Inflammation of periodontal tissue at the apex of the tooth root is called apical periodontitis.
Apical periodontitis can be infectious, traumatic and drug-induced. In most cases, infectious apical periodontitis occurs. Infectious periodontitis occurs when caries is advanced - the infection spreads from the tooth pulp to the periodontium. Infectious periodontitis can be determined by the following symptoms - sharp pain caused by suppuration, swelling and mobility of the teeth occurs, and the color of the tooth crown may also change. Traumatic apical periodontitis occurs when there is trauma to the face or mechanical impact on the teeth (eating solid food or biting off threads is sufficient for the appearance of traumatic periodontitis). Inflammation during injury is accompanied by swelling, as well as acute and severe pain. Drug-induced apical periodontitis occurs as a result of medical errors, at improper treatment pulpitis strong drugs penetrate into the periodontium, causing irritation and the development of an inflammatory process.
Apical periodontitis is inflammation of the periodontal tissue at the apex of the tooth root. The inflammatory process can involve cement and dentin of the tooth root. It happens that the infection penetrates into the alveolar bone.
Etiology and clinic of apical periodontitis
Different types periodontitis differ in their etiology and clinical manifestations. The following types of apical periodontitis are distinguished:
- Infectious is a type of periodontitis that occurs more often than others. Develops as a complication of caries: infection from the pulp spreads to the periodontium. In the acute phase apical periodontitis manifests itself as sharp pain. The pain is constant, concentrated near the affected tooth. Pain radiating to other areas is a sign of suppuration. The tooth may become mobile. At this stage, soft tissue swelling develops. Without adequate treatment acute apical periodontitis enters the chronic phase. Chronic apical periodontitis characterized by mild symptoms. Patients report minor pain, and sometimes the color of the tooth crown changes.
- Traumatic periodontitis develops after facial trauma. It happens that the development of the disease is facilitated by prolonged mechanical impact on the tooth. This happens when a filling is placed unsuccessfully or when there are constant traumatic habits. Frequent biting of thread or biting into hard food is sufficient. Inflammation during injury is acute and manifests itself as sharp pain and swelling.
- Drug-induced periodontitis is a consequence of medical errors. If pulpitis is treated incorrectly, strong drugs penetrate into the periodontium. There, irritation occurs and an inflammatory process develops.
Diagnosis of the disease
Methods for diagnosing apical periodontitis include a set of procedures. First of all, the clinical picture of the disease is studied. The clinical picture of acute periodontitis is pronounced: the tooth hurts greatly. Probing and percussion of a diseased tooth causes pain to the patient. The gums are swollen, liquid exudate may be released, and a fistula may form. The patient may have a headache and discomfort to nearby lymph nodes. The temperature may be elevated, and leukocytosis is observed in the blood. Acute periodontitis is not detected x-ray; the diagnosis is made based on the clinical picture.
The chronic form of periodontitis is more difficult to diagnose based on the clinical picture. The professional will pay attention to the widening of the gap between the gum and tooth. The tooth becomes mobile, its crown color changes. The reaction to cold and hot is not expressed. During probing and percussion, the patient may experience pain. When entering the tooth cavity, you can see the destroyed pulp. When such clinic, diagnosis of apical periodontitis clarified by x-ray. A periodontal cyst appears on an x-ray as a clear formation at the root apex. With fibrous periodontitis, the photographs clearly show an enlarged periodontal gap. Granulating chronic periodontitis is characterized by destruction of the bone tissue of the alveoli. In this periodontitis, cementum and dentin are also replaced by granulomatous tissue. In the picture, this form of the disease appears as blurred contours of the tooth root. The surrounding bone tissue may also be eroded.
These menacing manifestations signal one thing: the tooth needs to be treated immediately! A correct diagnosis allows you to begin treatment immediately.
Treatment
Treatment of apical periodontitis is a complex process. If treatment is started on time, it is possible to stop infectious process in the gum. Planning and preparation for treatment of apical periodontitis are required. An experienced dentist first determines how advanced the inflammatory process is. After an accurate assessment of the condition of the tooth, the doctor draws up a plan therapeutic measures. If there is an abscess at the root apex, the exudate is drained. This relieves swelling and reduces painful manifestations. The patient is prescribed physical therapy, rinsing with antiseptic solutions, and taking antibiotics. Next, the destroyed pulp is carefully removed. The root canals are completely cleared of affected tissue. After mechanical cleaning, therapy is carried out aimed at bone restoration. Drugs are injected into the root of the tooth to relieve inflammation of the bone tissue. There are also medications that stimulate regenerative processes within the affected bone. After the inflammatory process subsides, sealing of the tooth begins. Cleaned canals and carious cavities are carefully filled. If it is not possible to stop the apical inflammation of the root, I act differently. The root apex can be removed, after which the tooth is further fixed. Therapeutic measures in this case are carried out according to the same plan. If it is not possible to stop the inflammation, the tooth must be
By virtue of various factors oral tissues are exposed to pathogenic effects. A third of the diseases are due to apical periodontitis. It can be chronic, acute, and the symptoms are not always clear, which excludes timely treatment.
