I would like to tell you about the main diagnostic method - ECG for myocardial infarction. Using a cardiogram, you will learn to determine the degree of damage to your heart by pathologies.
Nowadays, myocardial infarction is very common dangerous disease. Many of us may confuse the symptoms of a heart attack with acute angina, which can lead to tragic consequences and death. With this diagnostic method, cardiologists can accurately determine the condition of the human heart.
If you notice the first symptoms, you should urgently do an ECG and consult a cardiologist. In our article you can find out how to prepare yourself for this procedure and how it will be deciphered. This article will be useful to everyone, since no one is immune from this pathology.
 ECG for myocardial infarction
ECG for myocardial infarction Myocardial infarction is necrosis (tissue death) of part of the heart muscle, which occurs due to insufficient oxygen supply to the heart muscle due to circulatory failure. It is myocardial infarction that is main reason mortality, today, and disability of people around the world.
ECG for myocardial infarction main tool for its diagnosis. If symptoms characteristic of the disease appear, you should immediately visit a cardiologist and undergo an ECG test, since the first hours are very important.
You should also undergo regular examinations for early diagnosis of deterioration in heart function. Main symptoms:
- dyspnea;
- chest pain;
- weakness;
- rapid heartbeat, interruptions in heart function;
- anxiety;
- heavy sweating.
The main factors due to which oxygen poorly enters the blood and blood flow is disrupted are:
- coronary stenosis (due to a blood clot or plaque, the opening of the artery is acutely narrowed, which becomes the cause of large-focal myocardial infarction).
- coronary thrombosis (the lumen of the artery is suddenly blocked, causing large-focal necrosis of the walls of the heart).
- stenosing coronary sclerosis (the lumens of some coronary arteries, which causes small focal myocardial infarctions).
Myocardial infarction quite often develops against the background of arterial hypertension, diabetes mellitus and atherosclerosis. It can also occur due to smoking, obesity and a sedentary lifestyle.
Conditions that provoke myocardial infarction, due to which oxygen supply decreases, can be:
- constant anxiety;
- nervous tension;
- excessive physical activity;
- surgical intervention;
- changes in atmospheric pressure.
An ECG during myocardial infarction is carried out using special electrodes that are attached to an ECG machine and which record the signals sent by the heart. For a regular ECG, six sensors are sufficient, but for the most detailed analysis of the functioning of the heart, twelve leads are used.


Cardiac pathology can acquire various shapes. Electrocardiographic diagnosis of myocardial infarction can detect the following types of disease:
- transmural;
- subendocardial;
- intramural.
Each disease is characterized by a specific state of zones of necrosis, damage, and ischemia. Transmural myocardial infarction has signs of large-focal necrosis, which affects from 50% to 70% of the walls of the left ventricle. The vector of depolarization of the opposite wall helps to detect signs of myocardial infarction of this type.
The difficulty of diagnosis lies in the fact that a significant part of the myocardium does not demonstrate the changes occurring in it and only vector indicators can indicate them. Subendocardial myocardial infarction does not belong to small focal forms of the disease.
It almost always occurs extensively. The greatest difficulty for doctors in studying the condition internal organ represents blurring of the boundaries of areas of the affected myocardium.
When signs of subendocardial damage are detected, doctors observe the time of their manifestation. Signs of myocardial infarction of the subendocardial type can be considered full confirmation of the presence of pathology if they do not disappear within 2 days. Intramural myocardial infarction is considered to be medical practice rarity.
It is detected quite quickly in the first hours of its occurrence, since the vector of myocardial excitation on the ECG indicates changes in the heart metabolic processes. Potassium leaves cells affected by necrosis. But the difficulty in detecting pathology is that potassium damage currents are not formed, because it does not reach the epicardium or endocardium.
To identify this type of myocardial infarction, even longer monitoring of the patient's condition is required. An ECG must be performed regularly for 2 weeks. One transcript of the analysis results is not a full confirmation or denial preliminary diagnosis. It is possible to clarify the presence or absence of a disease only by analyzing its signs in the dynamics of their development.


Depending on the symptoms, there are several types of myocardial infarction:
- Anginal is the most common option. It manifests itself as severe pressing or squeezing pain behind the sternum that lasts more than half an hour and does not go away after taking medication (nitroglycerin). This pain can radiate to the left side of the chest, as well as to left hand, jaw and back. The patient may experience weakness, anxiety, fear of death, and severe sweating.
- Asthmatic - a variant in which shortness of breath or suffocation is observed, palpitations. Most often there is no pain, although it may be a precursor to shortness of breath. This variant of the development of the disease is typical for older people. age groups and for people who have previously suffered a myocardial infarction.
- Gastralgic is a variant characterized by an unusual localization of pain that manifests itself in the upper abdomen. It can spread to the shoulder blades and back. This option is accompanied by hiccups, belching, nausea, and vomiting. Due to intestinal obstruction, bloating is possible.
- Cerebrovascular - symptoms associated with cerebral ischemia: dizziness, fainting, nausea, vomiting, loss of orientation in space. The appearance of neurological symptoms complicates the diagnosis, which can be absolutely correctly made in this case only with the help of an ECG.
- Arrhythmic - an option when the main symptom is palpitations: a feeling of cardiac arrest and interruptions in its work. Pain is absent or mild. You may experience weakness, shortness of breath, fainting, or other symptoms caused by a drop in blood pressure.
- Asymptomatic – a variant in which detection suffered a heart attack myocardium is possible only after taking an ECG. However, a heart attack can be preceded by mild symptoms such as causeless weakness, shortness of breath, and interruptions in heart function.
For any type of myocardial infarction, an ECG must be done for an accurate diagnosis.
Cardiac cardiogram
Human organs pass a weak current. This is precisely what allows us to make an accurate diagnosis using a device that records electrical impulses. The electrocardiograph consists of:
- a device that enhances weak current;
- voltage measuring device;
- recording device on an automatic basis.
Based on the cardiogram data, which is displayed on the screen or printed on paper, the specialist makes a diagnosis. There are special tissues in the human heart, otherwise called the conduction system, they transmit signals to the muscles indicating relaxation or contraction of the organ.
The electric current in the heart cells flows in periods, these are:
- depolarization. The negative cellular charge of the heart muscles is replaced by a positive one;
- repolarization. The negative intracellular charge is restored.
A damaged cell has lower electrical conductivity than a healthy one. This is exactly what the electrocardiograph records. Passing a cardiogram allows you to record the effect of currents that arise in the work of the heart.
When there is no current, the galvanometer records a flat line (isoline), and if the myocardial cells are excited in different phases, the galvanometer records a characteristic tooth directed up or down.
An electrocardiographic test records three standard leads, three reinforced leads and six chest leads. If there are indications, then leads are also added to check the posterior parts of the heart.
The electrocardiograph records each lead with a separate line, which further helps to diagnose cardiac lesions.
As a result, a complex cardiogram has 12 graphic lines, and each of them is studied.
On the electrocardiogram, five teeth stand out - P, Q, R, S, T, there are cases when U is also added. Each has its own width, height and depth, and each is directed in its own direction.
There are intervals between the teeth, they are also measured and studied. Interval deviations are also recorded. Each tooth is responsible for the functions and capabilities of certain muscular parts of the heart. Experts take into account the relationship between them (it all depends on the height, depth and direction).
All these indicators help to distinguish normal myocardial function from impaired, caused by various pathologies. main feature electrocardiogram is to identify and record symptoms of pathology that are important for diagnosis and further treatment.


