· Introduce drugs according to medical prescription.
Ensure compliance treatment dose and frequency of use.
· Carry out individual dosing.
· Consider the method of administration.
· Respect the injection time.
Associate with food intake.
Teaching the patient how to take medicines
1. Motivate the patient to perform correctly drug treatment using the rules of bioethics, deontology.
2. Find out possible reaction body for certain drugs.
3. List everyone medicines prescribed by the doctor.
4. Add to the list of medicines home first aid kit which the patient receives without medical prescription.
5. Add to list herbal remedies: vitamin and mineral supplements, decoctions, herbal teas.
6. Mark drugs to be taken in the list, for example:
in the morning - the letter "U",
In the afternoon - "D",
in the evening - "B",
and also group medicines depending on food intake:
· while eating;
· after meal;
· before bedtime.
7. Write special features for each drug (for example, tablet shape, size, color, inscriptions on it).
8. Note the features of the administration of medicines (sublingually, intranasally, rectally),
9. Determine the rules for taking each drug, for example: how to drink the medicine, how much liquid, what products to combine with.
10. Pay attention to symptoms that may appear during treatment: dizziness, weakness, diarrhea or constipation, rash, arrhythmia, difficulty breathing.
11. Write down the phone number of the attending physician and emergency services.
The nurse should be aware that the patient and his relatives have the right to information about the drugs prescribed by the doctor, and to refuse to administer them.
A nurse does not have the right to dispense medicines at the request of patients, without a doctor's prescription, with the exception of heart remedies (validol, nitroglycerin) and sedative drops. If the patient refuses to take the medicine, the nurse should try to persuade him, convince or invite the doctor.
Rules for the distribution of medicines for enteral use
OBJECTIVE: Prepare medicines for distribution and intake by patients.
INDICATIONS: Doctor's appointment.
CONTRAINDICATIONS: They are revealed during the examination of the patient by a doctor or nurse.
EQUIPMENT:
1. Appointment sheets.
2. Medicines for internal use.
3. Mobile table for the day of the layout of medicines,
4. Container with boiled water,
5. Beakers, pipettes (separately for each bottle with drops).
6. Scissors.
PATIENT PREPARATION:
1. Inform the patient about the prescribed drug, its effect, therapeutic effect, a possible side complication.
2. Get consent.
METHODS OF DISTRIBUTION OF MEDICINES
INDIVIDUAL
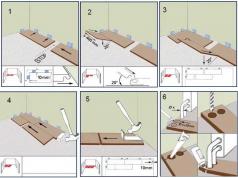
Place the lek on the mobile table. substances, pipettes, beakers, scissors, a carafe of water, prescription sheets.
1. Wash your hands and dry them dry.
2. As you pass from patient to patient, distribute the medicine. substances directly at the patient's bedside according to the prescription sheet (m / s must carefully read the name of the drug, its dosage on the package, pay attention to the expiration date).
3. Giving lek. means to the patient, warn him about the features of this remedy: bitter taste, pungent odor, discoloration of urine or feces after ingestion.
4. The patient must take the lek. substance in your presence.
Squeeze the package of foil or paper tablets into a beaker, and carefully place the tablets from the vial into a spoon. Liquid lek. means should be mixed thoroughly.
ADVANTAGES OF THIS DRUG DISTRIBUTION METHOD:
1. The nurse controls the intake of lek. substances.
2. The nurse can answer the patient's questions about the prescribed medication. means.
3. Eliminated errors in the distribution of lek. funds.
POST
In order to save time, the nurse lays out the lek in advance. funds in trays divided into cells In each cell, the full name of the patient and the number of the ward.
ALGORITHM
1. Wash your hands and dry them dry.
2. Read the prescription sheet carefully
3. Read carefully the name of the lek. means and dosage on the package, check it with the prescription sheet.
4. Pay attention to the expiration date of the lek. facilities.
5. Lay out the lek. funds for the cells for each patient at one time.
6. Spread the tray with lek. funds in the wards (do not leave drugs on the bedside tables at the patient's bedside if the patient is not in the ward, with the exception of validol, nitroglycerin).
7. Make sure that the patient takes the lek. funds in your presence.
8. Process used beakers and pipettes in accordance with the requirements of the SanPiN regime.
DISADVANTAGES OF THIS DRUG DISTRIBUTION METHOD
1. Lack of control over the intake of lek. funds by the patient (patients forget to take, throw them away, take them late).
2. The individual scheme of reception and distribution is not observed (before meals, during meals, after meals, etc.).
3. Errors are possible during distribution (due to the carelessness of the nurse, medicines may fall into another cell).
4. It is difficult to answer the patient's questions about the medications prescribed to him, because they are in the tray without pharmacy packaging.
