Pericoronitis can occur at any age, but in 60-80% of cases it is observed with the appearance of lower wisdom teeth - third molars (eighth teeth in a row), which erupt at 14-25 years of age.
The cause of pericoronitis is the proliferation of conditionally pathogenic microorganisms (streptococci, staphylococci, anaerobic bacteria) in the gingival pocket under the overhanging mucous membrane.
The main factors that complicate the process of wisdom teeth eruption:
- abnormal localization of the tooth or its roots;
- thickening of the walls of the dental sac surrounding the crown or the mucous membrane of the gums;
- lack of free space for the tooth, leading to the fact that it either remains in the jaw branch or erupts in a non-physiological direction (buccal, lingual, towards the adjacent tooth).
These prerequisites lead to the fact that a mucoperiosteal “hood” hangs completely or partially over the crown of the tooth. Infectious agents, food debris and plaque accumulate under it. This starts the inflammatory process, causing swelling. The situation is aggravated due to traumatization of the “hood” by antagonist teeth.
Symptoms
Pericoronitis can occur in acute or chronic form. In the first case, there is a rapid increase pathological manifestations, in the second, periods of exacerbations are replaced by a temporary improvement in the patient’s condition.
Acute pericoronitis has the following symptoms:
- Pain in the area of the inflamed gum. In the first 2-3 days discomfort are aching in nature, they intensify when talking and eating. Then the pain becomes constant and acute. It radiates to the temples and ears.
- Deterioration general condition. There is malaise, weakness, headache. In some cases, body temperature rises to 37-37.5 °C. On the affected side, the lymph nodes enlarge and become painful.
- Swelling and redness of the “hood” over the tooth. Pus with a characteristic odor is released from under the gums. There is an unpleasant taste in the mouth.
Acute purulent pericoronitis may be accompanied by a subperiosteal abscess - an accumulation of pus under the periosteum at the base of the alveolar process. It develops as a result of the spread infectious process from the top of the tooth root.
Chronic pericoronitis occurs when the acute form is not properly treated. Its manifestations are not very pronounced. During periods of exacerbation painful sensations are intensifying.
The main symptoms of pericoronitis in chronic form:
- the mucous membrane of the “hood” over the tooth is hyperemic, swollen, but painless;
- opening the mouth and chewing food does not cause discomfort;
- purulent-serous fluid is sometimes released from the pathological focus;
- observed bad smell from mouth;
- the submandibular lymph node is enlarged, when touching it, unpleasant sensations occur;
- in advanced cases due to atrophy bone tissue the tooth begins to loosen.
Diagnostics
Pericoronitis is diagnosed based on patient complaints, visual examination of the oral cavity and radiography. An x-ray is necessary to determine the exact position of the wisdom tooth and assess the condition of the periodontium and surrounding bone. The disease is differentiated from pulpitis and periodontitis.
Treatment
Treatment tactics for pericoronitis are selected depending on the severity of the clinical picture. Basic methods:
- use of medications;
- laser therapy;
- surgical intervention.
As medicines drugs are used that relieve inflammation in the gum tissue, as well as antiseptic rinsing solutions. Typically, they are prescribed before or after surgery or a laser procedure.
Get rid of the disease only conservative methods impossible. Treatment of pericoronitis at home is advisable only in combination with surgical manipulations. Rinsing saline solutions, herbal decoctions and taking painkillers help to temporarily reduce the severity of the symptoms of the pathology, but do not eliminate its cause.
The essence laser therapy for pericoronitis consists of exposing the affected area to a low-intensity infrared ray. Thanks to the procedure, the following results are achieved:
- tissues are saturated with oxygen;
- in the mucous membrane, blood circulation increases and metabolic processes are activated;
- swelling and inflammation are relieved.
One session is carried out over 10-15 days.
In advanced cases, treatment of pericoronitis is carried out surgically under local anesthesia. The dentist excises the “hood”, removes the pus and rinses the mucous membrane with antiseptics. The issue of tooth preservation is decided individually. As a rule, doctors recommend removing wisdom teeth, since they do not have a functional load.
