.).
Radiation examination allows you to diagnose the disease, clarify the localization and extent of the process, monitor the dynamics, monitor recovery, and detect complications.
The leading role in the study of the lungs belongs to X-ray examination. Among the research methods, fluoroscopy and radiography should be noted, which allow assessing both morphological and functional changes. The methods are simple and not burdensome for the patient, highly informative, and publicly available. Typically, survey images are taken in frontal and lateral projections, targeted images, superexposed (super-rigid, sometimes replacing tomography). To identify fluid accumulation in the pleural cavity, photographs are taken in a later position on the affected side. In order to clarify the details (the nature of the contours, the homogeneity of the shadow, the condition of the surrounding tissues, etc.), tomography is performed. For mass examination of the chest organs, fluorography is used. Contrast methods include bronchography (to detect bronchiectasis), angiopulmonography (to determine the extent of the process, for example in lung cancer, to detect thromboembolism of the branches of the pulmonary artery).
X-ray anatomy. Analysis of X-ray data of the chest organs is carried out in a certain sequence. Evaluated:
1) image quality (correct positioning of the patient, degree of film exposure, capture volume, etc.),
2) the condition of the chest as a whole (shape, size, symmetry of the pulmonary fields, position of the mediastinal organs),
3) the condition of the skeleton that forms the chest (shoulder girdle, ribs, spine, collarbones),
4) soft tissues (skin strip over the collarbones, shadow and sternoclavicular muscles, mammary glands),
5) state of the diaphragm (position, shape, contours, sinuses),
6) condition of the roots of the lungs (position, shape, width, condition of the outer skin, structure),
7) state of the pulmonary fields (size, symmetry, pulmonary pattern, transparency),
8) condition of the mediastinal organs. It is necessary to study the bronchopulmonary segments (name, location).
X-ray semiotics of lung diseases is extremely diverse. However, this diversity can be reduced to several groups of characteristics.
1. Morphological characteristics:
1) dimming
2) enlightenment
3) a combination of darkening and brightening
4) changes in pulmonary pattern
5) root pathology
2. Functional characteristics:
1) change in the transparency of the lung tissue in the inhalation and exhalation phases
2) mobility of the diaphragm during breathing
3) paradoxical movements of the diaphragm
4) movement of the median shadow in the inhalation and exhalation phases. Having detected pathological changes, it is necessary to decide what disease they are caused by. It is usually impossible to do this “at first glance” if there are no pathognomonic symptoms (needle, badge, etc.). The task is made easier if you isolate the radiological syndrome. The following syndromes are distinguished:
1. Total or subtotal blackout syndrome:
1) intrapulmonary opacities (pneumonia, atelectasis, cirrhosis, hiatal hernia),
2) extrapulmonary opacities (exudative pleurisy, moorings). The distinction is based on two features: the structure of the darkening and the position of the mediastinal organs.
For example, the shadow is homogeneous, the mediastinum is shifted towards the lesion - atelectasis; the shadow is homogeneous, the heart is shifted to the opposite side - exudative pleurisy.
2. Restricted dimming syndrome:
1) intrapulmonary (lobe, segment, subsegment),
2) extrapulmonary ( pleural effusion, changes in the ribs and mediastinal organs, etc.).
Limited darkening is the most difficult way of diagnostic decoding (“oh, not lungs - these lungs!”). They occur in pneumonia, tuberculosis, cancer, atelectasis, thromboembolism of the branches of the pulmonary artery, etc. Consequently, the detected shadow should be assessed in terms of position, shape, size, nature of the contours, intensity and homogeneity, etc.
Round (spherical) darkening syndrome - in the form of one or several foci that have a more or less rounded shape measuring more than one cm. They can be homogeneous or heterogeneous (due to decay and calcification). A rounded shadow must be determined in two projections.
According to localization, rounded shadows can be:
1) intrapulmonary (inflammatory infiltrate, tumor, cysts, etc.) and
2) extrapulmonary, originating from the diaphragm, chest wall, mediastinum.
Today there are about 200 diseases that cause a round shadow in the lungs. Most of them are rare.
Therefore, most often it is necessary to carry out differential diagnosis with the following diseases:
1) peripheral lung cancer,
2) tuberculoma,
3) benign tumor,
5) lung abscess and foci of chronic pneumonia,
6) solid metastasis. These diseases account for up to 95% of rounded shadows.
When analyzing a round shadow, one should take into account the localization, structure, nature of the contours, the state of the lung tissue around, the presence or absence of a “path” to the root, etc.
4.0 focal (focal-like) darkenings are round or irregularly shaped formations with a diameter of 3 mm to 1.5 cm. Their nature is varied (inflammatory, tumor, cicatricial changes, areas of hemorrhage, atelectasis, etc.). They can be single, multiple or disseminated and vary in size, location, intensity, nature of contours, and changes in the pulmonary pattern. So, when localization of foci in the area of the apex of the lung, subclavian space, one should think about tuberculosis. Uneven contours usually characterize inflammatory processes, peripheral cancer, foci of chronic pneumonia, etc. The intensity of the foci is usually compared with the pulmonary pattern, rib, and median shadow. In differential diagnosis, dynamics (increase or decrease in the number of lesions) are also taken into account.
Focal shadows are most often found in tuberculosis, sarcoidosis, pneumonia, metastases of malignant tumors, pneumoconiosis, pneumosclerosis, etc.
5. Dissemination syndrome - spread of multiple focal shadows in the lungs. Today there are over 150 diseases that can cause this syndrome. The main delimiting criteria are:
1) sizes of lesions - miliary (1-2 mm), small (3-4 mm), medium (5-8 mm) and large (9-12 mm),
2) clinical manifestations,
3) preferential localization,
4) dynamics.
Miliary dissemination is characteristic of acute disseminated (miliary) tuberculosis, nodular pneumoconiosis, sarcoidosis, carcinomatosis, hemosiderosis, histiocytosis, etc.
When assessing the X-ray picture, one should take into account the localization, uniformity of dissemination, the state of the pulmonary pattern, etc.
Dissemination with focal sizes greater than 5 mm reduces the diagnostic task to distinguishing between focal pneumonia, tumor dissemination, and pneumosclerosis.
Diagnostic errors in dissemination syndrome are quite frequent and amount to 70-80%, and therefore adequate therapy is delayed. Currently, disseminated processes are divided into: 1) infectious (tuberculosis, mycoses, parasitic diseases, HIV infection, respiratory distress syndrome), 2) non-infectious (pneumoconiosis, allergic vasculitis, drug changes, radiation consequences, post-transplant changes, etc.).
About half of all disseminated lung diseases are related to processes of unknown etiology. For example, idiopathic fibrosing alveolitis, sarcoidosis, histiocytosis, idiopathic hemosiderosis, vasculitis. In some systemic diseases, dissemination syndrome is also observed (rheumatoid diseases, liver cirrhosis, hemolytic anemia, heart disease, kidney disease, etc.).
Recently, X-ray computed tomography (XCT) has provided great assistance in the differential diagnosis of disseminated processes in the lungs.
6. Clearance syndrome. Clearances in the lungs are divided into limited (cavity formations - ring-shaped shadows) and diffuse. Diffuse, in turn, are divided into structureless (pneumothorax) and structural (pulmonary emphysema).
Ring shadow (clearance) syndrome manifests itself in the form of a closed ring (in two projections). If a ring-shaped clearing is detected, it is necessary to establish the location, wall thickness, and condition of the lung tissue around. Hence, they distinguish:
1) thin-walled cavities, which include bronchial cysts, racemose bronchiectasis, post-pneumonic (false) cysts, sanitized tuberculous cavities, emphysematous bullae, cavities with staphylococcal pneumonia;
2) unevenly thick cavity walls (disintegrating peripheral cancer);
3) uniformly thick walls of the cavity (tuberculous cavities, lung abscess).
7. Pathology of the pulmonary pattern. The pulmonary pattern is formed by the branches of the pulmonary artery and appears as linear shadows located radially and not reaching the costal margin by 1-2 cm. The pathologically altered pulmonary pattern can be enhanced or depleted.
1) Strengthening of the pulmonary pattern manifests itself in the form of coarse additional stringy formations, often randomly located. Often it becomes loopy, cellular, and chaotic.
Strengthening and enrichment of the pulmonary pattern (per unit area of lung tissue there is an increase in the number of elements of the pulmonary pattern) is observed with arterial congestion of the lungs, congestion in the lungs, and pneumosclerosis. Strengthening and deformation of the pulmonary pattern is possible:
a) small-cell type and b) large-cell type (pneumosclerosis, bronchiectasis, cystic lung).
Strengthening of the pulmonary pattern can be limited (pneumofibrosis) and diffuse. The latter occurs in fibrosing alveolitis, sarcoidosis, tuberculosis, pneumoconiosis, histiocytosis X, tumors (cancerous lymphangitis), vasculitis, radiation injuries, etc.
Depletion of the pulmonary pattern. At the same time, there are fewer elements of the pulmonary pattern per unit area of the lung. Depletion of the pulmonary pattern is observed with compensatory emphysema, underdevelopment of the arterial network, valve blockage of the bronchus, progressive pulmonary dystrophy (disappearing lung), etc.
The disappearance of the pulmonary pattern is observed with atelectasis and pneumothorax.
8. Pathology of roots. There are normal roots, infiltrated roots, stagnant roots, roots with enlarged lymph nodes and fibrosis-unchanged roots.
A normal root is located from 2 to 4 ribs, has a clear outer contour, the structure is heterogeneous, the width does not exceed 1.5 cm.
At the core differential diagnosis pathologically altered roots, the following points are taken into account:
1) one or two sided lesions,
2) changes in the lungs,
3) clinical picture (age, ESR, changes in blood, etc.).
The infiltrated root appears expanded, structureless with an unclear outer contour. Occurs in inflammatory lung diseases and tumors.
Stagnant roots look exactly the same. However, the process is two-sided and there are usually changes in the heart.
Roots with enlarged lymph nodes are structureless, expanded, with a clear outer boundary. Sometimes there is polycyclicity, a symptom of “backstage”. Occurs in systemic blood diseases, metastases of malignant tumors, sarcoidosis, tuberculosis, etc.
The fibrotic root is structural, usually displaced, often has calcified lymph nodes and, as a rule, there are fibrotic changes in the lungs.
9. The combination of darkening and clearing is a syndrome that is observed in the presence of a decay cavity of a purulent, caseous or tumor nature. Most often it occurs in the cavitary form of lung cancer, tuberculosis cavity, disintegrating tuberculosis infiltrate, lung abscess, suppurating cysts, bronchiectasis, etc.
10. Pathology of the bronchi:
1) violation of bronchial obstruction due to tumors and foreign bodies. There are three degrees of bronchial obstruction (hypoventilation, ventilatory obstruction, atelectasis),
2) bronchiectasis (cylindrical, saccular and mixed bronchiectasis),
3) deformation of the bronchi (with pneumosclerosis, tuberculosis and other diseases).
RADIATION STUDY OF THE HEART AND GREAT VESSELS
Radiation diagnostics of diseases of the heart and large vessels has come a long way in its development, full of triumph and drama.
The great diagnostic role of X-ray cardiology has never been in doubt. But this was her youth, a time of loneliness. In the last 15-20 years, there has been a technological revolution in diagnostic radiology. Thus, in the 70s, ultrasound devices were created that made it possible to look inside the cavities of the heart and study the condition of the drip apparatus. Later, dynamic scintigraphy made it possible to judge the contractility of individual segments of the heart and the nature of blood flow. In the 80s, computerized methods of obtaining images entered the practice of cardiology: digital coronary and ventriculography, CT, MRI, cardiac catheterization.
Recently, the opinion has become widespread that traditional X-ray examination of the heart has become obsolete as a technique for examining cardiac patients, since the main methods for examining the heart are ECG, ultrasound, and MRI. However, in assessing pulmonary hemodynamics, which reflects the functional state of the myocardium, X-ray examination retains its advantages. It not only allows you to identify changes in the vessels of the pulmonary circulation, but also provides an idea of the chambers of the heart that led to these changes.
Thus, radiation examination of the heart and large vessels includes:
non-invasive methods (fluoroscopy and radiography, ultrasound, CT, MRI)
invasive methods (angiocardiography, ventriculography, coronary angiography, aortography, etc.)
Radionuclide methods make it possible to judge hemodynamics. Consequently, today radiology diagnostics in cardiology is experiencing its maturity.
X-ray examination of the heart and great vessels.
Method value. X-ray examination is part of the general clinical examination of the patient. The goal is to establish the diagnosis and nature of hemodynamic disorders (the choice of treatment method depends on this - conservative, surgical). In connection with the use of URI in combination with cardiac catheterization and angiography, broad prospects have opened up in the study of circulatory disorders.
Research methods
1) Fluoroscopy is the technique with which the study begins. It allows you to get an idea of the morphology and give a functional description of the shadow of the heart as a whole and its individual cavities, as well as large vessels.
2) Radiography objectifies the morphological data obtained during fluoroscopy. Its standard projections:
a) front straight
b) right anterior oblique (45°)
c) left anterior oblique (45°)
d) left side
Signs of oblique projections:
1) Right oblique - triangular shape of the heart, gas bubble of the stomach in front, along the posterior contour on top is the ascending aorta, the left atrium, below - the right atrium; along the anterior contour, the aorta is determined from above, then there is the cone of the pulmonary artery and, below, the arch of the left ventricle.
2) Left oblique - oval in shape, the gastric bladder is behind, between the spine and the heart, the bifurcation of the trachea is clearly visible and all parts of the thoracic aorta are identified. All chambers of the heart open onto the circuit - the atrium is on top, the ventricles are below.
3) Examination of the heart with a contrasted esophagus (the esophagus is normally located vertically and is adjacent to the arch of the left atrium for a considerable length, which allows one to determine its condition). With enlargement of the left atrium, there is a displacement of the esophagus along an arc of large or small radius.
4) Tomography - clarifies the morphological features of the heart and large vessels.
5) X-ray kymography, electrokymography - methods of functional study of myocardial contractility.
6) X-ray cinematography - filming the work of the heart.
