29.08.2017
Phlebectasia or varicose veins of the stomach is a dangerous disease, which is manifested by an increase in the volume of the gastric veins and the occurrence of blood clots in them. The pathology is insidious due to its asymptomatic course initial stage. The disease is quite serious and therefore requires urgent treatment.
What are gastric varicose veins?
Dilatation of the veins of the mucous tissues of the stomach is not as common as varicose veins in the legs. The difference between pathologies lies in the reasons for their occurrence and progression. Often high blood pressure portal vein becomes the result of cirrhosis of the liver, although sometimes the result genetic pathologies or compression of the portal vein by a large tumor.
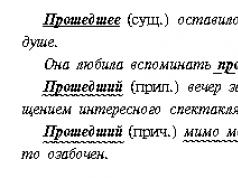
In the stomach, varicose veins are divided into 4 stages of development:
- Symptoms do not appear, the dilation of the lumen of blood vessels is isolated, so the patient has no complaints. Only endoscopy can reveal this degree.
- Vein structures take on a tortuous and uneven shape. In this case, the increase does not exceed 3 mm, and the narrowing of the lumens occurs at small intervals. Bleeding at this stage is a rare occurrence. Pathology can be detected by x-ray or endoscopy.
- There is a noticeable narrowing of the lumen of the veins and their swelling. The stage is characterized by the presence of nodes and narrowing of the tone of the walls. The main signs are already appearing; it is only necessary to recognize them in a timely manner, since the threat of hemorrhage at this stage increases significantly. Transfer of therapy is prohibited.
- The nodes are noticeably visible, the lumens are narrowing, the gastric mucosa is thoroughly depleted. It is likely that a whole thread of damaged vessels will diverge from a large node. The vessels are thinned to such an extent that hemorrhage is likely to open at any time. If this happens, the patient is at risk.
It is important to highlight that the development of gastric varicose veins requires a significant period; for this reason, short-term compression of the veins by a neoplasm is not capable of provoking the occurrence of characteristic changes.
The disease is classified into the following types:
- acquired - appears in the event of an increase in pressure in the portal vein. This vessel performs the function of delivering blood to the liver. Difficulties are created by a disruption in the movement of blood through this organ. Pathology makes the veins soft, brittle, with every chance of rupturing at any moment;
- inherited - the disease is determined from birth. As a rule, the complex course of the period of bearing a child may be associated with a genetic predisposition.
Congenital varicose veins of the gastric veins are a rare phenomenon. Most often, doctors diagnose an acquired type of illness. The pathology mainly affects patients over 50 years of age.
Gastric varicose veins causes of development

Cirrhosis of the liver can cause varicose veins
The main factor contributing to the onset of the disease is portal hypertension, which causes enlargement of the veins in digestive organ. Often, a similar condition is observed with cirrhosis of the liver due to the appearance of numerous scars on it. However, this is not the only condition for the occurrence dangerous disease. Other reasons causing the pathology:
- liver diseases that cause disruptions in blood flow;
- thrombus formation;
- compression of the portal vein by neoplasms;
- cardiovascular failure.
Particular care should be taken when diagnosing varicose veins in the stomach in patients affected by cirrhosis of the liver and hepatitis. This is due to greater vulnerability of organs and can end in disaster.
Symptoms of the disease and diagnosis
In the early stages, phlebectasia is asymptomatic, which creates difficulties in identifying the disease. Over time, the patient experiences following signs manifestations of pathology:
- Heaviness and discomfort in the chest area.
- An increase in abdominal volume caused by the accumulation of fluid in abdominal cavity.
- In the anterior lobe abdominal wall probably the outline of a “jellyfish head” - a pattern created by dilated veins.
- Difficulty breathing after physical activity.
- Increased heartburn not related to eating.
- Problems with the swallowing reflex.
It's good when a person pays attention to indicated symptoms and goes to the doctor. Diagnosis of the disease, due to the listed signs, will make it possible to carry out surgical measures aimed at treating phlebectasia. However, cases of visiting a doctor at this stage are rare. Typically, varicose veins of the gastric veins appear during rupture of blood vessels. At the beginning of hemorrhage, the pathology picture acquires the following signs:
- vomiting accompanied by bloody discharge (indicates the opening of hemorrhage in the stomach);
- drop in blood pressure;
- increased heart rate with irregularities;
- stomach ache;
- state of shock.

