Most clinicians believe that young children tolerate burns much worse than adults. General phenomena in their body develop with a smaller area of damage than in adults; mortality is high. Burns covering an area of 5-8% of the child's body surface cause signs of shock and require general treatment; over 20% are life-threatening. Meanwhile, the organization proper treatment and caring for a burned child is quite a difficult task.
Causes of more severe burns in children, as well as the difficulties associated with their treatment and care, are explained by some anatomical and physiological features childhood, characteristic of the first 5 years of life. At school age, children become more independent, more conscious, the body matures, and care becomes easier.
After a severe widespread burn, a child may remain irritable for a long time, bad dream, bedwetting, absent-mindedness and other disorders of the emotional-volitional and mental sphere.
Despite significant advances made in the treatment of burn victims, the number of children dying from complications of burn disease is still very high.
The outcome of a burn primarily depends on the extent and depth of the thermal injury. Children tolerate superficial burns relatively easily. If the burn does not exceed 70% of the body surface in size, the child usually recovers. The situation is completely different with deep third and fourth degree burns. In these cases, death can occur even in a relatively small area, and the younger the child, the more severe the burn disease and the less likely there is for a favorable outcome.
Anatomical and physiological features child's body, affecting the course of burns and complicating their treatment
Reasons that aggravate the severity of burns
- 1. Thinness of the skin, poor development of the protective keratinizing layer of the skin, poor resistance to the destructive effects of heat and electric current.
- 2. The relationship between the child’s body weight and its area is different from that of an adult skin, per the same unit of mass. A burn of 5% of the body surface in a child corresponds to a burn of 10% in an adult.
- 3. Different relationships between different body segments than in an adult. In a child, the head makes up 20%, in an adult - 9% of the body surface. Burns to the face and head are common in children. They have a severe course. The supply of skin available for borrowing and grafting is reduced since the head and face cannot be used as donor sites.
- 4. Incomplete growth, underdevelopment of some organs, weakness of compensatory and defense mechanisms. The child’s body is unable to cope with the increased demands that a burn causes, so an irreversible condition quickly develops. Noted increased sensitivity to certain medications, instability of thermoregulation, poor resistance to infection, a tendency to develop complications that are not typical for an adult.
- 5. Greater need for oxygen and proteins. Rapid onset of metabolic disorders and exhaustion.
- 6. Tendency to rapid development connective tissue. There is often excessive growth of scar tissue at the site of a healed burn. This scar is itchy and ulcerates easily.
Reasons that make caring for a child difficult
- 1. Helplessness of the child, the need for constant supervision, maintenance, and pedagogical influence.
- 2. Poor development of the saphenous vein network and difficulties associated with their puncture and transfusion treatment.
- 3. Large, not controlled by the intellect, physical activity child, leading to the pulling out of the probe, catheter, needle from the vein, and breakage of the plaster cast.
- 4. Good blood supply, looseness and tenderness of soft tissues, leading to the rapid development of edema when a bandage is applied to injured tissues. Swelling can cause compression of blood vessels and poor circulation in the parts of the limb located below the bandage.
- 5. The child’s inability to analyze his feelings and pinpoint what is bothering him. At the same time, a violent reaction to pain is typical.
- 6. The child’s negative attitude towards the need for treatment and hospital stay. The child is overwhelmed with fear and a desire to return to the familiar home environment of his mother.
- 7. The child’s inability to demonstrate volitional efforts to achieve a faster recovery - reluctance to eat unusual food, exercise therapeutic exercises, be in a forced position, etc.
- 8. Tendency to become infected with acute contagious childhood diseases infectious diseases requiring compliance with a special epidemiological regime.
- 9. Easy development complications from respiratory and digestive system in a sick child if the sanitary and hygienic diet in the department is not followed
- 7. Continued growth of the child's body. After the burn has healed, scars have a restraining effect on bone growth, cause the formation of secondary deformities in the joints and shortening of the limb.
Currently, deep burns covering an area of more than 30% of the body surface are considered critical for infants and toddlers; for older children - deep burns exceeding 40% of the body surface in size. The cause of death in the vast majority of children is infection, which causes general infection of the body and death even before plastic closure of the wounds becomes possible.
Burns in children. Kazantseva N.D. 1986
Refers to life-threatening injuries that result from local impact high temperatures on body tissue. Most common reason burns are caused by hot liquids (boiling water, tea, coffee) coming into contact with the skin. In second place is touching hot objects, in third place are flame burns.
Severe thermal damage leads primarily to direct cell damage due to coagulative necrosis of varying depth and extent.