7) Catheterization of the cavities of the heart (determining blood oxygen saturation, measuring pressure, determining the minute and stroke volume of the heart).
8) Angiocardiography more accurately determines anatomical and hemodynamic disorders in heart defects (especially congenital ones).
X-ray data study plan
1. Study of the skeleton of the chest (attention is drawn to anomalies in the development of the ribs, spine, curvature of the latter, “abnormalities” of the ribs during coarctation of the aorta, signs of pulmonary emphysema, etc.).
2. Study of the diaphragm (position, mobility, fluid accumulation in the sinuses).
3. Study of the hemodynamics of the pulmonary circulation (the degree of bulging of the pulmonary artery cone, the condition of the roots of the lungs and pulmonary pattern, the presence of pleural lines and Kerley lines, focally infiltrative shadows, hemosiderosis).
4. X-ray morphological study of the cardiovascular shadow
a) position of the heart (oblique, vertical and horizontal).
b) heart shape (oval, mitral, triangular, aortic)
c) heart size. On the right, 1-1.5 cm from the edge of the spine, on the left, 1-1.5 cm not reaching the midclavicular line. We judge the upper limit by the so-called waist of the heart.
5. Determination of the functional characteristics of the heart and large vessels (pulsation, “yoke” symptom, systolic displacement of the esophagus, etc.).
Acquired heart defects
Relevance. The introduction of surgical treatment of acquired defects into surgical practice required radiologists to clarify them (stenosis, insufficiency, their predominance, the nature of hemodynamic disturbances).
Causes: almost all acquired defects are a consequence of rheumatism, rarely septic endocarditis; collagenosis, trauma, atherosclerosis, syphilis can also lead to heart disease.
Mitral valve insufficiency is more common than stenosis. This causes the valve flaps to shrink. Hemodynamic disturbances are associated with the absence of a period of closed valves. During ventricular systole, part of the blood returns to the left atrium. The latter is expanding. During diastole, a larger amount of blood returns to the left ventricle, which is why the latter has to work harder and hypertrophies. With a significant degree of insufficiency, the left atrium expands sharply, its wall sometimes becomes thinner to a thin sheet through which blood can be seen.
Violation of intracardiac hemodynamics with this defect is observed when 20-30 ml of blood is thrown into the left atrium. For a long time, no significant changes in circulatory disturbances in the pulmonary circle were observed. Congestion in the lungs occurs only in advanced stages - with left ventricular failure.
X-ray semiotics.
The shape of the heart is mitral (the waist is flattened or bulging). The main symptom is an enlargement of the left atrium, sometimes extending onto the right contour in the form of an additional third arch (symptom of “crossover”). The degree of enlargement of the left atrium is determined in the first oblique position in relation to the spine (1-III).
The contrasted esophagus deviates along an arc of large radius (more than 6-7 cm). There is an expansion of the tracheal bifurcation angle (up to 180) and a narrowing of the lumen of the right main bronchus. The third arc along the left contour prevails over the second. The aorta is of normal size and fills well. Among the X-ray functional symptoms, the most noteworthy are the “yoke” symptom (systolic expansion), systolic displacement of the esophagus, and Roesler’s symptom (transfer pulsation of the right root.
After surgery, all changes are eliminated.
Stenosis of the left mitral valve (fusion of the leaflets).
Hemodynamic disturbances are observed with a decrease in the mitral orifice by more than half (about one sq. cm). Normally, the mitral orifice is 4-6 sq. see, pressure in the left atrium cavity is 10 mm Hg. With stenosis, the pressure increases by 1.5-2 times. The narrowing of the mitral orifice prevents the expulsion of blood from the left atrium into the left ventricle, the pressure in which rises to 15-25 mm Hg, which complicates the outflow of blood from the pulmonary circulation. The pressure in the pulmonary artery increases (this is passive hypertension). Later, active hypertension is observed as a result of irritation of the baroreceptors of the endocardium of the left atrium and the mouth of the pulmonary veins. As a result, a reflex spasm of arterioles and larger arteries develops - the Kitaev reflex. This is the second barrier to blood flow (the first is the narrowing of the mitral valve). This increases the load on the right ventricle. Prolonged spasm of the arteries leads to cardiogenic pulmonary fibrosis.
Clinic. Weakness, shortness of breath, cough, hemoptysis. X-ray semiotics. The earliest and most characteristic sign is a violation of the hemodynamics of the pulmonary circulation - congestion in the lungs (expansion of the roots, increased pulmonary pattern, Kerley lines, septal lines, hemosiderosis).
X-ray symptoms. The heart has a mitral configuration due to the sharp bulging of the pulmonary artery cone (the second arch predominates over the third). There is hypertrophy of the left atrium. The coitrasted esophagus is deviated along a small radius arc. There is an upward displacement of the main bronchi (more than the left one), an increase in the angle of tracheal bifurcation. The right ventricle is enlarged, the left one is usually small. The aorta is hypoplastic. Heart contractions are calm. Calcification of the valves is often observed. During catheterization, an increase in pressure is noted (1-2 times higher than normal).
Aortic valve insufficiency
Hemodynamic disturbances with this heart defect are reduced to incomplete closure of the aortic valves, which during diastole leads to the return of 5 to 50% of the blood to the left ventricle. The result is dilation of the left ventricle due to hypertrophy. At the same time, the aorta expands diffusely.
The clinical picture includes palpitations, heart pain, fainting and dizziness. The difference in systolic and diastolic pressures is large (systolic pressure is 160 mm Hg, diastolic pressure is low, sometimes reaching 0). The carotid “dancing” symptom, Mussy’s symptom, and pallor of the skin are observed.
X-ray semiotics. An aortic configuration of the heart (deep, emphasized waist), enlargement of the left ventricle, and rounding of its apex are observed. All parts of the thoracic aorta expand evenly. Of the X-ray functional signs, noteworthy is the increase in the amplitude of heart contractions and increased pulsation of the aorta (pulse celer et altus). The degree of aortic valve insufficiency is determined by angiography (grade 1 - a narrow stream, in stage 4 - the entire cavity of the left ventricle is co-traced in diastole).
Aortic stenosis (narrowing more than 0.5-1 cm 2, normal 3 cm 2).
Hemodynamic disturbances result in obstructed blood outflow from the left ventricle into the aorta, which leads to prolongation of systole and increased pressure in the cavity of the left ventricle. The latter sharply hypertrophies. With decompensation, congestion occurs in the left atrium, and then in the lungs, then in the systemic circulation.
At the clinic, people notice heart pain, dizziness, and fainting. There is systolic tremor, pulse parvus et tardus. The defect remains compensated for a long time.
X-ray semiotics. Left ventricular hypertrophy, rounding and lengthening of its arch, aortic configuration, poststenotic dilation of the aorta (its ascending part). Heart contractions are tense and reflect difficult ejection of blood. Calcification of the aortic valves is quite common. With decompensation, mitralization of the heart develops (the waist is smoothed due to an enlargement of the left atrium). Angiography reveals narrowing of the aortic opening.
Pericarditis
Etiology: rheumatism, tuberculosis, bacterial infections.
1. fibrous pericarditis
2. effusion (exudative) pericarditis Clinic. Pain in the heart, pallor, cyanosis, shortness of breath, swelling of the veins of the neck.
The diagnosis of dry pericarditis is usually made based on clinical findings (pericardial friction rub). When fluid accumulates in the pericardial cavity (the minimum amount that can be detected x-ray is 30-50 ml), a uniform increase in the size of the heart is noted, the latter taking on a trapezoidal shape. The arcs of the heart are smoothed and not differentiated. The heart is widely adjacent to the diaphragm, its diameter prevails over its length. The cardiophrenic angles are sharp, the vascular bundle is shortened, and there is no congestion in the lungs. Displacement of the esophagus is not observed, cardiac pulsation is sharply weakened or absent, but preserved in the aorta.
Adhesive or compressive pericarditis is the result of fusion between both layers of the pericardium, as well as between the pericardium and the mediastinal pleura, which makes it difficult for the heart to contract. With calcification - “shell heart”.
Myocarditis
There are:
1. infectious-allergic
2. toxic-allergic
3. idiopathic myocarditis
Clinic. Pain in the heart, increased pulse rate with weak filling, rhythm disturbance, signs of heart failure. At the apex of the heart there is a systolic murmur, muffled heart sounds. Noticeable congestion in the lungs.
The X-ray picture is due to myogenic dilatation of the heart and signs of decreased contractile function of the myocardium, as well as a decrease in the amplitude of heart contractions and their increase in frequency, which ultimately leads to stagnation in the pulmonary circulation. The main X-ray sign is enlargement of the ventricles of the heart (mainly the left), trapezoidal shape of the heart, the atria are enlarged to a lesser extent than the ventricles. The left atrium may extend onto the right circuit, deviation of the contrasted esophagus is possible, heart contractions are shallow and accelerated. When left ventricular failure occurs, stagnation appears in the lungs due to obstruction of blood outflow from the lungs. With the development of right ventricular failure, the superior vena cava expands and edema appears.
X-RAY STUDY OF THE GASTROINTESTINAL TRACT
Diseases of the digestive system occupy one of the first places in the overall structure of morbidity, admission and hospitalization. Thus, about 30% of the population have complaints from the gastrointestinal tract, 25.5% of patients are admitted to hospitals for emergency care, and pathology of the digestive organs accounts for 15% of overall mortality.
A further increase in diseases is predicted, mainly those in the development of which stress, dyskinetic, immunological and metabolic mechanisms play a role (peptic ulcer, colitis, etc.). The course of the disease becomes more severe. Often diseases of the digestive organs are combined with each other and diseases of other organs and systems; damage to the digestive organs is possible due to systemic diseases (scleroderma, rheumatism, diseases of the hematopoietic system, etc.).
The structure and function of all parts of the digestive canal can be studied using radiation methods. Optimal radiation diagnostic techniques have been developed for each organ. Establishing indications for radiation examination and its planning are carried out on the basis of anamnestic and clinical data. Endoscopic examination data is also taken into account, allowing one to examine the mucous membrane and obtain material for histological examination.
X-ray examination of the digestive canal occupies a special place in X-ray diagnostics:
1) recognition of diseases of the esophagus, stomach and colon is based on a combination of transillumination and photography. Here the importance of the experience of a radiologist is most clearly demonstrated,
2) examination of the gastrointestinal tract requires preliminary preparation (examination on an empty stomach, use of cleansing enemas, laxatives).
3) the need for artificial contrast (an aqueous suspension of barium sulfate, the introduction of air into the stomach cavity, oxygen into the abdominal cavity, etc.),
4) examination of the esophagus, stomach and colon is carried out mainly “from the inside” from the mucous membrane.
X-ray examination, due to its simplicity, universal accessibility and high efficiency, allows:
1) recognize most diseases of the esophagus, stomach and colon,
2) monitor the results of treatment,
3) carry out dynamic observations for gastritis, peptic ulcers and other diseases,
4) screen patients (fluorography).
Methods for preparing barium suspension. The success of X-ray examination depends, first of all, on the method of preparing the barium suspension. Requirements for an aqueous suspension of barium sulfate: maximum fineness, mass volume, adhesiveness and improvement of organoleptic properties. There are several ways to prepare barium suspension:
1. Boiling at the rate of 1:1 (per 100.0 BaS0 4 100 ml of water) for 2-3 hours.
2. Use of “Voronezh” type mixers, electric mixers, ultrasonic units, micro-pulverizers.
3. Recently, in order to improve conventional and double contrast, they have been trying to increase the mass volume of barium sulfate and its viscosity through various additives, such as distilled glycerin, polyglucin, sodium citrate, starch, etc.
4. Ready-made forms of barium sulfate: sulfobar and other proprietary preparations.
X-ray anatomy
The esophagus is a hollow tube 20-25 cm long, 2-3 cm wide. The contours are smooth and clear. 3 physiological constrictions. Sections of the esophagus: cervical, thoracic, abdominal. Folds - about longitudinal ones in the amount of 3-4. Projections of the study (direct, right and left oblique positions). The speed of movement of barium suspension through the esophagus is 3-4 seconds. Ways to slow down are to study in a horizontal position and take a thick paste-like mass. Research phases: tight filling, study of pneumorelief and mucosal relief.
Stomach. When analyzing the x-ray picture, it is necessary to have an idea of the nomenclature of its various sections (cardiac, subcardial, body of the stomach, sinus, antrum, pyloric section, gastric vault).
The shape and position of the stomach depend on the constitution, gender, age, tone, and position of the person being examined. There is a hook-shaped stomach (vertically located stomach) in asthenics and a horn (horizontally located stomach) in hypersthenic individuals.
The stomach is located mostly in the left hypochondrium, but can move within a very wide range. The most variable position of the lower border (normally 2-4 cm above the crest of the iliac bones, but in thin people it is much lower, often above the entrance to the pelvis). The most fixed sections are the cardiac and pyloric. The width of the retrogastric space is of greater importance. Normally, it should not exceed the width of the lumbar vertebral body. During volumetric processes, this distance increases.
The relief of the gastric mucosa is formed by folds, interfold spaces and gastric fields. Folds are represented by stripes of enlightenment 0.50.8 cm wide. However, their sizes are highly variable and depend on gender, constitution, stomach tone, degree of distension, and mood. Gastric fields are defined as small filling defects on the surface of the folds due to elevations, at the top of which the ducts of the gastric glands open; their sizes normally do not exceed 3 mm and look like a thin mesh (the so-called thin relief of the stomach). With gastritis, it becomes rough, reaching a size of 5-8mm, resembling a “cobblestone street”.
Secretion of the gastric glands on an empty stomach is minimal. Normally, the stomach should be empty.
Stomach tone is the ability to embrace and hold a sip of barium suspension. There are normotonic, hypertonic, hypotonic and atonic stomachs. With normal tone, the barium suspension drops slowly, with low tone it drops quickly.
Peristalsis is the rhythmic contraction of the stomach walls. Attention is paid to rhythm, duration of individual waves, depth and symmetry. There are deep, segmenting, medium, superficial peristalsis and its absence. To stimulate peristalsis, it is sometimes necessary to resort to a morphine test (s.c. 0.5 ml of morphine).
