> X-ray (pyelography) of the kidneys, types of pyelography
This information cannot be used for self-medication!
Consultation with a specialist is required!
What is pyelography and how is it performed?
Pyelography is an X-ray examination of the kidneys with pre-filling urinary tract contrast agent. Using pyelography, the size, shape, location of the calyces and pelvis of the kidneys, the structure and function of the ureters are assessed.
Most often, retrograde (ascending) pyelography is performed. In this case, the contrast agent is injected through the ureter using a catheterization cystoscope. Antegrade (descending) pyelography is usually used in cases where, due to obstruction of the ureter, it is impossible to administer contrast through it, or when the patient has contraindications to cystoscopy. In the descending version of the study, contrast is injected directly into the renal collecting system by puncture or by installing a drainage.
The contrast can be a liquid, a gas (pneumopyelography), or both at the same time (double contrast).
Indications for pyelography
Pyelography is prescribed to confirm the diagnosis of hydronephrosis, pyelonephritis, urolithiasis or cancer. The images visualize tumors, stones, blood clots and other obstacles to the passage of urine. The study helps surgeons plan the course of the upcoming operation.
Who sends you for the study, and where can you get it?
Nephrologists, urologists, oncologists, and surgeons refer for pyelography. It is advisable to undergo it in a therapeutic or diagnostic medical center, equipped with an X-ray machine and specializing in the diagnosis and treatment of pathologies of the urinary organs.
Contraindications for pyelography
The study is contraindicated when hypersensitivity to contrast and during pregnancy. The retrograde technique is not used in cases of impaired patency of the ureters, insufficient bladder capacity, hematuria (presence of blood in the urine), and the antegrade method is not used in cases of blood clotting disorders.
Preparation for pyelography
Method of performing pyelography
When performing retrograde pyelography, the patient lies on a special table with knees and knees bent. hip joints legs, the position of which is fixed with special stirrups. After preliminary anesthesia, the doctor injects bladder cystoscope, and through it to the level renal pelvis– a special catheter. Under X-ray control A contrast agent is slowly injected through the catheter. When the required filling of the collecting system is achieved, radiographs are taken in the anteroposterior projection, and in some cases additionally in semilateral and lateral projections.
When performing antegrade pyelography, the patient lies on a special table with his back up. After preliminary local anesthesia the doctor inserts a needle into the collecting system (below the level of the 12th rib) to a depth of approximately 7–8 cm and connects a flexible tube to it. Under fluoroscopic control, a contrast agent is injected through it. Then radiographs are taken in posteroanterior, anteroposterior and semilateral projections.
Interpretation of pyelography results
Normally, the passage of the contrast agent through the catheters occurs without difficulty, the calyces and pelvis of the kidneys fill quickly, have smooth, clear contours and normal sizes. Kidney mobility (assessed during inhalation and exhalation) should not be more than 2 cm.
Incomplete filling of the upper urinary tract with contrast, its dilation, and delayed emptying after catheter removal indicate the presence of a tumor, stone, or other obstruction. Impaired kidney mobility may indicate pyelonephritis, paranephritis, tumor or kidney abscess. With hydronephrosis, the renal collecting system dilates.
The results of the study (images and the radiologist’s report) should be shown to the doctor who referred for pyelography.
Antegrade pyelography - x-ray method studies of the upper urinary tract, based on the direct introduction of a contrast agent into the renal pelvis either by percutaneous puncture or through pyelo-(nephrostomy) drainage. Consequently, there are two types of antegrade pyelography: antegrade percutaneous pyelography and antegrade pyelography with the introduction of a contrast agent through the pyelostomy. While antegrade pyelography by introducing a contrast agent into the pelvis through a pyelo-(nephrostomy) has been used for a long time, percutaneous puncture pyelography has found its use relatively recently.
The first report on puncture of the renal pelvis with filling it with contrast fluid and immediate pyelography was made by Kapandi in 1949, and Ainsworth and Vest in 1951 proposed using this method in urological practice. In the USSR, the first report on the use of antegrade percutaneous pyelography was made by A. Ya. Pytel in 1956 at All-Russian Conference radiologists and radiologists in Moscow and they introduced this method into our practice. Antegrade percutaneous pyelography is indicated in those difficult cases when other methods urological examination do not allow to recognize diseases of the kidneys and upper urinary tract. This primarily applies to those diseases in which the excretory urogram does not show the release of a contrast agent as a result of impaired renal function, and retrograde pyeloureterography cannot be performed due to the presence of a small bladder capacity, ureteral obstruction (stone, stricture, obliteration, tumor, periureteritis and etc.). Puncture percutaneous antegrade pyelography is indicated mainly for hydronephrosis, hydroureter, or when these diseases are suspected, when other research methods do not allow a correct diagnosis.
Using percutaneous antegrade pyelography in such cases, it is possible not only to recognize hydronephrosis, but also to find out its cause (stricture, stone, tumor). By combining antegrade pyelography with urokymography, it is possible to obtain an idea of the motor function of the upper urinary tract, which is important for deciding the feasibility of a particular plastic surgery.
Sometimes only thanks to antegrade pyelography it is possible to recognize a neoplasm of the pelvis or a tumor implant in the ureter (Goodwin, 1956; A. Ya. Pytel, 1958; Granone, 1961; Brazilay et al., 1961). Further, antegrade pyelography is indicated in cases where other research methods cannot accurately determine the level of ureteral stenosis, as well as the extent of ureteral obliteration or stricture, which is very important for deciding the type and nature of the upcoming reconstructive operation.