Forecast
Pericoronitis has a favorable prognosis provided adequate treatment. Possible spread without treatment inflammatory process.
The main complications of pericoronitis:
- ulcerative stomatitis;
- purulent lymphadenitis;
- osteomyelitis;
- abscesses and phlegmon in the oral cavity;
- deformation of adjacent teeth.
Prevention
The main preventive measure purulent pericoronitis is regular visit dentist During preventive examination The doctor can identify difficulties in the teething process at an early stage.
One of the types of acute periodontitis, which is characterized by the formation of purulent exudate in the periodontal tissues at the apex of the root. Exudate is a liquid that is released into tissue from blood vessels during inflammatory processes.
As a rule, acute purulent periodontitis occurs due to the lack of professional dental treatment serous periodontitis and is accompanied by general malaise, fever and headache. The disease is especially dangerous because the outflow of pus can occur not into the tooth cavity, but under the periosteum.
Clinical manifestations
Purulent acute periodontitis is characterized by constant pain that increases when biting, lightly tapping the tooth, and even touching it with the tongue. Due to the spread of pus, the gums swell in acute purulent periodontal disease, a reaction is noted lymph nodes. In addition, the following clinical manifestations are observed:
- There is a feeling that the tooth is protruding from the dental arch and does not fit into it (a symptom of an overgrown tooth);
- The pain becomes reflected and can spread to the entire jaw or half of the head;
- Periodontal fibers swell due to the formation of pus and increased acidity, which causes tooth mobility;
- The tooth changes color.
Diagnostics
In order to correctly prescribe treatment for purulent periodontitis, it is necessary to carry out diagnostics, which, in addition to a visual examination by a dentist, includes the following:
- X-ray diagnostics - allows you to detect a slight increase in the periodontal gap near the apex of the tooth root;
- electroodontometry - allows you to determine the sensitivity of the tooth.
It is important to carry out correct differential diagnosis, which allows one to distinguish purulent periodontitis from serous periodontitis, acute purulent pulpitis, osteomyelitis and others. inflammatory diseases maxillofacial region.
Treatment
Treatment of acute purulent periodontitis is complex and requires several visits to the dentist. First of all, it is aimed at ensuring the free outflow of purulent fluid from the source of inflammation. In addition, measures are being taken to stop inflammatory processes and restore appearance and functionality of the tooth.
The dentist performs mechanical cleaning of the canals and removes damaged dentin and pulp tissue from them. In order to completely stop the inflammatory processes, anti-inflammatory and antibacterial pastes are placed at the mouths of the canals. This procedure is repeated several times and is accompanied by rinsing, taking antibiotics and analgesics.
The tooth-periodontal system, or in the arms of a gentle but powerful
To understand what it is acute periodontitis and why it develops, one should realize that the tooth is not firmly driven into the gum and jaw, not driven like a nail into a board, but has sufficient freedom of movement in these structures due to the presence of ligaments between the jaw socket and the surface of the tooth.
The ligaments have the necessary power to hold the tooth in place, preventing it from excessively swinging back and forth, left and right, or rotating around a vertical axis. At the same time, providing the tooth with the possibility of “springy squats” - up and down movements in the socket limited by the elasticity of the ligaments, they do not allow it to be pressed too much inward when chewing, maintaining jaw bone from damage by this fairly hard formation.
In addition to the shock-absorbing and fixing role, periodontal structures also perform the following functions: 
- protective, because they represent a histohematic barrier;
- trophic - ensuring communication with the body of the vascular and nervous systems;
- plastic - promote tissue repair;
- sensory - the implementation of all types of sensitivity.
In case of acute damage to the periodontium, all these functions are disrupted, which leads the patient to the door to the dentist’s office at any time of the day. The symptoms can be so acute that even the thought of “enduring” and “waiting it out” does not arise (unlike when the sensations are quite tolerable).