Evacuation. During the first 30 minutes, half of the ingested aqueous suspension of barium sulfate is evacuated from the stomach. The stomach is completely freed from barium suspension within 1.5 hours. In a horizontal position on the back, emptying slows down sharply, while on the right side it accelerates.
Palpation of the stomach is normally painless.
The duodenum has the shape of a horseshoe, its length is from 10 to 30 cm, its width is from 1.5 to 4 cm. It consists of a bulb, upper horizontal, descending and lower horizontal parts. The pattern of the mucous membrane is feathery, inconsistent due to the Kerckring folds. In addition, there are small and
greater curvature, medial and lateral recesses, as well as the anterior and posterior walls of the duodenum.
Research methods:
1) usual classical examination (during examination of the stomach)
2) study under conditions of hypotension (probe and tubeless) using atropine and its derivatives.
The small intestine (ileum and jejunum) is examined similarly.
X-ray semiotics of diseases of the esophagus, stomach, colon (main syndromes)
X-ray symptoms of diseases of the digestive tract are extremely diverse. Its main syndromes:
1) change in the position of the organ (dislocation). For example, displacement of the esophagus by enlarged lymph nodes, a tumor, a cyst, the left atrium, displacement due to atelectasis, pleurisy, etc. The stomach and intestines are displaced by an enlarged liver, hiatal hernia, etc.;
2) deformation. Stomach in the form of a pouch, snail, retort, hourglass; duodenum - a trefoil-shaped bulb;
3) change in size: increase (achalasia of the esophagus, stenosis of the pyloroduodenal zone, Hirschsprung’s disease, etc.), decrease (infiltrating form of gastric cancer),
4) narrowing and expansion: diffuse (achalasia of the esophagus, gastric stenosis, intestinal obstruction, etc., local (tumor, scar, etc.);
5) filling defect. Usually determined by tight filling due to a space-occupying formation (exophytically growing tumor, foreign bodies, bezoars, fecal stone, food debris and
6) “niche” symptom - is the result of ulceration of the wall during an ulcer, tumor (cancer). A “niche” is distinguished on the contour in the form of a diverticulum-like formation and on the relief in the form of a “stagnant spot”;
7) changes in the folds of the mucosa (thickening, breakage, rigidity, convergence, etc.);
8) rigidity of the wall during palpation and inflation (the latter does not change);
9) change in peristalsis (deep, segmenting, superficial, lack of peristalsis);
10) pain on palpation).
Diseases of the esophagus
Foreign bodies. Research methodology (candling, survey photographs). The patient takes 2-3 sips of a thick barium suspension, then 2-3 sips of water. If a foreign body is present, traces of barium remain on its upper surface. Pictures are taken.
Achalasia (inability to relax) is a disorder of the innervation of the esophagogastric junction. X-ray semiotics: clear, even contours of narrowing, the “writing pen” symptom, pronounced suprastenotic expansion, elasticity of the walls, periodic “dropping” of barium suspension into the stomach, absence of a gas bubble of the stomach and the duration of the benign course of the disease.
Esophageal carcinoma. In an exophytically growing form of the disease, X-ray semiotics is characterized by 3 classic signs: filling defect, malignant relief, wall rigidity. In the infiltrative form, there is rigidity of the wall, uneven contours, and changes in the relief of the mucous membrane. It should be differentiated from cicatricial changes after burns, varicose veins, and cardiospasm. With all these diseases, peristalsis (elasticity) of the walls of the esophagus is preserved.
Stomach diseases
Stomach cancer. In men it ranks first in the structure of malignant tumors. In Japan it is a national catastrophe; in the USA there is a downward trend in the disease. The predominant age is 40-60 years.
Classification. The most common division of stomach cancer is:
1) exophytic forms (polypoid, mushroom-shaped, cauliflower-shaped, cup-shaped, plaque-shaped form with and without ulceration),
2) endophytic forms (ulcerative-infiltrative). The latter account for up to 60% of all gastric cancers,
3) mixed forms.
Stomach cancer metastasizes to the liver (28%), retroperitoneal lymph nodes (20%), peritoneum (14%), lungs (7%), bones (2%). Most often localized in the antrum (over 60%) and in the upper parts of the stomach (about 30%).
Clinic. Cancer often masquerades as gastritis, peptic ulcers, or cholelithiasis for years. Hence, for any gastric discomfort, X-ray and endoscopic examination is indicated.
X-ray semiotics. There are:
1) general signs (filling defect, malignant or atypical relief of the mucosa, absence of peristoglytics), 2) specific signs (in exophytic forms - a symptom of breakage of folds, flow around, splashing, etc.; in endfit forms - straightening of the lesser curvature, unevenness of the contour, deformation of the stomach; with total damage - a symptom of microgastrium.). In addition, with infiltrative forms, the filling defect is usually poorly expressed or absent, the relief of the mucous membrane almost does not change, the symptom of flat concave arcs (in the form of waves along the lesser curvature), the symptom of Gaudek's steps, is often observed.
X-ray semiotics of gastric cancer also depends on the location. When the tumor is localized in the gastric outlet, the following is noted:
1) elongation of the pyloric region by 2-3 times, 2) conical narrowing of the pyloric region occurs, 3) a symptom of undermining of the base of the pyloric region is observed 4) dilation of the stomach.
With cancer of the upper section (these are cancers with a long “silent” period) the following occur: 1) the presence of an additional shadow against the background of a gas bubble,
2) lengthening of the abdominal esophagus,
3) destruction of the mucosal relief,
4) the presence of edge defects,
5) flow symptom - “deltas”,
6) splashing symptom,
7) blunting of the Hiss angle (normally it is acute).
Cancers of the greater curvature are prone to ulceration - deep in the form of a well. However, any benign tumor in this area is prone to ulceration. Therefore, one must be careful with the conclusion.
Modern radiodiagnosis of gastric cancer. Recently, the number of cancers in the upper parts of the stomach has increased. Among all methods of radiological diagnostics, X-ray examination with tight filling remains the basic one. It is believed that diffuse forms of cancer today account for from 52 to 88%. In this form, cancer spreads predominantly intramural for a long time (from several months to one year or more) with minimal changes on the surface of the mucosa. Hence, endoscopy is often ineffective.
The leading radiological signs of intramural growing cancer should be considered uneven contour of the wall with tight filling (often one portion of barium suspension is not enough) and its thickening at the site of tumor infiltration with double contrast for 1.5 - 2.5 cm.
Due to the small extent of the lesion, peristalsis is often blocked by neighboring areas. Sometimes diffuse cancer manifests itself as a sharp hyperplasia of the folds of the mucosa. Often the folds converge or go around the affected area, resulting in the effect of no folds - (bald space) with the presence of a small barium spot in the center, caused not by ulceration, but by depression of the stomach wall. In these cases, methods such as ultrasound, CT, and MRI are useful.
Gastritis. Recently, in the diagnosis of gastritis, there has been a shift in emphasis towards gastroscopy with biopsy of the gastric mucosa. However, X-ray examination occupies an important place in the diagnosis of gastritis due to its accessibility and simplicity.
Modern recognition of gastritis is based on changes in the subtle relief of the mucous membrane, but double endogastric contrast is necessary to identify it.
Research methodology. 15 minutes before the test, 1 ml of a 0.1% atropine solution is injected subcutaneously or 2-3 aeron tablets are given (under the tongue). Then the stomach is inflated with a gas-forming mixture, followed by the intake of 50 ml of an aqueous suspension of barium sulfate in the form of an infusion with special additives. The patient is placed in a horizontal position and 23 rotational movements are made, followed by taking pictures on the back and in oblique projections. Then the usual examination is carried out.
Taking into account radiological data, several types of changes in the fine relief of the gastric mucosa are distinguished:
1) finely reticulated or granular (areolas 1-3 mm),
2) modular - (areola size 3-5 mm),
3) coarse nodular - (the size of the areolas is more than 5 mm, the relief is in the form of a “cobblestone street”). In addition, in the diagnosis of gastritis, such signs as the presence of fluid on an empty stomach, rough relief of the mucous membrane, diffuse pain on palpation, pyloric spasm, reflux, etc. are taken into account.
Benign tumors. Among them, polyps and leiomyomas are of greatest practical importance. A single polyp with tight filling is usually defined as a round filling defect with clear, even contours measuring 1-2 cm. Folds of the mucosa bypass the filling defect or the polyp is located on the fold. The folds are soft, elastic, palpation is painless, peristalsis is preserved. Leiomyomas differ from the X-ray semiotics of polyps in the preservation of mucosal folds and significant size.
Bezoars. It is necessary to distinguish between stomach stones (bezoars) and foreign bodies (swallowed bones, fruit pits, etc.). The term bezoar is associated with the name of a mountain goat, in whose stomach stones from licked wool were found.
For several millennia, the stone was considered an antidote and was valued higher than gold, as it supposedly brings happiness, health, and youth.
The nature of stomach bezoars is different. The most common:
1) phytobezoars (75%). Formed when eating a large amount of fruits containing a lot of fiber (unripe persimmon, etc.),
2) sebobezoars - occur when eating large amounts of fat with a high melting point (lamb fat),
3) trichobezoars - found in people who have the bad habit of biting off and swallowing hair, as well as in people caring for animals,
4) pixobesoars - the result of chewing resins, gum, gum,
5) shellac-bezoars - when using alcohol substitutes (alcohol varnish, palette, nitro varnish, nitro glue, etc.),
6) bezoars can occur after vagotomies,
7) bezoars consisting of sand, asphalt, starch and rubber are described.
Bezoars usually occur clinically under the guise of a tumor: pain, vomiting, weight loss, palpable swelling.
X-ray bezoars are defined as a filling defect with uneven contours. Unlike cancer, the filling defect shifts during palpation, peristalsis and the relief of the mucous membrane are preserved. Sometimes a bezoar simulates lymphosarcoma, gastric lymphoma.
Peptic ulcer of the stomach and duodenum is extremely common. 7-10% of the planet's population suffers. Annual exacerbations are observed in 80% of patients. In the light of modern concepts, this is a general chronic, cyclical, recurrent disease, which is based on complex etiological and pathological mechanisms of ulcer formation. This is the result of the interaction of aggression and defense factors (too strong aggression factors with weak defense factors). The aggression factor is peptic proteolysis during prolonged hyperchlorhydria. The protective factors include the mucous barrier, i.e. high regenerative ability of the mucosa, stable nervous trophism, good vascularization.
During the course of a peptic ulcer, three stages are distinguished: 1) functional disorders in the form of gastroduodenitis, 2) the stage of a formed ulcerative defect and 3) the stage of complications (penetration, perforation, bleeding, deformation, degeneration into cancer).
X-ray manifestations of gastroduodenitis: hypersecretion, impaired motility, restructuring of the mucosa in the form of coarse expanded cushion-shaped folds, rough microrelief, spasm or gaping of the transvaricus, duodenogastric reflux.
Signs of peptic ulcer disease are reduced to the presence of a direct sign (a niche on the contour or on the relief) and indirect signs. The latter, in turn, are divided into functional and morphological. Functional ones include hypersecretion, pyloric spasm, slower evacuation, local spasm in the form of a “pointing finger” on the opposite wall, local hypermatility, changes in peristalsis (deep, segmented), tone (hypertonicity), duodenogastric reflux, gastroesophageal reflux, etc. Morphological signs are filling defect due to the inflammatory shaft around the niche, convergence of folds (during scarring of the ulcer), cicatricial deformation (stomach in the form of a pouch, hourglass, snail, cascade, duodenal bulb in the form of a trefoil, etc.).
More often, the ulcer is localized in the area of the lesser curvature of the stomach (36-68%) and proceeds relatively favorably. In the antrum, ulcers are also located relatively often (9-15%) and are found, as a rule, in young people, accompanied by signs of duodenal ulcer (late hunger pain, heartburn, vomiting, etc.). X-ray diagnosis is difficult due to pronounced motor activity, rapid passage of barium suspension, and difficulty in removing the ulcer to the contour. Often complicated by penetration, bleeding, perforation. In the cardiac and subcardial region, ulcers are localized in 2-18% of cases. Usually found in older people and present certain difficulties for endoscopic and radiological diagnosis.
The shape and size of the niches in peptic ulcer disease are variable. Often (13-15%) there is a multiplicity of lesions. The frequency of identifying a niche depends on many reasons (location, size, presence of fluid in the stomach, filling of the ulcer with mucus, blood clot, food debris) and ranges from 75 to 93%. Quite often there are giant niches (over 4 cm in diameter), penetrating ulcers (2-3 niches of complexity).
An ulcerative (benign) niche should be differentiated from a cancerous one. Cancer niches have a number of features:
1) the predominance of the longitudinal size over the transverse,
2) ulceration is located closer to the distal edge of the tumor,
3) the niche has an irregular shape with bumpy outlines, usually does not extend beyond the contour, the niche is painless on palpation, plus signs characteristic of a cancerous tumor.
Ulcer niches are usually
1) located near the lesser curvature of the stomach,
2) extend beyond the contours of the stomach,
3) have a cone shape,
4) the diameter is larger than the length,
5) painful on palpation, plus signs of peptic ulcer disease.
RADIATION STUDY OF THE MUSCULOSKETAL SYSTEM
In 1918, the world's first laboratory for studying the anatomy of humans and animals using x-rays was opened at the State X-ray Radiological Institute in Petrograd.
The X-ray method made it possible to obtain new data on the anatomy and physiology of the musculoskeletal system: to study the structure and function of bones and joints intravitally, in the whole organism, when a person is exposed to various environmental factors.
A group of domestic scientists made a great contribution to the development of osteopathology: S.A. Reinberg, D.G. Rokhlin, PA. Dyachenko and others.
The X-ray method is the leading one in the study of the musculoskeletal system. Its main methods are: radiography (in 2 projections), tomography, fistulography, images with magnified X-ray images, contrast techniques.