ECG diagnosis of myocardial infarction allows you to determine the localization of ischemia. For example, it may appear in the walls of the left ventricle, on the anterior walls, septa or lateral walls.
It is worth noting that myocardial infarction most rarely occurs in the right ventricle, therefore, to determine it, specialists use special chest leads in diagnosis.
Localization of myocardial infarction by ECG:
- Anterior infarction - the LAP artery is affected. Indicators: V1-V4. Leads: II,III, aVF.
- Posterior infarction - the RCA artery is affected. Indicators: II,III, aVF. Leads: I, aVF. Lateral infarction - the Circunflex artery is affected. Indicators: I, aVL, V5. Leads: VI.
- Basal infarction - the RCA artery is affected. Indicators: none. Leads V1,V2.
- Septal infarction – the Septal performan artery is affected. Indicators: V1,V2, QS. Leads: none.
Preparation and procedure


Many people believe that the ECG procedure does not require special preparation. However, for a more accurate diagnosis of myocardial infarction, it is necessary to adhere to the following rules:
- Stable psycho-emotional background, the patient must be extremely calm and not nervous.
- If the procedure takes place in the morning, you should refuse to eat.
- If the patient smokes, it is advisable to refrain from smoking before the procedure.
- It is also necessary to limit fluid intake.
Before the examination, it is necessary to remove outerwear, and expose your shins. The specialist wipes the electrode attachment site with alcohol and applies a special gel. Electrodes are placed on the chest, ankles and arms. During the procedure the patient is in horizontal position. The ECG takes approximately 10 minutes.
During normal operation of the organ, the line has the same cyclicity. The cycles are characterized by sequential contraction and relaxation of the left and right atria and ventricles. At the same time, complex processes occur in the heart muscle, accompanied by bioelectric energy.
Electrical impulses generated in different parts of the heart are evenly distributed throughout the human body and reach skin person, which is fixed by the device using electrodes.
Interpretation of ECG for myocardial infarction


Myocardial infarction is divided into 2 types - large focal and small focal. An ECG allows you to diagnose large focal myocardial infarction. The electrocardiogram consists of teeth (protrusions), intervals and segments.
On a cardiogram during a heart attack, the protrusions look like concave or convex lines. In medical practice, there are several types of teeth that are responsible for the processes occurring in the myocardium; they are designated by Latin letters.
The P protrusion characterizes the contractions of the atria, the Q R S protrusions reflect the state of the contractile function of the ventricles, and the T protrusion records their relaxation. The R wave is positive, the Q S waves are negative and directed downward. A decrease in the R wave indicates pathological changes in heart.
Segments are straight line segments connecting the protrusions to each other. The ST segment located in the midline is considered normal. An interval is a specific area consisting of protrusions and a segment.
A large focal myocardial infarction is shown on the cardiogram as a modification of the complex of Q R S protrusions. The appearance of a pathological Q protrusion indicates the development of pathology. The Q indicator is considered the most stable sign of myocardial infarction.
An electrocardiogram does not always show signs that determine the development of pathology the first time, but only in 50% of cases. The first characteristic sign of the development of pathology is ST segment elevation.
What does a large heart attack look like on a cardiogram? The following picture is typical for large focal MI:
- R wave - completely absent;
- Q wave - significantly increased in width and depth;
- ST segment - located above the isoline;
- T wave - in most cases has a negative direction.


During the study, the following features and deviations are checked:
- Poor circulation, which leads to arrhythmia.
- Restriction of blood flow.
- Failure of the right ventricle.
- Thickening of the myocardium – development of hypertrophy.
- Cardiac arrhythmia as a result of pathological electrical activity hearts.
- Transmural infarction of any stage.
- Features of the location of the heart in the chest.
- Heart rate regularity and activity intensity.
- The presence of damage to the myocardial structure.
Normal indicators
All heart rate impulses are recorded in the form of a graph, where changes in the curve are marked vertically, and the time of declines and rises is calculated horizontally.
Teeth - vertical stripes are designated by letters of the Latin alphabet. Horizontal segments are measured that record changes - the intervals of each cardiac process (systole and diastole).
Adults have normal levels healthy heart are:
- Before the contraction of the atria, the P wave will be indicated. It is a determinant sinus rhythm.
- The PQ interval has a duration of 0.1 seconds.
- The T wave explains the processes during repolarization of the right and left ventricles. It indicates the stage of diastole.
- The QRS process lasts 0.3 seconds on the graph, which includes several teeth. This is a normal depolarization process during ventricular contraction.
It can be negative or positive, and the duration of such a marker is no more than a tenth of a second. Deviation from the norm may indicate impaired diffuse metabolic processes.
It is during this time that the sinus impulse has time to pass through the artioventicular node.


ECG indicators during myocardial infarction are very important in diagnosing the disease and identifying its features. Diagnosis must be quick in order to find out the features of damage to the heart muscle and understand how to resuscitate the patient.
The location of the affected area can be different: death of the tissues of the right ventricle, damage to the pericardial sac, death of the valve.
The lower left atrium may also be affected, preventing blood from leaving this area. Transmural infarction leads to blockage of blood vessels in the area of the coronary supply to the heart muscle. Defining points in diagnosing a heart attack:
- Exact localization of the site of muscle death.
- Period of effect (how long the condition lasts).
- Depth of damage. On an ECG, signs of myocardial infarction are easily detected, but it is necessary to find out the stages of the lesion, which depend on the depth of the lesion and the strength of its spread.
- Concomitant lesions of other areas of the heart muscles.
Important to consider. The indicators of the teeth are also in the case of blockade of the His bundle in the lower part, which provokes the onset of the next stage - transmural infarction of the left ventricular septum.
With absence timely treatment the disease can spread to the area of the right ventricle, since the blood flow is disrupted and necrotic processes in the heart continue. To prevent a deterioration in health, the patient is administered metabolic and diffuse drugs.
Stages of myocardial necrosis