Vasoactive substances are released, which lead to increased vascular permeability and loss of fluid, protein from vascular bed.
Rapidly developing fluid deficiency is aggravated by exudation through the wound surface and the formation of edema in the interstitial space. Further loss of fluid occurs through evaporation from the wound surface, imperceptible perspiration losses through the lungs, with tachypnea almost always occurring, and also due to loss through the gastrointestinal tract, the so-called third space.
All lost fluid leaves the vascular bed, and losses reach a maximum in the first three to four hours after the burn. They are often underestimated, especially in young children. After a moderate burn, the intravascular deficit is already 20-30% of the blood volume within an hour!
The severity of the burn is determined depending on the degree of damage and the percentage of the burn.
It should be borne in mind that the palmar surface of the victim makes up approximately 1% of the body surface. You can calculate the burn percentage using the rule of nines.
9% have:
- head and neck;
- breast;
- stomach;
- half of the back surface;
- one hip;
- one lower leg and foot.
In children, a more accurate calculation of the percentage of burn can be made using the Lund and Browder chart.
Depending on the depth of the lesion, degrees of thermal burns are distinguished.
- I degree is accompanied by skin hyperemia, moderate swelling, pain;
- II degree - there is a detachment of the epidermis (bubbles with clear liquid appear), severe pain;
- III A degree. The skin is not affected to its full depth (partial necrosis of the skin, elements of the dermis are preserved). It is characterized by:
— the germ layer of the skin is partially preserved,
— the burn bladder is filled with liquid with a yellowish tint;
— burn wound Pink colour, wet;
- decreased pain and tactile sensitivity; - III B degree. There is skin damage to the entire depth with the formation of a necrotic scab. At this degree:
- all layers of the skin are affected;
- a dense, gray-brown or brown scab with areas of white “pork” skin is formed;
— thrombosed vessels and fragments of the epidermis are visible;
- no pain sensitivity;
— burn blisters with hemorrhagic contents;
- IV degree. With this degree, not only the skin, but also the underlying tissues (muscles, tendons, joints) become dead.
A severe burn (more than 10% of the body surface) and subsequent changes are considered a burn disease, which is characterized by the development of shock, toxemia, and septicotoxemia.
Burn disease in children is more severe the younger the child is.
Clinical picture.
When more than 10% of the body surface is burned (in children under 3 years of age, 5% of the surface), burn shock develops. Hypovolemia, blood deposition, and decreased cardiac output. A decrease in CVP to zero indicates true hypovolemia, and an increase in the norm indicates relative hypovolemia, due to the weakness of the pumping function of the heart.
There are 3 degrees of burn shock:
First degree burn shock.
The child's condition is moderate. Drowsiness, pale skin, chills, and thirst are observed. Pulse satisfactorily filled, tachycardia, central venous pressure decreased. Compensated metabolic acidosis. Diuresis is sufficient.
Second degree burn shock.
The condition is serious. Conscious. The child is lethargic and sometimes excited. There is chills, severe pallor of the skin, and cyanosis. Severe tachycardia. BP is moderately reduced. Thirst is expressed, there may be vomiting. Metabolic acidosis. Hourly diuresis is reduced.
Burn shock III degree .
The child's condition is extremely serious. Consciousness is impaired or absent. Pronounced pallor, marbling of the skin, cyanosis. Shortness of breath, pulse may be undetermined or thread-like. Sharp tachycardia, muffled heart sounds. Blood pressure is reduced, body temperature is low-grade. Significant decrease in central venous pressure, increase peripheral resistance. Hourly diuresis is reduced to 2/3 - 1/2 of the age norm. Hemoconcentration and metabolic acidosis are noted.
To determine the severity of a burn injury, the damage index is determined, which is determined in this way: 1% burn of the I-II degree. - 1 unit, 1% burn III A - 2 units, 1% burn III B. — 3 units, 1% burn IV degree. — 4 units.
With a damage index of up to 10 units. — mild degree burn, 10-15 units - moderate degree, 15-30 units - severe degree, more than 30 units - very severe.
Treatment.
Emergency measures at the scene:
- Abundant skin washing or dousing cold water(at least 15 0 C) until the pain disappears or significantly decreases.
- Anesthesia. For moderate burns, analgesia is not given. narcotic analgesics with diazepam (seduxen) intramuscularly.
In case of severe burn injuries, pain is treated with narcotic analgesics - promedol 1% solution 0.1 ml/year. - Apply an aseptic bandage (for extensive burns, cover with a sterile sheet) moistened with a 0.5% solution of novocaine with furatsilin (1:5000) 1:1. Before applying a bandage, the location, area, and depth of skin damage is accurately determined.