An important method in the study of bones and joints is X-ray computed tomography. Magnetic resonance imaging should also be recognized as a valuable method, especially when examining bone marrow. To study metabolic processes in bones and joints, radionuclide diagnostic methods are widely used (bone metastases are detected before X-ray examination by 3-12 months). Sonography opens up new ways to diagnose diseases of the musculoskeletal system, especially in the diagnosis of foreign bodies that weakly absorb X-rays, articular cartilage, muscles, ligaments, tendons, accumulation of blood and pus in the periosseous tissues, periarticular cysts, etc.
Radiation research methods allow:
1. monitor the development and formation of the skeleton,
2. assess the morphology of the bone (shape, outline, internal structure, etc.),
3. recognize traumatic injuries and diagnose various diseases,
4. judge functional and pathological changes (vibration disease, marching foot, etc.),
5. study the physiological processes in bones and joints,
6. evaluate the response to various factors (toxic, mechanical, etc.).
Radiation anatomy.
Maximum structural strength with minimal waste of building material is characterized by the anatomical features of the structure of bones and joints (the femur can withstand a load along the longitudinal axis of 1.5 tons). Bone is a favorable object for x-ray examination, because contains many inorganic substances. Bone consists of bone beams and trabeculae. In the cortical layer they are closely adjacent, forming a uniform shadow, in the epiphyses and metaphyses they are located at some distance, forming a spongy substance, with bone marrow tissue between them. The relationship between the bone beams and the medullary spaces creates the bone structure. Hence, in the bone there are: 1) a dense compact layer, 2) a spongy substance (cellular structure), 3) a medullary canal in the center of the bone in the form of a lightening. There are tubular, short, flat and mixed bones. In each tubular bone, there are epiphysis, metaphysis and diaphysis, as well as apophyses. The epiphysis is an articular part of the bone covered with cartilage. In children it is separated from the metaphysis by the growth cartilage, in adults by the metaphyseal suture. Apophyses are additional points of ossification. These are the attachment points for muscles, ligaments and tendons. The division of bone into epiphysis, metaphysis and diaphysis is of great clinical importance, because some diseases have a favorite localization (osteomyelitis in the metadiaphysis, tuberculosis affects the pineal gland, Ewing's sarcoma is localized in the diaphysis, etc.). Between the connecting ends of the bones there is a light stripe, the so-called x-ray joint space, caused by cartilage tissue. Good photographs show the joint capsule, joint capsule, and tendon.
Development of the human skeleton.
In its development, the bone skeleton goes through membranous, cartilaginous and bone stages. During the first 4-5 weeks, the fetal skeleton is webbed and not visible on photographs. Developmental disorders during this period lead to changes that make up the group of fibrous dysplasias. At the beginning of the 2nd month of uterine life of the fetus, the membranous skeleton is replaced by cartilaginous skeleton, which is also not reflected on radiographs. Developmental disorders lead to cartilaginous dysplasia. Starting from the 2nd month and up to 25 years, the cartilaginous skeleton is replaced by bone. By the end of the prenatal period, most of the skeleton is osseous and the bones of the fetus are clearly visible on photographs of the pregnant abdomen.
The skeleton of newborns has the following features:
1. the bones are small,
2. they are structureless,
3. at the ends of most bones there are no ossification nuclei yet (the epiphyses are not visible),
4. X-ray joint spaces are large,
5. large brain skull and small facial skull,
6. relatively large orbits,
7. weakly expressed physiological curves of the spine.
The growth of the bone skeleton occurs due to the growth zones in length, in thickness - due to the periosteum and endosteum. At the age of 1-2 years, differentiation of the skeleton begins: ossification points appear, bones synostose, increase in size, and curvatures of the spine appear. The skeleton of the skeleton ends by the age of 20-25. Between 20-25 years and up to 40 years of age, the osteoarticular apparatus is relatively stable. From the age of 40, involutive changes begin (dystrophic changes in articular cartilage), thinning of the bone structure, the appearance of osteoporosis and calcification at the attachment points of ligaments, etc. The growth and development of the osteoarticular system is influenced by all organs and systems, especially the parathyroid glands, pituitary gland and central nervous system.
Plan for studying radiographs of the osteoarticular system. Need to evaluate:
1) shape, position, size of bones and joints,
2) state of the circuits,
3) the state of the bone structure,
4) identify the state of growth zones and ossification nuclei (in children),
5) study the condition of the articular ends of the bones (X-ray joint space),
6) assess the condition of soft tissues.
X-ray semiotics of bone and joint diseases.
The X-ray picture of bone changes in any pathological process consists of 3 components: 1) changes in shape and size, 2) changes in contours, 3) changes in structure. In most cases, the pathological process leads to bone deformation, consisting of lengthening, shortening and curvature, to a change in volume in the form of thickening due to periostitis (hyperostosis), thinning (atrophy) and swelling (cyst, tumor, etc.).
Changes in bone contours: Bone contours are normally characterized by evenness (smoothness) and clarity. Only in the places of attachment of muscles and tendons, in the area of tubercles and tuberosities, the contours are rough. Lack of clarity of contours, their unevenness is often the result of inflammatory or tumor processes. For example, bone destruction as a result of the germination of cancer of the oral mucosa.
All physiological and pathological processes occurring in the bones are accompanied by changes in the bone structure, a decrease or increase in bone beams. A peculiar combination of these phenomena creates in the X-ray image such pictures that are inherent in certain diseases, allowing them to be diagnosed, the phase of development, and complications to be determined.
Structural changes in bone can be in the nature of physiological (functional) and pathological restructuring caused by various reasons (traumatic, inflammatory, tumor, degenerative-dystrophic, etc.).
There are over 100 diseases that are accompanied by changes in the mineral content of the bones. The most common is osteoporosis. This is a decrease in the number of bone beams per unit volume of bone. In this case, the overall volume and shape of the bone usually remain unchanged (if there is no atrophy).
There are: 1) idiopathic osteoporosis, which develops for no apparent reason and 2) with various diseases of internal organs, endocrine glands, as a result of taking medications, etc. In addition, osteoporosis can be caused by nutritional disorders, weightlessness, alcoholism, unfavorable working conditions, prolonged immobilization , exposure to ionizing radiation, etc.
Hence, depending on the causes, osteoporosis is distinguished as physiological (involutive), functional (from inactivity) and pathological (from various diseases). Based on prevalence, osteoporosis is divided into: 1) local, for example, in the area of a jaw fracture after 5-7 days, 2) regional, in particular, involving the area of the lower jaw branch with osteomyelitis 3) widespread, when the area of the body and jaw branches is affected, and 4) systemic, accompanied by damage to the entire bone skeleton.
Depending on the X-ray picture, there are: 1) focal (spotty) and 2) diffuse (uniform) osteoporosis. Spotty osteoporosis is defined as foci of rarefaction of bone tissue ranging in size from 1 to 5 mm (reminiscent of moth-eaten matter). Occurs with osteomyelitis of the jaws in the acute phase of its development. Diffuse (glassy) osteoporosis is more often observed in the jaw bones. In this case, the bone becomes transparent, the structure is broadly looped, the cortical layer becomes thinner in the form of a very narrow dense line. It is observed in old age, with hyperparathyroid osteodystrophy and other systemic diseases.
Osteoporosis can develop within a few days and even hours (with causalgia), with immobilization - in 10-12 days, with tuberculosis it takes several months and even years. Osteoporosis is a reversible process. Once the cause is eliminated, the bone structure is restored.
Hypertrophic osteoporosis is also distinguished. At the same time, against the background of general transparency, individual bone beams appear hypertrophied.
Osteosclerosis is a symptom of bone diseases that are quite common. Accompanied by an increase in the number of bone beams per unit volume of bone and a decrease in interblock bone marrow spaces. At the same time, the bone becomes denser and structureless. The cortex expands, the medullary canal narrows.
There are: 1) physiological (functional) osteosclerosis, 2) idiopathic as a result of developmental anomalies (with marbled disease, myelorheostosis, osteopoikilia) and 3) pathological (post-traumatic, inflammatory, toxic, etc.).
Unlike osteoporosis, osteosclerosis requires quite a long time (months, years) to occur. The process is irreversible.
Destruction is the destruction of bone with its replacement by pathological tissue (granulation, tumor, pus, blood, etc.).
There are: 1) inflammatory destruction (osteomyelitis, tuberculosis, actinomycosis, syphilis), 2) tumor (osteogenic sarcoma, reticulosarcoma, metastases, etc.), 3) degenerative-dystrophic (hyperparathyroid osteodystrophy, osteoarthritis, cysts in deforming osteoarthritis, etc.) .
X-ray, regardless of the reasons, destruction is manifested by clearing. It can appear small or large focal, multifocal and extensive, superficial and central. Therefore, to establish the causes, a thorough analysis of the source of destruction is necessary. It is necessary to determine the location, size, number of lesions, the nature of the contours, the pattern and reaction of the surrounding tissues.
Osteolysis is the complete resorption of bone without its replacement by any pathological tissue. This is the result of deep neurotrophic processes in diseases of the central nervous system, damage to peripheral nerves (tabes dorsalis, syringomyelia, scleroderma, leprosy, lichen planus, etc.). The peripheral (end) parts of the bone undergo resorption ( nail phalanges, articular ends of large and small joints). This process is observed in scleroderma, diabetes mellitus, traumatic injuries, and rheumatoid arthritis.
Osteonecrosis and sequestration are a frequent accompaniment of bone and joint diseases. Osteonecrosis is the necrosis of a section of bone due to malnutrition. At the same time, the amount of liquid elements in the bone decreases (the bone “dries out”) and radiographically such an area is determined in the form of darkening (compaction). There are: 1) aseptic osteonekoosis (with osteochondropathy, thrombosis and embolism of blood vessels), 2) septic (infectious), occurring with osteomyelitis, tuberculosis, actinomycosis and other diseases.
The process of delimiting an area of osteonecrosis is called sequestration, and the rejected area of bone is called sequestration. There are cortical and spongy sequestra, regional, central and total. Sequestration is characteristic of osteomyelitis, tuberculosis, actinomycosis and other diseases.
Changes in bone contours are often associated with periosteal layers (periostitis and periostosis).
4) functional-adaptive periostitis. The last two forms should be called per gostoses.
When identifying periosteal changes, you should pay attention to their localization, extent and nature of the layers. Most often, periostitis is detected in the area of the lower jaw.
According to their shape, linear, layered, fringed, spicule-shaped periostitis (periostosis) and periostitis in the form of a visor are distinguished.
Linear periostitis in the form of a thin strip parallel to the cortical layer of the bone usually occurs in inflammatory diseases, injuries, Ewing's sarcoma and characterizes the initial stages of the disease.
Layered (bulbous) periostitis is radiologically determined in the form of several linear shadows and usually indicates a jerky course of the process (Ewing's sarcoma, chronic osteomyelitis, etc.).
When linear layers are destroyed, fringed (broken) periostitis occurs. In its pattern it resembles pumice and is considered characteristic of syphilis. With tertiary syphilis, the following may be observed: and lace (comb-shaped) periostitis.
Spiculous (needle-shaped) periostitis is considered pathognomonic for malignant tumors. Occurs in osteogenic sarcoma as a result of tumor release into soft tissue.
Changes in X-ray joint space. which is a reflection of articular cartilage and can be in the form of narrowing due to the destruction of cartilage tissue (tuberculosis, purulent arthritis, osteoarthritis), expansion due to an increase in cartilage (osteochondropathia), as well as subluxation. When fluid accumulates in the joint cavity, the X-ray joint space does not widen.
Changes in soft tissues are very diverse and should also be the object of close X-ray examination (tumor, inflammatory, traumatic changes).
Damage to bones and joints.
Objectives of X-ray examination:
1. confirm the diagnosis or reject it,
2. determine the nature and type of fracture,
3. determine the number and degree of displacement of fragments,
4. detect dislocation or subluxation,
5. identify foreign bodies,
6. establish the correctness of medical manipulations,
7. exercise control during the healing process. Signs of a fracture:
1. fracture line (in the form of clearing and compaction) - transverse, longitudinal, oblique, intra-articular, etc. fractures.
2. displacement of fragments: widthwise or lateral, lengthwise or longitudinal (with entry, divergence, wedging of fragments), axially or angularly, along the periphery (spiral-shaped). The displacement is determined by the peripheral fragment.
Features of fractures in children are usually subperiosteal, in the form of a crack and epiphysiolysis. In elderly people, fractures are usually comminuted in nature, with intra-articular localization, with displacement of fragments; healing is slow, often complicated by the development of a pseudarthrosis.
Signs of vertebral body fractures: 1) wedge-shaped deformity with the tip directed anteriorly, compaction of the vertebral body structure, 2) the presence of a shadow of a hematoma around the affected vertebra, 3) posterior displacement of the vertebra.
There are traumatic and pathological fractures (as a result of destruction). Differential diagnosis is often difficult.
Monitoring fracture healing. During the first 7-10 days, the callus is of a connective tissue nature and is not visible on photographs. During this period, there is an expansion of the fracture line and rounding and smoothing of the ends of the broken bones. From 20-21 days, more often after 30-35 days, islands of calcification appear in the callus, clearly visible on radiographs. Complete calcification takes 8 to 24 weeks. Hence, radiographically it is possible to identify: 1) a slowdown in the formation of callus, 2) its excessive development, 3) Normally, the periosteum is not visible on the images. To identify it, compaction (calcification) and detachment are necessary. Periostitis is a response of the periosteum to one or another irritation. In children, radiological signs of periostitis are determined at 7-8 days, in adults - at 12-14 days.
Depending on the cause, they are distinguished: 1) aseptic (in case of injury), 2) infectious (osteomyelitis, tuberculosis, syphilis), 3) irritative-toxic (tumors, suppurative processes) and emerging or formed false joint. In this case, there is no callus, the ends of the fragments are rounded and polished, and the medullary canal is closed.
Restructuring of bone tissue under the influence of excessive mechanical force. Bone is an extremely plastic organ that is rebuilt throughout life, adapting to living conditions. This is a physiological change. When the bone is presented with disproportionately increased demands, pathological restructuring develops. This is a breakdown of the adaptive process, disadaptation. Unlike a fracture, in this case there is repeated traumatization - the total effect of frequently repeated blows and shocks (the metal cannot withstand it either). Special zones of temporary disintegration arise - zones of restructuring (Loozerov zones), zones of enlightenment, which are little known to practical doctors and are often accompanied by diagnostic errors. Most often the skeleton of the lower extremities (foot, thigh, lower leg, pelvic bones) is affected.