About the mechanics of the destructive process, its stages
For the occurrence of acute periodontitis, either a medicinal effect on periodontal tissue, as in the treatment of pulpitis, is necessary, or the infection itself must penetrate into the bowels of the tooth - into the pulp. For this to happen, an entrance is required for infection to enter the tooth cavity, the role of which is performed by:
- apical canal;
- a cavity machined or formed along the way of insufficient quality;
- line of damage resulting from ligament rupture.
Infection can also enter through pathologically deep periodontal pockets.
From the damaged pulp, microbial toxins (or a drug in the “arsenical” genesis of the condition) seep through the dentinal tubules into the periodontal fissure, first causing irritation of its structures, and then their inflammation.
The inflammatory process manifests itself: 
- pain due to the reaction of nerve endings;
- microcirculation disorder, manifested by stagnation in tissues, externally appearing as hyperemia and swelling;
- the body’s general reaction to intoxication and other changes in its biochemistry.
The destructive process goes through a series of successive stages:
- On periodontal stage a lesion (or several) appears, delimited from the intact periodontal zones. The lesion expands or merges into one smaller one, involving a large volume of periodontal tissue in the process. Due to the increase in tension in the closed volume, the exudate, looking for a way out, breaks either through the marginal zone of the periodontium into oral cavity, or by melting the compact plate of the dental alveoli into the bowels of the jaw. At this moment, due to sharp decline pressure exerted by the exudate, the pain is greatly reduced. The process moves into the next phase - it spreads under the periosteum.
- Subperiosteal (subperiosteal) the phase in which symptoms appear - with the bulging of the periosteum into the oral cavity, which, thanks to the density of its structure, restrains the pressure of the purulent exudate accumulated under it. Then, having melted the periosteum, the pus appears under the mucous membrane, which is not a serious obstacle to its breakthrough into the oral cavity.
- At the third stage, due to emergence– anastomosis of the apical zone with the oral cavity, the pain can almost completely disappear or become insignificant, while the painful swelling in the projection of the apex disappears. The danger of this phase is that the inflammation does not end there, but continues to spread, capturing new areas, which can lead to serious consequences, including the development. Sometimes the formation of a fistula means a transition acute condition into chronic.

Clinical symptoms of the main forms
According to the composition of the exudate, acute periodontitis can be serous and purulent, and according to the mechanism of occurrence:
- infectious;
- traumatic;
- medicinal.
Serous phase
Serous periodontitis corresponds to initial stage process - an acute nervous reaction of periodontal structures to their irritation with the appearance of initially barely perceptible, but then increasingly increasing changes.
Due to the increased permeability of the capillary walls, a serous effusion is formed, which then includes living and dead leukocytes, products of the vital activity of microbes, and the remains of dead cells. This entire complex of microorganisms, active chemically and enzymatically, acts on the sensory nerve endings, causing them irritation, perceived as pain.
It is permanent, being mild at first, but gradually and methodically increasing, becoming unbearable when beaten on the tooth. In some cases, prolonged and volitional pressing of a tooth by closing the jaws can lead to a decrease in pain manifestations(but without going through them completely). External manifestations in the environment of the affected tooth is not observed, because inflammation in this case does not reach its peak.

Purulent phase
If you manage to overcome the initial pain without seeking treatment dental care, the process moves into the next phase of purulent melting, and accordingly periodontitis becomes purulent.
Foci of microabscesses form a single, accumulated pus creates excess tension in a closed volume, causing unforgettable and unbearable sensations.
 Characteristic symptoms are acute pain of a tearing nature, which radiates to the nearest teeth and further, right up to the opposite jaw. Even a light touch to a tooth causes an explosion of pain, calmly closing the mouth gives the effect of the greatest pressure on the painful area, the symptom of an “overgrown tooth” is positive in the absence of the reality of its protrusion from the socket. The degree of fixation in the socket decreases, temporarily and reversibly increasing.
