In the book "Eye of Revelation" Colonel Bradford indicates clockwise rotation:
“The First Ritual,” said the colonel, “is quite simple. It is intended to accelerate the movement of the Whirlwinds. As children, we used this in our games. Your actions: stand straight, with your arms extended horizontally along your shoulders. Begin to spin around your axis until you feel slight dizziness. One warning: you must rotate from left to right. In other words, if you place a watch on the floor with the dial facing up, your hands should move in the direction of the hands."
Note that Colonel Bradford defines the "clockwise" direction as the direction in which a person rotates from left to right, regardless of his location on the planet.
Given that Bradford was in the northern hemisphere when he wrote that you need to rotate from left to right (clockwise), some people wonder whether to adapt his instructions and rotate counterclockwise while in the southern hemisphere.
When I ask them: " Why do you think we should change the direction of rotation?"
Their answer is usually along the lines of " Water in the southern hemisphere swirls counterclockwise, while in the northern hemisphere it swirls clockwise.".
However, this concept itself is based on a popular misconception, and therefore the reason for the change in direction of rotation is also not convincing.
Alistair B. Fraser Ph.D., Professor Emeritus of Meteorology, Penn State University, USA, explains in detail:
"Compared to the rotations we see every day (car tires, CDs, sink drains), the Earth's rotation is almost imperceptible - only a revolution per day. Water in a sink rotates in a few seconds, so its rotation speed is ten thousand times higher than that of the Earth. This is not surprising, given that the Coriolis force is several orders of magnitude smaller than any of the forces involved in these everyday examples of rotation. The Coriolis force is so small that it affects the direction of rotation of water no more than the direction of rotation of a compact disk.
The direction of rotation of the water in the sink drain is determined by how it was filled, or what turbulence was created in it during washing. The size of these rotations is small, but compared to the rotation of the Earth, they are simply huge."
It is difficult to describe the Coriolis effect in more detail without resorting to mathematical equations or complex concepts such as angular mechanics. First of all, our frame of reference is: “ What we see depends on where we are" This means that we are standing on a solid surface, when in fact this is not the case - after all, the earth is a rotating ball.
Coriolis effect
In physics Coriolis effect is the obvious deviation of moving objects when viewed from a rotating frame of reference. As an example, consider two children on opposite sides of a rotating carousel throwing a ball to each other (Figure 1). From these children's point of view, the ball's path is bent sideways by the Coriolis effect. From the thrower's perspective, this deflection is directed to the right as the carousel rotates counterclockwise (as viewed from above). Accordingly, when moving clockwise, the deflection is directed to the left.

If you are really interested in a detailed explanation of the Coriolis effect, enter “Coriolis effect” into a search engine and study this issue thoroughly.
Direction of chakra rotation
Peter Kalder did not describe the direction of movement of the vortices (chakras):
“The body has seven centers, which can be called Vortexes. They are a kind of magnetic centers. IN healthy body they rotate at high speed, and when their rotation slows down, this can be called old age, illness or decline. The fastest way to restore youth, health and vitality is to make these vortices spin again at the same speed. There are five simple exercises to achieve this goal. Any one of them is useful on its own, but all five are needed to get the best results. Lamas call them rituals, and I will treat them the same way.” - Peter Kalder, edited by Alina and Mikhail Titov, “The Eye of Revelation”, 2012.
I wonder if Calder deliberately avoided mentioning the counterclockwise direction? According to Barbara Ann Brennan, former research fellow NASA and authority on human energy, healthy chakras should rotate clockwise; and closed, unbalanced ones are counterclockwise.
In her successful book, Hands of Light, she says:
"When the chakras are functioning normally, each of them will be open and will rotate clockwise to absorb the specific energy needed from the global field. Rotating clockwise to receive energy from the Global Energy Field into the chakras is reminiscent of the right hand rule in electromagnetism, which states, what a change magnetic field around a wire will cause a current to flow in that wire.
When the chakras rotate counterclockwise, there is an outflow of energy from the body, causing metabolic disorders. In other words, when the chakra rotates counterclockwise, we do not receive the energy we need, which we perceive as psychological reality. Such a chakra is considered closed to incoming energy."
Possible influences of traditions
(a) Traditional Tibetan "trul-hor" yantra yoga
Chogal Namhai Norbu, one of the great masters of Dzogchen and Tantra, was born in Tibet in 1938. His book " Yantra Yoga: Tibetan Yoga of Movement"Published by the publishing house "Snow Lion".
"Trul-hor" means "magic wheel", says Alejandro Chaul-Reich, a faculty member at the Ligmincha Institute and an assistant professor at the University of Texas Medical School. He says:
"The characteristic trul-khor movements arose as a result of the practice deep meditation adherents of Tibetan yoga. Traditionally practiced in remote Himalayan caves and monasteries, trul-hor movements are now accessible to serious Western students. They are a powerful tool for clearing, balancing and harmonizing the subtle aspects of your energetic dimension."
Ryan Parker specialist in Five Tibetan Rituals, is currently conducting research comparing the Five Rituals and the Trul-Hor. According to Peter Kelder in The Eye of Revelation, the rituals, like the trul-khor, date back about 2,500 years.
In his latest Comparative Table he states:
"The Buddhist 'trul-hor' presupposes the existence energy centers, rotating clockwise. Thrul-chorus is sometimes called a stimulus for the rotation of energy centers. Moreover, they begin to rotate in unison. Although this rotation can be caused in many ways, the rotation of the body is associated in a special way with the stimulation of the centers. Clockwise rotation is considered beneficial and is the suggested direction of rotation in the Buddhist "trul-hor."
(b) Pradakshina

Throughout history, Tibet and India exchanged ancient knowledge, and it is possible - but not proven - that the First Ritual may have been influenced by the practice of Pradakshina.
In Hinduism Pradakshina means the act of worship - walking clockwise around a holy place, temple, shrine. Dakshina means right, so you go to the left, with the spiritual object always on your right.
During Pradakshina, you walk clockwise around a temple, shrine, person, mountain, place or even yourself. Hindu temples even have special passages so that people can perform these movements around them in a clockwise direction.
The purpose of such circular movements– concentrate or purify oneself, or honor the object of worship.
Circling is so common that it is found in the cultures of the Greeks, Romans, Druids and Hindus. This is usually associated with a sacrifice or purification process. The interesting thing is that for all these cultures the direction of movement is always the same - clockwise!
Other interesting facts about clockwise rotation
During one of my classes, a dance teacher told me that children are initially taught to spin in a clockwise direction. Obviously, it's easier for them (although there are exceptions). He said it was well known among dance teachers - If you need to calm children down, make them spin counterclockwise. And so that activate them - let them circle clockwise!
This energetic effect is exactly what people experience when performing Ritual No. 1, as described by Colonel Bradford. It seems to me that if the lamas gave instructions to rotate clockwise, then this is how it should be!
Who practices counterclockwise rotation
However, I am familiar with a certain Marina who rotates counterclockwise due to a life-threatening health condition that she is trying to correct. She is very committed to meeting her body's needs, as you can read below:
"According to Qi Gong and Traditional Chinese Medicine, clockwise movement speeds up life processes by increasing the speed of movement of the chakras to the original. Counterclockwise movement slows down the chakras. Most of those who practice rituals want to speed up chakras that have slowed down due to age, weight and so on, because it is logical that they rotate clockwise. However, one day, during morning prayer I realized that in my case, chakra acceleration will only have Negative consequences, since the chakra affecting my lungs is unable to accelerate! So I started spinning counterclockwise and soon noticed that other rituals became easier to perform!”
To summarize, until documents or teachers are found, all attempts to understand the motives of Ritual No. 1 will only be theoretical. Therefore, you should do what you personally feel is good for you!
The rotations of the heart around the longitudinal axis, conventionally drawn through the apex and base of the heart, are determined by the configuration of the QRS complex in the chest leads, the axes of which are located in the horizontal plane (Fig. 66).
To do this, it is usually necessary to localize the transition zone, as well as evaluate the shape of the QRS complex in lead V 6.
In the normal position of the heart in the horizontal plane (Fig. 56, a), the transition zone, as is known, is most often located in lead V 3. In this lead, R and S waves of equal amplitude are recorded.
In lead V 6, the ventricular complex usually has the shape of qRs. In this case, the q and s waves have a very small amplitude. This, as you remember, is due to the corresponding spatial arrangement of the three moment vectors (0.02 s, 0.04 s and 0.06 s) shown in Fig. 56, a.