Between healthy and dead (necrotic) myocardium, intermediate stages are distinguished in electrocardiography:
- ischemia,
- damage.
ISCHEMIA: this is the initial damage to the myocardium, in which there are no microscopic changes in the heart muscle yet, and the function is already partially impaired.
As you should remember from the first part of the cycle, on the cell membranes of nerve and muscle cells Two opposite processes occur sequentially: depolarization (excitation) and repolarization (restoration of the potential difference). Depolarization is a simple process, for which you only need to open ion channels in the cell membrane, through which, due to the difference in concentrations, ions will flow outside and inside the cell.
Unlike depolarization, repolarization is an energy-intensive process that requires energy in the form of ATP. Oxygen is necessary for the synthesis of ATP, therefore, during myocardial ischemia, the repolarization process first begins to suffer. Impaired repolarization is manifested by changes in the T wave.
With myocardial ischemia, the QRS complex and ST segments are normal, but the T wave is changed: it is widened, symmetrical, equilateral, increased in amplitude (span) and has a pointed apex. In this case, the T wave can be either positive or negative - this depends on the location of the ischemic focus in the thickness of the heart wall, as well as on the direction of the selected ECG lead.
Ischemia is a reversible phenomenon; over time, metabolism (metabolism) is restored to normal or continues to deteriorate with the transition to the damage stage.
DAMAGE: this is a deeper damage to the myocardium, in which an increase in the number of vacuoles, swelling and degeneration of muscle fibers, disruption of membrane structure, mitochondrial function, acidosis (acidification of the environment), etc. are determined under a microscope. Both depolarization and repolarization suffer. The injury is thought to primarily affect the ST segment.
The ST segment can shift above or below the isoline, but its arc (this is important!) when damaged is convex in the direction of displacement. Thus, when the myocardium is damaged, the arc of the ST segment is directed towards the displacement, which distinguishes it from many other conditions in which the arc is directed towards the isoline (ventricular hypertrophy, bundle branch block, etc.).
When damaged, the T wave can be of different shapes and sizes, which depends on the severity of concomitant ischemia. The damage also cannot exist for long and turns into ischemia or necrosis.
NECROSIS: death of the myocardium. Dead myocardium is unable to depolarize, so dead cells cannot form an R wave in the ventricular QRS complex. For this reason, during transmural infarction (death of the myocardium in a certain area along the entire thickness of the heart wall), there is no R wave at all in this ECG lead, and a QS-type ventricular complex is formed.
If necrosis has affected only part of the myocardial wall, a QrS type complex is formed, in which the R wave is reduced and the Q wave is increased compared to normal. Normally, the Q and R waves must obey a number of rules, for example:
- the Q wave should always be present in V4-V6.
- The width of the Q wave should not exceed 0.03 s, and its amplitude should NOT exceed 1/4 of the amplitude of the R wave in this lead.
- the R wave should increase in amplitude from V1 to V4 (i.e., in each subsequent lead from V1 to V4, the R wave should howl higher than in the previous one).
- in V1, the r wave may normally be absent, then the ventricular complex has the appearance of QS. In people under 30 years of age, the QS complex can normally occasionally be in V1-V2, and in children - even in V1-V3, although this is always suspicious for an infarction of the anterior part of the interventricular septum.
Diagnosis in patients with bundle branch blocks


The presence of a blockade of the right leg does not prevent the detection of large-focal changes. And in patients with left leg block, ECG diagnosis of a heart attack is very difficult. Many ECG signs of large-focal changes against the background of left leg block have been proposed. When diagnosing acute MI, the most informative of them are:
- The appearance of a Q wave (especially a pathological Q wave) in at least two leads from leads aVL, I, v5, v6.
- Reduction of the R wave from lead V1 to V4.
- Serration of the ascending limb of the S wave (Cabrera sign) in at least two leads from V3 to V5.
- Concordant ST segment shift in two or more adjacent leads.
If any of these signs are detected, the probability of a heart attack is 90-100%, however, these changes are observed only in 20-30% of patients with MI due to blockade of the left leg (changes in the ST segment and T wave in dynamics are observed in 50%). Therefore, the absence of any ECG changes in a patient with left leg block does not in any way exclude the possibility of a heart attack.
For accurate diagnosis it is necessary to determine the activity of cardiac-specific enzymes or troponin T. Approximately the same principles for diagnosing MI in patients with ventricular pre-excitation syndrome and in patients with an implanted pacemaker (continuous ventricular stimulation).
In patients with blockade of the left anterior branch, signs of large-focal changes in the lower localization are:
- Registration in lead II of complexes like QS, qrS and rS (wave r
- The R wave in lead II is smaller than in lead III.
Presence of blockade of the left posterior branch, as a rule, does not make it difficult to identify large-focal changes.
Transmural infarction ECG
Experts divide the stage of transmural infarction into 4 stages:
- The most acute stage, which lasts from a minute to several hours;
- Acute stage, which lasts from an hour to two weeks;
- Non-acute stage, which lasts from two weeks to two months;
- The scar stage, which occurs after two months.
Transmural infarction refers to the acute stage. According to the ECG, it can be determined by the rising wave “ST” to “T”, which is in a negative position. On last stage transmural infarction, the formation of the Q wave occurs. The “ST” segment remains on the instrument readings from two days to four weeks.
If, upon repeated examination, the patient continues to rise in the ST segment, this indicates that he is developing a left ventricular aneurysm. Thus, transmural infarction characterized by the presence of a Q wave, a movement of “ST” towards the isoline and a “T” wave expanding in the negative zone.


Infarction of the posterior regions of the ventricle is quite difficult to diagnose using an ECG. In medical practice, in about 50% of cases, diagnostics do not show problems with the posterior regions of the ventricle. The posterior wall of the ventricle is divided into the following parts:
- The diaphragmatic region, where the posterior walls adjacent to the diaphragm are located. Ischemia in this part causes an inferior infarction (posterior phrenic infarction).
- The basal region (upper walls) adjacent to the heart. Cardiac ischemia in this part is called posterobasal infarction.
An inferior infarction occurs as a result of blockage of the right coronary artery. Complications are characterized by damage to the interventricular septum and posterior wall.
With a lower infarction, ECG indicators change as follows:
- The third Q wave becomes larger than the third R wave by 3 mm.
- The cicatricial stage of the infarction is characterized by a decrease in the Q wave to half R (VF).
- The expansion of the third Q wave to 2 mm is diagnosed.
- With a posterior infarction, the second Q wave rises above the first Q (in a healthy person these indicators are the opposite).
It is worth noting that the presence of a Q wave in one of the leads does not guarantee a posterior infarction. It can disappear and appear when a person breathes intensely. Therefore, to diagnose a posterior infarction, perform an ECG several times.