Characteristic symptoms are acute pain of a tearing nature, which radiates to the nearest teeth and further, right up to the opposite jaw. Even a light touch to a tooth causes an explosion of pain, calmly closing the mouth gives the effect of the greatest pressure on the painful area, the symptom of an “overgrown tooth” is positive in the absence of the reality of its protrusion from the socket. The degree of fixation in the socket decreases, temporarily and reversibly increasing.
In the case where inadequately deep gingival pockets serve as the entry point for infection into periodontal tissues, we speak of a marginal form of periodontitis (as in acute damage to the marginal periodontium). , occasionally, the process is accompanied copious discharge pus up to suppuration with the corresponding smell of decomposition inherent in it.
Due to active drainage, pain in general symptoms fades into the background than with .
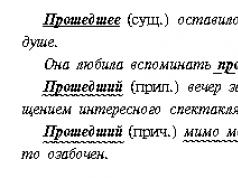
Acute purulent periodontitis under x-ray:
Traumatic form
In the case of a short-term effect of great destructive force (as with a blow that can cause rupture of ligaments over a large area), the development of traumatic periodontitis is possible. The intensity of pain depends on the degree of destruction of periodontal structures, increasing significantly when touching the painful area.
Characterized by increased mobility. For chronic negative impact periodontal tissues are capable of restructuring, the resorption of the bone walls of the alveoli begins, the destruction of the fixing ligaments occurs, which leads to the expansion of the periodontal gap and loosening of the tooth.
Medicinal form
A distinctive feature of the medicinal form of the disease is its occurrence due to the impact on periodontal structures of drugs introduced into the root canals by mistake, or due to violations during the use of therapeutic therapy.
Most often, the development of arsenic periodontitis is diagnosed, which develops both when the required dose arsenic for, and when it remains in the tooth cavity for an excessively long time. The most popular “scenario” for the development of this form of the disease is insufficient tightness - the toxic drug must be immediately removed and the tissues treated with an antidote (Unithiol).
About diagnosis and differentiation from other diseases
To make a diagnosis, questioning the patient is usually sufficient (especially important with diagnostic point visual signs in the past and significant pain in the tooth, sharply increasing from touch, in the present), plus objective research data (painlessness of probing and a specific picture of crown destruction).
It is necessary to differentiate acute periodontitis from:
- in a state of exacerbation;

A sign of pulpitis is throbbing pain of a paroxysmal nature, its character and intensity does not change with percussion tapping, but with a tendency to intensify at night, while periodontitis manifests itself as pain that does not go away and is unbearable, tearing in nature and sharply increasing from touching the tissues.
Unlike chronic periodontitis the data do not demonstrate changes during an acute process in the periodontium.
With osteomyelitis, the image shows the extent of the lesion, including the roots of adjacent teeth. The accuracy of the diagnosis is confirmed by the pain of several adjacent teeth during percussion.
Features of treatment
The treatment strategy for the acute phase of periodontitis involves two options: complete healing of all tooth cavities, cleaning them of infection and decay products, or, as a last resort, its removal along with all pathological contents.
After confirmation of the diagnosis, acute periodontitis is performed, for which the highest quality anesthesia is performed due to the extreme susceptibility of the inflamed tissues to touch and vibration.
First visit
At the first visit to the clinic, the defect in the tooth crown is eliminated by preparing to healthy tissue; if there are already installed fillings, they are removed. 
The next stage is the detection and opening of the root canal orifices. In the case of their previous filling, the filling material is removed, and during the initial opening of the canals, the most thorough removal of detritus is carried out, the walls are processed mechanically with the excision of all non-viable tissues. At the same time, the lumen of the canals is expanded to a diameter sufficient for further passage and filling.
All procedures are carried out using an antiseptic solution (Sodium hypochlorite or).
Once a sufficiently reliable drainage has been created, treatment of the apical region involves three tasks:
- destruction of painful flora in the main root cavities;
- extermination of infection in all branches of the root canals up to the dentinal tubules;
- suppression of periodontal inflammation.