TO
Rice. 56. The shape of the ventricular QRS complex in the chest leads when the heart rotates around the longitudinal axis (modification of the diagram by A.Z. Chernov and M.I. Kechker, 1979. explanation in the text.
REMEMBER! Electrocardiographic signs of clockwise rotation of the heart around the longitudinal axis are:
1) QRS complex of the RS form in lead V 6, as well as in standard lead I;
2) possible shift of the transition zone to the left in leads V 4 - V 5.
When the heart rotates around the longitudinal axis counterclockwise (Fig. 56, c), the interventricular septum is perpendicular to the anterior chest wall, so the transition zone can shift to the right to lead V 2. The initial torque vector (0.02 s) turns out to be almost parallel to the axis of lead V 6, and therefore there is some deepening of the Q wave in this lead. The Q wave is now fixed not only in V 5.6, but also in lead V 4 (less often in V 3). On the contrary, the direction of the final torque vector (0.06 s) turns out to be almost perpendicular to the axis of lead V 6, therefore the S wave is not expressed in this lead. The QRS complex in standard lead I (qR) has the same shape.
REMEMBER! Electrocardiographic signs of rotation of the heart around the longitudinal axis counterclockwise are:
1) QRS complex of the qR form in lead V 6, as well as in standard lead I;
2) possible shift of the transition zone to the right to lead V 2.
It should be added that clockwise rotations of the heart around the longitudinal axis are often combined with a vertical position of the electrical axis of the heart or deviation of the heart axis to the right, and counterclockwise rotations are often combined with a horizontal position or deviation of the electrical axis of the heart to the left.
When the heart rotates with its apex forward around its transverse axis, the average QRS vector deviates forward, the initial vector (Q) is directed more to the right and upward than usual (in the F plane). It is located parallel to the frontal plane and therefore clearly projects to the minus axes of all standard leads (I, II and III).
The ECG shows a pronounced wave QI, II, III. The final vector (S) deviates posteriorly and downward, perpendicular to the frontal plane and is not projected to minus on the axis of standard leads, therefore, the S wave is not recorded in leads I, II, III. Thus, when the heart rotates with its apex forward around the transverse axis on the ECG in leads I, II and III record the qR complex.
When the heart rotates with its apex backward around the transverse axis, the average QRS vector deviates backward (in the S plane), the final vector (S) deviates to the right and upward, giving a significant projection to the negative pole of the axes of leads I, II and III. The ECG shows a pronounced wave SI, II, III. The initial vector (Q) is directed downward and forward and therefore is not projected to the negative pole of the axes of standard leads. As a result, there is no Q wave in the ECG in leads I, II and III. The QRSI, II, III complex is represented by the RS type.
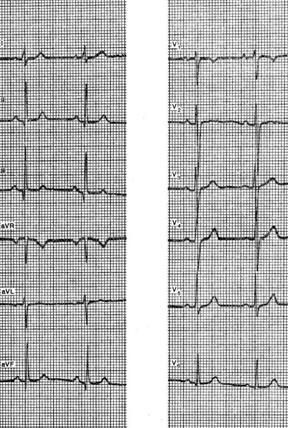
ECG healthy woman D., 30 years old. The sinus rhythm is regular, 67 per minute. P - Q=0.12 sec. P = 0.10 sec. QRS = 0.08 sec. Q - T = 0.38 sec. Ru>RI>Rir AQRS=+52°. Ap=+35°. At=+38°. Complex QRSI,II,III type qR. This shows that the initial vector (Q) is directed to the right and upward more than usual, and is therefore projected to the minus of all standard leads (wave qI, II, III). The final vector (S) deviates posteriorly and downward, perpendicular to the frontal plane and is not projected onto the axes of leads I, II, III (there is no S wave, cw). Such changes in the direction of the initial and final vectors may be due to the rotation of the heart with the apex forward. It should be noted that the QRS transition zone coincides with lead V2, which is right border its normal location. Complex QRSV5V6 type RS, which reflects a simultaneous slight rotation clockwise around the longitudinal axis. The P, T waves and the RS - T segment are normal in all leads.
Conclusion. A variant of a normal ECG (rotation of the heart with the apex forward around the transverse axis and clockwise around the longitudinal axis).
ECG of a healthy man K., 37 years old. Severe sinus bradycardia, 50 per 1 min. Interval P - Q=0.15 sec. P = 0.11 sec. QRS=0.09 sec. Q - T=0.39 sec. RII>RI>RIII. AQRS = +50°. Ar=+65°. At=+50°. QRS angle - T=0°. Complex QRSI,II,III type qR. The Q wave is most pronounced in lead II, where its amplitude is 3 mm and its duration is slightly less than 0.03 sec. ( normal sizes). The described QRS shape is associated with the heart turning its apex forward.
In the chest leads, the QRSV5, V6 complex is also of the qR type, and the RV1 wave is pronounced, but not enlarged (amplitude 5 mm). These QRS changes indicate a counterclockwise rotation of the heart around its longitudinal axis. The transition zone is located normally (between V2 and V3). Rest ECG waves normal. The RS segment - TII,III is elevated by no more than 0.5 mm, which may be normal.
Conclusion. Sinus bradycardia. Turning the heart counterclockwise and with the apex forward (a variant of a normal ECG).
ECG of a healthy woman K., 31 years old. The sinus rhythm is regular, 67 per minute. P - Q=0.16 sec. P=0.09 sec. QRS=0.08 sec. Q - T=0.39 sec. RII>RI>RIII. AQRS=+56°. At=+26°. QRS angle - T=30°. Ar=+35°.
Complex QRSI,II,III type Rs. Pronounced S in leads I, II, III indicates a significant deviation of the final vector (S) to the right and upward. The absence of the QI, II, III wave is associated with the direction of the initial QRS vector down and forward (towards the positive pole of the standard leads). This orientation of the initial and final QRS vectors may be due to the rotation of the heart with its apex backwards around its transverse axis (type SI, SII, SIII ECG). The remaining ECG waves are within normal limits normal characteristics: QRSV6 type qRs. The QRS transition zone between V2 and V3, the RS segment - TV2 is shifted upward by 1 mm. In the remaining leads, RS-T is at the level of the isoelectric line, TIII is slightly negative, TaVF is positive, TV1 is negative, TVJ_V6 is positive, with a slightly larger amplitude in V2V3. The P wave is of normal shape and size.
Conclusion. Variant of normal ECG type SI, SII, SIII (rotation of the heart with the apex backwards around the transverse axis).
A little glitter and colored yarn, a little imagination - and the new toy is ready.
A few colored cocktail straws, glue and a shoebox lid are all you need.
You can play it for real while having fun with your family or friends.
When the heart rotates around its longitudinal axis clockwise (as viewed from the apex), the right ventricle moves forward and upward, and the left- back and down. This position is a variant of the vertical position of the heart axis. In this case, a deep Q wave appears on the ECG in lead III, and occasionally in lead aVF, which can simulate signs of focal changes in the posterior phrenic region of the left ventricle.
At the same time, a pronounced S wave is detected in leads I and aVL (the so-called Q III S I syndrome). There is no q wave in leads I, V 5 and V 6. The transition zone may shift to the left. These changes also occur with acute and chronic enlargement of the right ventricle, which requires appropriate differential diagnosis.
The figure shows an ECG of a healthy 35-year-old woman asthenic build. There are no complaints about dysfunction of the heart and lungs. There is no history of diseases that could cause hypertrophy of the right heart. On physical and x-ray examination pathological changes no heart or lungs were identified.
The ECG shows the vertical position of the atrial and ventricular vectors. Â P = +75°. Â QRS = +80°. Noteworthy are the pronounced q waves along with tall R waves in leads II, III and aVF, as well as S waves in leads I and aVL. Transition zone in V 4 -V 5. The indicated ECG features could provide grounds for determining hypertrophy of the right heart, but the absence of complaints, anamnesis data, and the results of clinical and X-ray examinations allowed us to exclude this assumption and consider the ECG to be a normal variant.
The rotation of the heart around the longitudinal axis counterclockwise (i.e., with the left ventricle forward and upward), as a rule, is combined with deviation of the apex to the left and is a rather rare variant of the horizontal position of the heart. This variant is characterized by a pronounced Q wave in leads I, aVL and left chest along with pronounced S waves in leads III and aVF. Deep Q waves may mimic signs of focal changes in the lateral or anterior wall of the left ventricle. The transition zone with this option is usually shifted to the right.