The difficulty is this:
- Excess weight of the patient can affect the conduction of cardiac current.
- It is difficult to identify new scars of myocardial infarction if there is already scarring on the heart.
- Impaired conduction of complete blockade, in this case it is difficult to diagnose ischemia.
- Frozen cardiac aneurysms do not record new dynamics.
Modern medicine and new ECG machines are able to easily carry out calculations (this happens automatically). Using Holter monitoring, you can record the work of the heart throughout the day.
Modern wards have cardiac monitoring and an audible alarm, which allows doctors to notice altered heartbeats. The final diagnosis is made by a specialist based on the results of an electrocardiogram and clinical manifestations.
An ECG during a heart attack is of great importance for its diagnosis, in particular for diagnosing localization, the magnitude of necrosis, for differential diagnosis in case of an unclear picture, pain of a different nature, and for prognosis.
Typical ECG changes during a heart attack are:
- a sharp shift of the RS-T interval (discordant) up and down in standard leads I and III;
- rapid decrease in the amplitude of the QRS complex or the formation of Q, QS waves;
- rapid development of inversion and deformation (discordant in leads) of the T wave.
Changes in the QRS complex on the ECG during a heart attack
According to relatively recent studies, the positive QRS complex recorded in standard leads is a mirror image of the negative potential that occurs normally inner layers myocardium (i.e. its intracavitary surface). If, during this movement of excitation, non-functioning, “dead” tissue appears between the inner and outer layers, which loses its polarization property, negative deviations of the electrocardiogram are perceived from the outer layers of the heart. In this case, the intracavitary negative potential is transmitted either unchanged (negative QRS complex) or in the form of a positive, but reduced or deformed QRS complex (due to the partial loss of the depolarization function of the myocardium). The location and size of the inactive, damaged (“dead”) area accordingly affect the ECG during a heart attack. This theory explains the main ECG abnormalities during a heart attack.
If there is damage (necrotization) of the entire thickness of the myocardial wall, QS waves appear on the ECG with the disappearance of the P wave, which means the transition of a negative potential through the “hole” (i.e., an area of dead tissue) to the epicardium. With such “end-to-end” necrosis, “cavitary type” complexes are transmitted, emanating directly from the genetic system (as is known, it is located in the form of branches of the His bundle and Purkinje fibers subendocardially). In case of partial damage to the myocardium with preservation of part of the living muscle tissue in the damage zone (in the form of “inclusions”), the negative QS potential will be conducted to the outer layers, but at the same time, modifications occur on the ECG during a heart attack due to the depolarization exhibited by the preserved areas of the myocardium.
Changes in the S-T segment and T wave on the ECG during a heart attack
Electrocardiograms acquire the so-called mural type with a sharp shift S-T segment. The displacement down and up from the isoline depends on whether this zone passes closer to the endocardium or epicardium.
It is clinically accepted that the displacement of the S-T line in coronary atherosclerosis is also a reflection of the degree of ischemia of the corresponding part of the myocardium.
The T wave was previously considered an indicator of the process of restoration of the bioelectric ability of the heart after systole. It is a very common idea that this tooth reflects the state of myocardial metabolism associated with the expenditure and replenishment of myocardial energy resources caused by its contraction. The metabolic and functional basis of this electrocardiographic indicator did not raise doubts among clinicians due to the fact that changes in the T wave turned out to be characteristic of a very wide range of physiological and pathological conditions(the tooth becomes altered not only with necrotic, inflammatory or sclerotic changes in the heart, but also with inhalation of a mixture poor in oxygen during hard work). In the experiment, T wave inversion was obtained when the heart was exposed to heat or cold. Of all the changes that are observed in coronary atherosclerosis and other myocardial lesions, changes in the direction and T wave are the most common on the ECG during a heart attack, detectable already at weak degrees lesions and are most reversible. The dynamic, temporary nature of the changes in this wave serves as one of the proofs of the metabolic nature of the changes underlying it.
The question arises: what are the chemical changes in the myocardium that lead to disruption of the electrical potentials and pathological ECG during a heart attack? An important prerequisite for clarifying this issue was the experience of M. G. Udelnov, which consists of the following. A piece of dead muscle tissue (taken from any animal) was applied to the heart of a cold-blooded (frog) or warm-blooded (rabbit) in situ (in vivo). As soon as a piece of dead tissue is applied to the heart, the electrocardiogram changes and becomes monophasic from normal. As soon as a piece of tissue is removed from the surface of the heart, the electrocardiogram becomes normal. Similar experience has shown that to obtain a monophasic electrocardiogram there is no need to apply a ligature to the coronary artery. Obviously, changes in the electrocardiogram under these conditions are caused by some chemical products that pass from a piece of dead tissue attached to the heart into the heart muscle.
Some clinical data also support the significance of changes in the composition of electrolytes in the myocardium during a heart attack (in the sense of the electrocardiographic picture). Thus, during cardiac catheterization in patients with infarction, an increase in potassium content was noted in the blood of the coronary sinus. In the acute phase of the disease, hyperkalemia is observed (with a simultaneous decrease in the content of other electrolytes, in particular sodium). Excess potassium in the blood is the result of its transfer from the infarcted left ventricle.
In case of severe heart attacks, the entire electrocardiographic triad is usually observed on the ECG (changes in the ST segment, QRS complex, T wave); with limited necrosis that does not cover the entire thickness of the heart wall, a monophasic curve on the ECG during a heart attack is not observed, but there is only a decrease S-T interval and inversion (or other changes) of the T wave.
Changes in standard leads I and II on the ECG during a heart attack indicate lesions localized in the anterior wall of the heart, and changes in standard leads III and II of the electrocardiogram indicate lesions localized in the posterior wall of the heart.
Changes in chest leads
With the introduction into practice of ECG for infarction of the precordial leads, the boundaries of topical diagnosis of myocardial lesions (and, of course, diagnostic capabilities in general) have expanded significantly. Usually six chest leads are used, but their number can be increased if necessary; in essence, every point on the surface of the chest wall can serve to tap one of the electrodes. Using multiple chest leads, it is possible to create a kind of topographical map of the location of changes in the myocardium and at the same time give an assessment of the degree of their massiveness (size). Of course, chest leads are suitable for recognizing focal lesions of the anterior and partly lateral walls of the heart. With extensive lesions of the anterior and anterolateral walls of the heart, changes in the electrocardiogram are noted both in standard I and II and in all chest leads.
Unipolar leads according to Wilson or Goldberger provide undoubted advantages for topical and early diagnosis using ECG during a heart attack. Changes in the ECG during a heart attack in leads V1-V2 indicate the localization of the lesion in the anterior part of the interventricular septum. Changes in the ECG during a heart attack in leads V5-V6 are characteristic of lesions in the outer (lateral) part of the left ventricle. Isolated changes indicate damage to the anterior wall in the area adjacent to the interventricular septum (with partial involvement of it) and the apex.
As is known, changes in the T wave in lead III sometimes occur in healthy individuals, but at the same time they can also indicate the presence of foci of necrosis in the posterior wall. To differentiate a negative T wave caused by organic changes from similar changes in this wave that are not associated with myocardial diseases (but depending on the position of the heart, the high position of the diaphragm, cardiac hypertrophy), unipolar lead aVF can be used. When the posterior wall is damaged (usually due to coronary atherosclerosis, especially with infarctions of this localization), a deep Q wave is observed, negative wave T both in standard lead III and in lead aVF, whereas in people without myocardial damage, in whom these changes are detected in standard lead III, in aVF the value of the Q wave is normal, and the T wave is positive.
An ECG during a heart attack allows one to determine atrial necrosis (although they are rarely isolated); in these cases, the atrial P waves change and the P-Q interval, With left atrial infarction, a change in the P wave in the form of widening, splitting or inversion in lead I, and the P-Q interval shifts downward; with a right atrium infarction, changes in the P wave and a downward shift of the P-Q interval are noted. Electrocardiographic signs of atrioventricular block and atrial form are important for diagnosing atrial infarction paroxysmal tachycardia, atrial extrasystole and atrial fibrillation.
ECG for myocardial infarction
One of the key topics in electrocardiography is the diagnosis of myocardial infarction. Let's look at this important topic in the following order:
Information relevant to “ECG in myocardial infarction”
Introduction Causes of myocardial infarction Symptoms of myocardial infarction Forms of infarction Factors in the development of myocardial infarction Prevention of myocardial infarction Probability of developing complications of myocardial infarction Complications of myocardial infarction Diagnosis of acute myocardial infarction Urgent Care in case of myocardial infarction Help before the ambulance arrives in case of myocardial infarction Must be able to resuscitate
Rice. 99. Intramural myocardial infarction With this type of infarction, the vector of myocardial excitation does not change significantly; potassium released from necrotic cells does not reach the endocardium or epicardium and does not generate damage currents that can be displayed on the ECG tape by displacement of the S-T segment. Consequently, of the ECG signs of myocardial infarction known to us, only
The above enumeration of ECG signs of myocardial infarction allows us to understand the principle of determining its localization. So, myocardial infarction is localized in those anatomical regions of the heart in the leads from which the 1st, 2nd, 3rd and 5th signs are recorded; The 4th sign plays a role
Consecutive changes in the ECG during myocardial infarction, depending on the stage of this disease, are strictly natural (see Chapter VII.3). However, in practice, sometimes situations arise when ECG signs of the acute or subacute stage of myocardial infarction persist long time and do not go into the scarring stage. In other words, the ECG shows an elevation of the S-T segment above for quite a long time
Rice. 98. Subendocardial myocardial infarction With this infarction, the magnitude of the myocardial excitation vector does not change, since it originates from the ventricular conduction system located under the endocardium and reaches the intact epicardium. Consequently, the first and second ECG signs of a heart attack are absent. During necrosis of myocardiocytes, potassium ions pour out under the endocardium, forming
Rice. 97. Large-focal myocardial infarction The above figure shows that recording electrode A, located above the area of transmural infarction, will not record the R wave, since the entire thickness of the myocardium has died and there is no excitation vector here. Electrode A will register only the pathological Q wave (display of the vector of the opposite wall). In case of subepicardial
In Fig. 89 schematically shows the ventricular myocardium. Rice. 89. Excitation of normal myocardium Excitation vectors of the ventricular myocardium spread from the endocardium to the epicardium, i.e. they are directed to the recording electrodes and will be graphically displayed on the ECG tape as R waves (vectors between the ventricular septum are not considered for ease of understanding). Whenever
At their core, myocardial infarctions are divided into two large groups: large-focal and small-focal. This division is focused not only on the volume of necrotic muscle mass, but also on the characteristics of the blood supply to the myocardium. Rice. 96. Features of the blood supply to the myocardium The heart muscle is fed through the coronary arteries, anatomically located under the epicardium. By
Myocardial infarction is dangerous in many ways due to its unpredictability and complications. The development of complications of myocardial infarction depends on several important factors: 1. the amount of damage to the heart muscle, the larger the area of the myocardium affected, the more pronounced the complications; 2. localization of the zone of myocardial damage (anterior, posterior, lateral wall of the left ventricle, etc.), in most cases it occurs
Sometimes, when recording an ECG in patients during an anginal attack or immediately after it, the electrocardiogram reveals signs characteristic of the acute or subacute stage of myocardial infarction, namely, a horizontal rise of the S-T segment above the isoline. However, this elevation of the segment persists for seconds or minutes, the electrocardiogram quickly returns to normal, unlike a heart attack
Myocardial infarction clinic. ECG for myocardial infarction
The condition that determines results of therapy for myocardial infarction. is his early diagnosis and adequate assessment of the patient’s condition for timely interventions, since all etiopathogenetic therapy produces main results within a “time window” lasting up to 6 hours.
Generally accepted criteria diagnosis of myocardial infarction are the nature of the pain syndrome, ECG changes, and enzyme disorders. The consequences appear later than 6 hours, and therefore they do not play a special role for early intervention.
For early ECG diagnostics of myocardial infarction it is necessary to dwell on modern data on the ECG picture of MI in the acute phase. The most common classification of myocardial infarction has been based on the identification of electrocardiographic and anatomical features. Thus, MI is divided into transmural and non-transmural, large- and small-focal. It has now been established that ECG signs and morphology are not identical, that is, MI with a pathological Q wave will not necessarily be through and vice versa. A new classification of MI has been adopted based on ECG signs based on their comparison with the clinical picture, course and prognosis. According to it, MI is divided into a heart attack with a Qr wave on the ECG (the presence of a pathological Q wave in at least 2 leads) and a heart attack without a Q wave with changes only in the final part of the ventricular complex of ST segment elevation, the presence of an “ischemic” T wave.
From the analysis of clinical data it follows that a heart attack with a Q-wave on the ECG has a more severe prognosis in the acute period, however, heart attacks without a Q-wave on the ECG, in turn, have a number of adverse consequences in the first year after their development.