When should you see a doctor and how does such an unpleasant pathology manifest itself? Even ordinary people, far from medicine, you need to know what to look for at the first manifestations of the disease, and most importantly, how to prevent any complications.
What is apical periodontitis?
This pathology is a consequence of inflammation of the connective tissues of the periodontal ligament and is located in the area of the apex of the tooth root. The acute stage is manifested by severe pain, which is simply impossible not to notice. The chronic variety is much more insidious, when all the signs and symptoms are blurred and the disease proceeds hidden.
Apical periodontitis is of pulpal origin, that is, it most often occurs as a result of advanced pulpitis. From a small inflammation that forms, a larger focus very quickly develops and the surrounding tissues are affected. Doctors note that most often a third of their patients aged 20 to 60 experience this form of the disease.
To detect and treat it in time, you need to regularly contact your dentist and visit a doctor at the first discomfort. Having carried out a high-quality and complete diagnosis, as well as collecting a medical history (anamnesis), he will be able to make an accurate diagnosis and prescribe adequate treatment. Typically, anti-inflammatory and antibacterial drugs, cleaning and treatment of the canals, and at the end the open affected cavities are filled.
If you miss a timely diagnosis and elimination of the causes of the symptoms that appear, then apical periodontitis will develop into other more complex pathologies. Thus, an untreated form of the disease is fraught with complications such as perimandibular abscess, periostitis, phlegmon, osteomyelitis, the formation of cysts, fistulas, etc.
Causes
Even people who practice regular hygiene and frequently visit the dentist can develop apical periodontitis. Why does this happen and what are the causes of the disease? There are main groups of factors that contribute to inflammation of the root apex:
- Infectious - as a result of an infection that has entered the body, and dental or gingival tissues in particular. This can be caused by an advanced form of caries, the presence of streptococci, staphylococci and other dangerous microorganisms in the mouth. They penetrate the apical foramen and lead to infection of the tissue, creating acute inflammation. Diseases such as sinusitis or osteomyelitis can also cause periodontitis.
- Medicinal – when medical drugs with a destructive effect enter the periodontal tissue. For example, arsenic in any form, phenol, phosphate cement or formalin will negatively affect the condition of soft tissues, irritating them and causing inflammation. Also, factors in the appearance of apical periodontitis include illiterate actions of the doctor, when he accidentally damages the hard tissues and extends beyond the apical region.
- Traumatic – most often cause chronic forms diseases, especially if this happened as a result of incorrectly installed orthodontic structures, fillings, crowns, etc. They constantly put pressure on soft tissues, causing inflammation. Another cause of periodontitis is considered to be the result of a strong blow, unexpected injury, fractures or bruises of the jaw.
Classification
In dentistry, types of periodontitis can be distinguished depending on the factors listed above and named accordingly. But there is another classification that better determines what stage the inflammation is at:
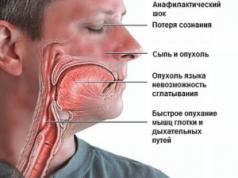
- Acute apical periodontitis - manifested by severe increasing pain, which is significantly intensified by any touch. The tooth also reacts to cold and hot foods and becomes too sensitive. The nature of the sensations is pulsating, sometimes radiating to nearby organs (ears, eyes, nose, throat, The lymph nodes). The disease develops rapidly and leads to general deterioration the patient’s condition – his body temperature rises to 38 degrees, headaches begin. Symptoms grow actively and bother you for up to two weeks in a row. If you do not consult a doctor at this time, it will lead to the appearance of cysts, fistulas, or progress to the next stage with various complications.
- Chronic apical periodontitis is mostly asymptomatic, but sometimes exacerbations occur, which are similar in symptoms to the acute form of the disease. In the remission stage, that is, when the main symptoms fade, the patient may experience mild pain when chewing, as well as bad smell from mouth. In some cases, fistulas appear in the gums, and there is a feeling of distension and swelling in the tooth. In advanced form, pus begins to secrete.
If we talk about a more detailed classification, then in the acute stage there are varieties such as serous and purulent, depending on the discharge. And chronic is divided into granulating, granulomatous or fibrous.
Symptoms
The manifestations of the disease depend greatly on both individual characteristics the patient, and on the specific form and cause of the disease:
- Infectious apical periodontitis causes severe pain whenever the affected tooth is touched, and also manifests itself in the form of swelling and redness of the gums around it and the discharge of pus. At the same time, the person’s temperature rises.
- The medicinal form is felt by aching pain, but can intensify during meals. Distention and the resulting mobility indicate that inflammatory processes are occurring inside.
- After impact or mechanical injury sharp pain appears, swelling of the mucous membrane quickly increases, and in some cases blood is released. The tissues of periodontitis themselves turn pink, and the tooth may begin to become loose.
- The symptoms are also very different in the chronic and acute forms, which can transform into one another. Therefore, if the pain suddenly stopped bothering others visible symptoms disappeared, this does not mean that the disease went away on its own. Most likely, it simply developed into a chronic form.
Diagnostics