A typical example of this variant of the norm is the ECG shown in the figure of a 50-year-old patient with a diagnosis of chronic gastritis. This curve shows a pronounced Q wave in leads I and aVL and a deep S wave in lead III.
The likelihood that a physician will diagnose a patient with cor pulmonale depends on the physician's awareness that the patient's existing lung disease may result in pulmonary hypertension. The correct diagnosis is usually made in the presence of obliterating changes in the vessels of the pulmonary circulation, for example, with multiple embolism in the pulmonary trunk. The diagnosis of cor pulmonale is not so obvious in obstructive airway diseases due to the fact that clinical manifestations chronic bronchitis and bronchiolitis may be less pronounced, and clinical indices pulmonary hypertension not very reliable. Of course, the first attack of pulmonary hypertension and cor pulmonale, which developed secondary to the presence of chronic bronchitis, can only be diagnosed retrospectively, that is, after the development of an obvious episode of right ventricular failure. Diagnosis can be particularly difficult if systemic venous congestion and peripheral edema develop insidiously over days or weeks rather than suddenly, as occurs with acute bronchopulmonary infections. IN Lately Much attention is paid to the problem of the gradual development of cor pulmonale and right ventricular failure in patients with alveolar hypoventilation, which is one of the manifestations apnea syndrome in a dream, and not as a consequence of a disease of the lungs themselves.
Differential diagnosis
The presence of cor pulmonale is especially important to establish in elderly patients, when there is a high probability of sclerotic changes in the heart, especially if for many years they have been bothered by a cough with sputum production (chronic bronchitis) and there are obvious clinical manifestations of right ventricular failure. Determination of the blood gas composition is most informative if it is necessary to determine which of the ventricles (right or left) is the root cause of heart disease, since severe arterial hypoxemia, hypercapnia and acidosis rarely occur with left heart failure, unless pulmonary edema develops simultaneously.
Additional confirmation of the diagnosis of pulmonary heart disease is provided by radiographic and ECG signs of enlargement of the right ventricle. Sometimes, if cor pulmonale is suspected, right heart catheterization is required. When this test is performed, it typically reveals pulmonary hypertension, normal left atrial pressure (pulmonary wedge pressure), and classic hemodynamic signs of right ventricular failure.
Enlargement of the right ventricle is characterized by the presence of a cardiac impulse along the left border of the sternum and a fourth heart sound arising in the hypertrophied ventricle. Concomitant pulmonary hypertension is suspected in cases where a cardiac impulse is detected in the second left intercostal space near the sternum, an unusually loud 2nd component of the second heart sound is heard in the same area, and sometimes in the presence of a murmur of pulmonary valve insufficiency. With the development of right ventricular failure, these signs are often accompanied by an additional heart sound, causing the occurrence of a gallop rhythm of the right ventricle. Hydrothorax rarely occurs even after the onset of overt right ventricular failure. Persistent arrhythmias, such as atrial fibrillation or flutter, are also rare, but transient arrhythmias usually occur in cases of severe hypoxia when respiratory alkalosis occurs due to mechanical hyperventilation. The diagnostic value of electrocardiography for cor pulmonale depends on the severity of changes in the lungs and ventilation disorders (Table 191-3). This is most valuable when vascular diseases lungs or damage to interstitial tissue (especially in cases where they are not accompanied by exacerbation of respiratory tract diseases), or with alveolar hypoventilation in normal lungs. On the contrary, with cor pulmonale, which developed secondary to chronic bronchitis and emphysema, increased airiness of the lungs and the episodic nature of pulmonary hypertension and overload of the right ventricle, diagnostic signs Right ventricular hypertrophy is rare. And even if the enlargement of the right ventricle due to chronic bronchitis and emphysema is quite pronounced, as happens during exacerbations during an upper respiratory tract infection, ECG signs may be inconclusive as a result of rotation and displacement of the heart, an increase in the distance between the electrodes and the surface of the heart, and the predominance of dilatation over hypertrophy with enlarged heart. Thus, a reliable diagnosis of right ventricular enlargement can be made in 30% of patients with chronic bronchitis and emphysema, in which autopsy reveals right ventricular hypertrophy, while such a diagnosis can be easily and reliably established in the vast majority of patients with cor pulmonale arising from pulmonary pathology other than chronic bronchitis and emphysema. With this in mind, the following seem to be more reliable criteria for right ventricular hypertrophy in a patient with chronic bronchitis and emphysema: S 1 Q 3 -type, deviation of the electrical axis of the heart more than 110°, S 1 . S2. S 3 type, R/S ratio in lead V6<1,0. Сочетание этих признаков увеличивает их диагностическую ценность.
Table191-3. ECG signs of chronic pulmonary heart disease
1. Chronic obstructive pulmonary diseases (probable, but not diagnostic signs of enlargement of the right ventricle) a) “P-pulmonale” (in leads II, III, aVF) b) deviation of the heart axis to the right more than 110°c) R/S ratio in V6< 1. г) rSR в правых грудных отведениях д) блокада правой ножки пучка Гиса (частичная или полная)
2. Diseases of the pulmonary vessels or interstitial tissue of the lungs; general alveolar hypoventilation (diagnostic signs of right ventricular enlargement) a) classic signs in V1 or V3R (dominant R or R with inverted T tooth in the right precordial leads) b) often combined with the probable criteria indicated above
Among the likely criteria, it is difficult to single out those that reflect an increase in the right ventricle (hypertrophy and dilatation) from anatomical changes and changes in the electrical axis of the heart caused by increased airiness of the lungs. Accordingly, probable criteria as a confirmatory circumstance are more useful than diagnostic ones.
X-ray is of greater diagnostic value when right ventricular enlargement is suspected or for confirming such a condition than for detecting it. Suspicion arises when the patient has signs of a pre-existing predisposing lung disease associated with large central pulmonary arteries and a reduced peripheral arterial network, i.e. signs of pulmonary hypertension. A series of x-ray studies has greater diagnostic value than a single determination of heart size, especially in obstructive airway diseases, when significant changes in heart size can occur during periods between exacerbations of acute respiratory failure and remission.
IN last years To detect pulmonary hypertension, echocardiography began to be used, based on recording the movement of the pulmonary valve. This technique is quite complex, but it is gaining popularity.
Diagnosis and examinations – Chronic cor pulmonale
Page 4 of 5
Laboratory and instrumental diagnostics
IN clinical blood test in patients with chronic pulmonary heart disease, in most cases it is detected erythrocytosis, increase hematocrit and content hemoglobin, which is very typical for chronic arterial hypoxemia. In severe cases, polycythemia develops with an increase in the content of red blood cells, platelets and white blood cells. A decrease in ESR is often associated with an increase in blood viscosity, which is also naturally observed in many patients suffering from respiratory failure.
The described changes in blood tests are naturally not direct evidence of the presence of cor pulmonale, but they usually indicate the severity of pulmonary arterial hypoxemia - the main link in the pathogenesis of chronic cor pulmonale
Electrocardiography
An electrocardiographic study in patients with chronic cor pulmonale reveals signs of right ventricular hypertrophy and right ventricle. The earliest ECG changes are the appearance in leads II, III, aVF (sometimes in V1) of high-amplitude (more than 2.5 mm) with a pointed apex of P waves ( P — pulmonary ) and their duration does not exceed 0.10 s.
Somewhat later, ECG signs of right ventricular hypertrophy begin to appear. Depending on the pressure level in pulmonary artery the magnitude of the muscle mass of the right ventricle and the severity of concomitant pulmonary emphysema in patients with cor pulmonale, three types of ECG changes can be identified:
rSR ‘- mun observed when moderate right ventricular hypertrophy when its mass approaches the mass of the LV myocardium or is slightly less than it (Fig. 1):
- appearance of a QRS complex of the rSR type in lead V1
- increase in the amplitude of the R waves V1,2. S V5, 6, with amplitude RV1 > 7 mm or
RV1 + S v5.6 > 10 5 mm,
transition zone to the left to leads V5, V6 and the appearance in leads V5, V5 of the QRS complex type RS)
III, aVF, Vl, V2,
qR — mun detected when severe right ventricular hypertrophy when its mass is slightly greater than the mass of the LV myocardium. This type of ECG changes is typical (Fig. 2):
- appearance of a QRS complex of the QR or qR type in lead V1
- an increase in the amplitude of teeth RV1 and SV5.6, with the amplitude of RV1 > 7 mm or
RV1 + S V5, 6 > 10 5 mm,
transition zone to the left to leads V5, Vb and the appearance in leads V5, V6 of the QRS complex type RS),
maintained (Vi) for more than 0.03 s,
III, aVF, V1, V2,
Thus, the main differences between these two types of ECG changes in right ventricular hypertrophy lie in the shape of the QRS complex in lead V1.