At the first symptoms of the disease, consult a doctor for examination
Bleeding may be small, although it is often profuse. It is necessary to start therapy urgently due to the fact that the pathology can worsen or result in the death of the patient.
Diagnosis of phlebectasia is carried out through endoscopy, as well as studies to detect coagulopathy. Varicose veins are identified using x-ray examination upper sections digestive system with the introduction of contrast and angiography.
Preference is given to endoscopy - it identifies veins affected by varicose veins, their volume and establishes hemorrhage in them. In patients with liver cirrhosis and phlebectasia, in 40% of cases they do not act as a source of hemorrhage. In such situations, bleeding is caused by erosions and bleeding of the gastric mucosa.
Endoscopy allows you to identify nodes with an increased risk of bleeding, even in the case of the confirmed presence of varicose veins. Due to the fact that the pathology occurs due to cirrhosis of the liver, it is necessary to find out possible problems with blood clotting. Lab tests include blood tests taking into account the number of platelets and characteristics of liver function.
Treatment of pathology
Since gastric varicose veins are not considered a self-occurring disease, there is no therapy for it. The use of certain medications makes it possible to reduce portal hypertension, so they are used comprehensively, exclusively as prescribed by the doctor.
If it is possible to eliminate the cause of hypertension, proper treatment or surgery is carried out; in most cases, the only cure is liver transplantation.
Drug treatment is carried out using the following means:
- Vasopressin - normalizes the condition of narrowed veins.
- Nitrates included in Nitroglycerin due to a decrease in pressure in the portal vein.
- Somatostatin or Ocreotide – reduce arterial pressure internal organs.
Help is provided at the onset of hemorrhage, for which a Blackmore probe is inserted into the digestive tract, through which the veins are compressed and the bleeding stops. At the same time, treatment is given to increase blood clotting.
Phlebectasia becomes a severe exacerbation of portal hypertension due to the fact that at one stage or another it provokes the formation of gastrointestinal hemorrhage, accompanied by the loss of a large volume of blood and threatening life.
In parallel, assistance with bleeding still remains symptomatic, and complete therapy involves eliminating portal hypertension directly. This is not acceptable in every case; for this reason, the prevention of both portal hypertension and phlebectasis is of particular importance, because it turns out to be very difficult to overcome existing disorders.
Prevention measures
The formation of pathology can be prevented by maintaining healthy blood vessels. To do this you need:
- monitor the condition of the liver;
- strictly follow the doctor’s recommendations;
- normalize blood pressure in time;
- lead healthy image life - give up bad habits, eat right;
- avoid lifting heavy objects.
Paying attention to your health means following simple principles. Such recommendations will actually help in maintaining the functioning of the gastrointestinal tract at required level and prevent the development of exacerbations.
A detailed description for our readers: causes of gastric varicose veins on the website in detail and with photographs.
Varicose veins develop when the blood supply to the stomach is disrupted. The condition is usually accompanied by changes in the structure of blood vessels, such as dilation, elongation, and the formation of loops or nodes. Pathology appears against the background of liver damage, in particular with cirrhosis. An invariable companion of varicose veins in the tissues of the stomach is small or heavy bleeding.
Varicose veins of the stomach refer to dangerous pathologies. The condition is characterized by an increase, often dilatation, of the veins of the organ with the formation of blood clots. The insidiousness of the disease lies in the absence of symptoms at an early stage, therefore timely diagnosis practically impossible. Mostly men suffer from this disease. The main provoking factors for the development of the disease, as well as liver damage, are:
- alcohol;
- unhealthy diet;
- uncontrolled drug treatment.
Return to contents
Symptoms
Varicose veins the veins of the stomach are scanty clinical picture. Symptoms are often similar to other gastrointestinal pathologies. However, there are distinctive features:
- Bloody vomiting with black vomit, indicating discovery stomach bleeding. Vomiting may be frequent and contain pink mucus.
- Increased heart rate with frequent interruptions.
- Abdominal pain.
The initial stages of gastric varicose veins are often accompanied by severe heartburn, which, although it causes discomfort, does not cause the need to go to the doctor. As the pathology develops, gastric bleeding begins. This condition is accompanied by symptoms such as:
- ascites, when free extrudate accumulates in the peritoneum, which provokes a strong increase in the size of the abdomen;
- abundant, bloody vomiting, does not cause pain;
- tachycardia with erratic and rapid pulse;
- hypotension, characterized by a sharp decrease in blood pressure;
- hypovolemic shock, accompanied by a sharp decrease in the effective volume of circulating blood.
Return to contents
Causes of gastric varicose veins
Gastric varices appear as a result of portal hypertension or increased pressure in the portal vein. The normal pressure in this vein is up to 6 mm Hg. Art. If this value jumps to 12-20 mm Hg. Art., blood flow is disrupted and vasodilation occurs. The root cause of portal hypertension is compression of the portal vein, which can cause thrombosis or stone passage in gallstone disease. Other causes of gastric varicose veins are:
- dysfunction of the pancreas, stomach;
- cirrhosis, hepatitis;
- echinecoccosis;
- tuberculosis;
- polycystic disease;
- acquired or congenital fibrosis;
- sarcoidosis;
- tumors, cysts, adhesions of various etiologies;
- aneurysms of the arteries of the spleen or liver;
- eosinophilic gastroenteritis;
- intestinal obstruction;
- general
Sometimes gastric varicose veins are preceded by a sudden load: heavy lifting, severe fever. Rarely, the disease is congenital. The reasons for this anomaly have not yet been discovered.
Return to contents
Diagnosis of the disease
Detection of varicose veins is possible only with instrumental examination. For this purpose the following methods are used:
- General and clinical researches blood, which is necessary for assessment general condition sick.
- Functional and hepatic examinations to determine coagulopathy.
- X-ray with contrast (barium sulfate), carried out to assess the functionality of the digestive tract.
- Esophagogastroscopy, used to visualize the condition of the internal walls of the stomach. The method is highly accurate, but requires increased attention and accuracy, since the affected tissues are fragile and the probe can cause bleeding.
- Ultrasound of the abdominal organs, which is necessary to confirm the diagnosis.
Return to contents
Treatment
There are three treatment approaches:
- therapeutic;
- medicinal;
- surgical.
The first two regimens are used in the early stages or after effective control of bleeding. Late stages are treated only surgically, as the risk of death associated with hypovolemic shock is high. The main approaches to treating gastric varicose veins are presented below.
Return to contents
Sclerotherapy
The essence of the method is to introduce special medical glue into the affected vessels endoscopically. A certain frequency of the procedure is required, which is determined by the doctor individually. More often, the technique is applied once every 7 or 30 days, and is completed when a permanent scar is formed.
Return to contents
Operation
Surgery can be performed in three ways:
- Ligation of dilated veins. For this, a special rubber bandage is used. The effectiveness of the technique is higher than sclerotherapy.
- Shunting in intrahepatic tissues. The technique is necessary to lower blood pressure. To do this, a stent is inserted into the middle of the liver. The procedure is performed under X-ray control. The goal is to create a connecting bridge between the hepatic and portal veins.
- Splenorenal shunting. The technique is used for preventive purposes - to prevent the development of bleeding. To do this, the veins of the spleen and left kidney are combined with a shunt.
Return to contents
Drug therapy for varicose veins
The essence of the method is to regularly take such means as:
- "Vasopressin" - to restore the normal state of narrowed blood vessels;
- nitrate containing “Nitroglycerin” - to lower pressure in the portal vein;
- "Somatostatin" or "Octreotide" - to lower blood pressure in the internal organs and restore the normal state of dilated blood vessels.
Return to contents
Diet therapy
To treat gastric varicose veins, it is important to maintain proper nutrition. The basic principles are as follows:
- Fractional meals in small portions - up to 6 times a day.
- The last snack is 3 hours before going to bed.
- Increasing in the diet the amount of foods rich in vitamins such as:
- vitamin E (greens, yolk, corn or sunflower oil);
- vitamin C (berries, potatoes, fresh peppers, all types of citrus fruits);
- rutin (nuts, tea, grapefruit, currants);
- bioflavonoids (cherries);
- plant fibers (legumes, fresh vegetables and fruits).
- Organize plenty of drinking - up to 2.5 liters of water per day.
- Complete rejection of harmful products:
- alcohol;
- concentrated black tea, coffee;
- sweets and sugar;
- hot seasonings and spices;
- flour products.
- Preferred culinary processing is boiling, baking in the oven, stewing, steaming.
- Dishes must be warm.
Return to contents
Prevention
The essence preventive measures- maintaining healthy veins. To do this you should:
- monitor the condition of the liver;
- follow the doctor's recommendations exactly;
- regulate high blood pressure in a timely manner;
- follow the rules of a healthy lifestyle (giving up bad habits, proper nutrition).
Return to contents
Complications
The most severe complication of gastric varicose veins is bleeding. They can even occur from overeating due to severe thinning of the walls of the organ. The amount of bleeding may vary, as will their frequency. The outcome depends on this. Bleeding causes severe vomiting, chronic iron deficiency.
Return to contents
Nerves and varicose veins
The condition of the body and its performance depend on stability nervous system. When a person is exposed to significant and long-term stress, anxiety, depression, the digestive system suffers first. Neurological causes development of varicose pathology:
- Chronic state of hatred.
- Feeling of chronic fatigue, severe overstrain.
- Loss of strength and spirit, disappointment and moral fatigue.
Therefore, during treatment it is important to have a positive attitude and eliminate all irritating factors.
Return to contents
Forecast
Mortality in gastric varicose veins is high due to the severity of complications and accompanying pathologies. More often, problems with the blood vessels of the main digestive organ, complicated by bleeding, are associated with progressive cirrhosis.
In 79% of cases, bleeding stops on its own with a mortality rate of 50%. After successful relief of the disease, the risk of the disease returning is 55-75%.
Gastric varicose veins are a pathological dilatation of blood vessels that develops under the influence of increased pressure in the portal vein. Varicose veins of the stomach manifest themselves in the form of protrusion and swelling of the walls and the formation of nodes. Varicose veins of internal organs, including the stomach, are a fairly rare pathology that is difficult to diagnose in the initial stages of development.
Varicose veins of the stomach
Varicose veins of the gastric vein can be congenital or acquired. Depending on how severe the ectasia (dilation of the veins) is, there are 4 degrees of gastric varicose veins:
- There are no clinical manifestations of the disease. The initial stage can only be established using endoscopic examination. In this case, the veins in the stomach are slightly dilated, in small areas on single vessels.
- The first signs of the disease appear, but they are so weak that it is impossible to suspect pathology. The blood vessels become tortuous, with alternating areas of swelling and narrowing.
- The patient's condition worsens. When performing an endoscopic or x-ray examination, pronounced ectasia is visible.
- Nodes are formed whose diameter exceeds the lumen of the vein by more than 1 cm. The affected vessels are thin and weak. This condition threatens not only a sharp deterioration in the patient’s health, but also his life.