The difference in early and long-term prognosis is associated with morphofunctional characteristics of myocardial infarction with and without a pathological Q-wave on the ECG. Q-wave MI typically results from rapid complete occlusion of a relatively large coronary artery (CA). The infarction process ends quickly. The prognosis is determined by the size of the MI and the condition of the myocardium. Non-Q-wave MI is the result of incomplete closure of a coronary artery, usually a smaller one. A significant number of patients have previous lesions of the coronary artery with the development of collaterals. All this determines the best prognosis acute period. However, partial thrombosis can later become complete, and the presence of previous atherosclerotic changes in the coronary artery creates conditions for progression in some patients. Hence the deterioration of the late prognosis for MI without a pathological Q wave.
ECG also does not make it possible to distinguish from the group of patients with MI without a Q-wave on the ECG of persons with “small-focal” MI. This purely anatomical representation cannot be accurately verified either by ECG or by clinical examination.
It is well known that more severe are anterior myocardial infarction. However, among diaphragmatic (posterior) MIs, severe forms. These include those in which the septal zone is involved with the development of severe arrhythmias and blockades, involvement of the right ventricle, as well as diaphragmatic MI with the appearance of a decrease in ST in the precordial leads V1-3 and an increase in the R wave in these positions, which is associated with the involvement of the posterior -high zones of the myocardium. The prognosis for such patients is relatively worse. To diagnose right ventricular MI, leads VR2-4 are used.
Availability clinical-electrocardiographic syndrome the development of myocardial infarction allows us to make a correct diagnosis in the first hours and begin intensive causal therapy.
To resolve the issue about the volume therapeutic measures it is also necessary, especially if several hours have passed since the onset of the painful attack, to determine the severity of the patient’s condition and his immediate prognosis.
On an ECG during myocardial infarction (photo 1), doctors clearly see signs of necrosis of cardiac tissue. The cardiogram for a heart attack is reliable diagnostic method and allows you to determine the degree of heart damage.

Interpretation of ECG for myocardial infarction
An electrocardiogram is a safe research method, and if a heart attack is suspected, it is simply irreplaceable. An ECG for myocardial infarction is based on a violation of cardiac conduction, i.e. in certain areas of the cardiogram, the doctor will see abnormal changes that indicate a heart attack. To obtain reliable information, doctors use 12 electrodes when taking data. Cardiogram for myocardial infarction(photo 1) registers such changes based on two facts:
- during a heart attack in a person, the process of excitation of cardiomyocytes is disrupted, and this occurs after cell death;
- in heart tissues affected by a heart attack, the electrolyte balance is disturbed - potassium largely leaves the damaged tissue pathologies.
These changes make it possible to register lines on the electrocardiograph that are signs of conduction disturbances. They do not develop immediately, but only after 2-4 hours, depending on the compensatory capabilities of the body. However, a cardiogram of the heart during a heart attack shows the accompanying signs that can be used to determine the dysfunction of the heart. The cardiology ambulance team sends the photo with a transcript to the clinic where such a patient will be admitted - cardiologists will be prepared in advance for a serious patient.
What does myocardial infarction look like on an ECG?(photo below) as follows:
- complete absence of the R wave or its significant decrease in height;
- extremely deep, falling Q wave;
- elevated S-T segment above the isoline level;
- presence of a negative T wave.
An electrocardiogram also shows the different stages of a heart attack. Heart attack on ECG(photo in gal.) can be subacute, when changes in the work of cardiomyocytes are just beginning to appear, acute, acute and at the stage of scarring.
An electrocardiogram also allows the doctor to evaluate the following parameters:
- diagnose the fact of a heart attack;
- determine the area where pathological changes have occurred;
- establish how long ago the changes occurred;
- decide on the patient’s treatment tactics;
- predict the possibility of death.
Transmural myocardial infarction is one of the most dangerous and severe types of heart damage. It is also called large-focal or Q-infarction. Cardiogram after myocardial infarction(photo below) with a large-focal lesion shows that the zone of dying heart cells covers the entire thickness of the heart muscle.