S — mun ECG changes are often observed in patients with severe emphysema and chronic pulmonary heart disease, when the hypertrophied heart is sharply displaced posteriorly mainly due to emphysema. In this case, the vector of ventricular depolarization is projected onto the negative parts of the axes of the chest leads and limb leads (signs of rotation of the heart around the transverse axis with the apex posteriorly). This explains the significant features of the changes in the QRS complex in these patients (Fig. 3):
- in all chest leads from V1 to Vb, the QRS complex looks like rS or RS with a pronounced S wave
- SISIISIII syndrome is often recorded in the limb leads (a sign of
gate of the heart around the transverse axis with the apex posteriorly)
arrow (shift of the transition zone to the left to leads V5, V6 and the appearance of an RS-type QRS complex in leads V5, V6)
Fig.1. ECG of a patient with chronic cor pulmonale Fig. 2 ECG of a patient with chronic cor pulmonale
(rSR ‘- mun right ventricular hypertrophy) ( qR — mun right ventricular hypertrophy)

Rice. 3. ECG of a patient with chronic cor pulmonale (p-pulmonale and S-type of right ventricular hypertrophy)
It should be noted that for all three types of ECG changes, the diagnosis of pancreatic hypertrophy is indirectly confirmed by the presence of signs of pancreatic hypertrophy P — pulmonary ), detected in leads II, III and aVF.
X-ray examination
X-ray examination allows us to clarify the nature lung damage, and also identify several important radiological signs indicating increase in the size of the right ventricle and availability pulmonary hypertension:
- Bulging of the pulmonary artery trunk in the right anterior oblique projection and less commonly
in direct projection (expansion of the second arch of the left cardiac contour)
With depletion of the vascular pattern in the periphery pulmonary fields due to narrowing
small pulmonary arteries
Echocardiographic examination in patients with chronic pulmonary heart disease is carried out with the aim of
— objective confirmation of the presence of right ventricular hypertrophy(with a thickness of the anterior wall of the right ventricle exceeding 5 mm) and PP(normally, the RA and LA are approximately the same size; dilatation of the RA leads to dominance of its image.)
— assessment of right ventricular systolic function. E This assessment is based primarily on identifying signs of dilatation - during dilatation, the diastolic size of the right ventricle from the parasterial approach along the short axis of the heart usually exceeds 30 mm. The contractility of the right ventricle is most often assessed visually - by the nature and amplitude of movement of the anterior wall of the right ventricle and the IVS. For example, volume overload of the right ventricle in patients with decompensated cor pulmonale is characterized not only by expansion of its cavity, but also by increased pulsation of its walls and paradoxical movements of the IVS: during systole, the IVS bends into the cavity of the right ventricle, and during diastole - towards the LV. Systolic dysfunction right ventricle can be assessed by the degree of collapse of the inferior vena cava during inspiration. Normally, at the height of deep inspiration, the collapse of the inferior vena cava is approximately 50%. Insufficient fall during inspiration indicates an increase in pressure in the RA and in the venous bed. great circle blood circulation
— determination of pressure in the pulmonary artery. Diagnosis of pulmonary arterial hypertension is necessary to assess the severity and prognosis of chronic pulmonary heart disease. For this purpose, Doppler study of the shape of blood flow in the outflow tract is used. right ventricular tract and at the mouth of the pulmonary valve. At normal pressure in the pulmonary artery, the shape of the blood flow approaches dome-shaped and symmetrical, and with pulmonary hypertension it becomes triangular or double-peaked.
quantitation systolic pulmonary artery pressure (PAPP) is possible using continuous wave Doppler study of tricuspid regurgitation, and diastolic pressure - when assessing the maximum speed of diastolic regurgitation of blood from the pulmonary artery in the right ventricle.
Catheterization of the right heart and pulmonary artery
Right heart catheterization is the primary method for directly measuring pulmonary artery pressure. The study is carried out in specialized clinics using a “floating” Swan-Ganz catheter. The catheter is inserted through the internal jugular, external jugular, subclavian or femoral vein into the right atrium, then into the right ventricle and pulmonary artery, measuring the pressure in these chambers of the heart. When the catheter is in one of the branches of the pulmonary artery, the balloon located at the end of the catheter is inflated. Short-term vascular occlusion allows the measurement of pulmonary artery occlusion pressure (pulmonary wedge pressure - PAWP), which approximately corresponds to the pressure in the pulmonary veins, LA and end-diastolic pressure in the LV.
When catheterizing the cavities of the heart and pulmonary artery in patients with chronic pulmonary heart disease, reliable signs pulmonary hypertension - pressure values in the pulmonary artery are more than 25 mm Hg. Art. at rest or more than 35 mm Hg. Art. under load . At the same time, the pulmonary artery wedge pressure (PAWP) remains normal or even reduced - no more than 10-12 mm Hg. Art. Let us recall that for patients with left ventricular failure or heart defects accompanied venous stagnation blood in the lungs, increased pressure in the pulmonary artery is combined with an increase in PAWP to 15-18 mm Hg. Art. and higher.
Function Study external respiration
As shown above, the occurrence of pulmonary hypertension and the formation of chronic pulmonary heart disease in most cases is based on disturbances in the function of external respiration, leading to the development of alveolar hypoxia and pulmonary arterial hypoxemia. Therefore, the severity of the course, prognosis and outcomes of chronic pulmonary heart disease, as well as the choice of the most effective ways Treatment of this disease is largely determined by the nature and severity of pulmonary dysfunction. In this regard, the main IS tasks following the external respiration function (ERF) in patients with cor pulmonale are:
- diagnosis of respiratory dysfunction and objective assessment of the severity of DN;
- differential diagnosis of obstructive and restrictive pulmonary ventilation disorders;
- rationale for pathogenetic therapy of DN;
- assessment of the effectiveness of the treatment.
These problems are solved using a number of instrumental and laboratory research methods: spirometry, spirography, pneumotachography, tests for the diffusion capacity of the lungs, etc.
Compensated and Decompensated cor pulmonale
Compensated cor pulmonale (CP)
It is impossible to identify specific complaints, since they do not exist. The complaints of patients during this period are determined by the underlying disease, as well as varying degrees of respiratory failure.
It is possible to identify a direct clinical sign of right ventricular hypertrophy - increased pulsation detected in the precordial region (in the fourth intercostal space to the left of the sternum). However, with severe emphysema, when the heart is pushed away from the anterior chest wall by emphysematously dilated lungs, it is rarely possible to detect this sign. At the same time, with pulmonary emphysema, epigastric pulsation, caused by increased work of the right ventricle, can be observed in the absence of its hypertrophy as a result of a low standing diaphragm and prolapse of the apex of the heart.
There are no auscultatory findings specific to compensated LS. However, the assumption of pulmonary hypertension becomes more likely when accentuation or clefting is detected II tone over the pulmonary artery. With high levels of pulmonary hypertension, a Graham-Still diastolic murmur may be heard. A loud first sound above the right tricuspid valve compared to the first sound above the apex of the heart is also considered a sign of compensated heart failure. The significance of these auscultatory signs is relative, since they may be absent in patients with severe emphysema.
Stage III of the diagnostic search. Decisive for diagnosing compensated drugs is III stage of diagnostic search, allowing to identify hypertrophy of the right heart.
The value of various instrumental diagnostic methods is not the same.
Indicators of external respiration function reflect the type of breathing disorder (obstructive, restrictive, mixed) and the degree of respiratory failure. However, they cannot be used to differentiate compensated LS from respiratory failure.
X-ray methods allow us to identify early sign LS - bulging of the cone of the pulmonary artery (better determined in the 1st oblique position) and its expansion. A moderate enlargement of the right ventricle may then be noted.
Electrocardiography is the most informative method for diagnosing cor pulmonale. There are convincing "direct" signs ECG hypertrophy right ventricle and right atrium, correlating with the degree of pulmonary hypertension.
If there are two or more “direct” signs on the ECG, the diagnosis of LS is considered reliable.
Of great importance is also the identification of signs of hypertrophy of the right atrium: (P-pulmonale) in II and III , aVF and in the right precordial leads.
Phonocardiography may assist in graphically identifying high amplitude pulmonary components II tone, Graham-Still diastolic murmur - a sign of a high degree of pulmonary hypertension.