The success of these activities is facilitated by the use of:
- electrophoresis with one of the antiseptic solutions;
- method of intensifying diffusion into root canals medicinal products using ultrasound techniques;
- treatment of root canals with laser irradiation (the effect is achieved by combining radiation with the bactericidal effect of atomic oxygen or chlorine released from specially used solutions under the influence of a laser).
The stage of mechanical treatment and antiseptic etching of the tooth canals is completed by leaving it uncovered for 2–3 days. The doctor gives recommendations to the patient regarding the dosage regimen and the use of rinses with medicinal solutions.
If there are signs, the cavity is opened with obligatory dissection of the periosteum along the transitional fold in the area of projection of the root apex, with obligatory jet washing antiseptic solution and closing the resulting wound with elastic drainage.
Second visit to the clinic
On the second visit dental clinic in the absence of the patient, it is performed either permanently or for a period of 5–7 days using the post-apical space for treatment. In this case, the installation of a permanent root filling and crown reconstruction are postponed until the third visit.
In case of complications
If the root canals are obstructed or endodontic treatment fails, the tooth is removed from further to the patient on tactics for treating alveoli at home.
When examined the next day (if necessary), the hole is cleaned of the remaining blood clots with loose tamponade with a bandage sprinkled with Iodoform, with the manipulation repeated after 1–2 days. If there are no symptoms, there is no need for additional manipulations.
The occurrence of “arsenic periodontitis” requires immediate removal of the toxic agent and treatment of the inflamed tissue with an antidote.
Possible consequences, regular visits to the dentist.
 Preventing the development of caries and its constant companion pulpitis is possible only by following the norms of common sense in the chewing process, because only a healthy periodontium successfully withstands the loads developed by all groups of masticatory muscles.
Preventing the development of caries and its constant companion pulpitis is possible only by following the norms of common sense in the chewing process, because only a healthy periodontium successfully withstands the loads developed by all groups of masticatory muscles.
In order to avoid the development of drug-induced periodontitis, strict adherence to standards and techniques in the treatment of oral diseases is necessary, as well as, should be done without excessive stress on the periodontium.
Any endodontic operation must be completed fully along its entire length. In the case of incompletely traversed canals or poor-quality filling, the development of pulpitis inexorably follows, followed by periodontitis.
One of the most serious illnesses in the field of dentistry is purulent periodontitis, especially in the phase of transition to acute form. If you even have suspicions, much less the first symptoms, you should immediately consult a doctor for treatment, since the consequences of this disease can be the most tragic. We can talk not only about the unpleasant prospect of losing a tooth, but also about the threat of developing other diseases of an equally serious nature.
All about periodontitis
This disease usually originates in the root system of the tooth and is an inflammatory process that poses a serious threat to the health of the human oral cavity. The dentist may suspect acute periodontitis even at the stage of visual examination, which will be confirmed by the following data:
- electrical odontometry;
- X-ray;
- aching pain in the patient.
In more than two thirds of cases, acute periodontitis is observed in patients under 40 years of age (approximately 70% of cases); this disease usually develops after 50 years of age.
Symptoms of the disease
The main complaint in patients who have started the inflammatory process is severe, growing and throbbing pain that can radiate to other organs, for example, to the ear, eye or nose. When you touch a tooth or try to bite, the pain increases sharply, which forces the person to either completely refuse food or not use the affected side of the jaw when chewing.
Determining the source of pain is difficult; patients cannot clearly name the place where the pain occurs, since it spreads to half of the head. Often a person begins to experience general malaise, he has a fever and a headache. In addition, the area where the disease is localized may experience swelling, in some cases this even makes it difficult to open the mouth. The color of a damaged tooth changes and it may become mobile. Another symptom may be inflammation submandibular lymph nodes, which demonstrate an increase in their size and a change in the density of the structure. Finally, the patient may experience the sensation that his tooth is lifted above its socket, which is explained by pressure due to the accumulation of pus.
Causes of purulent periodontitis
 There are three forms of this disease:
There are three forms of this disease:
- infectious;
- medicinal.