Before antegrade pyelography, a survey image and excretory urography are performed, since with their help the contours of the kidney can be identified, and with some preservation of kidney function, the shadow of the pelvis. Evaluation of these preliminary radiographs regarding the size, shape and position of the kidney can be significant in choosing the site of pelvic puncture.
The patient is placed (on his stomach) on an X-ray table (some foreign urologists perform a puncture of the pelvis with the patient in a sitting position, which we do not recommend). Lumbar puncture of the renal pelvis is performed under local novocaine anesthesia; anesthetize the skin and underlying muscles through which the puncture needle will be passed. Under the XII rib, retreating to the right or left 10-12 cm outward from the midline of the spine, the skin and underlying tissues are pierced with a needle (diameter 1-1.5 mm) in the direction from the outside to the inside and upward towards the medial third of the normally located kidney. If the patient’s kidney is significantly enlarged and therefore can be easily palpated, then it should be punctured in the middle part, medial from its longitudinal axis. Gradually inserting a needle deep into the tissues of the lower back and creating a vacuum with a syringe, usually at a depth of 9-12 cm (depending on the patient’s fatness and thickness abdominal wall) puncture the renal pelvis (Fig. 56). As soon as the needle penetrates the pelvis, its contents appear in the syringe - either pure urine, or urine mixed with pus, blood, etc. If urine does not appear in the syringe, you should immediately take an x-ray, which will help you navigate needle location.
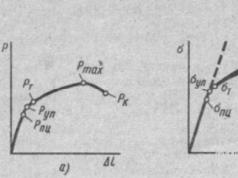
Rice. 56. Scheme of puncture of the renal pelvis for antegrade pyelography.
For better orientation and obtaining data on the functional capacity of the kidney, it is advisable to administer 5 ml of 0.4% indigo carmine solution intravenously 10 minutes before puncture of the renal pelvis. The appearance of blue-colored liquid in the syringe indicates a correctly performed puncture and the preserved functional ability of the kidney.
Urine is aspirated from the pelvis and sent for microscopy and bacteriological examination. Then 10-20 ml of a 40-50% solution of sergosine, triyotrast or cardiotrust is injected into the pelvis and the contents of the pelvis are mixed with the contrast agent by moving the syringe piston. After this, X-rays are taken in the prone position. If necessary they do x-rays on the side and in vertical position sick. In the presence of hydronephrosis, it is very large sizes It may be necessary to inject a larger amount of contrast agent into the pelvis (Fig. 57, 58, 59).
However, the amount of contrast agent administered should be 5-10 ml less than the amount of urine aspirated from the renal pelvis. This condition must be strictly observed, since overstretching of the pelvis is dangerous because the resulting significant increase in intrapelvic pressure can cause pyelo-renal reflux and lead to serious complications.
At the end of the study, its contents are aspirated from the pelvis with a syringe, and in the case of infected hydronephrosis, antibiotics are injected into the pelvis after urine is removed. Some foreign urologists remove the needle immediately after introducing a contrast agent into the pelvis, even before the image, and do not aspirate the contents of the pelvis after the X-ray. Using this technique, they observed no complications.
Having experience in performing antegrade percutaneous pyelography in 78 patients, we have never observed any serious complications. This is also supported by literature data from recent years. However, it must be borne in mind that in the first years of the introduction of this method into practice by foreign urologists, complications such as perforation were observed during puncture of the renal pelvis renal parenchyma, trauma to the kidney vessels, erroneous puncture of the liver and spleen. However, if a small-diameter needle is used to puncture the pelvis, usually no serious complications or consequences are observed even with accidental puncture of these organs.
It should be borne in mind that antegrade percutaneous pyelography cannot always be performed, since there may be cases when it is not possible to puncture the pelvis. Thus, Casey and Goodwin (1955) reported that in 7 out of 55 patients they were unable to puncture the pelvis. Among 86 patients, we were unable to puncture the pelvis in 8 people, and in 78 patients the puncture of the pelvis was performed easily. For percutaneous antegrade pyelography, gas (oxygen, carbon dioxide) can be used instead of liquid contrast agents; This study is called antegrade pneumopyelography.
In addition to percutaneous puncture antegrade pyelography, there is antegrade pyelography, when a contrast agent is injected into the pelvis via pyelo-(nephrostomy) drainage. This research method is used in postoperative period; its results allow us to judge the morphological and functional state upper urinary tract: the size of the pelvis and calyces, their tone, the degree of disruption of the passage of urine from the pelvis to the bladder through the ureter and its causes, as well as identify stones that were not accidentally removed during surgery, the location and extent of the ureteral stricture, etc. When If the patient has a pyelostomy (nephrostomy), it should be used to perform antegrade pyelography. This simple research method makes it possible to very often identify certain urinary passage disorders and promptly undertake the necessary treatment.
Antegrade pyelography is usually performed no earlier than 14-15 days after surgery. The peripheral end of the pyelo-(nephrostomy) drainage tube is treated with alcohol and its lumen is closed with a clamp; centrally to the latter, a drainage tube is punctured, through which a contrast agent is injected (usually 6-8 ml). It is impossible to overstretch the pelvis due to the possibility of pyelo-renal reflux and an outbreak of pyelonephritis. After the contrast agent is injected into the pelvis, the patient must take several deep breaths and exhales, and then an X-ray is taken.