- In case of severe burn, provide access to the vein and begin infusion therapy physical solution 20-30 ml/kg per hour.
- In the presence of shock, glucocorticoids are administered: prednisolone 2-5 mg/kg or hydrocortisone 5-10 mg/kg intravenously.
What not to do in case of burns:
- Ice should not be applied directly to the burn surface, as this can increase the area of tissue damage through frostbite;
- The burn surface should never be lubricated with substances containing fat (lard, Vaseline, sunflower oil);
- Also, you cannot apply various indifferent substances (ointments, powders, flour);
- When removing clothing, do not tear it off the burnt surface, but cut it with scissors;
- Do not touch the burn surface with your hands.
For burns respiratory tract smoke or hot air:
- Take the victim out of the enclosed space.
- Give the patient humidified 100% oxygen through a mask at a rate of 10-12 l/min.
- Patients with respiratory failure III Art. or with no breathing should be intubated and transferred to mechanical ventilation.
- If it comes clinical death conduct cardiopulmonary resuscitation.
- Anesthesia and infusion therapy listed above.
- For shock - glucocorticoids.
- For laryngo and bronchiospasm - 2.4% aminophylline at a rate of 2-4 mg/kg.
Treatment in a hospital in the first 24 hours.
For superficial burns of more than 40%, or deep burns of more than 20%, it is necessary to:
- Nasotracheal intubation and start mechanical ventilation;
- Access to the central vein;
- Place a tube in the stomach;
- Bladder catheterization;
- Monitor central hemodynamics and oxygen balance.
The goal of infusion therapy during shock is to restore plasma volume and basic vital functions. The calculation of the required fluid is made depending on age, body weight, and area of the burn. During infusion therapy, body weight should be monitored every 6 hours to avoid overhydration.
In the first 24 hours after injury, crystalloids are administered at the rate of 3-4 ml/kg per burn area (as a percentage). The first half is administered in the first 8 hours, the second in the next 16 hours.
If the serum albumin level is below 40 g/l or burn shock occurs. an infusion is prescribed colloidal solutions(albumin, fresh frozen plasma) 8 hours after injury. If on prehospital stage did not use hydroxyethyl starch, then they are prescribed in the hospital. Refortam or Stabizol is used at a dose of 4-8 ml/kg intravenously.
Adequate analgesia is indicated with a 1% solution of promedol at a dose of 0.1 ml per year of life, every 4 hours.
Carbon monoxide should be measured in all patients with inhalation burn injury. Such patients are given 100% oxygen until the level of carboxyhemoglobin in the blood decreases to 10%.
Stages of burn surface treatment:
- Clean the burn surface;
- Remove the walls of the bubbles;
- Treat the burn wound with sterile saline or antiseptic solutions;
- Blisters on the palms and soles are not opened;
- Lubricate the damaged surface with silver sulfadiosine cream or treat the surface with Levomekol or Levosin.
- Apply a sterile bandage.
- Antibiotic therapy is not prescribed for prophylactic purposes. If there are indications for prescribing, then they can be prescribed only after the child has been brought out of shock.
In conclusion, I would like to note that the treatment of burns I-II degrees. with an area of up to 2% in infants, and up to 4% in older children can be treated on an outpatient basis. If there are manifestations of shock, hospitalization with adequate pain relief and infusion therapy is required.
- a type of injury that occurs when tissue is damaged by physical and chemical factors(thermal energy, electricity, ionizing radiation, chemicals, etc.). The clinical picture of burns in children depends on the factor involved, the location, depth, and extent of tissue damage and includes local (pain, hyperemia, swelling, blistering) and general manifestations (shock). The main tasks of diagnosing burns in children are to determine the nature of the burn injury, the depth and area of damage, for which infrared thermography and measuring techniques are used. Treatment of burns in children requires anti-shock therapy, cleaning the burn surface, and applying bandages.

General information
Burns in children - thermal, chemical, electrical, radiation damage to the skin, mucous membranes and underlying tissues. Among the total number of people with burn injury, children make up 20–30%; Moreover, almost half of them are children under 3 years old. The mortality rate due to burns among children reaches 2-4%, in addition, about 35% of children remain disabled annually. The high prevalence of burns in the pediatric population, the tendency to develop burn disease and severe post-burn disorders make the prevention and treatment of burn injury in children a priority in pediatric surgery and traumatology.