Are essential bloodless methods for studying hemodi namiki, based on the results of which one can judge the pressure in the pulmonary artery:
- determination of pressure in the pulmonary artery system by the duration of the isometric relaxation phase of the right ventricle, determined during synchronous recording of ECG, CCG and venogram jugular vein or kinetocardiogram;
- rheopulmonography (the simplest and most accessible method for outpatient settings), which allows one to judge the increase in hypertension in the pulmonary circulation by changes in the apical-basal gradient.
In recent years, new instrumental methods have appeared that are used for early diagnosis of pulmonary heart disease, these include pulsed Dopplercardiography, magnetic resonance imaging and radionuclide ventriculography.
The most reliable way to detect pulmonary hypertension is measuring pressure in the right ventricle and pulmonary artery using catheter(at rest in healthy people, the upper limit of normal systolic pressure in the pulmonary artery is 25-30 mm Hg.) However, this method cannot be recommended as the main one, since its use is possible only in a specialized hospital.
Normal values of systolic pressure in the pulmonary artery at rest do not exclude the diagnosis of LS. It is known that even at minimal physical activity, as well as with exacerbation of bronchopulmonary infection and increased bronchial obstruction, it begins to increase (above 30 mm Hg) inappropriately to the load. With compensated drugs, venous pressure and blood flow velocity remain within normal limits.
Decompensated cor pulmonale
Diagnosis of decompensated HP, if there are undoubted signs of right ventricular failure, is simple. It is difficult to diagnose the initial stages of heart failure in patients with LS, since the early symptom of heart failure - shortness of breath - cannot help in in this case, since it exists in patients with COPD as a sign of respiratory failure long before the development of heart failure.
At the same time, analysis of the dynamics of complaints and main clinical symptoms makes it possible to detect initial signs decompensation of drugs.
At the first stage of the diagnostic search a change in the nature of shortness of breath is revealed: it becomes more constant and less dependent on the weather. The respiratory rate increases, but exhalation does not lengthen (it lengthens only with bronchial obstruction). After coughing, the intensity and duration of shortness of breath increase; it does not decrease after taking bronchodilators. At the same time, pulmonary insufficiency increases, reaching stage III (shortness of breath at rest). Fatigue progresses and ability to work decreases, drowsiness and headaches appear (the result of hypoxia and hypercapnia).
Patients may complain of unspecified pain in the heart area. The origin of these pains is quite complex and is explained by a combination of a number of factors, including metabolic disorders in the myocardium, hemodynamic overload during pulmonary hypertension, and insufficient development of collaterals in the hypertrophied myocardium.
Sometimes pain in the heart can be combined with severe suffocation, agitation, and sharp general cyanosis, which is typical for hypertensive crises in the pulmonary artery system. A sudden rise in pressure in the pulmonary artery is explained by irritation of the baroreceptors of the right atrium, high blood pressure blood in the right ventricle.
Complaints from patients about edema, heaviness in the right hypochondrium, an increase in the size of the abdomen with a corresponding (most often chronic) pulmonary history allow us to suspect decompensated LS.
At stage II of the diagnostic search a symptom of constantly swollen neck veins is revealed, since after joining pulmonary and heart failure, the neck veins swell not only on exhalation, but also on inhalation. Against the background of diffuse cyanosis (a sign of pulmonary failure), acrocyanosis develops, the fingers and hands become cold to the touch. Pastyness of the legs and swelling of the lower extremities are noted.
Constant tachycardia appears, and at rest this symptom is more pronounced than during exercise. A pronounced epigastric pulsation is detected, caused by contractions of the hypertrophied right ventricle. With dilatation of the right ventricle, relative insufficiency of the atrioventricular valve may develop, which causes the appearance of a systolic murmur at the xiphoid process of the sternum. As heart failure develops, heart sounds become muffled. Possible increase in blood pressure due to hypoxia.
One should remember about liver enlargement as early manifestation circulatory failure. The liver may protrude from under the costal margin in patients with emphysema and without signs of heart failure. With the development of heart failure in the initial stages, an increase in predominantly the left lobe of the liver is detected, its palpation is sensitive or painful. As the symptoms of decompensation increase, a positive Plesh symptom is revealed.
Ascites and hydrothorax are observed rarely and, as a rule, when drugs are combined with coronary artery disease or stage II-III hypertension.
III stage of diagnostic search has less significance in the diagnosis of decompensated drugs.
X-ray data allow us to identify a more pronounced enlargement of the right chambers of the heart and pathology of the pulmonary artery:
1) increased vascular pattern of the roots of the lungs with a relatively “light periphery”;
2) extension of the right descending branch pulmonary artery - the most important radiological sign pulmonary hypertension; 3) increased pulsation in the center of the lungs and weakened it in the peripheral parts.
On ECG - progression of symptoms of hypertrophy of the right ventricle and atrium, often blockade of the right leg of the atrioventricular bundle (bundle of His), rhythm disturbances (extrasystoles).
At hemodynamic study detect an increase in pressure in the pulmonary artery (above 45 mm Hg), a slowdown in blood flow, and an increase in venous pressure. The latter in patients with LS indicates the addition of heart failure (this symptom is not early).
IN blood tests Erythrocytosis (reaction to hypoxia), an increase in hematocrit, and an increase in blood viscosity may be detected, and therefore the ESR in such patients may remain normal even with the activity of the inflammatory process in the lungs.
In addition, the rotation of the heart occurs with severe kyphoscoliosis, pathological processes in the lungs, accompanied by a displacement of the heart and large vessels towards the pathological process. As a result of the rotation of the heart, the topography of the edge-forming arches of the heart changes, which in turn affects the configuration of the cardiovascular shadow (Fig. 1).
Rice. 1. Rotation of the heart (the dotted line indicates the contour of the superior vena cava):
1 - turn from right to left (posterior displacement of the left parts of the heart); 2 - rotation of the heart from left to right (the right ventricle is shifted to the right and is edge-forming).
Turning of the heart to the left is observed with severe isolated hypertrophy of the right ventricle (mitral stenosis, cor pulmonale, birth defects hearts with arterial hypertension in the lungs), enlargement of both cavities of the right heart (tricuspid insufficiency), right-sided kyphoscoliosis. The degree of rotation of the heart to the left can reach 10-40°.
The cardiovascular shadow in the direct projection acquires a mitral configuration as a result of lengthening and bulging of the arch of the pulmonary trunk. The left atrial appendage and left ventricle are displaced posteriorly; the latter usually remains edge-forming only at the apex of the heart. With significant rotations, the right ventricle and conus arteriosus become edge-forming along the left contour of the heart.
Turning of the heart to the left is observed with a significant volumetric increase in the left ventricle (aortic stenosis, aortic insufficiency, hypertonic disease), left-sided kyphoscoliosis. P.S. to the right, as a rule, occurs at a smaller angle than to the left (10-15°), and therefore changes in the topography of the heart are less significant. Cardiovascular shadow of the aortic configuration with an emphasized rounding of the enlarged left ventricular arch. The arch of the left atrium lengthens somewhat, the appendage of which is shifted anteriorly. The right atrium and superior vena cava are displaced posteriorly, the right ventricle becomes red-forming and the lower part along the right contour of the heart shadow.
Thus, when the heart turns to the right, both lower edge-forming arches are formed by the ventricles, and the upper ones by the corresponding atria. The vascular bundle is expanded as a result of the reversal of the aorta, so the shadow vascular bundle is a summary image of the ascending and descending aorta.
The rotation of the heart is approximately determined according to fluoroscopy, radiography and x-ray kymography in a direct projection. This sign is more reliably clarified by angiocardiography (the size of the cavity and displacement of the interventricular septum) or an angiogram of the coronary vessels (topography of the coronary vessels). The optimal projections are straight and both anterior oblique.
Determination of heart rotation around the transverse axis
Rotations of the heart around the transverse axis are usually associated with deviation of the apex of the heart forward or backward relative to its normal position. When the heart rotates around the transverse axis tip first the ventricular QRS complex in standard leads takes the form qR I qR II, qR III. On the contrary, when the heart rotates around the transverse axis tip back The QRS complex has the form rs I, rs II, rs III.
Atrial P wave analysis
Atrial P wave analysis includes:
1) measurement of the amplitude of the P wave (normally no more than 2.5 mm);
2) measurement of the duration of the P wave (normally no more than 0.1 s);
3) determination of the polarity of the P wave in leads I, II, III;
4) determination of the shape of the P wave.