With good tone of the upper urinary tract, usually within a minute the contrast agent moves through the ureter. If the tone of the upper urinary tract has not yet been restored, which is expressed in a decrease in the motor function of the calyces, pelvis and ureter, the contrast agent penetrates the ureter no earlier than 3-4 minutes. Determining the degree of tone of the upper urinary tract allows the doctor to decide on the time to remove the patient's drainage tube from the kidney and close the nephrostomy. It should be borne in mind that in order to obtain a true picture of the condition of the upper urinary tract on an antegrade pyelogram, the pressure in the renal pelvis when a contrast solution is introduced into it must be threshold, i.e., such that the opening of the ureteropelvic segment occurs and the contrast agent moves along ureter. Because the threshold pressure in the renal pelvis is very close to the pressure above which pyelorenal reflux occurs, it is necessary to very carefully inflate the pelvis during antegrade pyelography. The patient develops a feeling of heaviness and the slightest aching pain in the lower back with the introduction of a contrast agent indicates that the pressure in the renal pelvis is higher than permissible and, therefore, is not indifferent. When performing antegrade pyelography, the patient should not experience discomfort. In order to avoid an increase in intrapelvic pressure above the permissible level during antegrade pyelography, we suggest using a syringe without a piston. The contrast agent from such a syringe penetrates into the pelvis under the influence of gravity and, upon reaching a threshold pressure, its flow stops. After the renal pelvis is emptied and the pressure in it decreases, the flow of contrast agent into it from the syringe is resumed. This technique allows you to set the capacity of the pelvis, avoid sharp increase pressure in it and, therefore, prevents the occurrence of pyelorenal reflux and other complications.
Antegrade percutaneous pyelography is also used in children. A. Yu. Svidler and L. I. Sneshko (1961) reported the results of antegrade pyelography in 10 children aged 8 months to 10 years with renal polycystic disease, hydronephrosis of a dystopic kidney, hydronephrosis due to ureteral achalasia and closed pyonephrosis of tuberculous origin. Of the 10 patients, only one developed a small subcutaneous abscess at the puncture site. The authors believe that antegrade percutaneous pyelography in children, being a safe method, can be used successfully in some urological diseases.
Using both antegrade percutaneous pyelography and pyelography with the introduction of a contrast agent through the pyelo-(nephrostomy) stoma, we have repeatedly observed a peculiar phenomenon - an excretory urogram on the opposite side. Approximately 15-20 minutes after the introduction of a contrast agent into the pelvis of the kidney under study, shadows of the contrast agent appear on the opposite side, which fills the pelvis and calyces of the kidney. This phenomenon indicates the preservation of the fornical apparatus of the kidney under study, which ensures the absorption of the contrast agent into the general circulation followed by its subsequent release by the other kidney. This phenomenon, confirming the good functioning of the renal parenchyma on the opposite side, has important in assessing the indications for appropriate surgical interventions.
Antegrade percutaneous pyelography is very valuable for appropriate indications diagnostic method. Antegrade pyelography with the introduction of a contrast agent through the pyelo-(nephrostomy) is of equally great value. Antegrade pyelography does not replace, but complements the basic methods of X-ray diagnosis of diseases of the kidneys and upper urinary tract. However, in some patients, antegrade pyelography is the only research method that allows one to correctly recognize the disease.
Urostereoradiography is a method of radiopaque examination of the urinary tract using stereoscopy.
The technique of this study consists of taking two images (after filling the urinary tract with a contrast agent) with the X-ray tube shifted in both directions by a distance of 3-3.5 cm, i.e. 6-7 cm, all other conditions being equal. Both x-rays, taken at the angle of vision of the eyes, are examined using a special stereo-negatoscope or stereo binoculars. The difficulty in obtaining perfectly identical two radiographs lies in the existence of dynamic changes in the urinary tract that occur during the time from the first to the second image. This circumstance makes it difficult to obtain a clear stereoscopic effect. However, despite this, urostereography can be very valuable in diagnosis various kinds urological sufferings such as nephrolithiasis, hydronephrosis, tuberculosis, tumors of the calyces and renal pelvis. Urostereoradiography allows us to establish a more accurate localization of the disease process in the kidney, such as: tuberculous cavity, stone, tumor, which is very important for selection surgical method treatment, especially organ-preserving treatment.
Antegrade pyelography
Antegrade pyelography is an x-ray method for studying the upper urinary tract, based on the direct introduction of a contrast agent into the renal pelvis either by percutaneous puncture or through pyelo-(nephrostomy) drainage. Consequently, there are two types of antegrade pyelography: antegrade percutaneous pyelography and antegrade pyelography with the introduction of a contrast agent through the pyelostomy. While antegrade pyelography by introducing a contrast agent into the pelvis through a pyelo-(nephrostomy) has been used for a long time, percutaneous puncture pyelography has found its use relatively recently.
The first report on puncture of the renal pelvis with filling it with contrast fluid and immediate pyelography was made by Kapandi in 1949, and Ainsworth and Vest in 1951 proposed using this method in urological practice. In the USSR, the first report on the use of antegrade percutaneous pyelography was made by A. Ya. Pytel in 1956 at the All-Russian Conference of Radiologists and Radiologists in Moscow, and he introduced this method into our practice. Antegrade percutaneous pyelography is indicated in those difficult cases when other methods of urological examination do not allow the recognition of diseases of the kidneys and upper urinary tract. This primarily applies to those diseases in which the excretory urogram does not show the release of a contrast agent as a result of impaired renal function, and retrograde pyeloureterography cannot be performed due to the presence of a small bladder capacity, ureteral obstruction (stone, stricture, obliteration, tumor, periureteritis and etc.). Puncture percutaneous antegrade pyelography is indicated mainly for hydronephrosis, hydroureter, or when these diseases are suspected, when other research methods do not allow a correct diagnosis.