To prescribe competent treatment, a doctor needs to accurately diagnose and differentiate apical periodontitis from other diseases with similar symptoms (purulent diffuse pulpitis, perihilar cyst, periostitis, acute maxillary sinusitis, osteomyelitis, etc.). For this purpose they carry out X-ray examination, collect anamnesis, examine the oral cavity and do electroodontometry (EDI).
Thus, with chronic granulating periodontitis, an area with unclear boundaries of sparse hard tissue measuring 1-8 mm is noticeable. But the granulomatous form is manifested by precise rounded contours of the affected area around the apex of the tooth root. The fibrous appearance of the disease on x-ray appears as an enlarged space in the apical region with no resorption of the bone wall.
Treatment methods for apical periodontitis
The process of eliminating such inflammation cannot be solved in one visit. To do this, you need to go through a number of steps, which requires several calls:
- Mechanical preparation, during which the canals of the affected tooth are opened and direct contact with the root apex is created. This manipulation occurs under local anesthesia using special tools.
- Antiseptic treatment and cleansing of the inflamed area. In this case, the pulp is removed, tissues affected by caries are eliminated and the collected exudate is allowed to come out. Sometimes ultrasonic exposure is used to ensure disinfection of dental canals. But more often they resort to antibiotics and antiseptic solutions. The doctor also places an anti-inflammatory paste into the open cavity.
- After removing all unpleasant symptoms and disinfecting surfaces, the pulpless tooth is carefully filled.
In addition, the specialist may prescribe the patient other ways to speed up treatment - rinsing herbal decoctions or mineral water, taking sulfa drugs, antibiotics and physiotherapeutic procedures (Sollux, UHF, infrared laser treatment, etc.).
In the most difficult cases, when such treatment does not produce results or serious consequences and complications appear, it is necessary to use surgical methods elimination of apical periodontitis. In the most extreme forms of the disease, all that remains is to remove the affected tooth completely.
Video: algorithm for the treatment of periodontitis in children.
Prevention
TO preventive methods The simplest and most universal rules of oral care include:
- surface treatment twice a day;
- every six months you need to come to the dentist for examinations to monitor the condition of your teeth and mucous membranes;
- At the first symptoms of any disease, contact a specialist for help and follow the prescribed treatment.
If you don't pay attention to aching pain And discomfort, which occur only periodically and start the disease, then the prognosis turns out to be disappointing. Complications manifest themselves in the form of the formation of cysts, granulomas, damage to surrounding tissues, which will most likely lead to long-term and complex treatment or tooth extraction.
The previous article discussed general characteristics apical periodontitis and more in-depth features of the course of acute apical periodontitis. In this article we will take a detailed look at chronic apical periodontitis, clinical picture, diagnosis and treatment features. We will also touch on the features of the clinic and the treatment of traumatic and drug-induced periodontitis.
Let's remember the classification. According to some classifications, apical periodontitis is:
ICD classification – 10
K 04.4 Acute apical periodontitis of pulpal origin
K 04.5 Chronic apical periodontitis
Apical granuloma
K 04.6 Periapical abscess with fistula
- Dental
- Dentoalveolar
By 04.60 Having communication with the HF sinus
By 04.61 Having communication with the nasal cavity
By 04.62 Having communication with the oral cavity
K 04.63 Having a connection with the skin
K 04.69 Periapical abscess with fistula, unspecified
K 04.7 Periapical abscess without fistula
- Dental
- Dentoalveolar
- Periodontal abscess of pulpal origin
- Periapical abscess without fistula, unspecified
K 04.8 Root cyst
K 04.89 Root cyst, unspecified
K 04.9 Other unspecified diseases of the pulp and periapical tissues
Classification of periodontitis according to I. G. Lukomsky
- Acute periodontitis
- Serous
- Purulent
- Chronic periodontitis
- Fibrous
- Granulating
- Granulomatous
- Exacerbation of chronic periodontitis
Chronic apical periodontitis
Chronic apical periodontitis is most often an asymptomatic inflammation in the tissues of the apical periodontium, which is manifested by radiological changes at the apex of the tooth roots.
Many dentists use the clinically convenient classification of I. G. Lukomsky. It simplifies the diagnosis.
Chronic fibrous periodontitis
Occurs as an outcome acute periodontitis or cure granulating and granulomatous periodontitis. Traumatic etiology is also important due to overload, which occurs with the loss of a large number of teeth or non-physiological articulation.
Chronic fibrous periodontitis is detected on an x-ray as an expansion of the periodontal fissure in the apex area and is almost never accompanied by destruction of the adjacent bone.
Chronic granulating periodontitis
It is the most active form among all chronic periodontitis and is the outcome of an acute process.
The patient complains of unpleasant, slightly painful sensations when biting on the causative tooth.
Externally, the patient looks as usual, sometimes there is an enlargement of the submandibular lymph nodes. In the oral cavity we see hyperemic mucosa in the tooth area, painful on palpation. Distinctive feature This type of periodontitis is the presence of a fistula in the projection of the root apex. It may ooze pus or bulge granulations. Young granulation tissue grows through damaged cement or even dentin into the bone marrow spaces, often growing along the walls of the fistula tract. The tooth is destroyed or intact. Percussion is weakly positive.
On the x-ray we see a clearing area due to bone destruction in the area of the root apex. The lesion has unclear contours and comes in different sizes.