In the normal direction of movement of the excitation wave along the atria (from top to bottom), the P waves I, II, III are positive, and in the direction of movement of the excitation wave from bottom to top, they are negative. Split waves with two apexes P I, aVL, V 5, V 6 are characteristic of pronounced hypertrophy of the left atrium, and pointed high-amplitude teeth P II, III, aVF are characteristic of hypertrophy of the right atrium (see below).
Analysis of the ventricular QRS complex includes:
1) assessment tooth ratio Q, R, S in 12 leads, which allows you to determine the rotation of the heart around three axes (see above);
2) measurement amplitude and duration of the tooth Q. A pathological Q wave is characterized by an increase in its duration of more than 0.03 s and amplitude of more than 1/4 of the amplitude of the R wave in the same lead;
3) measurement tooth amplitude R, determination of its possible splitting, as well as the appearance of a second additional tooth R’ (r’);
4) measurement amplitude of the S wave, determination of its possible widening, jaggedness or splitting.
When analyzing the state of the RS-T segment, you must:
1) measure positive (+) or negative (-) connection point deviation j from the isoelectric line;
2) measure the displacement of the RS-T segment at a distance of 0.08 c to the right of connection point j;
3) determine the form of displacement of the RS-T segment: horizontal, oblique-downward or oblique-ascending displacement.
When analyzing the T wave you should:
1) determine the polarity of the T wave,
2) evaluate its shape and
3) measure the amplitude of the T wave.
The Q-T interval is measured from the beginning of the QRS complex (Q or R wave) to the end of the T wave and compared with the proper value calculated using Bazett's formula:
The electrocardiographic report indicates:
1) main pacemaker: sinus or non-sinus rhythm;
2) regularity of heart rhythm: correct or incorrect rhythm;
3) number of heartbeats (HR);
4) position of the electrical axis of the heart;
5) the presence of four ECG syndromes: rhythm and conduction disturbances, hypertrophy of the ventricular and/or atrium myocardium, as well as myocardial damage (ischemia, dystrophy, necrosis, scars, etc.).
Turning the heart backwards - what is it?
When the heart rotates with its apex forward around its transverse axis, the average QRS vector deviates forward, the initial vector (Q) is directed more to the right and upward than usual (in the F plane). It is located parallel to the frontal plane and therefore clearly projects to the minus axes of all standard leads (I, II and III).
The ECG shows a pronounced wave QI, II, III. The final vector (S) deviates posteriorly and downward, perpendicular to the frontal plane and is not projected to minus on the axis of standard leads, therefore, the S wave is not recorded in leads I, II, III. Thus, when the heart rotates with its apex forward around the transverse axis on the ECG in leads I, II and III record the qR complex.
When the heart rotates with its apex backward around the transverse axis, the average QRS vector deviates backward (in the S plane), the final vector (S) deviates to the right and upward, giving a significant projection to the negative pole of the axes of leads I, II and III. The ECG shows a pronounced wave SI, II, III. The initial vector (Q) is directed downward and forward and therefore is not projected to the negative pole of the axes of standard leads. As a result, there is no Q wave in the ECG in leads I, II and III. The QRSI, II, III complex is represented by the RS type.
ECG of a healthy woman D., 30 years old. The sinus rhythm is regular, 67 per minute. P - Q=0.12 sec. P = 0.10 sec. QRS = 0.08 sec. Q - T = 0.38 sec. Ru>RI>Rir AQRS=+52°. Ap=+35°. At=+38°. Complex QRSI,II,III type qR. This shows that the initial vector (Q) is directed to the right and upward more than usual, and is therefore projected to the minus of all standard leads (wave qI, II, III). The final vector (S) deviates posteriorly and downward, perpendicular to the frontal plane and is not projected onto the axes of leads I, II, III (there is no S wave, cw). Such changes in the direction of the initial and final vectors may be due to the rotation of the heart with the apex forward. It should be noted that the QRS transition zone coincides with lead V2, which is the right border of its normal location. Complex QRSV5V6 type RS, which reflects a simultaneous slight rotation clockwise around the longitudinal axis. The P, T waves and the RS - T segment are normal in all leads.
Conclusion. A variant of a normal ECG (rotation of the heart with the apex forward around the transverse axis and clockwise around the longitudinal axis).
ECG of a healthy man K., 37 years old. Severe sinus bradycardia, 50 per 1 min. Interval P - Q=0.15 sec. P = 0.11 sec. QRS=0.09 sec. Q - T=0.39 sec. RII>RI>RIII. AQRS = +50°. Ar=+65°. At=+50°. QRS angle - T=0°. Complex QRSI,II,III type qR. The Q wave is most pronounced in lead II, where its amplitude is 3 mm and its duration is slightly less than 0.03 sec. (normal sizes). The described QRS shape is associated with the heart turning its apex forward.
In the chest leads, the QRSV5, V6 complex is also of the qR type, and the RV1 wave is pronounced, but not enlarged (amplitude 5 mm). These QRS changes indicate a counterclockwise rotation of the heart around its longitudinal axis. The transition zone is located normally (between V2 and V3). The remaining ECG waves are normal. The RS segment - TII,III is elevated by no more than 0.5 mm, which may be normal.
Conclusion. Sinus bradycardia. Turning the heart counterclockwise and with the apex forward (a variant of a normal ECG).
ECG of a healthy woman K., 31 years old. The sinus rhythm is regular, 67 per minute. P - Q=0.16 sec. P=0.09 sec. QRS=0.08 sec. Q - T=0.39 sec. RII>RI>RIII. AQRS=+56°. At=+26°. QRS angle - T=30°. Ar=+35°.
Complex QRSI,II,III type Rs. Pronounced S in leads I, II, III indicates a significant deviation of the final vector (S) to the right and upward. The absence of the QI, II, III wave is associated with the direction of the initial QRS vector down and forward (towards the positive pole of the standard leads). This orientation of the initial and final QRS vectors may be due to the rotation of the heart with its apex backwards around its transverse axis (type SI, SII, SIII ECG). The remaining ECG waves are within the usual normal characteristics: QRSV6 type qRs. The QRS transition zone between V2 and V3, the RS segment - TV2 is shifted upward by 1 mm. In the remaining leads, RS-T is at the level of the isoelectric line, TIII is slightly negative, TaVF is positive, TV1 is negative, TVJ_V6 is positive, with a slightly larger amplitude in V2V3. The P wave is of normal shape and size.
Conclusion. Variant of normal ECG type SI, SII, SIII (rotation of the heart with the apex backwards around the transverse axis).
Training video for determining the EOS (electrical axis of the heart) using an ECG
We welcome your questions and feedback:
Please send materials for posting and wishes to:
By sending material for posting you agree that all rights to it belong to you
When quoting any information, a backlink to MedUniver.com is required
All information provided is subject to mandatory consultation with your attending physician.
The administration reserves the right to delete any information provided by the user
Standards of correct answers
Rice. 4.21. The position of the electrical axis of the heart is horizontal (angle a * +15 *). There is also a rotation of the heart around the longitudinal axis counterclockwise (complex QRS in leads V 5 and V 6 types QR, transition zone (TZ) in lead V 2 .
Rice. 4.22. There is a rotation of the electrical axis of the heart to the right (angle a * +120°), as well as a rotation of the heart around the longitudinal axis clockwise PZ in lead V 6 (complex QRS in leads V 5 (V 6 type AS).
Determination of heart rotation around the transverse axis (apex forward or backward)
Less commonly, the ECG records rotations of the heart around its transverse axis, occurring in the anteroposterior (sagittal) plane (Fig. 4.23). Rotations of the heart around the transverse axis are usually associated with deviation of the apex of the heart forward or backward along
in relation to its usual position, which leads to a violation of the usual spatial arrangement of the three moment vectors of ventricular depolarization in the sagittal and frontal planes. Rotations of the heart around the transverse axis with the apex forward or backward are best recorded in three standard limb leads. Take a look at fig. 4.23. It depicts the familiar six-axis Bailey coordinate system, rotated at a certain angle to the observer, as well as the spatial arrangement of three moment vectors (0.02 s, 0.04 s and 0.06 s).
In most cases, with a normal position of the heart (Fig. 4.23, a), the initial torque vector (0.02 s) is oriented slightly up and to the right, and the final torque vector (0.06 s) is oriented up and to the left or right. Both vectors are spatially located at a certain angle to the frontal plane, with the 0.02 s vector oriented forward, and the 0.06 s vector backward. Both vectors are projected onto the negative parts of the axes of standard leads, as a result of which relatively small amplitude Q and Q waves can be recorded in these leads. S. It should be remembered that the teeth Q And S can be recorded only in one or two of three standard leads: I and II or II and III.
tip first(Fig. 4.23, b) the initial moment vector (0.02 s) shifts even more upward and slightly to the right, and therefore the tooth Q begins to be registered in all three standard leads and becomes more pronounced.