Myocardial infarction
Myocardial infarction is a consequence of coronary heart disease. Most often, ischemia is caused by atherosclerosis of the heart vessels, spasm or blockage. happen heart attack(photo 2) may also result from surgery if the artery is ligated or angioplasty is performed.
Ischemic infarction goes through four stages of the pathological process:
- ischemia, in which heart cells stop receiving the required amount of oxygen. This stage can last quite a long time, since the body includes all compensatory mechanisms to ensure normal heart function. The immediate mechanism of ischemia is the narrowing of the heart vessels. Up to a certain point, the heart muscle copes with such a lack of blood circulation, but when thrombosis narrows the vessel to a critical size, the heart is no longer able to compensate for the deficiency. This usually requires a narrowing of the artery by 70 percent or more;
- damage occurring directly in cardiomyocytes, which begins within 15 minutes after the cessation of blood circulation in the damaged area. A heart attack lasts approximately 4-7 hours. It is here that the patient begins to experience the characteristic signs of a heart attack - chest pain, heaviness, arrhythmia. Extensive cardiac infarction(photo below) - the most severe outcome of the attack; with such damage, the necrosis zone can reach up to 8 cm in width;
- necrosis is the death of heart cells and the cessation of their functions. In this case, cardiomyocytes die, necrosis does not allow them to perform their functions;
- scarring is the replacement of dead cells with connective tissue formations that are not capable of taking on the function of predecessors. This process begins almost immediately after necrosis and gradually, over 1-2 weeks, a connective tissue scar of fibrin fibers forms on the heart at the site of damage.
Hemorrhagic cerebral infarction is a related condition in terms of mechanisms of injury, but it represents the release of blood from the vessels of the brain, which interferes with the functioning of cells.

Heart after a heart attack
Heart after myocardial infarction(photo 3) undergoes a process of cardiosclerosis. The connective tissue that replaces the cardiomyocytes turns into a rough scar - this can be seen by pathologists during autopsies of people who have suffered a myocardial infarction.
The scar after myocardial infarction has different thickness, length and width. All these parameters affect the further activity of the heart. Deep and large areas of sclerosis are called extensive infarction. Recovery from such a pathology is extremely difficult. With microsclerosation, a heart attack, like a heart attack, can leave minimal damage. Often, patients do not even know that they have suffered from such a disease, since the signs were minimal.
Scar on the heart after a heart attack(photo in gal.) does not hurt in the future and does not make itself felt for about 5-10 years after a heart attack, however, it provokes a redistribution of the cardiac load on healthy areas, which now have to do more work. After a certain time, the heart after a heart attack (photo below) looks worn out - the organ cannot carry out the load, ischemic disease The heart condition in patients worsens, pain in the heart appears, shortness of breath, they quickly get tired, and constant drug support is required.
Gallery of photos of myocardial infarction
Myocardial infarction on the ECG has a number of characteristic features, which help differentiate it from other disorders of conduction and excitability of the heart muscle. It is very important to conduct an ECG diagnosis in the first few hours after an attack in order to obtain data on the depth of the lesion, the degree of functional heart failure, and the possible localization of the lesion. Therefore, if possible, the cardiogram is taken while still in the ambulance, and if this is not possible, then immediately upon the patient’s arrival at the hospital.
ECG signs of myocardial infarction
An electrocardiogram reflects the electrical activity of the heart - by interpreting the data from such a study, one can obtain comprehensive information about the functioning of the conduction system of the heart, its ability to contract, pathological foci of excitation, as well as the course of various diseases.
The first sign to look for is deformation of the QRST complex, in particular, a significant reduction in the R wave or its complete absence.
The classic ECG picture consists of several areas that can be seen on any normal tape. Each of them is responsible for a separate process in the heart.
- P wave– visualization of atrial contraction. By its height and shape one can judge the state of the atria, their coordinated work with other parts of the heart.
- PQ interval– shows the spread of the excitation impulse from the atria to the ventricles, from the sinus node down to the atrioventricular node. Prolongation of this interval indicates a conduction disorder.
- QRST complex- ventricular complex, which gives full information about the condition of the most important chambers of the heart, the ventricles. Analysis and description of this part of the ECG is the most important part of diagnosing a heart attack; the main data is obtained from here.
- ST segment– an important part, which is normally an isoline (a straight horizontal line on the main ECG axis, without teeth), with pathologies capable of descending and rising. This may be evidence of myocardial ischemia, i.e. insufficient blood supply to the heart muscle.
Any changes in the cardiogram and deviations from the norm are associated with pathological processes in the cardiac tissue. In the case of a heart attack - with necrosis, that is, necrosis of myocardial cells with their subsequent replacement with connective tissue. The stronger and deeper the damage, the wider the area of necrosis, the more noticeable the changes on the ECG will be.
The first sign to look for is deformation of the QRST complex, in particular, a significant reduction in the R wave or its complete absence. This indicates a violation of ventricular depolarization (the electrical process responsible for heart contraction).
Any changes in the cardiogram and deviations from the norm are associated with pathological processes in the cardiac tissue. In the case of a heart attack - with the necrosis of myocardial cells, followed by their replacement with connective tissue.
Further changes affect the Q wave - it becomes pathologically deep, which indicates a disruption in the functioning of pacemakers - nodes made of special cells in the thickness of the myocardium that begin contraction of the ventricles.
The ST segment also changes - normally it is on the isoline, but during a heart attack it can rise higher or fall lower. In this case, they speak of elevation or depression of the segment, which is a sign of ischemia of the heart tissue. Using this parameter, it is possible to determine the localization of the area of ischemic damage - the segment is raised in those parts of the heart where necrosis is most pronounced, and lowered in the opposite leads.
Also, after some time, especially closer to the scarring stage, a negative deep T wave is observed. This wave reflects massive necrosis of the heart muscle and makes it possible to determine the depth of damage.
An ECG photo for myocardial infarction with interpretation allows you to consider the described signs in detail.