Infectious purulent periodontitis occurs most often; in most situations it develops against the background of other diseases, for example, gingivitis, or. In approximately 60-65% of cases, periodontal tissues are damaged by staphylococci, hemolytic and saprophytic streptococci. Infection with other microorganisms, for example, non-hemolytic streptococci, accounts for no more than 15% of cases.
The activity of pathogenic bacteria leads to a violation of the integrity of tooth enamel; they penetrate into the root canals and gum pockets, where, as a result of their continued reproduction, the concentration of toxins they release increases. There are cases when, with sinusitis or osteomyelitis, the infection penetrates into the periodontium through the lymph or through the blood.
The traumatic form of acute periodontitis is provoked by various injuries, such as blows or bruises. The traumatic form can develop into chronic illness because of poor quality treatment, or malocclusion, as well as the habit of gnawing on various hard objects.
The development of a medicinal form of the disease is associated with the wrong choice medicines during treatment or pulpitis. The use of arsenic or phenol with formalin can provoke an inflammatory process in the patient.
Among the risk factors, some types of somatic diseases should be mentioned, in particular, diseases gastrointestinal tract or diabetes, as well as insufficient attention to oral hygiene issues, lack of necessary for the body human microelements or vitamin deficiency.
Forms
There are several forms of manifestation of acute periodontitis.
Acute apical periodontitis
 May occur due to infection, injury, or as a result of medication. It is caused in an infectious form by pathogens that penetrate the tooth from the pulp through the root canal. Drug-induced inflammation is most often brought to life as a result of improper treatment of pulpitis or tooth root canal. Toxic periodontitis is most often provoked by the action of arsenic; in addition, the threat of the disease increases sharply in cases of filling material penetration beyond the apical tissues of resorcinol. When a tooth is injured, periodontal tissue often ruptures and is displaced; this can all be accompanied by an infectious lesion.
May occur due to infection, injury, or as a result of medication. It is caused in an infectious form by pathogens that penetrate the tooth from the pulp through the root canal. Drug-induced inflammation is most often brought to life as a result of improper treatment of pulpitis or tooth root canal. Toxic periodontitis is most often provoked by the action of arsenic; in addition, the threat of the disease increases sharply in cases of filling material penetration beyond the apical tissues of resorcinol. When a tooth is injured, periodontal tissue often ruptures and is displaced; this can all be accompanied by an infectious lesion.
Acute apical acute periodontitis will have the following clinical manifestations:
- swelling of the gums, pain during eating and biting (serous inflammation);
- pulsation of pain and its intensification, tooth mobility and asymmetric swelling of the face, rising temperature (purulent inflammation).
Due to the similarity of symptoms with other diseases, for example, jaw osteomyelitis, or periostitis, diagnosis should be differential.
Acute apical
Develops most often as a result of exacerbation of pulpitis; this disease is caused by the penetration of bacteria and their toxins into periodontal tissues. This form of periodontitis occurs in two phases; during the first, intoxication of periodontal tissues occurs, which is accompanied by acute pain in the tooth and gums when eating food. The patient is able to name the problematic place in the mouth, but the tooth does not lose stability, does not change its color and there are no difficulties when opening the mouth. This is the main difficulty, since a person often does not see a doctor at this stage, and it is this stage that is important for the timely detection of the disease and its elimination.
The second stage is clinically more pronounced, but much depends on the composition of the exudate. Some patients do not experience acute pain, but for some it becomes so intense that the need for immediate help becomes obvious. The tooth begins to be perceived as foreign element, one gets the impression of its growth and increase. When eating food, pain is felt, there is a reaction to changes in temperature, and the gums swell.
Acute purulent
This form brings with it sharp pain and the picture of inflammation develops as follows:
- periodontal localization of inflammation that occurs within clear and visible boundaries, resulting in overgrown tooth syndrome;
- the endosseous phase, in which pus penetrates the bone structures;
- subperiosteal phase, characterized by the accumulation of purulent masses under the periosteum, due to which the patient experiences throbbing pain, his gums swell and the development of gumboil is often observed;
- submucous phase, which is characterized by the penetration of pus into soft fabrics, which leads to a decrease in pain and an increase in swelling.