The peculiarities of children's anatomy and physiology are such that the skin of children is thinner and more delicate than that of adults, has a developed circulatory and lymphatic network and, therefore, has greater thermal conductivity. This feature contributes to the fact that exposure to a chemical or physical agent, which in an adult causes only superficial damage to the skin, leads to a deep burn in a child. The helplessness of children during injury causes longer exposure to the damaging factor, which also contributes to the depth of tissue damage. In addition, the imperfection of compensatory and regulatory mechanisms in children can lead to the development of burn disease even with damage of 5-10%, and in infancy or with a deep burn - only 3-5% of the body surface. Thus, any burns in children are more severe than in adults, since in childhood disorders of blood circulation, metabolism, and the functioning of vital organs and systems occur more quickly.

Causes and classification of burns in children
Depending on the damaging agent, burns in children are divided into thermal, chemical, electrical and radiation. The occurrence of thermal burns in children in most cases is caused by skin contact with boiling water, steam, open fire, melted fat, or hot metal objects. Children early age Most often they are scalded with hot liquids (water, milk, tea, soup). Often, burns in children occur as a result of parental negligence, when they immerse the child in a bath that is too hot or leave them to warm up with heating pads for a long time. At school age, various pyrotechnic fun, lighting fires, “experiments” with flammable mixtures, etc. pose a particular danger to children. Such pranks with fire, as a rule, end in failure, since they often lead to extensive thermal burns. At thermal burns Children are usually affected integumentary tissues However, burns to the eyes, respiratory tract and digestive tract may also occur.
Chemical burns are less common and usually occur when household chemicals are not stored correctly and within the reach of children. Young children may accidentally spill acid or alkali on themselves, spill powdery substances, spray dangerous chemicals, or drink caustic liquids by mistake. When aggressive chemicals are ingested, a burn to the esophagus in children is combined with a burn to the oral cavity and respiratory tract.
The causes of electrical burns in young children are malfunction of electrical appliances, their improper storage and operation, the presence in the house of electrical outlets accessible to the child, and exposed exposed wires. Older children usually get electrical burns when playing near high-voltage lines, riding on the roofs of electric trains, or hiding in transformer boxes.
Radiation burns in children are most often associated with direct contact with the skin. sun rays over a long period of time. In general, thermal burns in children account for about 65-80% of cases, electrical burns - 11%, and other types - 10-15%.
Within the framework of this topic, the features of thermal burns in children will be considered.
Symptoms of thermal burns in children
Depending on the depth of tissue damage, thermal burns in children can be of four degrees.
First degree burn(epidermal burn) is characterized by superficial damage to the skin due to short-term or low-intensity exposure. Children experience local pain, hyperemia, swelling and a burning sensation. At the site of the burn, slight peeling of the epidermis may be observed; superficial burns in children heal in 3-5 days on their own, completely without a trace or with the formation of slight pigmentation.
Second degree burn(superficial dermal burn) occurs with complete necrosis of the epidermis, under which clear liquid accumulates, forming blisters. Swelling, pain and redness of the skin are more pronounced. After 2–3 days, the contents of the bubbles become thick and jelly-like. Healing and restoration of the skin lasts about 2 weeks. With second degree burns in children, the risk of infection of the burn wound increases.
Third degree burn(deep dermal burn) can be of two types: IIIa degree - with preservation of the basal layer of the skin and IIIb degree - with necrosis of the entire thickness of the skin and partially the subcutaneous layer. Third degree burns in children occur with the formation of dry or wet necrosis. Dry necrosis is a dense scab of brown or black color, insensitive to touch. Wet necrosis has the appearance of a yellowish-gray scab with a sharp swelling of the tissue in the burn area. After 7-14 days, the scab begins to be rejected, and the complete healing process is delayed for 1-2 months. Epithelization of the skin occurs due to the preserved germ layer. IIIb degree burns in children heal with the formation of rough, inelastic scars.
IV degree burn(subfascial burn) is characterized by damage and exposure of tissues lying deeper than the aponeurosis (muscles, tendons, blood vessels, nerves, bones and cartilage). Visually, with fourth degree burns, a dark brown or black scab is visible, through the cracks of which the affected deep tissues are visible. With such lesions, the burn process in children (wound cleansing, formation of granulations) proceeds slowly, local, primarily purulent, complications often develop - abscesses, phlegmons, arthritis. IV degree burns are accompanied by a rapid increase in secondary changes in tissues, progressive thrombosis, damage internal organs and may result in the death of the child.
Burns of I, II and IIIa degrees in children are regarded as superficial, burns of IIIb and IV degrees - as deep. In pediatrics, as a rule, a combination of burns occurs various degrees.