Chronic granulomatous periodontitis
This type of periodontitis is asymptomatic and manifests itself clinically only during exacerbations. These manifestations can be of the type of granulating periodontitis in the form of fistulas and hyperemia of the mucous membrane.
The difference between granulomatous periodontitis and granulating periodontitis is the presence on the radiograph of a clearing focus at the apexes of the roots with a clear round shape (apical granuloma).
Currently, doctors are moving away from grading the size of the lesion (0.5 cm - granuloma, 0.6-0.8 cm - cystogranuloma, more than 0.8 cm - radicular cyst.

Cyst - what is it and why?
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts - true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage it is most likely epithelial cells Malasse islets proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their source of nutrition, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - theory about the closure of all open connective tissue areas by the epithelium, resulting in necrosis.
At the third stage of cyst formation after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to large sizes. A pocket cyst is called such because the enlargement of the root canal resembles an enlargement of the periodontal pocket.


Traumatic periodontitis
Periodontal trauma is one of the initiating factors in the occurrence of hemorrhage and the development of ischemia, which directly leads to the formation of pulp necrosis. The focus of necrosis attracts bacteria, colonizes them and infects the periodontium. With an increase in the number of microorganisms, acute inflammation begins. Traumatic periodontitis develops.
With chronic long-term trauma, periodontal restructuring occurs gradually, first due to its adaptation, then as chronic inflammation with lacunar resorption of the compact lamina.
The main reason for the development of pathology is the inflammatory response. As a result of occlusal trauma, inflammatory mediators are produced in the pulp; they are considered a protective reaction to mechanical aggression. They disrupt microcirculation and increase vascular permeability. The pulp dies.
When pulp necrosis reaches the apical periodontium, due to its cytotoxic effect, interleukins activate osteoclasts and bone resorption.
Medicinal periodontitis
Drug-induced periodontitis develops when aggressive liquids or drugs, such as arsenic paste, formalin, tri-cresol formalin, and phenol, enter the periodontium. Penetration into the periodontium occurs through the root canal.
This also includes periodontitis, which develops in response to the removal of phosphate cement, resorcinol-formalin paste, pins and other filling materials into the periodontium during the treatment of pulpitis. Drug-induced periodontitis also includes periodontitis due to allergies as a result of the use of drugs that can cause a local immune response (antibiotics, eugenol, etc.).