Causes
With gastric varicose veins, the causes of the development of pathology are different, the main of which is an increase in pressure in the portal vein, which leads to the formation of ectasia.
Varicose veins of the stomach are a consequence of other diseases:
- liver pathologies (cirrhosis, hepatitis, echinococcosis, etc.);
- tuberculosis;
- polycystic disease;
- malignant or benign formations located in the area of the portal vein and causing its compression;
- fibrosis or sarcoidosis;
- aneurysms of arteries located in the liver or spleen;
- diseases gastrointestinal tract(eosinophilic gastroenteritis, intestinal obstruction);
- cardiovascular failure.
Provoking factors for the development of pathology include physical or mental stress, infectious diseases accompanied by a significant increase in body temperature.
Based on which signs and symptoms of varicose veins predominate, the doctor develops an individual treatment regimen. After all, pathological dilation of the veins can be localized not only in the stomach, but also spread to the vessels of the abdominal cavity or esophagus, provoking new symptoms.
Signs and symptoms of the disease
Varicose veins of the stomach have similar symptoms to pathologies of the gastrointestinal tract. The main ones are nausea and heartburn.
Specific signs appear only on late stages diseases. First of all, this is bleeding from varicose veins. It manifests itself in the form of vomiting mixed with blood, which is not accompanied by painful sensations. The stool takes on a black tint, which indicates bleeding in the upper gastrointestinal tract.
Fluid forms and begins to accumulate in the abdominal cavity, which leads to ascites.
In addition, pain appears in the heart area, heart rate increases, chest pain and shortness of breath, especially after physical or mental stress. A sharp decrease in blood pressure develops against the background of massive blood loss. In some cases, the patient's condition is complicated by hypovolemic shock.

Diagnostic measures
Gastric varicose veins are often accompanied by pathological dilation of the veins in the esophagus. Diagnosis of the disease includes establishing the cause that provoked the occurrence of phlebectasia. Depending on this, an individual therapeutic regimen is developed.
The diagnosis is established based on the patient’s complaints, examination results, laboratory and instrumental research methods.
The doctor does not always associate heartburn with the development of gastric varicose veins, therefore, if health complaints arise, you should undergo a comprehensive examination and not refuse even the most unpleasant tests.
Varicose veins lead to the accumulation of free fluid in the abdominal cavity, as evidenced by an enlarged belly.
Laboratory tests include general clinical examinations of blood, urine and feces.
The most precise method diagnostics varicose veins of the stomach is esophagogastroscopy, which makes it possible to visually assess the condition of the organ’s vessels, establish the presence of areas of pathological expansion, nodes and the exact location of bleeding. The study should be approached very responsibly so as not to provoke damage to thin vessels.
Based on the results of esophagogastroscopy, one can not only verify the presence of gastric varicose veins, but also establish the cause of the development of the pathology. This is evidenced by certain signs - combined damage to the vessels of the stomach and esophagus is a symptom of portal hypertension, selective stretching of individual sections of the vessels - about thrombosis of the splenic veins, etc.
From additional methods Research uses radiography with barium sulfate (x-ray contrast agent), which can be used to determine the functionality of the gastrointestinal tract.
Ultrasound examination will help determine damage to the abdominal organs.
Treatment methods for gastric varicose veins
Therapy for pathological dilatation of the gastric veins is selected individually for each person, depending on the symptoms present and the stage of the pathology.
Drug treatment
Used in the initial stages as the only method of treatment or in combination with surgical methods. With its help, you can stabilize the patient’s condition, prevent the progression of the disease and avoid complications.
Among medications, drugs are used that have the ability to reduce pressure in the blood vessels of the internal organs and the portal vein, strengthen the tone and elasticity of the walls, and also narrow the lumen.

Fixed assets:
- Vasopressin. It has a vasoconstrictor effect, reduces pressure in the portal vein of the liver. Thanks to this, overfilling of the organ’s blood vessels is eliminated and the patient’s condition is stabilized. The drug Vasopressin is intended for intravenous administration. Side effects cannot exclude the development of massive vasospasm, which threatens ischemia of the myocardium, brain and other important organs.
- Nitrates. Reduce Negative influence Vasopressin on peripheral vessels. Expands portal-systemic collaterals, thereby reducing pressure in the portal vein. It is used sublingually (under the tongue) or as a patch.
- Somatostatin. It has the ability to selectively affect the blood vessels of internal organs. Thanks to this, it normalizes pressure in the veins of the stomach and restores blood vessels.
In addition, collidal solutions, astringents, antacids and vitamins are widely used in the treatment of the disease.
Surgical intervention
It is used in the later stages of the disease, as well as in cases of massive bleeding from veins and nodes.
Intrahepatic shunting shows good results. The operation is performed under X-ray control. This creates a kind of bridge between the hepatic and portal veins, which makes it possible to reduce pressure and prevent its increase in the future.
If the cause of the development of gastric varicose veins is pathology of the spleen vessels, it is advisable to use splenorenal shunting. In this case, the veins of the spleen and left kidney are combined. A similar manipulation is also indicated to prevent bleeding.
One of the most common surgical methods The treatment of pathology is sclerotherapy. The essence of the procedure is the introduction of a special solution into the lumen of the vessel, which leads to soldering of the vein walls. To achieve the desired effect, the manipulation should be repeated several times - after 5 days, 1 and 3 months. One of the main disadvantages of this honey is the need for repeated sclerosis every 6-12 months.
Surgical treatment of varicose veins includes ligation of pathologically dilated vessels. For this purpose, a rubber bandage is used. The method is characterized by high efficiency and minimal risk of relapse.
Folk remedies
Alternative medicine is used in the composition complex treatment disease, however, before using any method, you should agree on its appropriateness with your doctor. Despite all the safety folk remedies have certain contraindications that must be taken into account.
Used in pathology therapy medicinal plants, having the ability to strengthen the walls of blood vessels, increase their tone and elasticity.
Basic recipes:
- Collection based on chestnut fruits. To prepare the medicine, you need to mix 100 g of chestnut fruit, oak and birch bark, blackberry roots and sweet-leaved astragalus, add 2 tbsp. l. horsetail and Icelandic moss. Grind all ingredients and mix, 2 tbsp. l. pour 0.5 l of mixture hot water, to put on water bath and boil for 5-10 minutes. Before use, strain the medicine and take 100 ml 3-4 times a day. The decoction reduces the permeability of blood vessels, stabilizes blood circulation and removes swelling.
- Rowan and rosehip berries. They have anti-edematous properties, strengthen the walls, increase their tone and elasticity. 2 tbsp. l. berries should be poured with 0.5 liters of boiling water, wrapped and left for 50-60 minutes. Take 100-150 ml of the product throughout the day.
Possible complications
Varicose veins of the stomach often lead to bleeding and iron deficiency anemia. This is due to the fact that the disease is diagnosed in late stages.
Progression leads to involvement in pathological process intestinal vessels. We must not forget that there is a risk of relapse, so even after surgical treatment Preventive measures should be taken for varicose veins.
Prevention
Prevention of the disease is that a person must lead a healthy lifestyle - exercise, organize a nutritious and balanced diet, and get rid of bad habits.
Food restrictions and diet
Diet plays an important role in disease prevention. Proper nutrition for gastric varicose veins will help not only prevent the development of pathology, but also slow down the progression of existing ectasia.
A person should exclude spicy, fried, fatty and salty foods from the menu, give up alcohol, coffee and strong tea. You should limit your consumption of confectionery and bakery products. When preparing dishes, use high-quality and natural products, do not use hot spices, raising agents, flavorings and other harmful ingredients.