Burn disease in children
Except local phenomena, with burns in children, severe systemic reactions often develop, which are characterized as burn disease. During a burn disease, there are 4 periods - burn shock, acute burn toxemia, burn septicopyemia and recovery.
Burn shock lasts 1-3 days. In the first hours after receiving a burn, children are excited, react sharply to pain, and scream (erectile phase of shock). Chills, increased blood pressure, increased breathing, and tachycardia are noted. In severe shock, body temperature may drop. 2–6 hours after the burn, children enter the torpid phase of shock: the child is adynamic, inhibited, makes no complaints and practically does not react to the environment. The torpid phase is characterized by arterial hypotension, frequent thread-like pulse, severe pallor of the skin, severe thirst, oliguria or anuria, and in severe cases, vomiting “ coffee grounds"due to gastrointestinal bleeding. First degree burn shock develops in children with superficial damage to 15-20% of the body area; II degree – for burns of 20-60% of the body surface; III degree - more than 60% of the body area. Rapidly progressing burn shock leads to the death of the child on the first day.
At further development the period of burn shock is replaced by a phase of burn toxemia, the manifestations of which are caused by the entry of decay products from damaged tissues into the general bloodstream. At this time, children who have received burns may experience fever, delirium, convulsions, tachycardia, arrhythmia; in some cases coma. Against the background of toxemia, toxic myocarditis, hepatitis, acute erosive-ulcerative gastritis, secondary anemia, nephritis, and sometimes acute renal failure can develop. The duration of the period of burn toxemia is up to 10 days, after which, with deep or extensive burns in children, the septicotoxemia phase begins.
Burn septicotoxemia is characterized by the addition of a secondary infection and suppuration of the burn wound. General state children with burns remain severe; complications are possible in the form of otitis media, ulcerative stomatitis, lymphadenitis, pneumonia, bacteremia, burn sepsis and burn exhaustion. During the recovery phase, the processes of restoration of all vital functions and scarring of the burn surface predominate.
Diagnosis of burns in children
Diagnosis of burns in children is made on the basis of anamnesis and visual examination. To determine the area of a burn in young children, Lund-Browder tables are used, taking into account changes in area various parts bodies with age. For children over 15 years of age, the rule of nine is used, and for limited burns, the rule of the palm is used.
Children with burns need to have their hemoglobin and blood hematocrit examined. general analysis urine, biochemical analysis blood (electrolytes, total protein, albumin, urea, creatinine, etc.). In case of suppuration of a burn wound, the wound discharge is collected and bacteriologically inoculated for microflora.
It is mandatory (especially in case of electrical trauma in children) to be performed and repeated in the dynamics of the ECG. When chemical burn esophagus in children requires esophagoscopy (FGDS). If the respiratory tract is affected, bronchoscopy and lung radiography are required.
Treatment of burns in children
First aid for burns in children involves stopping the action of the thermal agent, freeing the affected area of skin from clothing and cooling it (by washing with water, an ice pack). To prevent shock at the prehospital stage, the child can be given analgesics.
IN medical institution Primary treatment of the burn surface, removal of foreign bodies and scraps of epidermis is carried out. Anti-shock measures for burns in children include adequate pain relief and sedation, infusion therapy, antibiotic therapy, and oxygen therapy. Children who have not received appropriate preventive vaccinations are given emergency immunization against tetanus.
Local treatment burns in children are carried out closed, open, mixed or surgically. With the closed method, the burn wound is covered with an aseptic bandage. For dressings, antiseptics (chlorhexidine, furatsilin), film-forming aerosols, ointments (ofloxacin + lidocaine, chloramphenicol + methyluracil, etc.) are used. enzyme preparations(chymotrypsin, streptokinase). Open way Treatment of burns in children involves the refusal to apply bandages and management of the patient under conditions of strict asepsis. It is possible to switch from a closed method to an open one to speed up the recovery process, or from an open to a closed one if an infection develops.
During the rehabilitation period, children with burns are prescribed exercise therapy, physiotherapy (Ural irradiation, laser therapy, magnetic laser therapy, ultrasound),
Prevention of burns in children, first of all, requires increased responsibility on the part of adults. A child should not be allowed to come into contact with fire, hot liquids, chemicals, electricity, etc. To do this, in a house where there are small children, safety measures must be provided (storing household chemicals in an inaccessible place, special plugs in sockets, hidden electrical wiring, etc.). d.). Constant supervision of children and a strict ban on touching dangerous objects are required.
Skin burn- injuries resulting from exposure to high temperatures: flame, boiling water, steam; electric current, chemical substance: acids or alkalis; ionizing radiation, i.e. radiation.