Foreign bodies
Gutta-percha, paper pins, calcium residues and a wide variety of other things can be found in the periapical tissues.
The apical periodontium always reacts to foreign bodies. They can enter through the root canal, through an injured mucous membrane or periodontal pocket.
In case of penetration of a paper pin, it should be remembered that human body does not know how to process cellulose, so the foreign body is surrounded by a bacterial plaque, which maintains inflammation.
Gutta-percha is a biocompatible material. However, at the same time it can give a reaction from the apical periodontium. In studies on guinea pigs It has been shown that large particles of gutta-percha are encapsulated, surrounded by collagen fibers, and small particles support a local tissue reaction. And magnesium and silicon, which are contained in excess gutta-percha, can cause resorption.

Diagnosis of chronic apical periodontitis
Diagnosis of chronic apical periodontitis is similar to that in the case of acute apical periodontitis. This means we use the basic additional methods diagnostics
The main ones include clarifying the patient’s complaints, medical history, probing, percussion, palpation and determining tooth mobility.
The patient’s complaints are most often absent, but they may complain of discomfort while eating when biting.
Probing is painless, palpation of the mucous membrane in the apical area is also painless. Percussion is weakly positive.
Additional special methods include determining the electrical excitability of the pulp (reduced to 200 μA), determining occlusion (the presence or absence of a traumatic factor), fistula tract, and temperature tests.
NB! We definitely do an X-ray examination.

Treatment of chronic apical periodontitis, traumatic and medicinal periodontitis
After diagnosis, they begin to draw up a treatment plan for chronic apical periodontitis, based on clinical and radiological data.
Treatment of traumatic periodontitis begins with identifying and eliminating the traumatic factor.
Treatment of medicinal periodontitis consists of antiseptic treatment of the root canal system, refilling when a foreign body is detected in the apical periodontium. When exposed to aggressive liquids outside the apex, a cotton ball is placed on the orifice or a cotton swab moistened with an antidote is placed in the canal (for example, for arsenic anhydride, the antidote is 5% unithiol solution or 2-3% iodine tincture). With arsenic periodontitis there is pain syndrome when biting on a tooth, from the mucous membrane there are rarely pathological changes.
When sodium hypochlorite is removed beyond the apex, sharp bursting pain, bruising, and swelling on the affected side are observed. The root canals are washed abundantly with saline solution, the area of the root apex is injected with saline solution in an amount 10 times greater than the volume of hypochlorite. Filling begins at next visit in the absence of progression of the pathological process.
Antibiotics, anti-inflammatory and antihistamines are prescribed.
Common among the treatments for all types of apical periodontitis is endodontic treatment of the causative tooth.

The article was written by O. Vishnyak. Please, when copying material, do not forget to provide a link to the current page.
Chronic Apical Periodontitis-Clinic Diagnostics Treatment updated: April 30, 2018 by: Valeria Zelinskaya
Inflammatory processes in the periodontal tissues of the pre-root area of dead teeth are painful and dangerous pathology– acute apical periodontitis. In this case, even the slightest impact on the tooth causes severe pain.
The disease is almost always a complication of ordinary caries, caused by inflammation of the pulp followed by necrosis of the latter. This is due to special microorganisms that from the tooth, penetrating deeper into the canal, eventually transfer to the jaw tissue. Unfortunately, the localization of the disease is rarely limited to the periodontal ligaments; it also destroys the root and alveolar bone.
Classification and reasons
The classification of the disease is based on the causes of its occurrence. On this moment There are the following types:
- Infectious - a consequence of delayed treatment of caries. In addition, development can be provoked by the destructive activity of staphylococci, streptococci or any other infectious pathogens in areas adjacent to the tooth, for example, maxillary sinuses. The pulp and nerve die from such activity. The method of penetration of infectious pathogens makes it possible to separate this type diseases into two subtypes - intradental (intradental) and extradental (extradental). Periodontitis, caused by the progression of inflammation of nearby tissues (sinusitis, etc.), belongs to the last subtype.
- Medication- the development is caused by doctors’ mistakes in the treatment of pulpitis. Strong drugs (highly toxic antiseptics) or irritating materials, penetrating during endodontic procedures, can cause serious problems in the periodontium. inflammatory reaction. Allergic periodontitis, capable of an immunological reaction, is considered a medicinal type.
- Traumatic - a strong single or chronic injury is a provoking factor. The process itself is almost always acute.
It should be added that infectious acute apical periodontitis most often occurs in children.
Pathogenesis
Initially, the occurrence of serious inflammatory process in the near-dental area begins due to the entry of microbes through the apical foramen of the root or from the periodontal pocket.
Damage to the apical area is possible due to pathological transformation (necrosis) of the pulp, during the penetration of infected microflora of the dental canal into the periodontal tissue. It happens that rotted particles are pushed out of the canal into the gum when a person chews food.
In the causative tooth is born strong pain, which intensifies when chewing or any other external influence on the chewing (cutting) surface. The patient experiences a sensation of transformation (change in size) of the tooth.
Over time, the pain becomes stronger, does not stop, and if it does stop, it is for a very long time. short term. It is often pulsating. Biting, the patient changing body position, touching a sore spot, or exposure to heat make the pain more intense. The pain spreads through the branches trigeminal nerve. The patient's state of health is assessed as normal.