The tape can move at speeds of 50 and 25 mm per second; more low speed with better detail. When diagnosing a heart attack, not only changes in leads I, II and III are taken into account, but also in the reinforced ones. If the device allows you to record the chest leads, then V1 and V2 will display information from the right parts of the heart - the right ventricle and atrium, as well as the apex, V3 and V4 about the apex of the heart, and V5 and V6 will indicate the pathology of the left parts.
Closer to the scarring stage, a negative deep T wave is observed. This wave reflects massive necrosis of the heart muscle and allows you to determine the depth of damage.
Stages of myocardial infarction on ECG
A heart attack occurs in several stages, and each period is marked by special changes on the ECG.
- Ischemic stage (damage stage, acute) related to development acute failure circulation in the tissues of the heart. This stage does not last long, so it is rarely recorded on a cardiogram tape, but it diagnostic value quite high. At the same time, the T wave increases and becomes sharper - they speak of a giant coronary T wave, which is a harbinger of a heart attack. Then ST rises above the isoline; its position here is stable, but further elevation is possible. When this phase lasts longer and becomes acute, a decrease in the T wave can be observed, as the focus of necrosis spreads to the deeper layers of the heart. Reciprocal and reverse changes are possible.
- Acute stage (necrosis stage) occurs 2-3 hours after the onset of the attack and lasts up to several days. On the ECG it looks like a deformed, wide QRS complex, forming a monophasic curve, where it is almost impossible to distinguish individual waves. The deeper the Q wave on the ECG, the deeper layers were affected by ischemia. At this stage, transmural infarction can be recognized, which will be discussed later. Characteristic rhythm disturbances are arrhythmias, extrasystoles.
- Recognize the onset of the subacute stage possible by stabilizing the ST segment. When it returns to the baseline, the infarction no longer progresses due to ischemia, and the recovery process begins. The greatest importance in this period is the comparison of the existing T wave sizes with the original ones. It can be either positive or negative, but will slowly return to the baseline in sync with the healing process. Secondary deepening of the T wave in the subacute stage indicates inflammation around the necrosis zone and does not last long, with proper drug therapy.
- In the scarring stage, the R wave rises again to its characteristic values, and T is already on the isoline. In general, the electrical activity of the heart is weakened, because some of the cardiomyocytes have died and been replaced by connective tissue, which does not have the ability to conduct and contract. Pathological Q, if present, is normalized. This stage lasts up to several months, sometimes six months.
It is very important to conduct an ECG diagnosis in the first few hours after an attack in order to obtain data on the depth of the lesion, the degree of functional heart failure, and the possible localization of the lesion.
Main types of heart attack on ECG
In the clinic, a heart attack is classified depending on the size and location of the lesion. This is important in the treatment and prevention of delayed complications.
Depending on the size of the damage, there are:
- Large-focal, or Q-infarction. This means that the circulatory disorder occurred in a large coronary vessel, and a large volume of tissue is affected. The main sign is a deep and widened Q wave, and the R wave cannot be seen. If the infarction is transmural, that is, affecting all layers of the heart, the ST segment is located high above the isoline, in the subacute period a deep T is observed. If the damage is subepicardial, that is, not deep and located next to the outer shell, then R will be recorded, albeit small.
- Small focal, non-Q infarction. Ischemia developed in areas supplied by the terminal branches of the coronary arteries; this type of disease has a more favorable prognosis. With an intramural infarction (the damage does not extend beyond the heart muscle), Q and R do not change, but a negative T wave is present. In this case, the ST segment is on the isoline. In subendocardial infarction (focus near the inner lining), T is normal and ST is depressed.

Depending on the location, the following types of heart attack are determined:
- Anteroseptal Q-infarction– noticeable changes in 1-4 chest leads, where there is no R in the presence of wide QS, ST elevation. In standard I and II – pathological Q, classic for this type.
- Lateral Q-infarction– identical changes affect chest leads 4-6.
- Posterior or diaphragmatic Q-infarction, also known as inferior– pathological Q and high T in leads II and III, as well as intensified from the right leg.
- Interventricular septal infarction– in standard I, deep Q, ST elevation and high T. In thoracic 1 and 2, R is pathologically high, and A-V block is also characteristic.
- Anterior non-Q infarction– in thoracic I and 1-4 T is higher than the preserved R, and in II and III there is a decrease in all waves along with ST depression.
- Posterior non-Q infarction– in standard II, III and chest 5-6 positive T, decreased R and depression ST.
Video
We offer you to watch a video on the topic of the article.
Applied in practical purposes In the 70s of the 19th century, the Englishman A. Waller created a device that records the electrical activity of the heart and continues to faithfully serve humanity to this day. Of course, over almost 150 years it has undergone numerous changes and improvements, but the principle of its operation, based on recordings of electrical impulses propagating in the heart muscle, remained the same.
Now almost every ambulance team is equipped with a portable, lightweight and mobile electrocardiograph, which allows you to quickly take an ECG, not waste precious minutes, diagnose and quickly transport the patient to the hospital. For large-focal myocardial infarction and other diseases that require emergency measures, minutes count, so an urgently taken electrocardiogram saves more than one life every day.
Deciphering an ECG for a cardiology team doctor is a common thing, and if it indicates the presence of acute cardiovascular pathology, then the team immediately turns on the siren and goes to the hospital, where, bypassing the emergency room, they will deliver the patient to the intensive care unit for treatment. urgent help. The diagnosis has already been made using an ECG and no time has been lost.
Patients want to know...
Yes, patients want to know what the strange teeth on the tape left by the recorder mean, so before going to the doctor, patients want to decipher the ECG themselves. However, everything is not so simple and in order to understand the “sophisticated” record, you need to know what the human “motor” is.
The heart of mammals, which includes humans, consists of 4 chambers: two atria, endowed with auxiliary functions and having relatively thin walls, and two ventricles, which bear the main load. The left and right parts of the heart are also different. Providing blood to the pulmonary circle is less difficult for the right ventricle than pushing blood into big circle blood circulation to the left. Therefore, the left ventricle is more developed, but also suffers more. However, regardless of the difference, both parts of the heart must work evenly and harmoniously.

The heart is heterogeneous in its structure and electrical activity, since contractile elements (myocardium) and non-contractile elements (nerves, vessels, valves, fatty tissue) differ from each other in varying degrees of electrical response.
Typically, patients, especially older ones, worry about whether there are signs of myocardial infarction on the ECG, which is quite understandable. However, to do this you need to learn more about the heart and the cardiogram. And we will try to provide this opportunity by talking about waves, intervals and leads and, of course, about some common heart diseases.
Heart Abilities
We first learn about the specific functions of the heart from school textbooks, so we imagine that the heart has:
- Automatically, caused by the spontaneous generation of impulses, which then cause its excitation;
- Excitability or the ability of the heart to activate under the influence of exciting impulses;
- or the “ability” of the heart to ensure the conduction of impulses from the place of their origin to the contractile structures;
- Contractility, that is, the ability of the heart muscle to contract and relax under the control of impulses;
- Tonicity, in which the heart does not lose its shape in diastole and ensures continuous cyclic activity.
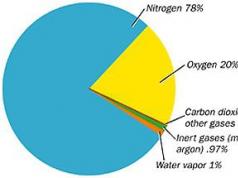
In general, the heart muscle in a calm state (static polarization) is electrically neutral, and biocurrents(electrical processes) are formed in it under the influence of exciting impulses.
Biocurrents in the heart can be recorded
Electrical processes in the heart are caused by the movement of sodium ions (Na+), which are initially located outside the myocardial cell, into it and the movement of potassium ions (K+), rushing from inside the cell to the outside. This movement creates conditions for changes in transmembrane potentials throughout cardiac cycle and recurring depolarizations(excitation, then contraction) and repolarizations(transition to the original state). All myocardial cells have electrical activity, but slow spontaneous depolarization is characteristic only of the cells of the conduction system, which is why they are capable of automatism.
 Excitement spreading through conducting system, sequentially covers the parts of the heart. Starting in the sinoatrial (sinus) node (the wall of the right atrium), which has maximum automaticity, the impulse passes through the atrial muscles, the atrioventricular node, the bundle of His with its legs and is directed to the ventricles, stimulating parts of the conduction system even before the manifestation of its own automaticity .
Excitement spreading through conducting system, sequentially covers the parts of the heart. Starting in the sinoatrial (sinus) node (the wall of the right atrium), which has maximum automaticity, the impulse passes through the atrial muscles, the atrioventricular node, the bundle of His with its legs and is directed to the ventricles, stimulating parts of the conduction system even before the manifestation of its own automaticity .
Excitation that occurs on the outer surface of the myocardium leaves this part electronegative in relation to areas not affected by excitation. However, due to the fact that body tissues have electrical conductivity, biocurrents are projected onto the surface of the body and can be recorded and recorded on a moving tape in the form of a curve - an electrocardiogram. The ECG consists of waves that are repeated after each heartbeat, and through them shows the disorders that exist in the human heart.
How is an ECG taken?
Many people can probably answer this question. Doing an ECG, if necessary, will also not be difficult - there is an electrocardiograph in every clinic. ECG technique? It only seems at first glance that it is so familiar to everyone, but meanwhile, only medical workers who have undergone special training in taking an electrocardiogram know it. But we hardly need to go into details, since no one will allow us to do such work without preparation anyway.