To strengthen blood vessels, the patient’s diet must be complete and balanced. You need to eat food 4-5 times a day, in small portions.
IN daily diet Vegetable soups, okroshka, porridge, especially buckwheat, should be present. Have a positive effect on the gastrointestinal tract dairy products, mild varieties of hard cheese, fresh vegetables and fruits. Dishes must be cooked in vegetable oil.
Regular consumption of small amounts of fresh raspberries, aronia or red rowan, currants, and grapes will help improve blood circulation and prevent the progression of varicose veins.
Home » Causes of varicose veins
Varicose veins of the stomach and lower esophagus are a disease characterized by a violation of the outflow of blood from the veins of these organs and a change in their structure (vessels dilate, become unnaturally looping, long and form nodes).
Esophageal varices, gastric varices: causes
Typically, varicose veins in the area of the stomach and esophagus occur due to a phenomenon called portal hypertension (increased pressure in the portal vein system), of various etiologies. Normal pressure in that blood vessel in normal condition does not exceed 6 mmHg. When this indicator increases to 12–20 mmHg, there is a disturbance in the outflow of blood and dilation of the veins. Portal hypertension is a consequence of thrombosis or compression of the portal vein, cholelithiasis and certain diseases of the pancreas, stomach and liver, including:
- Cirrhosis and chronic hepatitis;
- Echinococcosis;
- Polycystic disease;
- Fibrosis, including congenital;
- Sarcoidosis;
- Malignant and benign neoplasms;
- Aneurysms of the arteries of the spleen and liver.

This disease can be congenital or appear at any period of life, regardless of age. As a result of impaired venous circulation due to listed diseases or for other reasons. Most often, the disease is a consequence of liver cirrhosis, since this pathology is characterized by changes in the structure of the organ, modification and proliferation of its tissues, which, as the disease progresses, first lead to a weakening and then a complete cessation of liver function.
Clinical picture of gastric varicose veins
At the beginning, the disease is practically asymptomatic, without causing any discomfort to the patient. Sometimes patients experience severe heartburn. This symptom, most often, goes unnoticed and does not serve as a reason to contact a doctor. But even a doctor does not always associate heartburn with varicose veins of the digestive system. Therefore, the disease develops further and is complicated by bleeding, which is manifested by the following symptoms:
- Ascites (accumulation of fluid in the abdominal cavity, which causes the abdomen to increase in size).
- Painless vomiting of blood, usually profusely.
- Tachycardia (strong heartbeat).
- Hypotension (low blood pressure).
- In especially severe cases - hypovolemic shock.

Diagnostic methods for identifying the disease
At the initial stages, pathology can only be identified using instrumental diagnostic methods. Patients may be prescribed x-rays with a contrast agent (barium sulfate). Most in an exact way To establish the disease is esophagogastroscopy (internal examination of the esophagus and stomach). The examination must be carried out very carefully, trying not to cause injury that could cause bleeding.
After dilated veins are identified, the examination must be continued to establish the causes of the pathology. Portal hypertension most often leads to combined damage to the veins of both the stomach and esophagus. When certain sections of the vessels are stretched, thrombosis of the splenic vein can be suspected. In rare cases, the cause of esophageal varices may lie in eosinophilic gastroenteritis. As a result of damage to the intestinal mucous membranes, inflammation spreads to the smooth muscles, then fibrosis (tissue proliferation) and intestinal obstruction occur.

Since the disease can be caused cancerous tumors, patients are often prescribed histological examination.
Main stages of treatment
Unfortunately, the disease is most often discovered as a result of internal bleeding, which can cause hypovolemic shock and even lead to death. In such cases, the patient requires emergency hospitalization and resuscitation measures. As soon as possible, you need to stop the bleeding and replenish the blood volume.
After the patient’s condition has been stabilized, the underlying disease is treated and procedures are aimed at reducing portal vein pressure and preventing bleeding.
Now the following basic methods are used to solve the problem:
- Sclerotherapy, which consists of endoscopic injection of an adhesive solution into the vessels of the stomach or esophagus. This procedure is repeated, depending on the severity of the disease, once a week or month, until a scar forms.
- Ligation of varicose veins using a rubber bandage. The method is more effective than sclerotherapy.
- Intrahepatic shunting. Reducing pressure by introducing a stent under X-ray control into the middle zone of the liver to connect the hepatic and portal veins.
- Splenorenal shunt. It is produced to prevent bleeding by combining the splenic vein and the vein of the left kidney using a shunt.
- Drug treatment - the use of vasoconstrictor drugs (Vasopressin), nitrates to reduce pressure in the portal vein (Nitroglycerin), as well as Somatostatin (or its analogue Octreotide) to reduce blood pressure in internal organs and narrow dilated blood vessels (taken for a long time).
Prevention of complications
To prevent life-threatening complications such as heavy gastric bleeding from varicose veins, hemorrhage into the esophagus and stomach, acute liver failure, as well as ascites, a special regimen is required.

For diseases leading to portal hypertension, a gentle diet is indicated. You need to eat small portions 4-6 times a day. You should not eat later than four hours before bedtime. Preference should be given to boiled or steamed foods. You should completely avoid foods that are too hot or cold. It is necessary to prevent spicy and sour foods from entering the esophagus.
It is necessary to avoid elevated physical activity, weights need to be rolled, but under no circumstances lifted. I'll have to give up going to the gym.
If problems with the liver occur, you should immediately consult a doctor who will prescribe treatment in the early stages of the disease. For high portal pressure, the use of beta blockers is recommended.
Phlebectasia or varicose veins of the stomach is a dangerous disease, which is manifested by an increase in the volume of the gastric veins and the occurrence of blood clots in them. The pathology is insidious due to the asymptomatic course of the initial stage. The disease is quite serious and therefore requires urgent treatment.
What are gastric varicose veins?

Dilatation of the veins of the mucous tissues of the stomach is not as common as varicose veins in the legs. The difference between pathologies lies in the reasons for their occurrence and progression. Often, increased portal vein pressure is the result of cirrhosis of the liver, although sometimes it is the result of genetic pathologies or compression of the portal vein by a large tumor.
In the stomach, varicose veins are divided into 4 stages of development:
- Symptoms do not appear, the dilation of the lumen of blood vessels is isolated, so the patient has no complaints. Only endoscopy can reveal this degree.
- Vein structures take on a tortuous and uneven shape. In this case, the increase does not exceed 3 mm, and the narrowing of the lumens occurs at small intervals. Bleeding at this stage is a rare occurrence. Pathology can be detected by x-ray or endoscopy.
- There is a noticeable narrowing of the lumen of the veins and their swelling. The stage is characterized by the presence of nodes and narrowing of the tone of the walls. The main signs are already appearing; it is only necessary to recognize them in a timely manner, since the threat of hemorrhage at this stage increases significantly. Transfer of therapy is prohibited.
- The nodes are noticeably visible, the lumens are narrowing, the gastric mucosa is thoroughly depleted. It is likely that a whole thread of damaged vessels will diverge from a large node. The vessels are thinned to such an extent that hemorrhage is likely to open at any time. If this happens, the patient is at risk.
It is important to highlight that the development of gastric varicose veins requires a significant period; for this reason, short-term compression of the veins by a neoplasm is not capable of provoking the occurrence of characteristic changes.
The disease is classified into the following types:
- acquired - appears in the event of an increase in pressure in the portal vein. This vessel performs the function of delivering blood to the liver. Difficulties are created by a disruption in the movement of blood through this organ. Pathology makes the veins soft, brittle, with every chance of rupturing at any moment;
- inherited - the disease is determined from birth. As a rule, the complex course of the period of bearing a child may be associated with a genetic predisposition.
Congenital varicose veins of the gastric veins are a rare phenomenon. Most often, doctors diagnose an acquired type of illness. The pathology mainly affects patients over 50 years of age.
Gastric varicose veins causes of development