Symptoms of the pathology: acute apical periodontitis
Acute apical periodontitis, of pulpal origin or any other, is characterized by non-stop severe local pain. Painful sensations weakly expressed, aching, localized in the area of the causative tooth. Then the pain intensifies, begins to tear and pulsate, and at times radiates. The last fact is a sign of the beginning purulent inflammation. The duration of this process is 2 - 14 days. The course of acute periodontal inflammation can be divided into two phases (stages):
- Infection of the gum tissue around the root. At this time, prolonged, continuous, aching pain appears. It happens that all this is accompanied hypersensitivity to chewing and biting. There are no visual pathologies observed on the gum itself, however, with vertical tapping, increased sensitivity is recorded.
- At the next stage of development, the inflammatory process takes on a pronounced exudative form, characterized by constant pain. It always hurts from everything. From biting, from touching, from tapping. Irradiation is recorded. The resulting exudate in tandem with acidosis provokes swelling and destruction of the gums, which weakens the fixation of the tooth, making it mobile. An increase in the localization of serous (purulent-serous) infiltrate is accompanied by the formation of edema and the reaction of the lymph nodes. The patient is not feeling well, he has general malaise, leukocytosis, elevated temperature and headaches.
Diagnosis of periodontitis
The clinic of acute apical periodontitis, coupled with examination data, are the key components correct diagnosis the disease in question. Electrical odongometric examination and thermal stimuli make it possible to determine the degree of pulp necrosis.
In this case, X-ray is practically ineffective; it rarely detects pathological changes in the gum tissue even at the stage of an acute inflammatory process. The maximum he can do is identify an increase in the periodontal fissure, insignificant changes in the structure of the alveoli.
Exacerbation of the disease leads to changes in the body similar to those that occur with granulating, granulomatous periodontitis. The blood traditionally does not change; in some cases, leukocytosis was recorded (in the region of 9 - 109/l), insignificant neutrophilia due to leukocytes (segmental, rod-nuclear). ESR traditionally does not deviate from the norm.
Let's take as an example acute apical periodontitis of pulpal origin, the development history of which is similar to other types of periodontitis. It is treated in several stages by a dentist. First surgically intensive discharge of purulent-serous exudate is ensured, which eliminates inflammation.
The patient undergoes physical therapy and is prescribed rinsing the mouth with heated mineral water. In parallel, a course of treatment with antibiotics and sulfonamide drugs is carried out.
The treatment course ends with a filling. If the dentist determines that the treatment will not have an effect, or if the tooth cannot be properly sealed (ensure its tightness), then the latter must be removed.
Traditionally, people remember the dentist already in the acute form of the illness that has struck them. Immediate diagnosis of the pathology of acute apical periodontitis, associated with the most painful sensations, will simplify the doctor’s preparation of a course and implementation of treatment methods, and will help the patient recover quickly.
Treatment of the disease in question is rarely complete without surgical intervention(tooth extraction). However, today's medicine is far from what it was 5-10 years ago. IN Lately There are more and more cases of successful treatment of periodontitis without surgery. The inflamed cavity is cleaned, the canals are healed, and strong drugs are widely used to control the infection.