The clinical picture distinguishes 4 periods:
1. within 3-5 weeks (after drill training, jumping, working with a jackhammer, etc.) pain, lameness, and pastiness appear over the site of reconstruction. There are no radiological changes during this period.
2. after 6-8 weeks, lameness, severe pain, swelling and local swelling increase. The images show a tender periosteal reaction (usually spindle-shaped).
3. 8-10 weeks. Severe lameness, pain, severe swelling. X-ray - pronounced periostosis of a spindle-shaped form, in the center of which there is a “fracture” line passing through the diameter of the bone and a poorly traced bone marrow canal.
4. recovery period. Lameness disappears, there is no swelling, radiographically the periosteal zone is reduced, the bone structure is restored. Treatment is first rest, then physiotherapy.
Differential diagnosis: osteogenic sacroma, osteomyelitis, osteodosteoma.
A typical example of pathological restructuring is marching foot (Deutschlander's disease, recruits' fracture, overloaded foot). The diaphysis of the 2nd-3rd metatarsal bone is usually affected. The clinic is described above. X-ray semiotics boils down to the appearance of a clearing line (fracture) and muff-like periostitis. The total duration of the disease is 3-4 months. Other types of pathological restructuring.
1. Multiple Loozer zones in the form of triangular notches along the anteromedial surfaces of the tibia (in schoolchildren during the holidays, athletes during excessive training).
2. Lacunar shadows located subperiosteally in the upper third of the tibia.
3. Bands of osteosclerosis.
4. In the form of an edge defect
Changes in bones during vibration occur under the influence of rhythmically operating pneumatic and vibrating tools (miners, miners, asphalt road repairmen, some branches of the metalworking industry, pianists, typists). The frequency and intensity of changes depends on the length of service (10-15 years). The risk group includes persons under 18 years of age and over 40 years of age. Diagnostic methods: rheovasography, thermography, cappilaroscopy, etc.
Main radiological signs:
1. Islands of compaction (enostoses) can occur in all bones of the upper limb. The shape is irregular, the contours are uneven, the structure is uneven.
2. racemose formations are more often found in the bones of the hand (wrist) and look like a clearing 0.2-1.2 cm in size, round in shape with a rim of sclerosis around.
3. osteoporosis.
4. osteolysis of the terminal phalanges of the hand.
5. deforming osteoarthritis.
6. changes in soft tissues in the form of paraosseous calcifications and ossifications.
7. deforming spondylosis and osteochondrosis.
8. osteonecrosis (usually the lunate bone).
CONTRAST METHODS OF RESEARCH IN RADIATION DIAGNOSTICS
Obtaining an X-ray image is associated with uneven absorption of rays in the object. For the latter to receive an image, it must have a different structure. Hence, some objects, such as soft tissues and internal organs, are not visible on regular photographs and require the use of contrast media (CM) for their visualization.
Soon after the discovery of X-rays, ideas for obtaining images of various tissues using CS began to develop. One of the first CSs to achieve success were iodine compounds (1896). Subsequently, buroselectan (1930) for liver research, containing one iodine atom, found widespread use in clinical practice. Uroselektan was the prototype of all CS created later for the study of the urinary system. Soon, uroselectan (1931) appeared, which already contained two iodine molecules, which made it possible to improve image contrast while being well tolerated by the body. In 1953, a triiodinated urography drug appeared, which turned out to be useful for angiography.
In modern visualized diagnostics, CS provide a significant increase in the information content of x-ray examination methods, X-ray CT, MRI and ultrasound diagnostics. All CS have one purpose - to increase the difference between different structures in terms of their ability to absorb or reflect electromagnetic radiation or ultrasound. To fulfill their task, CS must reach a certain concentration in tissues and be harmless, which, unfortunately, is impossible, since they often lead to undesirable consequences. Hence, the search for highly effective and harmless CS continues. The urgency of the problem increases with the advent of new methods (CT, MRI, ultrasound).
Modern requirements for KS: 1) good (sufficient) image contrast, i.e. diagnostic effectiveness, 2) physiological validity (organ specificity, elimination along the route from the body), 3) general availability (cost-effectiveness), 4) harmlessness (absence of irritation, toxic damage and reactions), 5) ease of administration and speed of elimination from the body.
The routes of CS administration are extremely varied: through natural openings (lacrimal puncta, external auditory canal, through the mouth, etc.), through postoperative and pathological openings (fistula tracts, anastomosis, etc.), through the walls of the s/s and lymphatic system (puncture, catheterization, section, etc.), through the walls of pathological cavities (cysts, abscesses, cavities, etc.), through the walls of natural cavities, organs, ducts (puncture, trepanation), introduction into cellular spaces (puncture).
Currently, all CS are divided into:
1. X-ray
2. MRI - contrast agents
3. Ultrasound - contrast agents
4. fluorescent (for mammography).
From a practical point of view, it is advisable to subdivide CS into: 1) traditional X-ray and CT contrast agents, as well as non-traditional ones, in particular, those created on the basis of barium sulfate.
Traditional X-ray contrast agents are divided into: a) negative (air, oxygen, carbon dioxide, etc.), b) positive, absorbing X-rays well. Contrast agents of this group attenuate radiation 50-1000 times compared to soft tissues. Positive CS, in turn, are divided into water-soluble (iodide preparations) and water-insoluble (barium sulfate).
Iodine contrast agents - their tolerance by patients is explained by two factors: 1) osmolarity and 2) chemotoxicity, including ionic exposure. To reduce osmolarity, it was proposed: a) the synthesis of ionic dimeric CS and b) the synthesis of nonionic monomers. For example, ionic dimeric CS were hyperosmolar (2000 m mol/l), while ionic dimers and nonionic monomers already had an osmolarity significantly lower (600-700 m mol/l), and their chemotoxicity also decreased. The nonionic monomer “Omnipak” began to be used in 1982 and its fate has been brilliant. Of the nonionic dimers, Vizipak is the next step in the development of ideal CS. It has isosmolarity, i.e. its osmolarity is equal to blood plasma (290 m mol/l). Nonionic dimers, more than any other CS at this stage of development of science and technology, correspond to the concept of “Ideal contrast agents.”
KS for RKT. In connection with the widespread use of RCT, selective contrast CS began to be developed for various organs and systems, in particular, the kidneys and liver, since modern water-soluble cholecystographic and urographic CS turned out to be insufficient. To a certain extent, Josefanat meets the requirements of the CS for RCT. This CS is selectively concentrated in functional hepatocytes and can be used for tumors and cirrhosis of the liver. Good reviews are also received when using Vizipak, as well as capsulated Iodixanol. All these CT scans are promising for visualizing liver megastases, liver carcinomas, and hemangiomas.
Both ionic and non-ionic (to a lesser extent) can cause reactions and complications. Side effects of iodine-containing CS are a serious problem. According to international statistics, kidney damage by the CS remains one of the main types of iatrogenic renal failure, accounting for about 12% of hospital-acquired acute renal failure. Vascular pain with intravenous administration of the drug, a feeling of heat in the mouth, a bitter taste, chills, redness, nausea, vomiting, abdominal pain, increased heart rate, a feeling of heaviness in the chest - this is not a complete list of the irritating effects of the CS. There may be cardiac and respiratory arrest, and in some cases death occurs. Hence, there are three degrees of severity of adverse reactions and complications:
1) mild reactions (“hot waves”, skin hyperemia, nausea, slight tachycardia). No drug therapy is required;
2) moderate degree (vomiting, rash, collapse). S/s and antiallergic drugs are prescribed;
3) severe reactions (anuria, transverse myelitis, respiratory and cardiac arrest). It is impossible to predict reactions in advance. All proposed prevention methods turned out to be ineffective. Recently, a test “at the tip of a needle” has been proposed. In some cases, premedication is recommended, in particular with prednisone and its derivatives.
Currently, the quality leaders among CS are “Omnipak” and “Ultravist”, which have high local tolerability, overall low toxicity, minimal hemodynamic effects and high image quality. Used for urography, angiography, myelography, gastrointestinal tract examination, etc.
X-ray contrast agents based on barium sulfate. The first reports on the use of an aqueous suspension of barium sulfate as a CS belong to R. Krause (1912). Barium sulfate absorbs X-rays well, mixes easily in various liquids, does not dissolve and does not form various compounds with the secretions of the digestive canal, is easily crushed and allows you to obtain a suspension of the required viscosity, and adheres well to the mucous membrane. For more than 80 years, the method of preparing an aqueous suspension of barium sulfate has been improved. Its main requirements boil down to maximum concentration, fineness and adhesiveness. In this regard, several methods have been proposed for preparing an aqueous suspension of barium sulfate:
1) Boiling (1 kg of barium is dried, sifted, 800 ml of water is added and boiled for 10-15 minutes. Then passed through cheesecloth. This suspension can be stored for 3-4 days);
2) To achieve high dispersion, concentration and viscosity, high-speed mixers are currently widely used;
3) Viscosity and contrast are greatly influenced by various stabilizing additives (gelatin, carboxymethylcellulose, flax seed mucilage, starch, etc.);
4) Use of ultrasonic installations. In this case, the suspension remains homogeneous and practically barium sulfate does not settle for a long time;
5) The use of patented domestic and foreign drugs with various stabilizing substances, astringents, and flavoring additives. Among them, barotrast, mixobar, sulfobar, etc. deserve attention.
The effectiveness of double contrast increases to 100% when using the following composition: barium sulfate - 650 g, sodium citrate - 3.5 g, sorbitol - 10.2 g, antifosmilan -1.2 g, water - 100 g.
A suspension of barium sulfate is harmless. However, if it gets into the abdominal cavity and respiratory tract, toxic reactions are possible, and with stenosis, the development of obstruction.
Non-traditional iodine-containing CSs include magnetic liquids - ferromagnetic suspensions that move in organs and tissues by an external magnetic field. Currently, there are a number of compositions based on ferrites of magnesium, barium, nickel, copper, suspended in a liquid aqueous carrier containing starch, polyvinyl alcohol and other substances with the addition of powdered metal oxides of barium, bismuth and other chemicals. Special devices with a magnetic device have been manufactured that are capable of controlling these CS.
It is believed that ferromagnetic preparations can be used in angiography, bronchography, salpingography, and gastrography. This method has not yet received widespread use in clinical practice.
Recently, among non-traditional contrast agents, biodegradable contrast agents deserve attention. These are drugs based on liposomes (egg lecithin, cholesterol, etc.), deposited selectively in various organs, in particular in the RES cells of the liver and spleen (iopamidol, metrizamide, etc.). Brominated liposomes for CT have been synthesized and excreted by the kidneys. CWs based on perfluorocarbons and other non-traditional chemical elements such as tantalum, tungsten, and molybdenum have been proposed. It is too early to talk about their practical application.
Thus, in modern clinical practice, mainly two classes of X-ray CS are used - iodinated and barium sulfate.
Paramagnetic CS for MRI. Magnevist is currently widely used as a paramagnetic contrast agent for MRI. The latter shortens the spin-lattice relaxation time of excited atomic nuclei, which increases the signal intensity and increases the tissue image contrast. After intravenous administration, it is rapidly distributed in the extracellular space. It is excreted from the body mainly by the kidneys using glomerular filtration.
Application area. The use of Magnevist is indicated in the study of central nervous system organs, in order to detect a tumor, as well as for differential diagnosis in cases of suspected brain tumor, acoustic neuroma, glioma, tumor metastases, etc. With the help of Magnevist, the degree of damage to the brain and spinal cord is reliably determined for multiple sclerosis and monitor the effectiveness of the treatment. Magnevist is used in the diagnosis and differential diagnosis of spinal cord tumors, as well as to identify the prevalence of tumors. “Magnevist” is also used for MRI of the whole body, including examination of the facial skull, neck area, chest and abdominal cavities, mammary glands, pelvic organs, musculoskeletal system.
Fundamentally new CS have now been created and become available for ultrasound diagnostics. “Ekhovist” and “Levovost” deserve attention. They are a suspension of galactose microparticles containing air bubbles. These drugs make it possible, in particular, to diagnose diseases that are accompanied by hemodynamic changes in the right side of the heart.
Currently, thanks to the widespread use of radiopaque, paramagnetic agents and those used in ultrasound examinations, the possibilities for diagnosing diseases of various organs and systems have expanded significantly. Research continues to create new CS that are highly effective and safe.
FUNDAMENTALS OF MEDICAL RADIOLOGY
Today we are witnessing the ever-accelerating progress of medical radiology. Every year, new methods of obtaining images of internal organs and methods of radiation therapy are being introduced into clinical practice.
Medical radiology is one of the most important medical disciplines of the atomic age. It was born at the turn of the 19th and 20th centuries, when people learned that in addition to the familiar world we see, there is a world of extremely small quantities, fantastic speeds and unusual transformations. This is a relatively young science, the date of its birth is precisely indicated thanks to the discoveries of the German scientist W. Roentgen; (November 8, 1895) and the French scientist A. Becquerel (March 1996): discoveries of X-rays and the phenomena of artificial radioactivity. Becquerel's message determined the fate of P. Curie and M. Skladovskaya-Curie (they isolated radium, radon, and polonium). Rosenford's work was of exceptional importance for radiology. By bombarding nitrogen atoms with alpha particles, he obtained isotopes of oxygen atoms, i.e., the transformation of one chemical element into another was proven. This was the “alchemist” of the 20th century, the “crocodile”. He discovered the proton and neutron, which made it possible for our compatriot Ivanenko to create a theory of the structure of the atomic nucleus. In 1930, a cyclotron was built, which allowed I. Curie and F. Joliot-Curie (1934) to obtain a radioactive isotope of phosphorus for the first time. From that moment on, the rapid development of radiology began. Among domestic scientists, it is worth noting the studies of Tarkhanov, London, Kienbeck, Nemenov, who made a significant contribution to clinical radiology.