The final moment vector (0.06 s) deflects downwards and backwards, as a result of which it is now located almost perpendicular to the frontal plane. Therefore, its projection on the axes of all standard leads approaches zero, which leads to the disappearance of wave 5 in these leads.
When the heart rotates around the transverse axis tip back(Fig. 4.23, c) the initial moment vector (0.02 s) shifts forward and down so that its orientation in space turns out to be almost perpendicular to the frontal plane. Therefore, the projection of the 0.02 s vector on the axis of standard leads approaches zero, and the teeth themselves Q are not registered.
The final moment vector (0.06 s) shifts even more upward and begins to be projected onto the negative parts of the axes of all three standard limb leads, which leads to the appearance of fairly deep teeth S v S u And Sm.
Thus, to determine the rotation of the heart around the transverse axis, it is necessary to evaluate the configuration of the complex QRS in standard limb leads.
Atrial Wave Analysis R
After determining the rotation of the heart around the anteroposterior, longitudinal and transverse axes, proceed to the analysis of the atrial wave R. Prong analysis R includes: 1) measurement of tooth amplitude R, 2) tooth duration measurement RU 3) determination of tooth polarity R, 4) determination of tooth shape R.
Prong amplitude R is measured from the contour line to the top of the prong, and its duration is from the beginning to the end of the prong, as shown
in Fig. 4.24. Normal tooth amplitude R does not exceed 2.5 mm, and its duration is 0.1 s. Prong polarity R in leads I, II and III is the most important electrocardiographic sign, indicating the direction of movement of the excitation wave along the atria and, consequently, the localization of the source of excitation (pacemaker). As you remember, with normal movement of the excitation wave along the atria from top to bottom and to the left, the teeth are positive, and when the excitation is directed from bottom to top, they are negative. In this latter case, the pacemaker is located in the lower parts of the atria or in the upper part of the AV. node. With excitation emanating from the middle part of the right atrium, the depolarization wave is directed both upward and downward. Average vector R directed to the left, respectively, the tooth R increases, the tooth becomes larger Plv and the P wave ||(becomes negative and shallow.
Determining the tooth shape is of great practical importance R. Split with two apexes, widened tooth R in the left leads (I, aVL, V 5, V 6) is typical for patients with mitral heart defects and left atrial hypertrophy, and pointed high-amplitude teeth R in leads I, III, aVF are observed with hypertrophy of the right atrium in patients with cor pulmonale (for more details, see Chapter 7).
Ventricular complex analysis QRST
turning the heart upside down, what is it?
In chapter Children's health to the question ECG result. What does it mean -sinus rhythm and - turning the heart with the apex backwards. asked by the author Olimp Business the best answer is a variant of the norm
Normally, the rhythm is only sinus. and EOS depends on age and constitution.
Expensive! Heartbeat sets sinus ganglion Therefore, it is customary to evaluate the rhythm that does not have deviations from the norm - sinus. This is all, therefore, the norm. But turning the top back depends on a number of conditions. Peculiarities chest, muscle mass, lung condition, height of the diaphragm, etc. At least this is a variant of the norm and you should not have complexes about this. That's all.
Rotation of the heart by the left ventricle forward how to treat
ECG when the heart rotates around the longitudinal axis. An example of longitudinal rotation of the heart
The rotation of the heart around its longitudinal axis, drawn through the base and apex of the heart, according to Grant, does not exceed 30°. This rotation is viewed from the apex of the heart. The initial (Q) and final (S) vectors are projected onto the negative half of the lead V axis. Therefore, the QRSV6 complex has the shape of qRs (the main part of the QRS loop k + V6). The QRS complex has the same shape in leads I, II, III.
The clockwise rotation of the heart corresponds to the position of the right ventricle somewhat more anteriorly, and the left ventricle somewhat more posteriorly, than the normal position of these chambers of the heart. In this case, the interventricular septum is located almost parallel to the frontal plane, and the initial QRS vector, reflecting the electromotive force (EMF) of the interventricular septum, is oriented almost perpendicular to the frontal plane and to the axes of leads I, V5 and V6. It also tilts slightly up and to the left. Thus, when the heart is rotated clockwise around the longitudinal axis, the RS complex is recorded in all chest leads, and the RSI and QRIII complexes are recorded in standard leads.
ECG of a healthy man M, 34 years old. The rhythm is sinus, regular; heart rate - 78 per 1 min. (R-R = 0.77ceK.). Interval P - Q = 0.14 sec. P=0.09 sec. QRS=0.07 sec. (QIII=0.025 sec.), d -T= 0.34 sec. RIII RII RI SOI. AQRS=+76°. AT=+20°. AP=+43°. ZQRS - T = 56°. The wave PI-III, V2-V6, aVL, aVF is positive, not higher than 2 mm (lead II). The PV1 wave is biphasic +-) with a larger positive phase. Complex QRSr type RS, QRSIII type QR (Q pronounced, but not extended). Complex QRSV| _„ type rS. QRSV4V6 type RS or Rs. Transition zone of the QRS complex in lead V4 (normal). The RS segment - TV1 _ V3 is shifted upward by no more than 1 mm; in the remaining leads it is at the level of the isoelectric line.
The TI wave is negative. shallow. The TaVF wave is positive. TV1 is smoothed. TV2-V6 is positive, low and increases slightly towards leads V3, V4.
Vector analysis. The absence of QIV6 (type RSI, V6) indicates the orientation of the initial QRS vector forward and to the left. This orientation may be associated with the location of the interventricular septum parallel to the chest wall, which is observed when the heart is rotated clockwise around its longitudinal axis. The normal location of the QRS transition zone shows that in this case the hourly turn is one of the options for a normal ECG. A weakly negative TIII wave with a positive TaVF can also be regarded as normal.
Conclusion. Variant of a normal ECG. Vertical position of the electrical axis of the heart with clockwise rotation around the longitudinal axis.
The interventricular septum is almost perpendicular to the frontal plane. The initial QRS vector is oriented to the right and slightly downward, which determines the presence of a pronounced QI, V5V6 wave. In these leads there is no S wave (QRI, V5, V6 shape, since the base of the ventricles occupies a more posterior left position and the final vector is oriented back and to the left.
ECG of a healthy woman Z. 36 years old. Sinus (respiratory) arrhythmia. The number of contractions is 60 - 75 per minute. P-Q interval=0.12 sec. P=0.08 sec. QRS=0.07 sec. Q-T=0.35 sec. R, R1 R1II. AQRS=+44°. At=+30°. QRS angle - T=14°. Ar = +56°. Complex QRS1,V5,V6 type qR. QRSIII type rR's. The RV1 tooth is slightly enlarged (6.5 mm), but RV1 is SV1, and RV2 is SV2.
The described changes in the QRS complex are associated with a rotation of the initial vector to the right and the final vectors to the left, up and back. This position of the vectors is due to the rotation of the heart counterclockwise around the longitudinal axis.
Other teeth and ECG segments without deviation from the norm. Rp tooth (1.8 mm) P1 Rpg Vector P is directed downward, to the left along the axis of lead II. The average QRS vector in the horizontal plane (chest leads) is parallel to the axis of lead V4 (highest R in lead V4). TIII is smoothed, TaVF is positive.
Conclusion. A variant of a normal ECG (rotation of the heart around the longitudinal axis counterclockwise).
The ECG analysis protocol contains information about rotations around the longitudinal (as well as transverse) axis of the heart along ECG data noted in the description. It is not advisable to include them in the ECG conclusion, since they either constitute a variant of the norm, or are a symptom of ventricular hypertrophy, which should be written about in the conclusion.
When assessing the ECG, rotations of the heart around the longitudinal axis, passing from the base to its apex, are also distinguished. Rotation of the right ventricle forward shifts the transition zone to the left, and the S waves in leads V 3 deepen. V4. V5. V 6. the QS complex can be recorded in lead V 1. This rotation is accompanied by a more vertical position of the electrical axis, which causes the appearance of qR I and S III.
Anterior rotation of the left ventricle shifts the transition zone to the right, which causes enlargement of the R waves in leads V 3 . V 2. V 1 disappearance of S waves in the left precordial leads. This rotation is accompanied by a more horizontal arrangement of the electrical axis and registration of qR I and S III in the limb leads.