Eye drops
Wash your hands, tilt your head back, pull back your lower eyelid and look up. Drip eye drops into the pocket located between the lower eyelid and the eye. Do not apply eye drops directly to the cornea or touch the surface of the eye with the dropper. This can infect the remaining drops. Close your eye and gently remove excess with a tissue. eye drops from eyelashes or eyelids.
Drops in the ear
Tilt your head so that sore ear was on top. Straighten ear canal by pulling the earlobe down and back. Then drip the required number of drops into the ear. Try not to touch the walls of the auditory canal with a pipette to avoid infection. Keep your head tilted back for a few minutes to medicinal substance leaked into the ear.
Rectal suppositories
Wear rubber gloves before inserting the rectal suppository. For easier insertion, treat the anus with a lubricant such as petroleum jelly.
Lie on your side and enter rectal suppository with the pointed end as deep as possible into the rectum. Move the base of the rectal suppository to the side to make sure it is in contact with the intestinal wall. If you are unable to insert the rectal suppository, you may not insert it as deeply. It is desirable to move the buttocks together for a short time after the insertion of the rectal suppository.
Vaginal preparations
Most vaginal medications, such as those used to treat a yeast infection, come in the form of creams, gels, foams, and suppositories. Wash your hands before and after using the vaginal preparation. Part the labia and inject the drug as directed, usually a few centimeters into the vagina. After that, do not insert a swab, as it absorbs some of the medicine. Use a pad to help protect your clothing from escaping medication.
Local preparations
Creams, gels, ointments, and sprays that you apply directly to your skin can deliver medicine directly to the right place. Wash your hands before and after using the drug. For creams, gels and ointments, apply appropriate amount to the center of the affected area and rub into a thin layer. When using the spray, shake the can and spray from a distance of at least 10 centimeters from the skin, unless otherwise directed.
As with other forms of medicine, follow the principle - "more is not better." In fact, an overdose of some local preparations, such as glucocorticoid cream, may cause general action on your body and lead to the development of severe side effects.
Skin patches
One of the newer methods of drug delivery is patches attached to the skin. Skin patches can contain substances ranging from fentanyl, which helps relieve severe pain, to estrogen, which helps hide menopausal symptoms. The skin patch creates a constant "stream" of the drug until it runs out.
Your doctor will tell you where to attach the skin patch and when to change it. You can also read this information on the instructions that come with the medicine. To avoid skin irritation, change the place of application of the skin patch. If you still experience irritation, tell your doctor. Do not remove the patch until your doctor tells you to do so. Also, follow your doctor's advice on how to throw away the skin patch. It's usually best to fold it in half right side up.
Title Memo to safe use medicines
_Author
_Keywords
At present, it is rare to find a person who, at least occasionally, but did not take medications. But "ideal" drugs, as we know, do not yet exist. All of them, to a greater or lesser extent, have adverse effects that can adversely affect the health of the patient. But what to do if you can not do without medicine? How to make taking the medicine as minimally dangerous as possible? National Institute on Aging U. S. Department of Health and Human Services Public Health Service National Institutes of Health offer a simple enough reminder for the patient, which in many cases will minimize the risk to health when taking new drugs.
Here is a list of questions to ask the doctor who prescribes you a new drug.
- What is the name of the medicine and why should I take it?
- How does it sound generic name drugs and under what name is it still produced by other companies?
- What diseases are treated with this medicine?
- How does this medicine work?
- How long does its effect last?
- How often should it be taken?
- How can I be sure this medicine is working?
- How will I feel when I first take this medicine?
- When (in relation to time of day and food intake) should I take the medicine, how much and how many times?
- What should I do if I accidentally missed the time of taking the medicine, for example, what should I do?
- What adverse effects should I expect from this medication? Should I tell my doctor about them? How can I minimize the chance of these effects occurring?
- How long should I take the medicine?
- What should I do if I see that the medicine is not working?
- Does this medicine interact with other drugs, including plant origin as well as food and food additives which I currently also use.
- When taking medication, should I avoid:
- driving?
- drinking alcohol?
- eating certain types of food?
- taking certain medications?
- Are there any other regimen, diet or lifestyle restrictions that should be observed while taking the medication?
- Should treatment with this medicine be supplemented with another or other medicines?
- How (under what conditions) should the medicine be stored?
- If I don't take the medicine, is there anything else that works in a similar way to this medicine?
National Institute on Aging U.S. Department of Health and Human Services Public Health Service
National Institutes of Health -
Antibiotics
Remember! Antibiotics do not affect viruses and are therefore useless in the treatment of diseases caused by viruses (for example, influenza, hepatitis A, B, C, chicken pox, herpes, rubella, measles). Do not forget to read the instructions carefully (note that when long-term use an antibiotic is used with an antifungal drug, nystatin).