Using percutaneous antegrade pyelography in such cases, it is possible not only to recognize hydronephrosis, but also to find out its cause (stricture, stone, tumor). By combining antegrade pyelography with urokymography, it is possible to obtain an idea of the motor function of the upper urinary tract, which is important for deciding the feasibility of a particular plastic surgery.
Sometimes only thanks to antegrade pyelography it is possible to recognize a neoplasm of the pelvis or a tumor implant in the ureter (Goodwin, 1956; A. Ya. Pytel, 1958; Granone, 1961; Brazilay et al., 1961). Further, antegrade pyelography is indicated in cases where other research methods cannot accurately determine the level of ureteral stenosis, as well as the extent of ureteral obliteration or stricture, which is very important for deciding the type and nature of the upcoming reconstructive operation.
Before antegrade pyelography, a survey image and excretory urography are performed, since with their help the contours of the kidney can be identified, and with some preservation of kidney function, the shadow of the pelvis. Evaluation of these preliminary radiographs regarding the size, shape and position of the kidney can be significant in choosing the site of pelvic puncture.
The patient is placed (on his stomach) on an X-ray table (some foreign urologists perform a puncture of the pelvis with the patient in a sitting position, which we do not recommend). Lumbar puncture of the renal pelvis is performed under local novocaine anesthesia; anesthetize the skin and underlying muscles through which the puncture needle will be passed. Under the XII rib, retreating to the right or left 10-12 cm outward from the midline of the spine, the skin and underlying tissues are pierced with a needle (diameter 1-1.5 mm) in the direction from the outside to the inside and upward towards the medial third of the normally located kidney. If the patient’s kidney is significantly enlarged and therefore can be easily palpated, then it should be punctured in the middle part, medial from its longitudinal axis. Gradually inserting a needle into the depths of the lumbar tissue and creating a vacuum with a syringe, usually at a depth of 9-12 cm (depending on the patient’s fatness and the thickness of the abdominal wall), the renal pelvis is punctured (Fig. 56). As soon as the needle penetrates the pelvis, its contents appear in the syringe - either pure urine, or urine mixed with pus, blood, etc. If urine does not appear in the syringe, you should immediately take an x-ray, which will help you navigate needle location.
Rice. 56. Scheme of puncture of the renal pelvis for antegrade pyelography.
For better orientation and obtaining data on the functional capacity of the kidney, it is advisable to administer 5 ml of 0.4% indigo carmine solution intravenously 10 minutes before puncture of the renal pelvis. The appearance of blue-colored liquid in the syringe indicates a correctly performed puncture and the preserved functional ability of the kidney.
Urine is aspirated from the pelvis and sent for microscopic and bacteriological examination. Then 10-20 ml of a 40-50% solution of sergosine, triyotrast or cardiotrust is injected into the pelvis and the contents of the pelvis are mixed with the contrast agent by moving the syringe piston. After this, X-rays are taken in the prone position. If necessary, X-rays are taken on the patient's side and in an upright position. If hydronephrosis is very large, it may be necessary to inject a larger amount of contrast agent into the pelvis (Fig. 57 , 58 , 59 ).
|
|
Rice. 57. Ureterogram. Male 28 years old. Ureteral obstruction. Filling defect of the lower third of the ureter (see fig. 58 ). |
|
|
Rice. 58. Antegrade pyelogram. Male 28 years old. Giant hydronephrosis due to soil varicose veins vein system v. spermatica int. Nephrectomy. Recovery (see fig. 57 ). |
|
|
Rice. 59. Antegrade pyelogram. Male 47 years old. Obliteration of the ureter. Calculous hydronephrosis. Nephrectomy. Recovery. |
However, the amount of contrast agent administered should be 5-10 ml less than the amount of urine aspirated from the renal pelvis. This condition must be strictly observed, since overstretching of the pelvis is dangerous because the resulting significant increase in intrapelvic pressure can cause pyelo-renal reflux and lead to serious complications.
At the end of the study, its contents are aspirated from the pelvis with a syringe, and in the case of infected hydronephrosis, antibiotics are injected into the pelvis after urine is removed. Some foreign urologists remove the needle immediately after introducing a contrast agent into the pelvis, even before the image, and do not aspirate the contents of the pelvis after the X-ray. Using this technique, they observed no complications.
Having experience in performing antegrade percutaneous pyelography in 78 patients, we have never observed any serious complications. This is also supported by literature data from recent years. However, it must be borne in mind that in the first years of the introduction of this method into practice by foreign urologists, complications such as perforation of the renal parenchyma, trauma to the kidney vessels, and erroneous puncture of the liver and spleen were observed during puncture of the renal pelvis. However, if a small-diameter needle is used to puncture the pelvis, usually no serious complications or consequences are observed even with accidental puncture of these organs.
It should be borne in mind that antegrade percutaneous pyelography cannot always be performed, since there may be cases when it is not possible to puncture the pelvis. Thus, Casey and Goodwin (1955) reported that in 7 out of 55 patients they were unable to puncture the pelvis. Among 86 patients, we were unable to puncture the pelvis in 8 people, and in 78 patients the puncture of the pelvis was performed easily. For percutaneous antegrade pyelography, gas (oxygen, carbon dioxide) can be used instead of liquid contrast agents; This study is called antegrade pneumopyelography.