What is burn disease?
After a person has received a burn, the body begins to struggle with the damage. The immune system is activated, the fight against external infection and attempts to prevent those microbes that always live in us from “running wild” begin. The body puts all its efforts into restoring dead tissue, trying to get rid of dead cells that poison the body. Such a struggle unfolds not only at the site of the burn, but throughout the body as a whole. A very large load falls on the kidneys, heart, and blood vessels. There is not a single body that does not participate in this process. Burn disease is a very serious condition. A significant percentage of patients fail to survive this condition even with active use all modern medicines.
What complication can occur immediately after getting a burn?
With an extensive and deep burn, a condition occurs quite quickly, which in the medical literature is called shock. It is important to correctly understand what shock is.
Shock is fast developing condition, associated with damage to the body that disrupts normal blood flow. This disruption of the normal movement of blood in the vessels leads to a malfunction of all organs and systems. The person begins to die rapidly.
Burn shock can occur in children with a lesion area of 5% and is more severe the more younger age child.
Features of burns in young children
A child's skin cannot withstand the destructive effects of heat and electric current due to the thinness of the skin and the poor development of the protective keratinizing layer. This explains the ease of deep burns in children.
The relationship between the weight of a child and the area of the skin is such that the same weight unit accounts for twice the surface area of the skin than in adults. Therefore, a 5 percent burn in a child corresponds to a 10 percent burn in an adult. Due to incomplete growth, immaturity of some organs and imperfect immunity, it is difficult for a child’s body to cope with a burn injury.
Often burns lead to irreversible conditions. Thus, as a result of an extensive deep burn, a metabolic disorder may occur that will lead to the development of exhaustion.
After the burns heal, deep scars remain, which subsequently inhibit the growth of soft tissues and bones and contribute to the formation of deformities of the joints and limbs.
How to determine the area of the burn?
To determine the severity of a burn, both the depth of the burn and its area are important. The question arises: how to determine the area of the burn? There are two methods for determining the area of the burn. We are talking about the rule of “nines” and the rule of “palms”.
What is the palm rule?
The palm rule is a method of calculating the area of a burn based on the size of the victim’s palm along with the fingers. One such palm makes up 1% of the surface of the entire human body. Accordingly, by “covering” the surface of the burn with a person’s palm, the area of injury can be calculated quite accurately.
What is the rule of nines?
The surface of the human body can be divided into parts, the area of which is equal to 9% of the total body area.
Head, neck-9%
One upper limb-9%
One lower limb-9%
Posterior surface of the body - 18% (9%x2)
The front surface of the body is 18% (9%x2)
The area of the perineum is 1% of the body surface.
How to determine the depth of the burn?
1st degree redness and swelling of the skin.
2nd degree detachment of the epidermis with the formation of blisters. The bottom of the bladder is bright pink, very painful.
3rd degree A - damage to the skin up to the papillary layer. A thin light brown or whitish scab forms. Pain sensitivity is reduced.
3rd degree B - death of the entire thickness of the skin. The burns are represented by dense scabs, through which the pattern of thrombosed veins is visible.
Stage 4 - complete charring. There is no pain.
Superficial burns hurt, deep ones do not. It is imperative to inform the ambulance dispatcher which part of the body was damaged by the burn. This information will be enough for the dispatcher to understand the situation and send a team of the required profile.
Often there is a combination of thermal burns of the skin and respiratory tract. This is a very life-threatening situation. A burn of the upper respiratory tract can be suspected based on several signs.
Signs of thermal damage to the respiratory tract
presence of burns to the face, neck, upper chest.
coughing up black mucus.
Emergency first aid for thermal burns
Stop exposure to the traumatic factor. For any degree of burn, it is advisable to cool the body with cold water.
Remove clothing and, if possible, remove pieces of smoldering clothing. This must be done carefully so as not to damage the integrity of the skin. If the fabric is stuck to the body, there is no need to tear it off. It is best to cut off the clothes.
Cover the burn area with a clean cloth. You should not wash the surface of the burn with water of questionable purity, pierce the blisters, or touch the burn with your hands. If the burns are extensive, then you can wrap the victim in a clean, ironed sheet and wrap him in a blanket, since with extensive burns, patients’ thermoregulation is sharply impaired and they freeze.
Keep the wound cool by applying ice through a bandage.
Give any painkiller you have: “Analgin”, “Pentalgin”, “Nurofen”, you can inject “triad” intramuscularly.
If the injured child is conscious, it is advisable to give him any available drink in small sips every 5-10 minutes. It is advisable to give water mineral water or sweet tea.