The third variant of heart rotation is associated with its rotation around the transverse axis and is designated as rotation of the apex of the heart forward or backward.
The forward rotation of the apex of the heart is determined by the registration of q waves in standard leads and lead aVF. which is associated with the exit of the depolarization vector of the interventricular septum into the frontal plane and its orientation upward and to the right.
Posterior rotation of the apex of the heart is determined by the appearance of S waves in standard leads and lead aVF. which is associated with the release of the depolarization vector of the posterior basal sections into the frontal plane and its orientation upward and to the right. The spatial arrangement of the vectors of the initial and final forces of ventricular depolarization has the opposite direction, and their simultaneous registration in the frontal plane is impossible. In three (or four) Q syndrome, there are no S waves in these leads. With three (or four) S syndrome, registration of q waves in the same leads becomes impossible.
The combination of the above rotations and deviations of the electrical axis of the heart makes it possible to determine the electrical position of the heart as normal, vertical and semi-vertical, horizontal and semi-horizontal. It should be noted that determining the electrical position of the heart is of more historical than practical interest, while determining the direction of the electrical axis of the heart makes possible diagnostics intraventricular conduction disorders and indirectly determines the diagnosis of other pathological ECG changes.
Are you interested in holding children's parties in Ufa? Our agency will help make any holiday magical and unforgettable for your child.
Electrocardiogram when the heart rotates around the longitudinal axis
When the heart rotates clockwise around its longitudinal axis (as viewed from the apex), the right ventricle moves forward and upward, and the left ventricle moves backward and downward. This position is a variant of the vertical position of the heart axis. In this case, a deep Q wave appears on the ECG in lead III, and occasionally in lead aVF, which can simulate signs of focal changes in the posterior phrenic region of the left ventricle.
At the same time, a pronounced S wave is detected in leads I and aVL (the so-called Q III S I syndrome). There is no q wave in leads I, V 5 and V 6. The transition zone may shift to the left. These changes also occur with acute and chronic enlargement of the right ventricle, which requires appropriate differential diagnosis.
The figure shows an ECG of a healthy 35-year-old woman with an asthenic build. There are no complaints about dysfunction of the heart and lungs. There is no history of diseases that could cause hypertrophy of the right heart. Physical and x-ray examination revealed no pathological changes in the heart and lungs.
The ECG shows the vertical position of the atrial and ventricular vectors. Â P = +75 . Â QRS = +80. Noteworthy are the pronounced q waves along with tall R waves in leads II, III and aVF, as well as S waves in leads I and aVL. Transition zone in V 4 -V 5. The indicated ECG features could provide grounds for determining hypertrophy of the right heart, but the absence of complaints, anamnesis data, and the results of clinical and X-ray examinations allowed us to exclude this assumption and consider the ECG to be a normal variant.
The rotation of the heart around the longitudinal axis counterclockwise (i.e., with the left ventricle forward and upward), as a rule, is combined with deviation of the apex to the left and is a rather rare variant of the horizontal position of the heart. This variant is characterized by a pronounced Q wave in leads I, aVL and left chest along with pronounced S waves in leads III and aVF. Deep Q waves may mimic signs of focal changes in the lateral or anterior wall of the left ventricle. The transition zone with this option is usually shifted to the right.
A typical example of this variant of the norm is the ECG shown in the figure of a 50-year-old patient with a diagnosis of chronic gastritis. This curve shows a pronounced Q wave in leads I and aVL and a deep S wave in lead III.
Practical electrocardiography, V.L. Doshchitsin
Normal ECG with horizontal position the electrical axis of the heart must be distinguished from signs of left ventricular hypertrophy. When the electrical axis of the heart is vertical, the R wave has a maximum amplitude in leads aVF, II and III; in leads aVL and I, a pronounced S wave is recorded, which is also possible in the left chest leads. ÂQRS = + 70 – +90. Such#8230;
Posterior rotation of the heart is accompanied by the appearance of a deep S1 wave in leads I, II and III, as well as in lead aVF. A pronounced S wave may also be observed in all chest leads with a shift of the transition zone to the left. This variant of a normal ECG requires differential diagnosis with one of the ECG variants for right ventricular hypertrophy (S-type). The picture shows#8230;
The syndrome of premature, or early, repolarization refers to a relatively rare variants normal ECG. The main symptom of this syndrome is ST segment elevation, which has a peculiar shape of a convex downward arc and begins from a highly located J point on the descending knee of the R wave or on the terminal part of the S wave. Notch at the point of transition of the QRS complex to the descending segment ST#8230;
Peculiar ECG changes are observed in persons with dextrocardia. They are characterized by the opposite direction of the main teeth compared to the usual one. Thus, in lead I, negative P and T waves are detected, the main wave of the QRS complex is negative, and a QS type complex is often recorded. Deep Q waves may be observed in the precordial leads, which may give rise to erroneous diagnosis of large-focal changes #8230;
A variant of the norm may be an ECG with shallow negative T waves in leads V1-V3, in young people under 25 years of age (rarely older) in the absence of dynamics in them compared to previously recorded ECGs. These T waves are known as juvenile waves. Sometimes in healthy people on the ECG in leads V2 #8212; V4 is marked by tall T waves, which#8230;
Electrocardiogram when the heart rotates around the transverse axis
Posterior rotation of the heart is accompanied by the appearance of a deep S1 wave in leads I, II and III, as well as in lead aVF. A pronounced S wave may also be observed in all chest leads with a shift of the transition zone to the left. This variant of a normal ECG requires differential diagnosis with one of the ECG variants for right ventricular hypertrophy (S-type).
The figure shows an ECG of a healthy 16-year-old boy. Physical and x-ray examination revealed no signs of pathology. The ECG showed a pronounced S wave in leads I, II, III, aVF, V 1 – V 6, and a displacement of the transition zone to V 5. The Q wave and T wave inversion in lead aVL were also detected, which disappeared when recording the ECG during expiration.
When the heart turns its apex forward in leads I, II, III and aVF, a pronounced Q wave is recorded. The ventricular complex in these leads has a qR shape, and in some cases the depth of the Q wave can exceed 1/4 of the height of the R wave. Often this position of the axis is combined with turning the heart around its longitudinal axis counterclockwise. In such cases, a pronounced Q wave is also detected in the left chest leads.
The figure shows an ECG of a healthy 28-year-old man who had no anamnestic indications of cardiac pathology and its clinical signs. In leads I, II, III, aVF, V 3 – V 6, a pronounced Q wave is recorded, the depth of which does not exceed 1/4 of the amplitude of the R wave. These changes reflect the rotation of the heart with the apex forward and around the longitudinal axis counterclockwise.
“Practical electrocardiography”, V.L. Doshchitsin
In some cases, variants of a normal ECG associated with different position axis of the heart are mistakenly interpreted as a manifestation of one or another pathology. In this regard, we will first consider the “positional” variants of a normal ECG. As mentioned above, healthy people may have a normal, horizontal or vertical position of the electrical axis of the heart, which depends on body type, age and...
A normal ECG with a horizontal position of the electrical axis of the heart must be distinguished from signs of left ventricular hypertrophy. When the electrical axis of the heart is vertical, the R wave has a maximum amplitude in leads aVF, II and III; in leads aVL and I, a pronounced S wave is recorded, which is also possible in the left chest leads. ÂQRS = + 70° – +90°. Such...
When the heart rotates clockwise around its longitudinal axis (as viewed from the apex), the right ventricle moves forward and upward, and the left ventricle moves backward and downward. This position is a variant of the vertical position of the heart axis. On the ECG, a deep Q wave appears in lead III, and occasionally in lead aVF, which can simulate signs...
Premature or early repolarization syndrome is a relatively rare variant of a normal ECG. The main symptom of this syndrome is ST segment elevation, which has a peculiar shape of a convex downward arc and begins from a high J point on the descending knee of the R wave or on the terminal part of the S wave. A notch at the point of transition of the QRS complex to the descending ST segment ...
Peculiar ECG changes are observed in persons with dextrocardia. They are characterized by the opposite direction of the main teeth compared to the usual one. Thus, in lead I, negative P and T waves are detected, the main wave of the QRS complex is negative, and a QS type complex is often recorded. Deep Q waves may be observed in the chest leads, which may give rise to erroneous diagnosis of large-focal changes...
The information on the site is for informational purposes only and is not a guide for self-medication.