In addition to percutaneous puncture antegrade pyelography, there is antegrade pyelography, when a contrast agent is injected into the pelvis via pyelo-(nephrostomy) drainage. This research method is used in the postoperative period; its results make it possible to judge the morphological and functional state of the upper urinary tract: the size of the pelvis and calyces, their tone, the degree of disturbance in the passage of urine from the pelvis to the bladder through the ureter and its causes, as well as to identify stones that were not accidentally removed during surgery, the location and the extent of the ureteral stricture, etc. If the patient has a pyelostomy (nephrostomy), it should be used to perform antegrade pyelography. This simple research method makes it possible to very often identify certain urinary passage disorders and promptly undertake the necessary treatment.
Antegrade pyelography is usually performed no earlier than 14-15 days after surgery. The peripheral end of the pyelo-(nephrostomy) drainage tube is treated with alcohol and its lumen is closed with a clamp; centrally to the latter, a drainage tube is punctured, through which a contrast agent is injected (usually 6-8 ml). It is impossible to overstretch the pelvis due to the possibility of pyelo-renal reflux and an outbreak of pyelonephritis. After the contrast agent is injected into the pelvis, the patient must take several deep breaths and exhales, and then an X-ray is taken.
With good tone of the upper urinary tract, usually within a minute the contrast agent moves through the ureter. If the tone of the upper urinary tract has not yet been restored, which is expressed in a decrease in the motor function of the calyces, pelvis and ureter, the contrast agent penetrates the ureter no earlier than 3-4 minutes. Determining the degree of tone of the upper urinary tract allows the doctor to decide on the time to remove the patient's drainage tube from the kidney and close the nephrostomy. It should be borne in mind that in order to obtain a true picture of the condition of the upper urinary tract on an antegrade pyelogram, the pressure in the renal pelvis when a contrast solution is introduced into it must be threshold, i.e., such that the opening of the ureteropelvic segment occurs and the contrast agent moves along ureter. Because the threshold pressure in the renal pelvis is very close to the pressure above which pyelorenal reflux occurs, it is necessary to very carefully inflate the pelvis during antegrade pyelography. The appearance of a feeling of heaviness and the slightest aching pain in the lower back in the patient during the administration of a contrast agent indicates that the pressure in the renal pelvis is higher than permissible and, therefore, is not indifferent. When performing antegrade pyelography, the patient should not experience any discomfort. In order to avoid an increase in intrapelvic pressure above the permissible level during antegrade pyelography, we suggest using a syringe without a piston. The contrast agent from such a syringe penetrates into the pelvis under the influence of gravity and, upon reaching a threshold pressure, its flow stops. After the renal pelvis is emptied and the pressure in it decreases, the flow of contrast agent into it from the syringe is resumed. This technique allows you to establish the capacity of the pelvis, avoid a sharp increase in pressure in it and, therefore, prevent the occurrence of pyelorenal reflux and other complications.
Antegrade percutaneous pyelography is also used in children. A. Yu. Svidler and L. I. Sneshko (1961) reported the results of antegrade pyelography in 10 children aged 8 months to 10 years with renal polycystic disease, hydronephrosis of a dystopic kidney, hydronephrosis due to ureteral achalasia and closed pyonephrosis of tuberculous origin. Of the 10 patients, only one developed a small subcutaneous abscess at the puncture site. The authors believe that antegrade percutaneous pyelography in children, being a safe method, can be used successfully in some urological diseases.
Using both antegrade percutaneous pyelography and pyelography with the introduction of a contrast agent through the pyelo-(nephrostomy) stoma, we have repeatedly observed a peculiar phenomenon - an excretory urogram on the opposite side. Approximately 15-20 minutes after the introduction of a contrast agent into the pelvis of the kidney under study, shadows of the contrast agent appear on the opposite side, which fills the pelvis and calyces of the kidney. This phenomenon indicates the preservation of the fornical apparatus of the kidney under study, which ensures the absorption of the contrast agent into the general circulation followed by its subsequent release by the other kidney. This phenomenon, which confirms the good functioning of the renal parenchyma on the opposite side, is important in assessing the indications for appropriate surgical interventions.
Antegrade percutaneous pyelography is a very valuable diagnostic method when indicated. Antegrade pyelography with the introduction of a contrast agent through the pyelo-(nephrostomy) is of equally great value. Antegrade pyelography does not replace, but complements the basic methods of X-ray diagnosis of diseases of the kidneys and upper urinary tract. However, in some patients, antegrade pyelography is the only research method that allows one to correctly recognize the disease.
Diagnostic errors, dangers and complications of antegrade pyeloureterography - abstract review of the book by Yu.A. Pytel and I.I. Zolotareva "Errors and complications in x-ray diagnostics" urological diseases".
Diagnostic errors, dangers and complications of antegrade pyeloureterography.
During antegrade pyeloureterography, a radiopaque substance is injected into the renal pelvis by percutaneous lumbar puncture or through pyelo(nephrostomy) drainage. There is also a method of percutaneous puncture of the renal parenchyma (nephrography), which is used extremely rarely. Percutaneous ategrade pyeloureterography was proposed more than 30 years ago, but has received more wide application V last years, when ultrasound-guided puncture of the pelvis was introduced into practice.
Antegrade pyeloureterography has limited diagnostic capabilities. It is not enough to just diagnose the disease. It is necessary to obtain information about the functional state of the kidney and upper urinary tract, about vascular architecture, which will allow determining the volume and nature of the surgical intervention.
Antegrade pyeloureterography, performed by introducing a contrast agent into the pelvis through a pyelo(nephrostomy) drainage, is more widely used. This study makes it possible in the postoperative period to determine the patency of the upper urinary tract, the shape and size of the collecting system, their tone, the location of the stone, the extent of ureteral stenosis, or to resolve the issue of the possibility of removing pyelo(nephrostomy) drainage if it has fulfilled its purpose.