Prevention of periodontitis
Qualified and not late conservative treatment illness acute apical periodontitis, differential diagnosis which is carried out in a timely manner, ends safely for the patient.
Neglect of one's health or the dentist's dishonesty can result in the progression of chronic processes. There are known cases of inflammation transferring from the gums to the jaw bone and soft tissues.
In order not to bring the matter to medical intervention, it is advisable not to neglect basic prevention, which includes:
- sanitation of the oral cavity;
- unloading of teeth through orthopedic treatment methods;
- personal hygiene;
- health activities.
The diagnosis of chronic apical periodontitis threatens those who ignore the acute form of the disease. Many suffer pain under painkillers. And after waiting for the asymptomatic course of the disease, they believe that it has passed. This misconception can lead to serious consequences, which are more difficult and expensive to get rid of. Sometimes the chronic form occurs on its own. In any case, the pathology requires medical intervention.
Periodontitis is an inflammation of the periodontium, a complex of tissues surrounding the tooth root. The periodontium consists of connective fibers and root sheath.
The periodontium connects the teeth with the dental sockets - alveoli, distributes the load between them and reduces the pressure on the jaw apparatus. Damage to periodontal tissue can lead to tooth loss and further damage to the jaw structure.
The source of inflammation can be localized along the tooth root - marginal periodontitis. Or form under the apical foramen at the root apex. Through it, nerves and vessels connect to the pulp - soft cloth tooth

In the latter case, the pathology is called apical or apical periodontitis. We will consider the chronic course of this type of disease.
Two development paths
The disease begins with acute form, which we talked about in the article. Without treatment, after one to two weeks the pathology takes on a chronic form.
Chronic apical periodontitis can occur independently, without acute stage. This occurs with prolonged low-intensity action on the periodontium. Examples:
- chronic pulpitis, slowly destroying both pulpal and periodontal tissues;
- chronic inflammation of tissues adjacent to the periodontium: nasal sinuses, jaw bone, gums;
- consequences of a blow to the periodontal area;
- tooth root crack;
- long-term exposure to toxic filling material, potent medications: antibiotics, antiseptics, arsenic pastes;
- damage to periodontal tissue during treatment or expansion of tooth root canals during the treatment of pulpitis - inflammation of the pulp;
- prolonged pressure of the crown, pin, veneer, implant;
- allergic reaction to drugs, filling material;
- general allergy when the body reacts to an overdose of drugs or the introduction of a foreign gene.
General clinical picture
Manifestations of periodontitis with chronic course almost invisible. The fact that the disease continues to develop is indicated by a slight tingling pain when chewing solid foods. From time to time, discomfort is felt inside the damaged tooth. In some cases, there may be no discomfort.

Changes in periodontal tissues are accompanied by persistent putrid smell from the mouth and darkening of tooth enamel. It becomes dark gray, sometimes with a blue tint. Around the diseased tooth there is slight swelling gums
Exudate outflow
A sure sign of the disease is a fistula opening on the neck, cheek, nose or mouth. Exudate flows through it - liquid formed from inflamed periodontal tissues. It is its outflow that dulls the pain.
There are three types of chronic disease: granulating, granulomatous, fibrous. Separate view highlight an exacerbation of the pathology, which we discussed in the article.
Granulating and granulomatous varieties
When granulating apical disease appears, mild pain is felt in the area of the damaged tooth. It can burst from the inside. The gums around the tooth turn red due to blood flow. Periodontal tissue is gradually replaced by granulating tissue, part of which exits through the fistula opening along with exudate. In the article you will find full information about this form of the disease.

Fibrous variety
The apical fibrous course of the pathology is accompanied by a change in the color of the tooth enamel and a specific odor from the mouth, which is emitted by dead periodontal tissue. By the time the fibrous variety develops, the fistula opening most often closes.
The absence of other signs and symptoms makes chronic fibrous periodontitis difficult to diagnose. Moreover, he is similar clinical picture with chronic gangrenous pulpitis.
The asymptomatic occurrence of a variety does not make it harmless. Pathogenic microorganisms that influence periodontal inflammation or appear during the development of the disease can at any time “move” into neighboring tissues and cause other pathologies: suppuration, inflammation with tissue death and exfoliation, destruction of the jaw bone and nasal cartilage.