Patients need to know how to properly prepare: that is, it is advisable not to overeat, not to smoke, not to drink alcoholic beverages and medications, not to get involved in heavy physical labor and not to drink coffee before the procedure, otherwise you can fool the ECG. It will certainly be provided, if nothing else.
So, a completely calm patient undresses to the waist, frees his legs and lies down on the couch, and the nurse will lubricate the necessary places (leads) with a special solution, apply electrodes from which wires go to the device different colors, and take a cardiogram.
The doctor will decipher it later, but if you are interested, you can try to figure out your teeth and intervals yourself.
Teeth, leads, intervals
This section may not be of interest to everyone, in which case you can skip it, but for those who are trying to understand their ECG on their own, it may be useful.
The waves in the ECG are designated using Latin letters: P, Q, R, S, T, U, where each of them reflects the state of different parts of the heart:
- P – atrial depolarization;
- QRS wave complex – ventricular depolarization;
- T – ventricular repolarization;
- A weak U wave may indicate repolarization of the distal portions of the ventricular conduction system.

To record an ECG, 12 leads are usually used:
- 3 standard – I, II, III;
- 3 reinforced unipolar limb leads (according to Goldberger);
- 6 reinforced unipolar chest (according to Wilson).
In some cases (arrhythmias, abnormal location of the heart), there is a need to use additional unipolar chest and bipolar leads according to Neb (D, A, I).

When interpreting the ECG results, the duration of the intervals between its components is measured. This calculation is necessary to assess the rhythm frequency, where the shape and size of the teeth in different leads will be an indicator of the nature of the rhythm, the electrical phenomena occurring in the heart and (to some extent) the electrical activity of individual sections of the myocardium, that is, the electrocardiogram shows how our heart works at that time. or another period.
Video: lesson on ECG waves, segments and intervals
ECG analysis
A more rigorous interpretation of the ECG is made by analyzing and calculating the area of the teeth when using special leads (vector theory), however, in practice, they mainly make do with such an indicator as electrical axis direction, which is the total QRS vector. It is clear that everyone’s chest is structured differently and the heart does not have such a strict arrangement, the weight ratio of the ventricles and the conductivity inside them are also different for everyone, therefore, when deciphering, the horizontal or vertical direction of this vector is indicated.
Doctors carry out ECG analysis in a sequential order, determining the norm and violations:
- Assess heart rhythm and measure heart rate (at normal ECG– sinus rhythm, heart rate – from 60 to 80 beats per minute);
- Intervals (QT, norm – 390-450 ms) are calculated, characterizing the duration of the contraction phase (systole) using a special formula (I often use Bazett’s formula). If this interval lengthens, then the doctor has the right to suspect. Hypercalcemia, on the contrary, leads to a shortening of the QT interval. The conductivity of the pulses reflected through the intervals is calculated using a computer program, which significantly increases the reliability of the results;
- they begin to calculate from the isoline according to the height of the teeth (normally R is always higher than S) and if S exceeds R and the axis deviates to the right, then they think about disturbances in the activity of the right ventricle, if on the contrary - to the left, and the height of S is greater than R in II and III leads – left ventricular hypertrophy is suspected;
- The QRS complex is studied, which is formed during the conduction of electrical impulses to the ventricular muscle and determines the activity of the latter (the norm is the absence of a pathological Q wave, the width of the complex is not more than 120 ms). If this interval shifts, then we speak of blockades (full or partial) of the bundle branches or conduction disturbances. Moreover, incomplete blockade of the right bundle branch is an electrocardiographic criterion of right ventricular hypertrophy, and incomplete blockade of the left bundle branch may indicate left ventricular hypertrophy;
- They describe the ST segments, which reflect the period of restoration of the initial state of the heart muscle after its complete depolarization (normally located on the isoline) and the T wave, which characterizes the process of repolarization of both ventricles, which is directed upward, asymmetrical, its amplitude is lower than the wave in duration and is longer than the QRS complex.
The decoding work is carried out only by a doctor, however, some ambulance paramedics perfectly recognize common pathologies, which is very important in emergency cases. But first, you still need to know the ECG norm.

This is what the cardiogram of a healthy person looks like, whose heart works rhythmically and correctly, but not everyone knows what this record means, which can change with different physiological conditions, for example pregnancy. In pregnant women, the heart takes a different position in the chest, so the electrical axis shifts. In addition, depending on the duration, the load on the heart is added. An ECG during pregnancy will reflect these changes.
The cardiogram indicators in children are also excellent; they will “grow” with the baby, and therefore will change according to age; only after 12 years, the child’s electrocardiogram begins to approach the ECG of an adult.
The most disappointing diagnosis: heart attack

The most serious diagnosis on the ECG, of course, is, in the recognition of which the cardiogram plays the main role, because it is she (the first!) that finds areas of necrosis, determines the localization and depth of the lesion, and can distinguish an acute infarction from the scars of the past.
The classic signs of myocardial infarction on the ECG are the registration of a deep Q wave (OS), segment elevationST, which deforms R, smoothing it, and the subsequent appearance of a negative pointed isosceles tooth T. This elevation of the ST segment visually resembles a cat’s back (“cat”). However, a distinction is made between myocardial infarction with and without the Q wave.

Video: signs of a heart attack on an ECG
When there's something wrong with your heart
Often in ECG conclusions you can find the expression: “”. As a rule, such a cardiogram is obtained by people whose hearts have had an additional load for a long time, for example, due to obesity. It is clear that the left ventricle has a hard time in such situations. Then the electrical axis deviates to the left, and S becomes greater than R.

hypertrophy of the left (left) and right (right) ventricles of the heart on the ECG
Video: cardiac hypertrophy on ECG
One of the presenters will answer your question.
The questions in this section are currently answered by: Sazykina Oksana Yurievna, cardiologist, therapist
You can thank a specialist for their help or support the VesselInfo project at any time.
In questions about interpreting the ECG, be sure to indicate the patient’s gender, age, clinical data, diagnoses and complaints.