Cirrhosis of the liver can cause varicose veins
The main factor contributing to the onset of the disease is portal hypertension, which causes enlargement of the veins in the digestive organ. Often, a similar condition is observed with cirrhosis of the liver due to the appearance of numerous scars on it. However, this is not the only condition for the occurrence of a dangerous disease. Other reasons causing the pathology:
- liver diseases that cause disruptions in blood flow;
- thrombus formation;
- compression of the portal vein by neoplasms;
- cardiovascular failure.
Particular care should be taken when diagnosing varicose veins in the stomach in patients affected by cirrhosis of the liver and hepatitis. This is due to greater vulnerability of organs and can end in disaster.
Symptoms of the disease and diagnosis
In the early stages, phlebectasia is asymptomatic, which creates difficulties in identifying the disease. Over time, the patient experiences the following signs of pathology:
- Heaviness and discomfort in the chest area.
- An increase in abdominal volume caused by the accumulation of fluid in the abdominal cavity.
- In the anterior lobe of the abdominal wall there is likely to be an outline of a “jellyfish head” - a pattern created by dilated veins.
- Difficulty breathing after physical activity.
- Increased heartburn not related to eating.
- Problems with the swallowing reflex.
It’s good when a person pays attention to these symptoms and consults a doctor. Diagnosis of the disease, due to the listed signs, will make it possible to carry out surgical measures aimed at treating phlebectasia. However, cases of visiting a doctor at this stage are rare. Typically, varicose veins of the gastric veins appear during rupture of blood vessels. At the beginning of hemorrhage, the pathology picture acquires the following signs:
- vomiting accompanied by bloody discharge (indicates the opening of hemorrhage in the stomach);
- drop in blood pressure;
- increased heart rate with irregularities;
- stomach ache;
- state of shock.

At the first symptoms of the disease, consult a doctor for examination
Bleeding may be small, although it is often profuse. It is necessary to start therapy urgently due to the fact that the pathology can worsen or result in the death of the patient.
Diagnosis of phlebectasia is carried out through endoscopy, as well as studies to detect coagulopathy. Varicose veins are identified using X-ray examination of the upper digestive system with the introduction of contrast and angiography.
Preference is given to endoscopy - it identifies veins affected by varicose veins, their volume and establishes hemorrhage in them. In patients with liver cirrhosis and phlebectasia, in 40% of cases they do not act as a source of hemorrhage. In such situations, bleeding is caused by erosions and bleeding of the gastric mucosa.
Endoscopy allows you to identify nodes with an increased risk of bleeding, even in the case of the confirmed presence of varicose veins. Due to the fact that the pathology occurs due to cirrhosis of the liver, it is necessary to find out possible problems with blood clotting. Laboratory tests include blood tests taking into account the number of platelets and characteristics of liver function.
Treatment of pathology
Since gastric varicose veins are not considered a self-occurring disease, there is no therapy for it. The use of certain medications makes it possible to reduce portal hypertension, so they are used comprehensively, exclusively as prescribed by the doctor.
If it is possible to eliminate the cause of hypertension, proper treatment or surgery is carried out; in most cases, the only cure is liver transplantation.
Drug treatment is carried out using the following means:
- Vasopressin - normalizes the condition of narrowed veins.
- Nitrates included in Nitroglycerin due to a decrease in pressure in the portal vein.
- Somatostatin or Octreotide - reduce blood pressure in internal organs.
Help is provided at the onset of hemorrhage, for which a Blackmore probe is inserted into the digestive tract, through which the veins are compressed and the bleeding stops. At the same time, treatment is given to increase blood clotting.
Phlebectasia becomes a severe exacerbation of portal hypertension due to the fact that at one stage or another it provokes the formation of gastrointestinal hemorrhage, accompanied by the loss of a large volume of blood and threatening life.
In parallel, assistance with bleeding still remains symptomatic, and complete therapy involves eliminating portal hypertension directly. This is not acceptable in every case; for this reason, the prevention of both portal hypertension and phlebectasis is of particular importance, because it turns out to be very difficult to overcome existing disorders.
Gastric varicose veins or phlebectasia is a serious pathology that requires urgent measures to be taken to solve the problem. The disease provokes protrusion of the walls of the stomach and an increase in the lumen. As a result, tortuosity is observed in the area of the vessels, and this requires proper treatment.
More about phlebectasia
The name of the problem speaks for itself - with varicose veins in the stomach or esophagus, their enlargement is observed, which leads to protrusion of the walls. Something like nodes appears on the vessels.
The disease can be of two types:
- Acquired - develops with increased pressure in the portal vein. This vein is responsible for supplying blood to the liver. This problem is caused by impaired blood flow through the liver. IN in this case the veins become tender, fragile and capable of breaking literally at any moment.
- Congenital – the disease is diagnosed from the moment of birth. Usually associated with a genetic predisposition, it can be triggered by a difficult pregnancy.
Congenital esophageal varices are rare. In most situations, doctors diagnose the acquired form of the disease. This is mainly a problem for patients over 50 years of age.
Varicose veins of the stomach - causes of the disease

The main reason for the development of gastric varicose veins is portal hypertension, which provokes swelling of the veins in the esophagus. Often this condition is observed with cirrhosis of the liver, as many scars appear on it. But this is not the only reason for the manifestation of an unpleasant disease.
There are other reasons that can cause the disease:
- Liver diseases that cause impaired blood flow.
- The appearance of blood clots.
- Compression of the rotary vein by tumors.
- Vascular and heart failure.
Particular attention should be paid to diagnosing the likelihood of venous disease in patients suffering from liver cirrhosis and hepatitis. Since these organs become even more vulnerable and untimely treatment can lead to negative consequences.
Signs of the disease
At the initial stage of the disease there are no specific symptoms. Therefore, it is difficult to determine the problem. But as the problem develops, the patient experiences certain signs of phlebectasia.
- Heaviness and discomfort in the chest.
- Enlarged abdomen due to accumulation of fluid in the abdominal cavity.
- A “jellyfish head,” as it is called, may appear in the anterior part of the abdominal wall. This is a pattern of veins dilated in the esophagus.
- Shortness of breath as a result of activity.
- Severe heartburn regardless of food intake.
- Swallowing dysfunction.

It’s great if the patient pays attention to the listed signs and consults a doctor. Diagnosis of the disease based on the listed symptoms will make it possible to take urgent measures to treat gastric varicose veins. But situations when patients come to the doctor at this stage are rare. Most often, phlebectasia manifests itself already at the moment of vein rupture. When bleeding begins, the signs of the problem become more pronounced.
- Vomiting with bloody discharge.
- Black stool, as well as noticeable admixtures of blood in it.
- Decreased blood pressure.
- Cardiopalmus.
- State of shock.
Bleeding from varicose veins can be minor, but most often it is massive. Treatment must be started immediately, as the problem can lead to serious deterioration or death.
The degree of varicose veins of the stomach and diagnosis of the disease

In total, there are four degrees of varicose veins of the stomach or esophagus.
- Degree 1– no symptoms are observed, venous ectasia is isolated, which does not prevent the patient from feeling great. The first degree of the disease can only be determined using endoscopy.
- Degree 2– vascular structures become tortuous and uneven. But at the same time, swelling does not exceed 3 mm, and the gaps narrow to insignificant distances. In this case, bleeding is rare. The problem can also be identified mainly using x-rays or endoscopy. Symptoms are not expressed.
- Degree 3– the venous lumen noticeably narrows, the veins bulge. At this stage, the nodes are clearly visible, the tone of the walls narrows. The main symptoms are already appearing; all that remains is to notice them in time, since the risk of bleeding at this stage of the disease increases markedly. Treatment cannot be delayed at the third stage.
- Degree 4– the nodes are clearly visible, the lumens are narrowed, the gastric mucosa is seriously thinned. A whole thread of affected vessels may diverge from a large node. All of them are so thin that bleeding can open at any moment. If this happens, the patient is in serious danger.
To diagnose venous disease and determine its degree, doctors use different research methods:
- Laboratory research blood, urine and feces.
- Ultrasound of the abdominal organs.
- Esophagoscopy.
- X-ray studies.
Treatment methods
For varicose veins of the esophagus or stomach, a competent approach is needed. After determining the degree of the disease, it is important to find the causes of the development of the pathology. The doctor prescribes the necessary medications to strengthen the liver and blood vessels. The patient is also advised to adhere to a diet and not give up physical activity.