Medical radiology is a field of medicine that develops the theory and practice of using radiation for medical purposes. It includes two main medical disciplines: radiation diagnostics (diagnostic radiology) and radiation therapy(radiation therapy).
Radiation diagnostics is the science of using radiation to study the structure and functions of normal and pathologically altered human organs and systems for the purpose of preventing and recognizing diseases.
Radiation diagnostics includes x-ray diagnostics, radionuclide diagnostics, ultrasound diagnostics and magnetic resonance imaging. It also includes thermography, microwave thermometry, and magnetic resonance spectrometry. A very important direction in radiation diagnostics is interventional radiology: performing therapeutic interventions under the control of radiation studies.
Today no medical disciplines can do without radiology. Radiation methods are widely used in anatomy, physiology, biochemistry, etc.
Grouping of radiations used in radiology.
All radiation used in medical radiology is divided into two large groups: non-ionizing and ionizing. The former, unlike the latter, when interacting with the environment, do not cause ionization of atoms, i.e., their disintegration into oppositely charged particles - ions. To answer the question about the nature and basic properties of ionizing radiation, we should recall the structure of atoms, since ionizing radiation is intra-atomic (intranuclear) energy.
An atom consists of a nucleus and electron shells. Electron shells are a certain energy level created by electrons rotating around the nucleus. Almost all the energy of an atom lies in its nucleus - it determines the properties of the atom and its weight. The nucleus consists of nucleons - protons and neutrons. The number of protons in an atom is equal to the atomic number chemical element Periodic tables. The sum of protons and neutrons determines the mass number. Chemical elements located at the beginning of the periodic table have an equal number of protons and neutrons in their nucleus. Such nuclei are stable. The elements at the end of the table have nuclei that are overloaded with neutrons. Such nuclei become unstable and decay over time. This phenomenon is called natural radioactivity. All chemical elements located in the periodic table, starting with No. 84 (polonium), are radioactive.
Radioactivity is understood as a phenomenon in nature when an atom of a chemical element decays, turning into an atom of another element with different chemical properties, and at the same time energy is released into the environment in the form of elementary particles and gamma rays.
There are colossal forces of mutual attraction between the nucleons in the nucleus. They are characterized by a large magnitude and act at a very short distance, equal to the diameter of the nucleus. These forces are called nuclear forces, which do not obey electrostatic laws. In cases where there is a predominance of some nucleons over others in the nucleus, the nuclear forces become small, the nucleus is unstable, and decays over time.
All elementary particles and gamma quanta have charge, mass and energy. The unit of mass is taken to be the mass of a proton, and the unit of charge is the charge of an electron.
In turn, elementary particles are divided into charged and uncharged. The energy of elementary particles is expressed in ev, Kev, MeV.
To transform a stable chemical element into a radioactive one, it is necessary to change the proton-neutron equilibrium in the nucleus. To obtain artificially radioactive nucleons (isotopes), three possibilities are usually used:
1. Bombardment of stable isotopes with heavy particles in accelerators (linear accelerators, cyclotrons, synchrophasotrons, etc.).
2.Usage nuclear reactors. In this case, radionuclides are formed as intermediate products of the decay of U-235 (1-131, Cs-137, Sr-90, etc.).
3. Irradiation of stable elements with slow neutrons.
4. Recently, in clinical laboratories, generators have been used to obtain radionuclides (to obtain technetium - molybdenum, indium - charged with tin).
Several types of nuclear transformations are known. The most common are the following:
1. Decay reaction (the resulting substance shifts to the left at the bottom of the cell of the periodic table).
2. Electron decay (where does the electron come from, since it is not in the nucleus? It occurs when a neutron transforms into a proton).
3. Positron decay (in this case, a proton turns into a neutron).
4. Chain reaction - observed during the fission of uranium-235 or plutonium-239 nuclei in the presence of the so-called critical mass. The action of the atomic bomb is based on this principle.
5. Synthesis of light nuclei - thermonuclear reaction. The action of the hydrogen bomb is based on this principle. Fusion of nuclei requires a lot of energy; it is obtained from the explosion of an atomic bomb.
Radioactive substances, both natural and artificial, decay over time. This can be observed by the emanation of radium placed in a sealed glass tube. Gradually the glow of the tube decreases. The decay of radioactive substances follows a certain pattern. The law of radioactive decay states: “The number of decaying atoms of a radioactive substance per unit time is proportional to the number of all atoms,” that is, a certain part of the atoms always decays per unit time. This is the so-called decay constant (X). It characterizes the relative rate of decay. The absolute decay rate is the number of decays per second. The absolute decay rate characterizes the activity of a radioactive substance.
The unit of radionuclide activity in the SI system of units is the becquerel (Bq): 1 Bq = 1 nuclear transformation in 1 s. In practice, the extra-systemic unit curie (Ci) is also used: 1 Ci = 3.7 * 10 10 nuclear transformations in 1 s (37 billion decays). This is a lot of activity. In medical practice, milli and micro Ki are more often used.
To characterize the decay rate, the period during which the activity is halved (T = 1/2) is used. The half-life is determined in s, minutes, hours, years and millennia. The half-life, for example, of Ts-99t is 6 hours, and the half-life of Ra is 1590 years, and U-235 is 5 billion years. The half-life and decay constant are in a certain mathematical relationship: T = 0.693. Theoretically, complete decay of a radioactive substance does not occur, therefore, in practice, ten half-lives are used, i.e., after this period, the radioactive substance has almost completely decayed. The longest half-life of Bi-209 is 200 thousand billion years, the shortest is
To determine the activity of a radioactive substance, radiometers are used: laboratory, medical, radiographs, scanners, gamma cameras. All of them are built on the same principle and consist of a detector (receiving radiation), an electronic unit (computer) and a recording device that allows you to receive information in the form of curves, numbers or a picture.
Detectors are ionization chambers, gas-discharge and scintillation counters, semiconductor crystals or chemical systems.
The characteristic of its absorption in tissues is of decisive importance for assessing the possible biological effects of radiation. The amount of energy absorbed per unit mass of the irradiated substance is called dose, and the same amount per unit time is called radiation dose rate. The SI unit of absorbed dose is the gray (Gy): 1 Gy = 1 J/kg. The absorbed dose is determined by calculation, using tables, or by introducing miniature sensors into the irradiated tissues and body cavities.
A distinction is made between exposure dose and absorbed dose. Absorbed dose is the amount of radiation energy absorbed in a mass of matter. Exposure dose is the dose measured in air. The unit of exposure dose is the roentgen (milliroentgen, microroentgen). X-ray (g) is the amount of radiant energy absorbed in 1 cm 3 of air under certain conditions (at 0 ° C and normal atmospheric pressure), forming an electric charge equal to 1 or forming 2.08x10 9 pairs of ions.
Dosimetry methods:
1. Biological (erythemal dose, epilation dose, etc.).
2. Chemical (methyl orange, diamond).
3. Photochemical.
4. Physical (ionization, scintillation, etc.).
According to their purpose, dosimeters are divided into the following types:
1. To measure radiation in a direct beam (condenser dosimeter).
2. Control and protection dosimeters (DKZ) - for measuring dose rates in the workplace.
3. Personal control dosimeters.
All these tasks are successfully combined in a thermoluminescent dosimeter (“Telda”). It can measure doses ranging from 10 billion to 10 5 rad, i.e. it can be used both for monitoring protection and for measuring individual doses, as well as doses during radiation therapy. In this case, the dosimeter detector can be mounted in a bracelet, ring, chest tag, etc.
RADIONUCLIDE RESEARCH PRINCIPLES, METHODS, CAPABILITIES
With the advent of artificial radionuclides, tempting prospects opened up for the doctor: by introducing radionuclides into the patient’s body, it is possible to monitor their location using radiometric instruments. In a relatively short period of time, radionuclide diagnostics has become an independent medical discipline.
The radionuclide method is a way to study the functional and morphological state of organs and systems using radionuclides and compounds labeled with them, which are called radiopharmaceuticals. These indicators are introduced into the body, and then using various instruments (radiometers) they determine the speed and nature of their movement and removal from organs and tissues. In addition, pieces of tissue, blood, and patient secretions can be used for radiometry. The method is highly sensitive and is carried out in vitro (radioimmunoassay).
Thus, the goal of radionuclide diagnostics is to recognize diseases of various organs and systems using radionuclides and compounds labeled with them. The essence of the method is registration and measurement of radiation from radiopharmaceuticals introduced into the body or radiometry of biological samples using radiometric instruments.
Radionuclides differ from their analogues - stable isotopes - only in their physical properties, that is, they are capable of decaying, producing radiation. The chemical properties are the same, so their introduction into the body does not affect the course of physiological processes.
Currently, 106 chemical elements are known. Of these, 81 have both stable and radioactive isotopes. For the remaining 25 elements, only radioactive isotopes are known. Today, the existence of about 1,700 nuclides has been proven. The number of isotopes of chemical elements ranges from 3 (hydrogen) to 29 (platinum). Of these, 271 nuclides are stable, the rest are radioactive. About 300 radionuclides find or may find practical application in various fields of human activity.
Using radionuclides, you can measure the radioactivity of the body and its parts, study the dynamics of radioactivity, the distribution of radioisotopes, and measure the radioactivity of biological media. Consequently, it is possible to study metabolic processes in the body, the functions of organs and systems, the course of secretory and excretory processes, study the topography of an organ, determine the speed of blood flow, gas exchange, etc.
Radionuclides are widely used not only in medicine, but also in a wide variety of fields of knowledge: archeology and paleontology, metallurgy, agriculture, veterinary medicine, forensic medicine. practice, criminology, etc.
The widespread use of radionuclide methods and their high information content have made radioactive studies an obligatory part of the clinical examination of patients, in particular the brain, kidneys, liver, thyroid gland and other organs.
History of development. As early as 1927, there were attempts to use radium to study the speed of blood flow. However, extensive study of the issue of using radionuclides in widespread practice began in the 40s, when artificial radioactive isotopes were obtained (1934 - Irene and F. Joliot Curie, Frank, Verkhovskaya). P-32 was first used to study metabolism in bone tissue. But until 1950, the introduction of radionuclide diagnostic methods into the clinic was hampered by technical reasons: there were not enough radionuclides, easy-to-use radiometric instruments, or effective research methods. After 1955, research in the field of visualization of internal organs continued intensively in terms of expanding the range of organotropic radiopharmaceuticals and technical re-equipment. The production of a colloidal solution of Au-198.1-131, P-32 was organized. Since 1961, the production of rose bengal-1-131 and hippuran-1-131 began. By 1970, certain traditions had generally developed in the use of specific research techniques (radiometry, radiography, gammatopography, clinical radiometry in vitro. The rapid development of two new techniques began: scintigraphy on cameras and radioimmunological studies in vitro, which today account for 80% of all radionuclide studies in clinic. Currently, the gamma camera can become as widespread as x-ray examination.
Today, a broad program has been outlined to introduce radionuclide research into the practice of medical institutions, which is being successfully implemented. More and more new laboratories are opening, new radiopharmaceuticals and techniques are being introduced. Thus, literally in recent years, tumor-tropic (gallium citrate, labeled bleomycin) and osteotropic radiopharmaceuticals have been created and introduced into clinical practice.
Principles, methods, capabilities
The principles and essence of radionuclide diagnostics are the ability of radionuclides and compounds labeled with them to selectively accumulate in organs and tissues. All radionuclides and radiopharmaceuticals can be divided into 3 groups:
1. Organotropic: a) with directed organotropy (1-131 - thyroid gland, rose bengal-1-131 - liver, etc.); b) with an indirect focus, i.e. temporary concentration in an organ along the path of excretion from the body (urine, saliva, feces, etc.);
2. Tumorotropic: a) specific tumorotropic (gallium citrate, labeled bleomycin); b) nonspecific tumorotropic (1-131 in the study of metastases of thyroid cancer in the bones, rose bengal-1-131 in metastases to the liver, etc.);
3. Determination of tumor markers in blood serum in vitro (alphafetoprotein for liver cancer, carcinoembrysnal antigen - gastrointestinal tumors, choriogonadotropin - chorionepithelioma, etc.).
Advantages of radionuclide diagnostics:
1. Versatility. All organs and systems are subject to the radionuclide diagnostic method;
2. Complexity of research. An example is the study of the thyroid gland (determination of the intrathyroid stage of the iodine cycle, transport-organic, tissue, gammatoporgaphy);
3. Low radiotoxicity (radiation exposure does not exceed the dose received by the patient with one x-ray, and during radioimmunoassay, radiation exposure is completely eliminated, which allows the method to be widely used in pediatric practice;
4. High degree of accuracy of research and the possibility of quantitative recording of the obtained data using a computer.
From the point of view of clinical significance, radionuclide studies are conventionally divided into 4 groups:
1. Fully ensuring the diagnosis (diseases of the thyroid gland, pancreas, metastases of malignant tumors);
2. Determine dysfunction (kidneys, liver);
3. Establish the topographic and anatomical features of the organ (kidneys, liver, thyroid gland, etc.);
4. Get Additional information in a comprehensive study (lungs, cardiovascular, lymphatic systems).
Requirements for radiopharmaceuticals:
1. Harmlessness (no radiotoxicity). Radiotoxicity should be negligible, which depends on the half-life and half-life (physical and biological half-life). The sum of the half-lives and half-lives is the effective half-life. The half-life should be from a few minutes to 30 days. In this regard, radionuclides are divided into: a) long-lived - tens of days (Se-75 - 121 days, Hg-203 - 47 days); b) medium-living - several days (1-131-8 days, Ga-67 - 3.3 days); c) short-lived - several hours (Ts-99t - 6 hours, In-113m - 1.5 hours); d) ultra-short-lived - several minutes (C-11, N-13, O-15 - from 2 to 15 minutes). The latter are used in positron emission tomography (PET).
2. Physiological validity (selectivity of accumulation). However, today, thanks to the achievements of physics, chemistry, biology and technology, it has become possible to include radionuclides in various chemical compounds, the biological properties of which differ sharply from the radionuclide. Thus, technetium can be used in the form of polyphosphate, macro- and microaggregates of albumin, etc.