It is also important here differential diagnosis, since the similarity of symptoms is observed with other diseases, for example, sinusitis, or periostitis.
Acute serous periodontitis
 For pathogenic microorganisms, the pulp, which is in the stage of inflammation and decomposition, is a favorable environment for their development and reproduction. Typically, the inflammatory process develops gradually, but its exacerbation can occur as a result of injury or the influence of medications. As a consequence, the development of acute serous periodontitis is observed, during which toxins permeate all tissues and hyperemia of the mucous membrane develops.
For pathogenic microorganisms, the pulp, which is in the stage of inflammation and decomposition, is a favorable environment for their development and reproduction. Typically, the inflammatory process develops gradually, but its exacerbation can occur as a result of injury or the influence of medications. As a consequence, the development of acute serous periodontitis is observed, during which toxins permeate all tissues and hyperemia of the mucous membrane develops.
Due to its mild symptoms, this form is rarely diagnosed. The patient does not feel severe pain, he may experience some discomfort when eating, and also feel a slight itching in the gums. This form of the disease is considered reversible and treatment rarely leads to tooth loss; its removal may be necessary to stop the infection.
Acute traumatic form
But diagnosing this form is associated with considerable complications, since we are talking about trauma to the pulp. Symptoms are clearly expressed, but do not have specificity, since they appear as painful sensations caused by chewing food. Swelling of the mucous membrane is not observed, enlargement of the lymph nodes is also not detected, and the temperature remains normal. The appearance of obvious symptoms occurs only when a severe injury occurs, for example, with a serious bruise, when severe pain, hemorrhage in the oral cavity and visually noticeable damage to the tooth are observed.
Possible complications
If you don't timely treatment purulent periodontitis, then in the place of the highest concentration of toxins the canal can rupture and the entire mass purulent discharge will spread over the gum. The result may be defeat for now healthy teeth, but that's not the only thing possible complication, other factors can also have a negative effect, in particular:
- the appearance of fistulas as a result of pus trying to break through the gums;
- tissue necrosis due to further spread of infection, they will no longer be subject to restoration;
- the prospect of damage to bone tissue, which poses a particular threat to health;
- the possibility of damage to the cheeks with ulcers, which in the future can lead to limited mobility of the jaws.
Diagnosis of the disease
 The following methods can be used to diagnose the disease:
The following methods can be used to diagnose the disease:
- Differential diagnosis. The similarity of the symptoms of many purulent diseases in dentistry requires implementation additional methods for staging accurate diagnosis. Without this, treatment may be ineffective.
- X-ray diagnostics. Thanks to the pictures, you can see how much the periodontal gap located near the root apex has widened.
- Blood test for formula. The need for this technique is explained by the fact that when such a disease occurs, the blood formula changes quite significantly.
- Electroondometry. Using this method makes it possible to record indicators of tooth sensitivity.
Stages of the clinical picture
There are four stages of the periodontitis clinic, which allow timely detection of the symptoms of the disease and its timely treatment:
- Acute periodontitis. At this stage of the disease, an inflammatory process forms and pus is released. The patient has the sensation of a tooth growing in the mouth, the formation of ulcers and additional cracks through which the infection spreads.
- Endosseous stage. The onset of this stage occurs at the moment when purulent masses reach the bone tissue and its damage occurs.
- Subperiosteal stage. Outwardly it manifests itself severe swelling, the appearance of swelling and redness, as well as flux. This occurs due to the fact that harmful secretions have already reached the periosteum.
- Submucosal stage. Destruction of the periosteum and penetration of secretions into the soft tissues, which leads to a temporary subsidence of pain and reduction of the tumor, but then an exacerbation of painful sensations occurs and serious therapeutic measures are required for treatment.