Medicines for gastric varicose veins are mainly prescribed as follows:
- Drugs whose action is aimed at narrowing blood vessels and stopping bleeding.
- Colloidal solutions.
- Astringents.
- Antacids.
- Vitamins.
Conservative therapy with the prescription of medications is a long-term process. Considered more effective surgical intervention. Electrocoagulation of damaged vessels and squeezing them during bleeding, which is carried out using a special probe, helps to quickly improve the patient’s condition.
Unfortunately, no matter what treatment methods are attempted, it is impossible to cure the disease. Therefore, all measures are aimed exclusively at preventing further development pathology. In the first stages, maintaining the condition of the esophagus and stomach is much easier than in the third and fourth stages of the disease. And the appearance of bleeding further worsens the prognosis.
How to prevent the problem?

- From time to time you need to visit a doctor and undergo a routine examination.
- Do not lift heavy objects.
- Constantly take care of the proper functioning of the intestines.
Taking care of your own health consists of simple and understandable rules. But these recommendations will really help maintain the functioning of the gastrointestinal tract at the proper level and avoid many serious problems.
Garbuzenko D.V. Therapeutic tactics for bleeding from gastric varices // Annals of Surgical Hepatology - 2007. - T. 12, No. 1. - P. 96-103.
When citing an article, a link to the author is required!
Despite the fact that gastric varicose veins are a relatively rare pathology and occur in approximately 20% of patients with portal hypertension, the high mortality rate due to bleeding from them, as well as the lack of a uniform standard of treatment and preventive measures, makes the problem extremely relevant.
CLASSIFICATION OF GASTRIC VARICOSE VEINS
The most widespread classification of gastric varicose veins is based on their localization and connection with esophageal varicose veins. In addition, gastric varicose veins can be primary or secondary. In the latter case, they develop, as a rule, after endoscopic treatment.
Varicose veins that pass from the esophagus to the stomach are defined as gastroesophageal and are of two types:
1) gastroesophageal varicosities of the first type continue from varicose veins of the esophagus along the lesser curvature of the stomach 2-5 cm below the cardia;
2) gastroesophageal varices of the second type pass from the esophagus towards the fundus of the stomach.
Isolated gastric varices form in the absence of esophageal varices. Among them are:
1) isolated type 1 gastric varicose veins, which are located in the fundus of the stomach;
2) isolated type 2 gastric varicose veins, which are ectopic phlebectasias of the pylorus, antrum and body of the stomach. They are usually secondary.
The Japanese Society for the Study of Portal Hypertension classifies gastric varices according to color (white and blue), shape (straight, nodular and tortuous), presence of red color signs (RC0-3), localization (cardiac, fundal and varicosities occupying both sections) .
FORMATION MECHANISM
VARICOSE VEINS OF THE STOMACH
Gastroesophageal varicose veins, predominantly of the first type, are in most cases observed in patients with extrahepatic portal hypertension caused by impaired patency of the portal vein, less often in liver cirrhosis. The cause of isolated type 1 gastric varicose veins is often segmental (left-sided) portal hypertension, which develops as a result of thrombosis or narrowing of the splenic vein, usually against the background of pancreatic pathology.
Gastroesophageal varices of the first type, like varicose veins of the esophagus, drain predominantly through the left gastric and coronary veins. The term “coronary vein” refers to the anastomoses between the left and right gastric veins. The left gastric vein ascends along the lesser curvature of the stomach to the left into the lesser omentum to the esophageal opening of the diaphragm, where it communicates with the veins of the esophagus, and then, bending back down and to the right behind the omental bursa, flows into the portal vein or, when the blood flow changes its direction, into the azygos system veins. Isolated gastric varices are formed as a result of reversal of blood flow through the splenic, gastroepiploic and posterior gastric veins. In this case, the term “posterior gastric vein” refers to anastomoses between the left and short veins of the stomach. Isolated type 2 gastric varices are often combined with dilatation of the branches of the gastroepiploic veins. Varicose veins of the stomach, as a rule, are drained through spontaneous gastrorenal shunts, which are formed between the veins of the gastrosplenic vascular territory and the left renal vein, through the inferior phrenic or adrenal veins. A case of gastropericardial shunt formation with the participation of the posterior gastric vein is described.
Endoscopic treatment of esophageal varices often contributes to the development of secondary, predominantly isolated gastric varices. On the other hand, sclerotherapy of varicose veins of the esophagus, with the caudal direction of the drug flow, can achieve persistent eradication of gastroesophageal varicose veins, especially the first type.
DIAGNOSIS OF GASTRIC VARICOSE VEINS
AND RISK FACTORS FOR BLEEDING FROM THEM
Gastric varices are most often diagnosed during screening of patients with portal hypertension, being examined for the presence of varices, or in the case of gastric bleeding. However, standard endoscopic examination does not always allow an accurate assessment of the true prevalence of this pathology due to the deep location of dilated veins in the submucosa of the stomach and it can be difficult to distinguish them from folds. The quality of diagnosis can be improved through computed tomography and endoscopic ultrasonography.
However, information about the size and location of gastric varices and the presence of inflammatory changes in the gastric mucosa obtained during endoscopic examination is essential for assessing the danger hemorrhagic complications. In this case, risk factors for bleeding are large-nodular varicose veins blue color, its fundic localization, red spots on the gastric mucosa in combination with severe liver dysfunction.
It is believed that the leading mechanism contributing to the rupture of varicose veins is a combination of increased intraluminal pressure and weakness of the vessel wall. According to Laplace's law, the stress of the vascular wall (T) is proportional to the value of intravascular pressure (P), the diameter of the vessel (D) and inversely proportional to the thickness of its wall (W):
T=P*D/W
Although fundic varicosities are located in the submucosa, when large sizes they penetrate the muscular lamina of the gastric mucosa, pass through the lamina propria and protrude into the lumen of the stomach, becoming vulnerable to damage. In this case, the risk of their rupture increases sharply.
Due to the formation of spontaneous gastrorenal shunts, the indicators of the portohepatic pressure gradient in patients with gastric varices are lower than with esophageal varices, which is why most bleeding develops at values less than 12 mm Hg.
TREATMENT AND PREVENTIVE MEASURES
FOR BLEEDING
FROM VARICOSE VEINS OF THE STOMACH
Obturator probes play an important role in the complex of conservative measures to stop bleeding from gastric varices. For rupture of fundal and ectopic varicose veins, a Linton-Nachlas probe is used. In this case, hemostasis is achieved by inflating a single gastric balloon to 600 cm3. The Sengstaken-Blakemore triple-lumen probe is used in cases of rupture of esophageal varices or gastroesophageal varices. However, their effect is short-term and permanent hemostasis is observed in less than 50% of cases.
Pharmacotherapy
In contrast to esophageal varices, there is little data on the use of vasoactive drugs (analogues of vasopressin, somatostatin, nitroglycerin) for acute bleeding from gastric varices. However, given the similarity of formation and clinical course, it can be assumed that such treatment can be effective for gastroesophageal varicose veins of the first type. Antibiotic therapy should be carried out as early as possible, because It has been shown that the addition of a bacterial infection, especially in patients with liver cirrhosis, increases the incidence of complications and mortality, and with the use of cephalosporins, the short-term prognosis is significantly improved.
The role of non-selective β-blockers and nitrates in the primary prevention of bleeding from gastric varices and their relapses has not been fully established and requires further evaluation.
Endoscopic treatment
Standard endoscopic sclerotherapy for varicose veins of the esophagus and gastroesophageal varicose veins of the first type consists of injection of drugs that cause endothelial damage, thrombosis and subsequent sclerosis of varicose nodes, either directly into the dilated veins (5% ethanolamine oleate solution, 5% morruate solution sodium, 1.5-3% solution of sodium tetradecyl sulfate), and paravasally (1% solution of polidocanol (ethoxysclerol)). In order to obliterate gastric varicose veins, histoacryl (N-butyl-2-cyanoacrylate) is usually used. Administration of the drug in small doses through intravaricose injections leads to an instant polymerization reaction. When mixed with blood, it transforms from its natural liquid state into a solid state and blocks the lumen of the vein. This allows, in most cases, to quickly stop active bleeding from gastric varices. Despite the fact that the relapse rate reaches 40%, this method is more effective than standard endoscopic sclerotherapy and is currently considered not only as a “first-line” therapy for bleeding from fundic gastric varices, but also as a method of secondary prevention.
The most common and usually transient side effects of varicose vein obliteration with histoacryl are fever and mild abdominal pain. Severe complications are rare. These include embolism of the pulmonary artery and cerebral vessels, thrombosis of the portal and splenic veins, retroperitoneal abscess, and splenic infarction. The likelihood of developing embolism is higher in patients with large gastrorenal shunts and hepatopulmonary syndrome, which is characterized by arterial hypoxemia and intrapulmonary vascular dilatation with the presence of direct arteriovenous anastomoses, which facilitates the entry of the polymerizing substance into the systemic circulation. Therefore, in this category of patients, obliteration of varicose nodes with histoacryl should be avoided and replaced with sclerotherapy, for example, 5% ethanolamine oleate solution, combining it with vasopressin infusion, or resort to other treatment methods.
With endoscopic ligation, in contrast to the induction of chemical inflammation and thrombosis caused by the introduction of sclerosing agents, the elastic ring, capturing areas of the mucous and submucosal layer of the stomach in the area of varicose veins, leads to strangulation and subsequent fibrosis. However, in some cases, deep and extensive ulcers may form in the ligation area. Considering that the fundic gastric varices are usually large and directly connected to the significantly dilated left gastric or posterior gastric veins, the volume of blood flow through them is greater than through esophageal varices. In this regard, in areas of damaged gastric mucosa, bleeding often recurs, reducing the effectiveness of endoscopic ligation, compared with obliteration of varicose nodes with histoacryl, which is the “gold standard” of treatment in this situation.
Interventional radiology methods
In 1969, J. Rosh et al. put forward the idea of creating an intrahepatic fistula between the branches of the hepatic and portal veins for the treatment of portal hypertension. Currently, transjugular intrahepatic portosystemic shunt (TIPS) has received widespread clinical use. Its main advantage is that it is less invasive than with surgical methods decompression of the portal system.