3. The possibility of recording radiation from a radionuclide, i.e. the energy of gamma quanta and beta particles must be sufficient (from 30 to 140 KeV).
Methods of radionuclide research are divided into: a) research of a living person; b) examination of blood, secretions, excreta and other biological samples.
In vivo methods include:
1. Radiometry (of the whole body or part of it) - determination of the activity of a part of the body or organ. Activity is recorded as numbers. An example is the study of the thyroid gland and its activity.
2. Radiography (gammachronography) - on a radiograph or gamma camera, the dynamics of radioactivity is determined in the form of curves (hepatoradiography, radiorenography).
3. Gammatopography (on a scanner or gamma camera) - the distribution of activity in an organ, which allows one to judge the position, shape, size, and uniformity of drug accumulation.
4. Radioimmune anemia (radiocompetitive) - hormones, enzymes, drugs, etc. are determined in vitro. In this case, the radiopharmaceutical is introduced into a test tube, for example, with the patient’s blood plasma. The method is based on competition between a substance labeled with a radionuclide and its analogue in a test tube for complexing (combining) with a specific antibody. An antigen is a biochemical substance that needs to be determined (hormone, enzyme, drug). For analysis you must have: 1) the substance under study (hormone, enzyme); 2) its labeled analogue: the label is usually 1-125 with a half-life of 60 days or tritium with a half-life of 12 years; 3) a specific perceptive system, which is the subject of “competition” between the desired substance and its labeled analogue (antibody); 4) a separation system that separates bound radioactive substances from unbound ones (activated carbon, ion exchange resins, etc.).
Thus, radio competitive analysis consists of 4 main stages:
1. Mixing the sample, labeled antigen and specific receptor system (antibody).
2. Incubation, i.e., the antigen-antibody reaction to equilibrium at a temperature of 4 °C.
3. Separation of free and bound substances using activated carbon, ion exchange resins, etc.
4. Radiometry.
The results are compared with the reference curve (standard). The more of the starting substance (hormone, drug), the less of the labeled analogue will be captured by the binding system and the larger part of it will remain unbound.
Currently, over 400 compounds of various chemical natures have been developed. The method is an order of magnitude more sensitive than laboratory biochemical studies. Today, radioimmunoassay is widely used in endocrinology (diabetes mellitus diagnosis), oncology (search for cancer markers), in cardiology (myocardial infarction diagnosis), in pediatrics (child development disorders), in obstetrics and gynecology (infertility, fetal development disorders ), in allergology, toxicology, etc.
In industrialized countries, the main emphasis is now on organizing positron emission tomography (PET) centers in large cities, which, in addition to a positron emission tomograph, also includes a small-sized cyclotron for the on-site production of positron-emitting ultrashort-lived radionuclides. Where there are no small-sized cyclotrons, the isotope (F-18 with a half-life of about 2 hours) is obtained from their regional radionuclide production centers or generators (Rb-82, Ga-68, Cu-62) are used.
Currently, radionuclide research methods are also used for preventive purposes to identify hidden diseases. Thus, any headache requires a brain study with pertechnetate-Tc-99t. This type of screening allows us to exclude tumors and areas of hemorrhage. A reduced kidney detected in childhood by scintigraphy should be removed to prevent malignant hypertension. A drop of blood taken from the child's heel allows you to determine the amount of thyroid hormones. If there is a lack of hormones, replacement therapy is carried out, which allows the child to develop normally, keeping up with his peers.
Requirements for radionuclide laboratories:
One laboratory per 200-300 thousand population. It should preferably be placed in therapeutic clinics.
1. It is necessary to place the laboratory in a separate building, built according to a standard design with a security sanitary zone around it. It is forbidden to build children's institutions and catering units on the territory of the latter.
2. The radionuclide laboratory must have a certain set of premises (radiopharmaceutical storage, packaging, generator, washing, treatment room, sanitary inspection room).
3. Special ventilation is provided (five air changes when using radioactive gases), sewerage with a number of settling tanks in which waste of at least ten half-lives is kept.
4. Daily wet cleaning of the premises must be carried out.
This is due to the use of research methods based on high technologies using a wide range of electromagnetic and ultrasonic (US) vibrations.
To date, at least 85% clinical diagnoses is established or specified using various methods radiation research. These methods are successfully used to evaluate the effectiveness of various types of therapeutic and surgical treatment, as well as for dynamic monitoring of the condition of patients during the rehabilitation process.
Radiation diagnostics includes the following set of research methods:
- traditional (standard) x-ray diagnostics;
- X-ray computed tomography (XCT);
- magnetic resonance imaging (MRI);
- Ultrasound, ultrasound diagnostics (USD);
- radionuclide diagnostics;
- thermal imaging (thermography);
- interventional radiology.
Of course, over time, the listed research methods will be supplemented with new methods of radiation diagnostics. It is no coincidence that these sections of radiation diagnostics are presented in the same row. They have a single semiotics, in which the leading sign of the disease is the “shadow image”.
In other words, radiology diagnostics is united by skialogy (skia - shadow, logos - teaching). This is a special branch of scientific knowledge that studies the patterns of shadow image formation and develops rules for determining the structure and function of organs under normal conditions and in the presence of pathology.
The logic of clinical thinking in radiology diagnostics is based on the correct conduct of skiological analysis. It includes a detailed description of the properties of shadows: their position, quantity, size, shape, intensity, structure (pattern), nature of the contours and displacement. The listed characteristics are determined by the four laws of skiology:
- absorption law (determines the intensity of an object’s shadow depending on its atomic composition, density, thickness, as well as the nature of the X-ray radiation itself);
- the law of summation of shadows (describes the conditions for the formation of an image due to the superposition of the shadows of a complex three-dimensional object on a plane);
- projection law (represents the construction of a shadow image, taking into account the fact that the X-ray beam has a divergent nature, and its cross section in the plane of the receiver is always larger than at the level of the object under study);
- law of tangentiality (determines the contour of the resulting image).
The generated X-ray, ultrasound, magnetic resonance (MP) or other image is objective and reflects the true morpho-functional state of the organ being studied. Interpretation of the obtained data by a medical specialist is a stage of subjective cognition, the accuracy of which depends on the level of theoretical training of the researcher, ability for clinical thinking and experience.
Traditional X-ray diagnostics
To perform a standard x-ray examination, three components are required:
- X-ray source (X-ray tube);
- object of study;
- receiver (converter) of radiation.
All research methods differ from each other only in the radiation receiver, which is used: X-ray film, fluorescent screen, semiconductor selenium plate, dosimetric detector.
Today, one or another detector system is the main one as a radiation receiver. Thus, traditional radiography is completely switching to the digital principle of image acquisition.
The main advantages of traditional X-ray diagnostic techniques are their availability in almost all medical institutions, high throughput, relative cheapness, the possibility of multiple studies, including for preventive purposes. The presented methods have the greatest practical significance in pulmonology, osteology, and gastroenterology.
X-ray computed tomography
Three decades have passed since RCT began to be used in clinical practice. It is unlikely that the authors of this method, A. Cormack and G. Hounsfield, who received the Nobel Prize in 1979 for its development, could have imagined how fast the growth of their scientific ideas would be and what a host of questions this invention would raise for clinicians.
Each CT scanner consists of five main functional systems:
- a special stand called a gantry, which contains an X-ray tube, mechanisms for forming a narrow beam of radiation, dosimetric detectors, as well as a system for collecting, converting and transmitting pulses to an electronic computer (computer). In the center of the tripod there is a hole where the patient is placed;
- a patient table that moves the patient inside the gantry;
- Computer storage and data analyzer;
- tomograph control panel;
- display for visual control and image analysis.
Differences in tomograph designs are primarily due to the choice of scanning method. To date, there are five varieties (generations) of X-ray computed tomographs. Today, the main fleet of these devices is represented by devices with a spiral scanning principle.
The principle of operation of an X-ray computed tomograph is that the area of the human body of interest to the doctor is scanned with a narrow beam of X-ray radiation. Special detectors measure the degree of its attenuation by comparing the number of photons entering and leaving the area of the body being studied. The measurement results are transferred to the computer memory, and from them, in accordance with the law of absorption, the radiation attenuation coefficients for each projection are calculated (their number can range from 180 to 360). Currently, absorption coefficients on the Hounsfield scale have been developed for all normal tissues and organs, as well as for a number of pathological substrates. The starting point in this scale is water, the absorption coefficient of which is taken to be zero. The upper limit of the scale (+1000 HU units) corresponds to the absorption of X-rays by the cortical layer of bone, and the lower limit (-1000 HU units) corresponds to air. Below, as an example, are some absorption coefficients for various body tissues and fluids.
Obtaining accurate quantitative information not only about the size and spatial arrangement of organs, but also about the density characteristics of organs and tissues is the most important advantage of RCT over traditional techniques.
When determining indications for the use of RCT, it is necessary to take into account a significant number of different, sometimes mutually exclusive factors, finding a compromise solution in each specific case. Here are some provisions that determine the indications for this type of radiation examination:
- the method is additional, the feasibility of its use depends on the results obtained at the stage of the initial clinical and radiological examination;
- the feasibility of computed tomography (CT) is clarified by comparing its diagnostic capabilities with other, including non-radiation, research methods;
- the choice of RCT is influenced by the cost and availability of this technique;
- It should be taken into account that the use of CT is associated with radiation exposure to the patient.
The diagnostic capabilities of CT will undoubtedly expand as hardware and software improve to enable real-time examinations. Its importance has increased in X-ray surgical interventions as a control tool during surgery. Computed tomographs have been built and are beginning to be used in the clinic, which can be placed in the operating room, intensive care unit or intensive care unit.
Multislice computed tomography (MSCT) is a technique that differs from spiral in that one revolution of the X-ray tube produces not one, but a whole series of sections (4, 16, 32, 64, 256, 320). Diagnostic advantages are the ability to perform tomography of the lungs during one breath-hold in any of the phases of inhalation and exhalation, and therefore the absence of “silent” zones when examining moving objects; availability of constructing various planar and volumetric reconstructions with high resolution; possibility of performing MSCT angiography; performing virtual endoscopic examinations (bronchography, colonoscopy, angioscopy).
Magnetic resonance imaging
MRI is one of the newest methods of radiation diagnostics. It is based on the phenomenon of so-called nuclear magnetic resonance. Its essence lies in the fact that the nuclei of atoms (primarily hydrogen), placed in a magnetic field, absorb energy and then are able to emit it into the external environment in the form of radio waves.
The main components of the MP tomograph are:
- a magnet providing a sufficiently high field induction;
- radio transmitter;
- radio frequency receiving coil;
Today, the following areas of MRI are actively developing:
- MR spectroscopy;
- MR angiography;
- use of special contrast agents (paramagnetic liquids).
Most MRI scanners are configured to record radio signals from hydrogen nuclei. That is why MRI has found its greatest application in recognizing diseases of organs that contain large amounts of water. Conversely, the study of lungs and bones is less informative than, for example, RCT.
The study is not accompanied by radioactive exposure of the patient and personnel. Nothing is known for sure yet about the negative (from a biological point of view) effect of magnetic fields with induction, which is used in modern tomographs. Certain limitations in the use of MRI must be taken into account when choosing a rational algorithm for radiological examination of a patient. These include the effect of “pulling” metal objects into the magnet, which can cause metal implants in the patient’s body to shift. Examples include metal clips on vessels, the displacement of which can lead to bleeding, metal structures in the bones, spine, foreign bodies in eyeball etc. The work of the artificial cardiac pacemaker during MRI may also be disrupted, so examination of such patients is not allowed.
Ultrasound diagnostics
Ultrasonic devices have one distinctive feature. The ultrasonic sensor is both a generator and a receiver of high-frequency oscillations. The sensor is based on piezoelectric crystals. They have two properties: feeding electrical potentials on the crystal leads to its mechanical deformation with the same frequency, and its mechanical compression from reflected waves generates electrical impulses. Depending on the purpose of the study, use Various types sensors that differ in the frequency of the generated ultrasound beam, their shape and purpose (transabdominal, intracavitary, intraoperative, intravascular).
All ultrasound techniques are divided into three groups:
- one-dimensional examination (echography in A-mode and M-mode);
- two-dimensional examination (ultrasound scanning - B-mode);
- dopplerography.
Each of the above methods has its own variants and is used depending on the specific clinical situation. For example, M-mode is especially popular in cardiology. Ultrasound scanning (B-mode) is widely used in the study of parenchymal organs. Without Dopplerography, which makes it possible to determine the speed and direction of fluid flow, a detailed study of the chambers of the heart, large and peripheral vessels is impossible.
Ultrasound has virtually no contraindications, as it is considered harmless to the patient.
Over the past decade, this method has undergone unprecedented progress, and therefore it is advisable to separately highlight new promising directions for the development of this section of radiation diagnostics.
Digital ultrasound involves the use of a digital image converter, which increases the resolution of the devices.
Three-dimensional and volumetric image reconstructions increase diagnostic information due to better spatial anatomical visualization.
The use of contrast agents makes it possible to increase the echogenicity of the structures and organs being studied and achieve better visualization. Such drugs include “Echovist” (gas microbubbles introduced into glucose) and “Echogen” (a liquid from which gas microbubbles are released after injection into the blood).
Color Doppler mapping, in which motionless objects (for example, parenchymal organs) are displayed in shades of a gray scale, and vessels - in a color scale. In this case, the color shade corresponds to the speed and direction of blood flow.
Intravascular ultrasound not only allows one to assess the condition of the vascular wall, but also, if necessary, perform a therapeutic intervention (for example, crush an atherosclerotic plaque).
The method of echocardiography (EchoCG) stands somewhat apart from ultrasound. This is the most widely used method for non-invasive diagnosis of heart disease, based on recording the reflected ultrasound beam from moving anatomical structures and reconstructing the image in real time. There are one-dimensional EchoCG (M-mode), two-dimensional EchoCG (B-mode), transesophageal study (TE-EchoCG), Doppler EchoCG using color mapping. The algorithm for using these echocardiography technologies makes it possible to obtain sufficient full information about the anatomical structures and function of the heart. It becomes possible to study the walls of the ventricles and atria in various sections, non-invasively assess the presence of zones of contractility disorders, detect valvular regurgitation, study blood flow rates with calculation of cardiac output (CO), the area of the valve opening, as well as a number of other parameters that have important, especially in the study of heart defects.