Percutaneous antegrade pyeloureterography does not encounter difficulties with large kidney sizes, but puncture of the pelvis is very difficult or even impossible if the kidney is not enlarged. In cases where puncture of the pelvis is difficult, the contrast agent should be injected directly into the renal parenchyma, from where it penetrates into the pelvis through the canalicular route. In order to better judge the shape, size and position of the kidney, it is recommended to perform a puncture under the control of a fluoroscope, and if the contours of the kidney are not visible on a plain radiograph or excretory urogram, then after performing a pneumoren or pneumo-retroperitoneum. The technique of percutaneous puncture of the pelvis and, consequently, antegrade pyeloureterography has been simplified by performing it under ultrasound guidance. The information content of antegrade puncture pyeloureterography increases significantly if it is carried out under X-ray television control.
The indications for percutaneous antegrade pyelography are very limited. If there is advanced hydronephrotic transformation, a “switched off” kidney, or it is necessary to differentiate a tumor from a kidney cyst, then renal angiography is more appropriate, which will provide an idea not only of the state of the renal parenchyma, but also of the vascular architecture. The small diagnostic value of percutaneous antegrade pyelography lies in the fact that in most cases it is undertaken when the need for surgical treatment is beyond doubt.
When the cavity or cup is turned off, the needle may enter one of the isolated cavities, and a shadow of a single spherical formation appears on the radiograph, which leads to an erroneous diagnosis.
Due to the possibility of damage and infection by tuberculosis internal organs this method has not received recognition in phthisiourology. Patients with a disabled tuberculosis cavity are subject to surgical treatment. Pyelography allows you to assess the condition of the affected kidney without any risk and choose the method of operation.
Antegrade pyeloureterography by introducing a contrast fluid through a pyelo(nephrostomy) drainage deserves much more attention. To obtain a true image of the size and shape of the pyelocaliceal system and an idea of the tone of the ureter, when performing it, overdistension of the pelvis should be avoided, since the opening of the ureteropelvic segment depends on the intrapelvic-nocturnal threshold pressure. Exceeding it causes a short circuit in the segment. With a sharp increase in intrapelvic pressure, pelvic-renal refluxes and the danger of an attack of pyelonephritis occur.
At the time of administration of the contrast fluid, the patient should not experience pain or heaviness in the lumbar region, but, on the contrary, a sensation of fluid passing through the ureter. To avoid a sharp increase in intrapelvic pressure, the contrast agent should be injected with a syringe without a piston. In such cases, it enters the pelvis by gravity (the drainage tube and syringe are installed vertically), and when the threshold pressure is reached, the filling of the pelvis stops. It should be remembered that tight filling of the ureter with contrast fluid cannot in any way be identified with good functional ability upper urinary tract.
The kinetic capabilities of the ureter can be judged very relatively based on the data of an antegrade pyeloureterogram. The absence of a cystoid structure of the ureter indicates reduced tone of the upper urinary tract. Restoration of the tone of the upper urinary tract can only be determined by television pyeloscopy, when individual contractions of ureteral cystoids are noted.
Dangers and complications of percutaneous antegrade pyelography .
The risk of complications of percutaneous antegrade pyelography, according to the literature, is clearly underestimated. Some clinicians did not observe them, which may be explained by the small number of observations. Others are confident in the complete safety of the method. Still others indicate a small percentage of complications. N.V. Vasikhanov (1969) observed 43 different complications in 128 studies (hematuria in 21, increased body temperature in 16, injection of contrast fluid into the perinephric tissue in 5, injury colon in one patient), which means that complications are not so rare.
In reality, percutaneous antegrade pyelography is fraught with complications. There is a danger when puncturing the pelvis, and even more so when deliberately puncturing the renal parenchyma parenchymal bleeding with the formation of extensive perinephric and subcapsular hematomas, which require urgent lumbotomy. J. Popescu (1974) notes the formation of arteriovenous fistulas. There are known cases of rupture of the renal parenchyma. Even with successful antegrade pyelography, hematuria often occurs. More often, an increase in body temperature and extrarenal administration of contrast fluid are observed, and less commonly, the occurrence of paranephritis and subcutaneous abscesses. A dangerous complication is injury to the intestines and neighboring organs.
The risk of complications can be reduced if antegrade pyelography is performed immediately before surgery or puncture of the pelvis is performed under the control of ultrasound scanning.
We believe that the study has limited diagnostic value and must be used according to strict indications. The method is fraught with the risk of serious complications, and its low information content does not justify the risk. When performing antegrade pyelography through pyelostomy drainage, the most serious complication is a sharp increase in intrapelvic pressure.
Imaging techniques are often used to evaluate patients with nephrological and urological pathologies.
Plain radiography without contrast
X-ray abdominal cavity Without the use of radiopaque agents, it is practically useless in the diagnosis of nephrological and urological diseases. Such radiography is insensitive, capable of detecting only 50-60% kidney stones(calcium oxalate stones and rarely staghorn stones), detection of stone-like calcifications is also nonspecific.
X-ray using contrast
Images obtained after administration of water-soluble contrast agents allow visualization of the kidneys and collecting system. Currently, non-ionic isosmolar drugs (iohexol, iopamidol) are widely used; they have fewer side effects than the older hyperosmolar drugs, but still pose a risk of acute kidney injury (radiographic nephropathy).