Research by scientists
Against the background of the development of infectious or viral diseases (influenza, chickenpox, ARVI, AIDS, meningitis, dysentery) weakens protective system body. As a result, inflammation can occur near several apical foramina at once. Massive periodontal damage risks leading to the loss of several teeth at once.
Numerous studies by scientists have shown that patients who were missing many of their own teeth are most often at risk of endocrine and cardiovascular diseases. Unlike patients with a complete dentition.
Thorough diagnosis
To prescribe treatment, the dentist must establish a reliable diagnosis. Diagnostics begins with the collection of general data. The doctor is interested in what symptoms the patient feels, whether he has additional diseases, whether he has previously visited a dentist or periodontist, for what reasons, and whether there has been any impact on a suspicious tooth.
Next, the dentist examines appearance patient: facial symmetry, skin condition and color. Checks whether full opening of the mouth is possible. Feels the lymph nodes under the jaw. Special attention pays attention to the mucous membranes of the oral cavity and the condition of the entire dentition.
Radiography
Radiography allows one to distinguish between types of chronic periodontitis. On an x-ray, the granulating variety appears as a vague darkening near the apex of the tooth root. The granulomatous focus of inflammation has a round shape and clear boundaries. Expansion of the apical part of the periodontium in the form of an elongated darkening on x-ray is a sign of the fibrous variety.

Elongated darkening is a sign of the fibrous form
Diagnosis is complemented by electroodontometry (ED) and general analysis blood. EDI readings at chronic form pathologies range from 100 to 160 microamps.
Dental care
Treatment of the disease takes place in several stages. The first step is to carry out local anesthesia. One or more injections are made near the nerve needed to block. Possible “freezing” of the trigeminal nerve.
For anesthesia, high-quality and potent anesthetics are used: “Prilocaine”, “Buvicaine”, “Articaine”. To prolong the analgesic effect and reduce the absorption of the anesthetic into the blood, it can be combined with adrenaline.
You need to know this
If the patient is very nervous, he is given a sedative or put into a drowsy state with the help of a small amount of drugs used for general anesthesia– sedation method. Before this procedure, you need to undergo tests to identify possible allergies.
You should not use sedatives or painkillers on your own before going to the dentist. Only a specialist should select the appropriate remedy and prescribe the dosage. If you take anything, you must notify your doctor. Otherwise, there may be side effects, including cardiac arrest.
Tooth treatment and disinfection
As soon as the anesthesia takes effect, mechanical treatment of the diseased tooth begins. To get to the pulp, the filling is removed and damaged and healthy dental tissues are drilled. The pulp chamber is opened and the pulp is removed.

The root canals of the tooth are expanded with k-files or niti-files - hand-held cutting dental endodontic instruments. The treated canals are disinfected with antiseptic preparations and an ultrasonic device - a scaler.
Double strike on inflammation
Then special self-absorbing pastes are placed at the end of the canals, which fight inflammation and stimulate periodontal restoration. The tooth is covered with a temporary filling. Treatment in this way lasts several days, depending on the level of periodontal damage.
Secure the effect from medicinal paste Home therapy will help: rinsing with Chlorhexidine, Dimexide, decoctions of sage, oak bark, yarrow, alcohol tincture of propolis. We described how to conduct self-therapy in the article.
Physiotherapeutic procedures
After the appointed period, radiography is performed to assess the condition of periodontal tissues. If necessary, physiotherapeutic procedures are prescribed.
Laser therapy helps to increase the level of oxygen supply and start metabolism in periodontal cells, eliminate inflammation, relieve swelling, and heal tissue. Contraindications: malignant and benign tumors, diabetes, cardiac and pulmonary pathologies, nervous system problems.

Good results are obtained by galvanization - therapy with direct electric current up to 50 microamps with a voltage of 30-80 volts. It allows you to stimulate blood circulation in periodontal cells, improve tissue nutrition, get rid of inflammation, and restore the conductivity of nerve elements. Contraindications: tumors, pregnancy, epilepsy, acute skin dermatitis, diseases of the blood, heart, brain, nervous system.
The final stage
In addition to physiotherapy, antibiotics are prescribed: Tetracycline, Doxycycline, Amikacin, antimicrobial agents: “Nitroxoline”, “Formidron”, “Ethacridine lactate”. You can take any medications only on the recommendation of a dentist or therapist.
At favorable outcome The treatment is completed with careful filling of the root canals. Gutta-percha pins are installed in them and sealer, a root filling material, is compacted tightly. Then the tooth is closed permanent filling. To give the tooth an anatomical shape, the filling is ground and polished. It is mandatory to evaluate the work using a control x-ray.
Emergency measures
If it is not possible to suppress the inflammation or irreversible changes have occurred in the apical part of the tooth root, emergency measures are resorted to.

The end of the tooth root is surgically removed. If the pathology is complicated by the appearance of a hilar cyst, it is removed along with part of the root. Postoperative procedures are prescribed: disinfectant rinses, healing and restorative procedures. If after the operation the fixation of the tooth is broken, it is removed.
If you have anything to add to the article, please leave a comment.