Treatment of periodontitis
Treating a tooth for purulent periodontitis alone will not be enough; you will also need to use antibiotics to fight inflammation. The primary task is to remove the pus and tissues affected by it. For outflow harmful secretions All cavities are cleaned from inflamed pulp using a pulp extractor. In particularly advanced situations, dissection of the periosteum may be required to drain purulent masses. Tooth extraction becomes a last resort measure, which is forced to be taken if the treatment procedure does not give the desired result. The sooner you start fighting the disease, the higher the chances of preventing such a situation.
Preventive techniques
Treatment of acute periodontitis takes a lot of time and brings a lot of trouble and suffering to the patient, so prevention and prevention of the disease play a role vital role. It is necessary to visit the dentist regularly and take action as soon as the first symptoms of caries appear. Naturally, we must not forget about the standard hygiene procedures and proper oral care.
Video on the topic
Purulent periodontitis can be considered as further development an inflammatory process in the tissues of the apical periodontium, and this form is characterized by the presence of a purulent focus.
In most cases, the purulent process in periodontal tissues is characterized by a violation of the general condition, symptoms of intoxication appear - headache, fever, malaise, weakness, lack of sleep and loss of appetite. A blood test determines accelerated ESR and leukocytosis.
Patients experience severe pain, which over time becomes unbearable. Biting on a tooth, and in some cases any touching it, causes unbearable pain. In this case, painful sensations radiate along the branches trigeminal nerve, so the patient cannot accurately indicate the causative tooth. There is a feeling of an “overgrown” tooth.
During an external examination, facial asymmetry may sometimes be noted due to swelling of the soft tissues of the cheek or lip (depending on the number of the causative tooth). However, more often the facial configuration is not changed. The patient's mouth may be half-open, since the closing of the teeth leads to severe pain in the causative tooth.
When palpating the submandibular lymph nodes, they are sore, they are enlarged and compacted.
A causative tooth is found in the oral cavity, which can be:
- With a deep carious cavity, discolored.
- Destroyed to the level of the gums (root).
- Under a filling or crown.
Pressing on a tooth, not to mention percussion, causes severe pain. The mucous membrane in the projection of the causative tooth is swollen, hyperemic, and pain is noted upon palpation.

Despite the characteristic clinical picture, in most cases, the doctor sends the patient for an x-ray of the diseased tooth. In acute purulent periodontitis, no periapical changes are detected on the radiograph; the periodontal fissure is slightly widened.
Differential diagnosis
The purulent form of apical periodontitis must be distinguished from:
- Acute pulpitis, in which attacks of pain alternate with short pain-free periods. Also, with pulpitis, percussion is painless, there is no inflammatory reaction mucous membrane in the tooth area.
- Serous periodontitis, which is not characterized by disturbances in the general condition (fever, weakness, headache). There is also no irradiation of pain to other parts of the maxillofacial region.
- Exacerbations of chronic periodontitis, in which x-rays reveal bone changes in the area of the root apexes.
- Periostitis of the jaw, which is characterized by significant asymmetry of the face, smoothness transitional fold, the presence of infiltration. It is quite difficult to differentiate incipient periostitis from a purulent process in the periodontium, because a transitional process can often be observed.
- Odontogenic sinusitis, in which, in addition to dental symptoms, there will be signs of inflammation in the maxillary sinus– pain and a feeling of fullness in the sinus area, increasing when the head is tilted, discharge from the corresponding half of the nose.
Treatment
The choice of treatment method depends on functional state tooth Removal is indicated when:
- Severe tooth decay (below gum level).
- His mobility is grade II-III.
- Failure of therapeutic treatment.
- Inappropriateness of tooth preservation.

In other cases, endodontic treatment is performed. On the first visit, the tooth cavity is opened, mechanical and antiseptic treatment of the canals is carried out, and the tooth is left open for several days. The patient should rinse the tooth with a saline solution.
On the second visit (when the inflammatory process subsides), the canals are cleaned again and washed with antiseptics, after which they are sealed.