In urography, the image is taken after intravenous, percutaneous antegrade or retrograde, or cystoscopic retrograde administration of a radiocontrast agent. The main contraindications for all patients are allergies to iodine and risk factors for radiocontrast nephropathy.
IVU (IV urography or pyelography). IVU has been widely replaced by the rapid introduction of multislice CT and MRI with and without contrast agents. During IVU, abdominal compression and increased intra-abdominal pressure may improve visualization of the renal pelvis and proximal ureters (if established), and distal sections ureters (after its removal). Additional radiographs at 12 and 24 hours after contrast administration may be indicated to identify postrenal obstruction or hydronephrosis.
Percutaneous antegrade urography. When performing percutaneous antegrade urography, a radiopaque contrast agent is administered through the existing nephrostomy drainage or, less commonly, after percutaneous puncture of the pelvis under X-ray control. In some cases, ureterostomy or puncture of the intestinal reservoir may be used.
Antegrade urography is used in the following circumstances:
- When retrograde urography cannot be performed (for example, due to obstruction by a tumor at the level of the bladder).
- When should large kidney stones be visualized for which percutaneous assistance is required?
- When the presence of transitional cell carcinoma of the upper urinary tract is suspected.
- When patients cannot bear general anesthesia or the required degree of sedation for retrograde urography.
Complications associated with puncture and installation of drainage in the genitourinary tract and include bleeding, sepsis, damage to adjacent organs, microhematuria, pain and urinary extravasation.
Retrograde urography. Retrograde urography uses cystoscopy and ureteral catheterization to inject radiopaque contrast directly into the ureters and renal collecting systems. Sedation or general anesthesia is required. The technique is used when CT or MRI are necessary (for example, to accurately localize and determine the nature of the obstruction), but their implementation is ineffective.
It can also be used to study in detail the anatomy of the collecting system, ureters (for example, in the diagnosis of ureterovaginal fistulas) and the bladder. However, overdistension and reverse flow of fluid can distort the contours of the cups and hide detailed features of their anatomy. The risk of infection is higher than with other types of urography. Acute edema ureteral mucosa and the formation of iatrogenic strictures are rare complications.
Cystourethrography. In cistrourethrography, a radiopaque contrast agent is injected directly into the urethra and bladder. This technique provides more detailed information than other imaging studies for diagnosis.
Victory cystourethrography is performed during urination and is used to diagnose posterior urethral valves. No special preparation of the patient is required. A relative contraindication is extended urethral strictures.
Angiography. Traditional angiography using vascular catheters has been widely replaced by non-invasive vascular imaging techniques (eg, magnetic resonance angiography, CT angiography, ultrasound, radionuclide scanning). Remaining indications include measurement of renin levels in the blood of the renal veins, and, among patients with renal artery stenosis, angioplasty and stenting. Arteriography is rarely used for the diagnosis and treatment of renal bleeding and before organ-sparing kidney surgery. Digital subtraction angiography is no longer used given the availability of rapid serial multidimensional or helical CT.
Ultrasonography
Doppler ultrasonography commonly used for imaging the renal arteries, kidneys, bladder, etc. The test is safe, but does not provide information about renal function, and renal imaging is difficult to obtain in obese patients. Also, there is no way to improve the discrimination between tissue types, and image quality depends on the examiner. Ultrasound examination can determine the volume of urine after urination (residual urine volume). Doppler ultrasound in patients with testicular pain helps distinguish torsion from other causes by assessing testicular blood flow.
CT scan
CT scans can provide a complete picture of the urinary tract and surrounding structures. In most cases, conventional or spiral tomographs are used with or without the introduction of intravenous radiocontrast agents. The use of contrast agents for any technique resembles the IVU procedure, but can provide Additional information. Native multislice CT is the method of choice for imaging urinary stones. It is also best to avoid the use of radiocontrast agents for CT scanning of kidney injuries and other pathology, which may include acute bleeding (it may appear bright white and may be confused with contrast agent) and urinary extravasation. CT angiography is a less invasive alternative to traditional angiography.
Magnetic resonance imaging
MRI is safer than CT for patients at risk of radiopaque nephropathy and does not expose patients to ionizing radiation. Applications include all of the following:
- Differential diagnosis of kidney cysts complicated by hemorrhage and infection.
- Determination of the degree of tumor invasion into the bladder wall.
- High-quality visualization of the pelvic and genital organs using a pelvic or endorectal coil.
Magnetic resonance angiography, used to improve visualization blood vessels, has almost completely replaced traditional angiography in the diagnosis of renal artery stenosis and thrombosis renal vein in patients with normal function kidneys However, nephrogenic systemic fibrosis remains dangerous side effect use of gadolinium-based contrast agents. MRI does not visualize intrarenal calcifications well because... the latter contain few free protons. MRI with intravenously injected lymphotropic superparamagnetic nanoparticles (for example, monocrystalline iron oxide) can detect lymphatic metastases in prostate cancer, but is not available everywhere.
Radionuclide scanning
Cortical radiopharmaceuticals that have affinity for proximal tubular epithelial cells (for example, technetium-99m-dimercaptosuccinic acid [99m Ts-DMSA) are used to visualize the renal parenchyma. Excreted markers that are rapidly filtered and excreted into urine (eg, iodine-125-iothalmate, technetium-99m-diethylenetriamine pentaacetic acid (DTPA), technetium-99m-mercaptoacetyl-triglycerol-3 (MATG)) are used to estimate GFR and integral renal function. blood flow.Radioisotope scanning can be used to assess renal function when the use of intravenous radiocontrast agents is undesirable. Radioisotope scanning also provides more information than IVU or cross-sectional scanning about the following:
- Emboli in the segmental branches of the renal arteries.