What not to do!
Do not tear off melted liquids from the affected areas of the body. synthetic fabrics! This is an additional traumatic factor, which, moreover, can cause bleeding from a ruptured vessel during a superficial burn.
Do not clean the wound yourself and do not open blisters, even tense ones.
You should not leave jewelry or watches on burnt hands! Heated metal retains heat for a long time, which affects the body for a long time.
Do not give medications or drinks to the victim by mouth if he is unconscious! Liquid and pieces of tablets may enter the respiratory tract.
You cannot revive a patient by hitting him on the cheeks! You may not be aware of a head injury other than a burn.
The use of alcohol and alcohol-containing preparations to treat the burn surface is strictly prohibited. Do not use soda, starch, sour cream, soap or raw egg, as these substances will contaminate the exposed surface.
Never apply iodine or any other antiseptic to a burn of any degree. This will only worsen his condition.
After providing first aid, you should consult a doctor for further treatment. If you are concerned, the burn seems deep or extensive, call an ambulance immediately. For thermal burns that occupy 3 percent of the body surface in a child under 5 years of age and more than 5 percent in children over three years of age (we remind you that the palmar surface of the victim’s hand makes up 1 percent of the total area of his body), treatment in a hospital is required.
The need for treatment inpatient conditions determined not only by the extent, but by the depth of the burn and its location. For burns of limited areas (less than one percent), deep burns of the hands, feet, face, neck, joints and genitals, hospital treatment is necessary.
Most often, burns with a small area of damage are treated on an outpatient basis. In children, 2nd-3rd degree burns are treated closed, that is, by applying a sterile bandage, most often an ointment, daily. First degree burns are not treated with anything. For second degree burns, apply bandages with panthenol-based ointments, sea buckthorn oil or with calendula. If the blisters open on their own, the doctor may prescribe antibiotic ointments. In any case, treatment tactics are determined pediatrician, pediatric surgeon, combustiologist.
Chemical burns
Chemical burns are caused by caustic substances, which can be divided into acids (most often vinegar essence, preparations of hydrochloric, sulfuric, nitric acids) and alkalis (caustic soda, slaked lime, concentrated ammonia solution, ammonia and etc.)
Acids and alkalis are often taken orally, causing burns to the mucous membrane gastrointestinal tract(also called poisoning). They can also cause chemical burns to the skin.
Acids have a relatively superficial effect, because the protein coagulates to form a scab and this prevents deeper penetration. Alkalis do not coagulate proteins, dissolve fats and penetrate deeply, causing more severe damage.
The result of treatment depends exclusively on the timeliness of first aid.
Signs of a chemical skin burn
When the skin and mucous membranes are exposed to concentrated acids, a dry, dark brown or black, clearly defined scab quickly appears. A scab is a crust that looks like dried blood.
Under the influence of alkalis on the skin and mucous membranes, a moist gray-dirty scab appears without clear outlines. This burn resembles boiled meat.
Emergency first aid for a chemical burn
If we are talking about a chemical burn, it is necessary to wash the burned area of the body for several minutes.
It is advisable to let the water flow in a stream. The water jet should not have high pressure so as not to further injure body tissues.
It is better not to use heavily contaminated water, as it is a source of infection. Of course, each situation must be assessed adequately. If there is no choice, then wash the surface of the chemical burn with any water. It will no longer be about harm dirty water, but about saving the affected area.
The exceptions are burns:
Burn caused by hydrochloric acid. Upon contact of water and of hydrochloric acid a large amount of heat is generated, which can increase the severity of the burn. It is better to wash the burn area with a mild soap or soda solution.
A burn caused by quicklime should be treated only with a weak soap solution. Use water in in this case absolutely not possible.
A burn caused by exposure to phosphorus differs from a burn caused by an acid or alkali in that phosphorus flares up in the air and the burn becomes combined - thermal and chemical. It is better to immerse the burned part of the body in water and remove pieces of phosphorus under water.
After washing, apply a CLEAN, DRY bandage to the burn area. Call professional help.
What not to do!
Do not treat the burn surface with fats, oils, dyes, or ointments until examined by emergency medical personnel or before admission to the hospital! Firstly, it interferes with the examination of the patient. Secondly, these substances prevent excess heat from escaping from the surface of the burn and cause additional chemical irritation.
Do not treat the skin with alkali for an acid burn or with an acid for an alkali burn unless you have first rinsed it thoroughly with water! Chemical reaction the interaction of these substances will occur directly on the burned surface, causing additional injury from the heat generated. It's best to use plain water.