Antibiotics used to prevent and treat inflammatory processes caused by bacterial microflora. A huge variety of antibiotics and their effects on the human body was the reason for the division of antibiotics into groups.
According to the nature of the effect on bacterial cells, antibiotics are divided into 3 groups:
1. bactericidal antibiotics(bacteria die but remain physically present in the medium)
2. bacteriostatic antibiotics(bacteria are alive but unable to reproduce)
3. bacteriolytic antibiotics(bacteria die and bacterial cell walls collapse)
According to their chemical structure, antibiotics are divided into the following groups:
1. Beta lactam antibiotics, which in turn are divided into 2 subgroups:
Penicillins - produced by colonies of the fungus Penicillinum
Cephalosporins - have a similar structure to penicillins. Used against penicillin-resistant bacteria.
2. macrolides(bacteriostatic action, i.e. the death of microorganisms does not occur, but only a cessation of their growth and reproduction is observed) - antibiotics with a complex cyclic structure.
3. Tetracyclines(bacteriostatic action) - used to treat respiratory infections and urinary tract, treatment of severe infections such as anthrax, tularemia, brucellosis.
4. Aminoglycosides(bactericidal action - characterized by the fact that under the influence of an antibiotic, the death of microorganisms occurs. Achieving a bactericidal effect is especially important in the treatment of debilitated patients) - have high toxicity. Used to treat severe infections such as blood poisoning or peritonitis.
5. Levomycetins(bactericidal action) - use is limited due to the increased risk of serious complications - lesions bone marrow that produces blood cells.
6. Glycopeptides- disrupt the synthesis of the bacterial cell wall. They have a bactericidal effect, but against enterococci, some streptococci and staphylococci, they act bacteriostatically.
7. Lincosamides- have a bacteriostatic effect, which is due to the inhibition of protein synthesis by ribosomes. In high concentrations against highly sensitive microorganisms may have a bactericidal effect.
8. Antifungal antibiotics(lytic action - destructive action on cell membranes) - destroy the membrane of fungal cells and cause their death. Antifungal antibiotics are gradually being replaced by highly effective synthetic antifungal drugs.
Antishock and anti-inflammatory drugs
The most common remedy from this series is analgin, but it should be borne in mind that it has a rather weak and short-lived effect. It is better to use ketonal (ketoprofen), which is comparable in strength to analgin, but is more harmless (1-2 times per ampoule, maximum 3 times per day).
Even stronger in the action of ketans (ketorolac), it is administered up to 3 ampoules per day, but not more than 5 days, due to the risk of gastrointestinal bleeding.
Local anesthetics
The use of these drugs is the best option in the treatment of serious injuries. Anesthetics such as lidocaine and bupivacaine last the longest (novocaine can be omitted, as it is more weak drug duration of action).
Remember! Some people may be allergic to local anesthetics. If a person was treated by a dentist and no problems arose during treatment, then most likely there should not be an allergy.
If a man has spent enough in the cold long time, then for its warming, as a rule, they use means that stimulate breathing and heart contractions - caffeine, cordiamine, sulfocamphocaine and others. However, if possible, it is better to limit or even eliminate their use, as they bring too much harm to the body.
RULES FOR TAKE MEDICINES -
KEY TO SUCCESSFUL TREATMENT.
Efficiency drug therapy largely depends on how the intake of drugs is connected with the intake of food, its composition. Most instructions tell you to take this drug before or after a meal. Unless otherwise indicated, the drug is taken on an empty stomach. Fasting is considered the use of the drug at least 60 minutes before a meal or 2 hours after a meal. What we drink medicines with is very important point because, this or that liquid (milk, juice of various fruits, mineral water etc.) reacts with the drug, sometimes with the formation of insoluble complexes, destroying (modifying) the active drug substance. The drug appears to be ineffective. The conditions for taking the drug (before or after eating, chewing or not, what to drink, what to dilute, whether it is necessary to treat the oral cavity after taking the medicine, etc.) should be indicated in the instructions for the drug in the section "Method of application and doses".
Order of the Ministry of Health of the Russian Federation of March 26, 2001 N 88 approved the Industry Standard "State Information Standard medicinal product. Basic provisions" 91500.05.0002-2001, in section 02.04.02 "Instructions for the use of the medicinal product", which states that the instructions for the use of the medicinal product are divided into the following categories:
Instructions for use of the medicinal product for specialists;
Instructions for use of the medicinal product for consumers (leaflet).
Instructions for use of the medicinal product for consumers (leaflet) - official document, intended for the patient and containing the information necessary for the correct independent application medicinal product.