Radionuclide diagnostics
All radionuclide diagnostic methods are based on the use of so-called radiopharmaceuticals (RPs). They represent a kind of pharmacological compound that has its own “fate”, pharmacokinetics in the body. Moreover, each molecule of this pharmaceutical compound is labeled with a gamma-emitting radionuclide. However, radiopharmaceuticals are not always a chemical substance. It can also be a cell, for example a red blood cell, labeled with a gamma emitter.
There are many radiopharmaceuticals. Hence the variety of methodological approaches in radionuclide diagnostics, when the use of a specific radiopharmaceutical also dictates a specific research methodology. The development of new and improvement of used radiopharmaceuticals is the main direction of development of modern radionuclide diagnostics.
If we consider the classification of radionuclide research techniques from the point of view technical support, then three groups of methods can be distinguished.
Radiometry. The information is presented on the display of the electronic unit in the form of numbers and compared with the conventional norm. Typically, slow physiological and pathophysiological processes in the body are studied in this way (for example, iodine absorption function of the thyroid gland).
Radiography (gamma chronography) is used to study fast processes. For example, the passage of blood with administered radiopharmaceuticals through the chambers of the heart (radiocardiography), excretory function of the kidneys (radiorenography), etc. Information is presented in the form of curves designated as “activity-time” curves.
Gamma tomography is a technique designed to obtain images of organs and systems of the body. Available in four main options:
- Scanning. The scanner allows you to pass line by line over the area under study, perform radiometry at each point and apply information to paper in the form of strokes of different colors and frequencies. The result is a static image of the organ.
- Scintigraphy. A high-speed gamma camera allows you to monitor in dynamics almost all processes of the passage and accumulation of radiopharmaceuticals in the body. The gamma camera can receive information very quickly (with a frequency of up to 3 frames per 1 s), so dynamic observation becomes possible. For example, examination of blood vessels (angioscintigraphy).
- Single photon emission computed tomography. Rotation of the detector unit around the object makes it possible to obtain sections of the organ under study, which significantly increases the resolution of gamma tomography.
- Positron emission tomography. The youngest method is based on the use of radiopharmaceuticals labeled with positron-emitting radionuclides. When they are introduced into the body, positrons interact with nearby electrons (annihilation), as a result of which two gamma quanta are “born”, scattering oppositely at an angle of 180°. This radiation is recorded by tomographs on the principle of “coincidence” with very precise topical coordinates.
What is new in the development of radionuclide diagnostics is the emergence of combined hardware systems. Nowadays, a combined positron emission and computed tomography (PET/CT) scanner is beginning to be actively used in clinical practice. In this case, both isotope study and CT are performed in one procedure. Simultaneous acquisition of accurate structural and anatomical information (using CT) and functional information (using PET) significantly expands diagnostic capabilities, primarily in oncology, cardiology, neurology and neurosurgery.
A special place in radionuclide diagnostics is occupied by the method of radiocompetitive analysis (in vitro radionuclide diagnostics). One of the promising directions of the radionuclide diagnostic method is the search in the human body for so-called tumor markers for early diagnosis in oncology.
Thermography
The thermography technique is based on recording the natural thermal radiation of the human body with special thermal imaging detectors. The most common is remote infrared thermography, although thermography techniques have now been developed not only in the infrared, but also in the millimeter (mm) and decimeter (dm) wavelength ranges.
The main disadvantage of the method is its low specificity in relation to various diseases.
Interventional radiology
The modern development of radiation diagnostic techniques has made it possible to use them not only for recognizing diseases, but also for performing (without interrupting the study) the necessary medical manipulations. These methods are also called minimally invasive therapy or minimally invasive surgery.
The main areas of interventional radiology are:
- X-ray endovascular surgery. Modern angiographic complexes are high-tech and allow a medical specialist to super-selectively reach any vascular area. Interventions such as balloon angioplasty, thrombectomy, vascular embolization (for bleeding, tumors), long-term regional infusion, etc. become possible.
- Extravasal (extravascular) interventions. Under the control of X-ray television, computed tomography, ultrasound, it became possible to drain abscesses and cysts in various organs, carry out endobronchial, endobiliary, endourinary and other interventions.
- Radiation-guided aspiration biopsy. It is used to establish the histological nature of intrathoracic, abdominal, and soft tissue formations in patients.
Literature.
Test questions.
Magnetic resonance imaging (MRI).
X-ray computed tomography (CT).
Ultrasonography(ultrasound).
Radionuclide diagnostics (RND).
X-ray diagnostics.
Part I. GENERAL ISSUES IN RADIATION DIAGNOSTICS.
Chapter 1.
Radiation diagnostic methods.
Radiation diagnostics deals with the use of various types of penetrating radiation, both ionization and non-ionization, in order to identify diseases of internal organs.
Radiation diagnostics currently reaches 100% of use in clinical methods examination of patients and consists of the following sections: X-ray diagnostics (RDI), radionuclide diagnostics (RND), ultrasound diagnostics (USD), computed tomography (CT), magnetic resonance imaging (MRI). The order in which the methods are listed determines the chronological sequence of the introduction of each of them into medical practice. The share of radiological diagnostic methods according to WHO today is: 50% ultrasound, 43% X-ray (radiography of the lungs, bones, breast - 40%, X-ray examination of the gastrointestinal tract - 3%), CT - 3%, MRI -2 %, RND-1-2%, DSA (digital subtraction arteriography) – 0.3%.
1.1. Principle of X-ray diagnostics consists of visualizing internal organs using x-ray radiation directed at the object of study, which has a high penetrating ability, with its subsequent registration after leaving the object by some x-ray receiver, with the help of which a shadow image of the organ under study is directly or indirectly obtained.
1.2. X-rays are a type of electromagnetic waves (these include radio waves, infrared rays, visible light, ultraviolet rays, gamma rays, etc.). In the spectrum of electromagnetic waves they are located between ultraviolet and gamma rays, having a wavelength from 20 to 0.03 angstroms (2-0.003 nm, Fig. 1). For X-ray diagnostics, the shortest wavelength X-rays (so-called hard radiation) with a length of 0.03 to 1.5 angstroms (0.003-0.15 nm) are used. Possessing all the properties of electromagnetic vibrations - propagation at the speed of light

(300,000 km/sec), straightness of propagation, interference and diffraction, luminescent and photochemical action, X-ray radiation also has distinctive properties, which led to their use in medical practice: it is penetrating ability - X-ray diagnostics is based on this property, and biological action is a component the essence of x-ray therapy.. Penetrating ability, in addition to wavelength (“hardness”), depends on the atomic composition, specific gravity and thickness of the object under study (inverse relationship).
1.3. X-ray tube(Fig. 2) is a glass vacuum cylinder in which two electrodes are built in: a cathode in the form of a tungsten spiral and an anode in the form of a disk, which rotates at a speed of 3000 rpm when the tube is operating. A voltage of up to 15 V is applied to the cathode, while the spiral heats up and emits electrons that rotate around it, forming a cloud of electrons. Then voltage is applied to both electrodes (from 40 to 120 kV), the circuit is closed and electrons fly to the anode at speeds of up to 30,000 km/sec, bombarding it. In this case, the kinetic energy of flying electrons is converted into two types of new energy - the energy of X-rays (up to 1.5%) and the energy of infrared, thermal rays (98-99%).
 The resulting X-rays consist of two fractions: bremsstrahlung and characteristic. Bremsstrahlung rays are formed as a result of the collision of electrons flying from the cathode with electrons of the outer orbits of the atoms of the anode, causing them to move to inner orbits, which results in the release of energy in the form of quanta of bremsstrahlung X-ray radiation of low hardness. The characteristic fraction is obtained due to the penetration of electrons into the nuclei of the anode atoms, which results in the knocking out of characteristic radiation quanta.
The resulting X-rays consist of two fractions: bremsstrahlung and characteristic. Bremsstrahlung rays are formed as a result of the collision of electrons flying from the cathode with electrons of the outer orbits of the atoms of the anode, causing them to move to inner orbits, which results in the release of energy in the form of quanta of bremsstrahlung X-ray radiation of low hardness. The characteristic fraction is obtained due to the penetration of electrons into the nuclei of the anode atoms, which results in the knocking out of characteristic radiation quanta.
It is this fraction that is mainly used for diagnostic purposes, since the rays of this fraction are harder, that is, they have greater penetrating power. The proportion of this fraction is increased by applying a higher voltage to the X-ray tube.
1.4. X-ray diagnostic machine or, as it is now commonly referred to, the X-ray diagnostic complex (RDC) consists of the following main blocks:
a) X-ray emitter,
b) X-ray feeding device,
c) devices for generating x-rays,
d) tripod(s),
e) X-ray receiver(s).
X-ray emitter consists of an X-ray tube and a cooling system, which is necessary to absorb thermal energy generated in large quantities during operation of the tube (otherwise the anode will quickly collapse). Cooling systems use transformer oil, air cooling with fans, or a combination of both.
The next block of the RDK is x-ray feeding device, which includes a low-voltage transformer (to heat up the cathode spiral, a voltage of 10-15 volts is required), a high-voltage transformer (for the tube itself, a voltage of 40 to 120 kV is required), rectifiers (for efficient operation of the tube, direct current is required) and a control panel.
Radiation shaping devices consist of an aluminum filter that absorbs the “soft” fraction of X-rays, making it more uniform in hardness; a diaphragm, which forms an X-ray beam according to the size of the organ being removed; screening grid, which cuts off scattered rays arising in the patient’s body in order to improve image sharpness.
Tripod(s)) serve to position the patient, and in some cases, the X-ray tube. There are stands intended only for radiography - radiographic, and universal, on which both radiography and fluoroscopy can be carried out. , three, which is determined by the configuration of the RDK depending on the profile of the healthcare facility.
X-ray receiver(s). As receivers, a fluorescent screen is used for transmission, X-ray film (for radiography), intensifying screens (the film in the cassette is located between two intensifying screens), storage screens (for luminescent s. computer radiography), an X-ray image intensifier - URI, detectors (when using digital technologies).
1.5. X-ray imaging technologies Currently there are three versions:
direct analog,
indirect analog,
digital (digital).
With direct analogue technology(Fig. 3) X-rays coming from the X-ray tube and passing through the studied area of the body are unevenly attenuated, since along the X-ray beam there are tissues and organs with different atomic
 and specific gravity and different thicknesses. When they fall on the simplest X-ray receivers - X-ray film or a fluorescent screen, they form a summation shadow image of all tissues and organs that fall into the zone of passage of the rays. This image is studied (interpreted) either directly on a fluorescent screen or on X-ray film after its chemical processing. Classical (traditional) X-ray diagnostic methods are based on this technology:
and specific gravity and different thicknesses. When they fall on the simplest X-ray receivers - X-ray film or a fluorescent screen, they form a summation shadow image of all tissues and organs that fall into the zone of passage of the rays. This image is studied (interpreted) either directly on a fluorescent screen or on X-ray film after its chemical processing. Classical (traditional) X-ray diagnostic methods are based on this technology:
fluoroscopy (fluoroscopy abroad), radiography, linear tomography, fluorography.
X-ray currently used mainly in the study of the gastrointestinal tract. Its advantages are a) the study of the functional characteristics of the organ under study in real time and b) a complete study of its topographic characteristics, since the patient can be placed in different projections by rotating him behind the screen. Significant disadvantages of fluoroscopy are the high radiation exposure to the patient and low resolution, so it is always combined with radiography.
Radiography is the main, leading method of x-ray diagnostics. Its advantages are: a) high resolution of the x-ray image (pathological foci 1-2 mm in size can be detected on the x-ray), b) minimal radiation exposure, since the exposures when receiving the image are mainly tenths and hundredths of a second, c ) objectivity of obtaining information, since the radiograph can be analyzed by other, more qualified specialists, d) the ability to study the dynamics of the pathological process from radiographs taken in different periods illness, e) an x-ray is a legal document. The disadvantages of an x-ray include incomplete topographical and functional characteristics of the organ being studied.
Typically, radiography uses two projections, which are called standard: direct (front and back) and lateral (right and left). The projection is determined by the proximity of the film cassette to the surface of the body. For example, if the cassette for a chest x-ray is located at the anterior surface of the body (in this case, the x-ray tube will be located at the back), then such a projection will be called direct anterior; if the cassette is located along the posterior surface of the body, a direct posterior projection is obtained. In addition to standard projections, there are additional (atypical) projections that are used in cases where in standard projections, due to anatomical, topographical and skialological features, we cannot obtain a complete picture of the anatomical characteristics of the organ under study. These are oblique projections (intermediate between direct and lateral), axial (in this case, the X-ray beam is directed along the axis of the body or organ under study), tangential (in this case, the X-ray beam is directed tangentially to the surface of the organ being photographed). Thus, in oblique projections, the hands, feet, sacroiliac joints, stomach, duodenum etc., in the axial - the occipital bone, calcaneus, mammary gland, pelvic organs, etc., in the tangential - nasal bones, zygomatic bone, frontal sinuses, etc.
In addition to projections, during X-ray diagnostics, different positions of the patient are used, which is determined by the research technique or the patient’s condition. The main position is orthoposition– vertical position of the patient with a horizontal direction of x-rays (used for radiography and fluoroscopy of the lungs, stomach, and fluorography). Other positions are trichoposition– horizontal position of the patient with a vertical course of the X-ray beam (used for radiography of bones, intestines, kidneys, when studying patients in serious condition) and lateroposition- horizontal position of the patient with the horizontal direction of the x-rays (used for special research techniques).
Linear tomography(radiography of the organ layer, from tomos - layer) is used to clarify the topography, size and structure of the pathological focus. With this method (Fig. 4), during radiography, the X-ray tube moves over the surface of the organ under study at an angle of 30, 45 or 60 degrees for 2-3 seconds, and at the same time the film cassette moves in the opposite direction. The center of their rotation is the selected layer of the organ at a certain depth from its surface, the depth is