Indications for hospitalization: The indication for hospitalization is the presence of a chemical burn of any origin and area!
Ozhog.txt Last changes: 2013/04/23 12:39 (external change)
Most clinicians believe that young children tolerate burns much worse than adults. General phenomena in their body develop with a smaller area of damage than in adults; mortality is high. Burns covering an area of 5–8% of the child’s body surface cause signs of shock and require general treatment; over 20% are life-threatening.
Meanwhile, organizing proper treatment and care for a burned child- quite a difficult task.
The reasons for the more severe course of burns in children, as well as the difficulties associated with their treatment and care, are explained by some anatomical and physiological features of childhood, characteristic of the first 5 - 6 years of life. At school age, children become more independent, more conscious, the body matures, and care becomes easier.
After a severe widespread burn, a child may experience irritability, poor sleep, bedwetting, absent-mindedness and other emotional, volitional and mental disorders for a long time.
Despite significant advances made in the treatment of burnt victims, the number of children dying from complications is still very high.
The outcome of a burn primarily depends on the extent and depth of the thermal injury. Children tolerate superficial burns relatively easily. If the burn does not exceed 70% of the body surface in size, the child usually recovers. The situation is completely different with deep third and fourth degree burns. In these cases, death can occur even in a relatively small area, and the younger the child, the more severe the burn disease and the less likely there is for a favorable outcome.
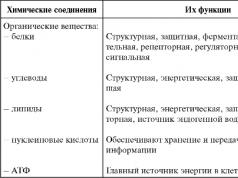
Anatomical and physiological characteristics of the child’s body that influence the course of burns and complicate their treatment
| Reasons that aggravate the severity of burns | Reasons that make caring for a child difficult |
| 1. Thinness of the skin, poor development of the protective keratinizing layer of the skin, poor resistance to the destructive effects of heat and electric current. | 1. Helplessness of the child, the need for constant supervision, maintenance, and pedagogical influence. |
| 2. The relationship between the child’s body weight and the area of his skin per one and the same unit of mass is different from that of an adult. A burn of 5% of the body surface in a child corresponds to a burn of 10% in an adult. | 2. Poor development of the network of subcutaneous veins and difficulties associated with their puncture and transfusion treatment. |
| 3. Different relationships between different body segments than in an adult. In a child, the head makes up 20%, in an adult - 9% of the body surface. Burns to the face and head are common in children. They have a severe course. The supply of skin available for borrowing and grafting is reduced since the head and face cannot be used as donor sites. | 3. Greater motor activity of the child, not controlled by the intellect, leading to the pulling out of the probe, catheter, needle from the vein, and breakage of the plaster cast. |
| 4. Incomplete growth, underdevelopment of some organs, weakness of compensatory and protective mechanisms. The child’s body is unable to cope with the increased demands that a burn causes, so an irreversible condition quickly develops. There is increased sensitivity to certain medications, instability of thermoregulation, poor resistance to infection, and a tendency to develop complications that are not typical for an adult. | 4. Good blood supply, looseness and tenderness of soft tissues, leading to the rapid development of edema when a bandage is applied to injured tissues. Swelling can cause compression of blood vessels and poor circulation in the parts of the limb located below the bandage. |
| 5. Greater need for oxygen and proteins. Rapid onset of metabolic disorders and exhaustion. | 5. The child’s inability to analyze his feelings and pinpoint what is bothering him. At the same time, a violent reaction to pain is typical. |
| 6. Tendency to rapid development of connective tissue. There is often excess growth of scar tissue at the site of a healed burn. This scar is itchy and ulcerates easily. | 6. The child’s negative attitude towards the need for treatment and hospital stay. The child is overwhelmed with fear and a desire to return to the familiar home environment of his mother. |
| 7. Continued growth of the child's body. After the burn has healed, scars have a restraining effect on bone growth, cause the formation of secondary deformations in the joints and shortening of the limb. | 7. The child’s inability to demonstrate volitional efforts to achieve a faster recovery - reluctance to eat unusual foods, do therapeutic exercises, be in a forced position, etc. |
| — | 8. Tendency to contract acute contagious childhood infectious diseases that require compliance with a special epidemiological regime. |
| — | 9. Mild development of complications from the respiratory and digestive system in a sick child if the sanitary and hygienic diet in the department is not observed. |
Currently, deep burns covering an area of more than 30% of the body surface are considered critical for infants and toddlers; for older children - deep burns exceeding 40% of the body surface in size.
The cause of death in the vast majority of children is infection, which causes general infection of the body and death even before plastic closure of the wounds becomes possible.
“Burns in children”, N.D. Kazantseva