There are few publications concerning the use of this method in patients with gastric varicose veins. It is indicated that in the vast majority of them, TIPS is effective both in cases of acute bleeding and when used for prophylactic purposes. Moreover, the relapse rate after achieving primary hemostasis is 15-30% within 1 year. Their cause in the long term, as a rule, is stenosis or occlusion of the shunt as a result of intimal hyperplasia of the area hepatic vein or thrombosis of the endoprosthesis due to low blood flow on it. This complication is observed in at least a third of patients and serves as an indication for re-intervention. Serious problem is post-shunt encephalopathy, which develops in 20-30% of cases and may be difficult to treat.
During the first year after the intervention, mortality varies from 10 to 50%, with the most common cause being sepsis, multi-organ systemic dysfunction, and recurrent bleeding. The prognosis is worse in patients with liver cirrhosis who are class C according to the Child-Pugh criteria. However, they are the main candidates for TIPS. Other unfavorable factors include high levels of serum bilirubin, creatinine, alanine aminotransferase, the presence of encephalopathy, and the viral nature of the disease.
The British Society of Gastroenterology recommended TIPS for patients with cirrhosis and gastric varices as a “second-line” treatment for acute bleeding, and for the prevention of recurrence in case of ineffective endoscopic measures. However, further research into the role of this method is necessary, especially when the portohepatic pressure gradient is less than 12 mmHg. and the presence of large gastrorenal shunts.
The balloon-occlusion retrograde transvenous obliteration (BRTO) method proposed by H. Kanagawa et al. in 1996 for the treatment of gastric varices, it is quite effective and safe and is a good alternative to TIPS. This intervention is technically feasible only in the presence of functioning gastrorenal shunts, which occur in almost 85% of patients with gastric varices. A sclerosing agent (usually a 5% solution of ethanolamine oleate with iopamidol) is inserted through a catheter with an inflatable balloon into the femoral or internal jugular vein, and then into the left adrenal vein through a gastrorenal shunt into the varicosities of the fundus of the stomach and the veins feeding them . To prevent leakage of sclerosant into the systemic circulation, small collaterals are embolized with microcoils.
For acute bleeding from gastric varices, BRTO is used both independently and in addition to endoscopic methods, increasing their efficiency. Hemostasis is achieved in almost 100% of patients with no relapses in within three years and a survival rate reaching 70%. BRTO is no less effective in preventing recurrent bleeding from gastric varices.
A potential concern is the development or progression of esophageal varices, which may be associated with increased portal pressure after this procedure. Other side effects include hemoglobinuria, abdominal pain, transient fever, pleural effusion, ascites, and temporary deterioration in liver biochemical parameters. Serious complications are rare. These primarily include pulmonary infarction, shock, and atrial fibrillation.
Another type of transcatheter embolotherapy is percutaneous endovascular obliteration of gastric varices. It consists of the transport introduction into the left gastric vein of a metal spiral or embolus made of Teflon felt, usually from a transhepatic or transsplenic access, which contributes to the separation of the esophageal-cardiac and portal-splenic vascular territories. This method has been noted to be highly effective in acute bleeding. However, due to the formation of new pathways of collateral blood flow, relapses often occur in the long term, which affects overall mortality. In this regard, it is proposed to combine percutaneous endovascular obliteration of gastric varicose veins with endoscopic sclerotherapy, or BRTO.
There are isolated reports of achieving stable hemostasis during bleeding from gastric varices in patients with segmental (left-sided) portal hypertension due to splenic vein thrombosis solely by embolization of the splenic artery with the installation of a Gianturco coil, or combining it with laparoscopic splenectomy.
Percutaneous transhepatic portal vein plasty with implantation of a self-expanding metal stent, described in 2001 by K. Yamakado et al., is used in patients with extrahepatic portal hypertension caused by stenosis or occlusion of the portal vein, both benign and malignant. A few publications indicate the effectiveness of this method as a preventive measure for gastric varicose veins.
Surgery
According to domestic authors, in the presence of bleeding from esophagogastric varices, the indication for urgent surgical intervention in patients with liver cirrhosis, classified according to the Child-Pugh criteria as class A and B, as well as with extrahepatic portal hypertension, is the ineffectiveness of conservative and endoscopic methods of hemostasis. In this case, the method of choice is the operation proposed by M. D. Patsiora (1959).
Surgical methods for preventing recurrence of variceal bleeding can be conditionally divided into shunting (various variants of portocaval anastomoses) and non-shunting (devascularizing operations of the esophagus and stomach, as well as other interventions not related to the diversion of portal blood into the inferior vena cava system). The latter do not impair liver function, however, they are mostly accompanied by a high frequency of recurrent bleeding. The most effective of them is the operation described in 1973 by M. Sugiura and S. Futagawa, which is a modification of the method of M. Hassab (1967). It requires both transthoracic and transabdominal access and includes transection and suturing of the esophagus in the lower third, extensive devascularization of the esophagus and stomach from the left inferior pulmonary vein to the upper half of the stomach, splenectomy, selective vagotomy and pyloroplasty. M. Tomikawa et al. investigated the effectiveness of this intervention in 42 patients with gastric varicose veins. In the absence of surgical mortality, the five-year survival rate was 76.2%. Persistent eradication of varicose veins was observed in all cases. However, it should be noted that similar unique results were not obtained by other clinics.
Operations associated with decompression of the portal system contribute to the reliable prevention of recurrence of variceal bleeding and consist of total, selective or partial shunting of blood from the portal to the inferior vena cava system. In the nearly 60 years since A.O. Whipple et al. performed direct portacaval shunting, questions about its feasibility have now been resolved. A significant drawback of the intervention is the total diversion of portal blood flow. Meanwhile, maintaining its constancy, as well as venous hypertension in the intestinal bed, is necessary to maintain normal metabolic processes in the liver. The consequence of this is progressive liver failure, which is accompanied by high postoperative mortality, and the resulting encephalopathy has a more severe course than the initial one. Despite the fact that various original modifications of the operation have been proposed, their results clinical application in most cases they turned out to be unsatisfactory.
W.D. Warren et al. in 1967 described a method that could minimize the complications inherent in total shunts. It consists of selective transsplenic decompression of esophagogastric varices through the creation of a distal splenorenal anastomosis. By reducing the pressure in the shunted section of the splenic vein, the operation effectively relieves the pressure on the gastrosplenial vascular area. However, more complex hemodynamic changes develop in the hepatoportal zone. Since portal pressure remains elevated even if its initial values decrease with decreased splenic blood flow, it is practically impossible to achieve long-term separation of the two high- and low-pressure venous systems through selective shunting. Hypertension in the portomesenteric zone after some time contributes to the formation of pronounced collateral circulation through the pancreas towards the low pressure area - the gastrosplenial vascular territory. This leads to a decrease in portal blood flow with a high probability of portal vein thrombosis. The development of the so-called “pancreatic siphon” between the portal and splenic veins worsens the results of the operation, primarily due to the progression of hepatic encephalopathy, the level of which in some cases is similar to total bypass surgery. Careful separation of collaterals makes it possible to avoid these undesirable consequences.
Partial bypass involves a side-to-side anastomosis through an H-shaped polytetrafluoroethylene graft with a diameter of 8 mm between the portal or superior mesenteric vein and the inferior vena cava. This makes it possible to achieve effective decompression of the portal system while maintaining adequate progradient blood flow. As a result, the risk of developing encephalopathy is significantly reduced, and the number of recurrent bleedings is comparable to total or selective bypass surgery.
However, the role of bypass operations in patients with gastric varices is currently not sufficiently assessed, especially in the presence of spontaneous gastrorenal anastomoses. The British Society of Gastroenterology suggests considering them as an alternative to TIPS, i.e. a “second-line” treatment measure for the prevention of recurrent bleeding from gastric varices when endoscopic methods of hemostasis are ineffective.
CONCLUSION
Treatment of patients with bleeding from gastric varices remains an important clinical problem that is far from being resolved. A number of optimistic techniques have not yet received widespread practical application. Thus, most of the described methods of interventional radiology are widespread mainly in Japan. At the world consensus conference in Baveno (Italy, 2005), dedicated to the methodology of diagnosis and therapy of portal hypertension, the following concept on this issue was defined. To treat acute bleeding and prevent their recurrence, obliteration of gastric varices with histoacryl (N-butyl-2-cyanoacrylate) is recommended. In addition, for the purpose of secondary prevention of bleeding from gastric varices, non-selective β-blockers can be used; in patients with type 2 gastroesophageal varices and isolated type 1 gastric varices, TIPS was performed; in patients with type 1 gastroesophageal varices, endoscopic ligation was performed. It was noted that further randomized controlled trials of each of the proposed methods are required to determine the optimal management of patients with gastric varices.
Gastric varicose veins are less common than other types of varicose veins. The main cause of the disease is portal hypertension. Portal vein carries blood from the stomach, intestines and spleen to the liver. By various reasons Blood flow in the vein becomes difficult and pressure rises. Gastric varicose veins develop in approximately 20% of such patients.
Symptoms
The process of pathological expansion of veins (varicose veins) can be sluggish or rapid. At first, nothing bothers the patient except heartburn, belching, rapid heartbeat. Then there is discomfort when swallowing, a squeezing feeling behind the sternum. The vein expands, the stomach responds with inflammation of the mucous layer. There may be blood in the stool. Small but regular bleeding causes anemia. Pallor and weakness are added.
At acute course the disease causes profuse bleeding without pain. Gastric juice acts on hemoglobin, changing the color of the blood.
Vomit " coffee grounds" - a sign that there is blood in the stomach. If there are scarlet clots in such vomit, vomiting of unchanged blood soon begins. These symptoms are life threatening. Immediate treatment in a hospital is required.
Causes
The following diseases can cause varicose veins of the stomach:

The disease is detected more often in the following categories of patients:
- men;
- patients aged 50 years and older;
- those who have diseases of the liver, stomach, heart, pancreas.
Patients suffering from cirrhosis are at risk. For them, the statistics are sad: only every tenth person can avoid the appearance of gastric varicose veins.
Diagnostics
The size and condition of the veins in this form of varicose veins can be assessed by esophagogastroduodenofibroscopy. This method has become the standard when it comes to diagnosing varicose veins of the stomach and esophagus.  The examination will help determine whether there is a risk of bleeding and when it may begin if major varicose veins or markers of high bleeding risk are of concern. Laboratory blood tests are needed to evaluate clotting disorders.
The examination will help determine whether there is a risk of bleeding and when it may begin if major varicose veins or markers of high bleeding risk are of concern. Laboratory blood tests are needed to evaluate clotting disorders.
To improve the quality of diagnosis, especially when gastric bleeding begins, endosonography, angiography, echo and Dopplerography are used.
Treatment
A therapist can suspect a disease by examining and interviewing the patient. Laboratory tests prescribed by the doctor will help not only confirm the disease, but also assess the extent of the damage. If varicose veins are detected, but there is no bleeding, it is necessary to establish in which organ the original disease is hidden. Then the disease that caused it is treated, and medications are prescribed to prevent the first bleeding.
When a patient arrives at the hospital with bleeding, stopping it is the first priority. Medicines that lower blood pressure are prescribed. The fight against blood loss and bleeding disorders begins. Only then is therapy prescribed for varicose veins, which will reduce the risk of vessel rupture. 
If there is a threat of repeated damage to the vessel, and the measures taken are not enough to completely stop the bleeding, endoscopic intervention or surgery is required.
Diet
The patient will help his body in the fight against gastric varicose veins if he eats right. The walls of blood vessels will become stronger, the veins will become more elastic, and excess fluid will drain away.
Overeating should be avoided. It is advisable to eat little and often, 4-6 times a day, the last time 3 hours before bedtime. To make the stomach more comfortable, food should not be hot or very cold. It is better to boil, bake or steam foods. 
Risks and forecasts
Gastric varicose veins are less likely to cause bleeding than esophageal veins. However, repeated bleeding is more common in the stomach than in the esophagus.
If varicose veins are diagnosed, bleeding is possible in a third of cases. Often, minor bleeding will stop on its own. However, without treatment, the disease will develop. After a year or two, recurrence of varicose veins is possible in 50-75% of patients in a more severe form.
Treatment is considered successful when the threat of bleeding is eliminated and varicose veins are minimized. To stop varicose veins, the patient must help the doctor: take medications, eat right, and do not lift heavy objects.
The disease remains important medical problem. But the main thing remains - the earlier gastric varicose veins are diagnosed, the easier it is to treat the patient.