IN guidelines dated December 7, 2009 "Preparation of the text of instructions for medical use medicinal product” sets out the basic requirements for the construction and presentation of instruction texts. Are given additional terms, which must be followed when using the drug: the time of application, the ratio with food intake ("before meals" 30 - 60 minutes before the start of a meal, "during the meal" - the period of direct food intake for 30 minutes before it starts, or after its completion, "after a meal" - a period within 30 - 120 minutes after a meal, "on an empty stomach" - not less than 60 minutes before the start of a meal and not earlier than 120 minutes after it ends), the need adherence to a special diet, dose titration, the patient's actions in case of missing the next dose.
In the absence of any instructions in the package insert, the medicine should be taken 30 minutes before meals. This applies to most drugs.
Any Chemical substance- this is a foreign compound, which, if we are talking about a medicine, should be absorbed in the human body with the greatest benefit for its health. Meanwhile, following the rules of administration can greatly, if not decisively, affect the effect of the drug.
If multiple medical preparations must be taken separately. Even the most harmless drugs for the body, while taking several drugs, will put a lot of stress on the stomach and liver. In addition, no one will ever say how, under the influence of the individual environment of the stomach of each person, several medications taken at the same time will behave. Will they cause the formation of toxic agents in the stomach. Therefore, the intake of medicines must be diluted in time so that the interval between doses is at least 15-30 minutes.
What to drink?
It is best, if there are no special instructions, to drink plain boiled water. Water is a good solvent and does not affect the active substance.
You shouldn't take medication milk, because the effectiveness of drugs similar in structure to proteins decreases - cardiac glycosides, caffeine, antiulcer drugs. Enzymes should not be taken with milk. Antibiotics are not recommended to be combined with dairy products. Sometimes in the annotation to the drug you can find a direct mention of the inadmissibility of drinking milk.
It has been established that iron preparations cannot be taken together with milk and products with a high content of oxalic acid and tannins (strong tea, coffee, spinach, blueberries).
Calcium supplements should not be taken with milk, sparkling water, combined with foods rich in fat.
Do not take medications and tea. Tea contains tannin, which forms insoluble compounds with nitrogen-containing agents.
Separately, it should be said about the simultaneous reception drugs and alcohol . This should not be categorical. Practice shows that it is with such a combination that the most severe complications. For example, with long-term nonsteroidal drugs and alcoholic beverages damage the gastric mucosa and an ulcer can form. A antibiotics, when taken simultaneously with alcohol, not only lose half their medicinal properties, but they can also form chemical compounds harmful to the body.
Is it important - on an empty stomach, before meals, after? Usually accepted:
- On an empty stomach: tinctures, infusions, decoctions and similar herbal preparations.
- Before meals : diuretics;; sulfa drugs are recommended to be washed down with alkaline drinks, for example, mineral water during treatment should be excluded food products containing sulfur (eggs, beans, tomatoes, liver); calcium gluconate (avoid foods containing oxalic, acetic and fatty acids).
- Half an hour before meals: acid-reducing agents gastric juice(antacids and choleretic agents); antiulcer drugs, antiarrhythmic drugs;
- While eating: gastric juice preparations or digestive enzymes because they help the stomach digest food; water soluble vitamins(C and group B).
- After meal
: painkillers(non-steroidal) anti-inflammatory drugs; fat soluble vitamins(A, D, E, K), complex multivitamin preparations; drugs that are components of bile, cardiac glycosides (in this case, it is recommended to grind the tablets, drink with starchy mucus, exclude protein food); calcium chloride
- Regardless of food
:bronchodilators; drugs that improve cerebral circulation.
- don't have their time medications prescribed under the tongue».
Take your medicines at regular intervals. Hormonal And " heart medications, majority antibiotics should be taken strictly by the clock.
If the instructions say " three times a day”, this does not mean at all: breakfast - lunch - dinner. The medicine must be taken every eight hours so that its concentration in the blood is evenly maintained. Even at night it is necessary to take medicines.
Treatment must be completed. This is especially true for antibiotic treatment. In no case should you stop taking antibiotics, even if the symptoms of the disease have decreased or disappeared. Indeed, during the treatment with these drugs, the weakest microorganisms die first, then the more resistant ones, and at the very end, all the rest. If the full course of treatment is not carried out, then the most resistant microorganisms will survive, adapt to these drugs, and in subsequent diseases they will no longer be sensitive to this antibiotic, or sensitive, but to a higher, not harmless to the body, dose.
Expired medicines are not allowed. The least that will come from this is the ineffectiveness of treatment, and the biggest - irreparable harm to health. After all, when the expiration date expires, the reaction of drugs, when they enter the human body, may differ for the worse from that provided for by the instructions. The same applies to drugs that stored incorrectly (temperature, humidity, light warnings were not observed).
KGKUZ "Center for Quality Control and Certification
medicines"
Khabarovsk, st. Sovetskaya, 34