- Scarring of the renal parenchyma due to vesicoureteral reflux.
- Functional significance of renal artery stenosis.
- Kidney function in a living donor before transplantation.
Technetium-99m-pertechnetate can be used to visualize blood flow in the testicles and to differential diagnosis torsion from epididymitis in patients with acute pain in the testicle, although Doppler ultrasound is used more often because it is faster. Not required for radionuclide scanning special training, but patients should be asked about known allergies to the radiopharmaceutical.
Urological manipulations
Some manipulations are used only for diagnosis, and some for treatment.
Bladder catheterization
Bladder catheterization is used for the following purposes:
- Obtaining a urine sample for testing.
- Measurement of residual urine volume.
- Resolving urinary retention or incontinence.
- Delivery of radiopaque or medicines directly into the bladder.
- Bladder rinsing.
Catheterization can be performed through the urethra or suprapubic access.
Catheters. Catheters vary in gauge (thickness), tail configuration, number of strokes, balloon size, material type, and length.
Gauge is described in French (F) units, also known as Charrière (Ch) units. Each unit represents 0.33 mm, so the 14Ch catheter has a diameter of 4.6 mm. Sizes range from 14 to 24 Ch for adults and from 8 to 12 Ch for children. Smaller catheters are usually sufficient to allow urine flow in the absence of preexisting disease and are suitable for use in urethral strictures.
Most catheter tips have a straight configuration (eg, the whistle tip of a Robinson catheter) and are used for single-use catheterizations. Foley catheters have a straight tip and an inflatable balloon that is used to hold itself in the bladder. Other self-retaining catheters may have a flared mushroom cap tip (Pezzer catheter) or a four-winged mushroom cap tip (Malecote catheter); they are used for suprapubic catheterization or nephrostomy. Curved catheters, which may have self-retaining balloons, have a curved tip to facilitate passage through strictures and obstructive sites (eg, prostatic urethra).
All catheters used for long-term urine drainage have passages. Many catheters have ports for balloon inflation, irrigation, or both (eg, 3-way Foley catheter).
Balloons on self-retaining catheters come in a variety of volumes, from 2.5 to 5 ml in balloons intended for use in children and from 10 to 30 ml in balloons used in adults. Large balloons and catheters are commonly used to treat bleeding.
Stylets are flexible metal guides inserted into the lumen of the catheter to stiffen it and facilitate passage through strictures and obstructive areas.
The material of the catheter depends on the purpose of its use. Plastic, latex, or polyvinyl chloride catheters are intended for single use. Latex-silicone, hydrogel, or polymer (to reduce bacterial contamination) catheters are intended for continuous use.
Urethral catheterization. Urethral catheter can be administered by any doctor and sometimes by the patient himself. No patient preparation is required; therefore, unless the urethral route of catheterization is contraindicated, the bladder is catheterized through the urethra. Relative contraindications include the following:
- Urethral strictures.
- Current UTIs.
- Reconstructive urethral surgery or bladder surgery.
- Urethral injuries.
After thoroughly cleaning the external opening of the urethra with an antibacterial solution under conditions of strict sterility, the catheter is lubricated with sterile gel and carefully passed through the urethra into the bladder. To help reduce discomfort, lidocaine gel may be injected into the male urethra before the catheter is inserted.
Complications of bladder catheterization include all of the following:
- Trauma to the urethra or bladder with bleeding or microhematuria (common).
- Urinary tract infection
- Creation of false moves.
- Scarring and stricture formation.
- Bladder perforation. Suprapubic catheterization.
Suprapubic catheterization for percutaneous cystostomy is performed by a urologist or other an experienced doctor. No preliminary preparation of the patient is required. General indications include the need for long-term bladder drainage and the inability to pass a catheter through the urethra or contraindications to the use of a catheter if catheterization is necessary.
Contraindications include the following:
- Inability to determine the position of the bladder clinically or ultrasound.
- Empty bladder.
- Suspicion of adhesions.
After local anesthesia of the abdominal wall in the suprapubic region, a spinal needle is passed into the bladder; If possible, use ultrasound guidance. The catheter is then placed through a special trocar or along a string passed through a puncture needle. Presence in anamnesis surgical intervention in the lower parts of the abdominal cavity is a contraindication to blind insertion of the needle. Complications include urinary tract infection, intestinal damage, and bleeding.
Cystoscopy
Cystoscopy involves inserting a rigid or fiber optic instrument into the bladder.
Indications include the following:
- Help in diagnosing urological pathology.
- Treatment of urethral strictures.
- Access to the bladder for radiological visualization of the ureters or placement of JJ stents.
The main contraindication is active UTI.
Cystoscopy is usually performed on an outpatient basis using local anesthesia or, if necessary, sedation or general anesthesia. Complications include urinary tract infection, bleeding, and trauma to the urethra and bladder.
Biopsy
Carrying out a biopsy requires the presence of a qualified specialist (nephrologist, urologist or interventional radiologist).
Kidney biopsy. Indications for diagnostic biopsy include idiopathic nephritic or nephrotic syndrome or acute renal impairment. A biopsy is sometimes used to evaluate response to treatment. Relative contraindications include hemorrhagic diathesis and uncompensated arterial hypertension. Moderate preoperative sedation with benzodiazepines may be required. Complications are rare but may include renal bleeding, which requires blood transfusion, radiological or surgical intervention.
Bladder biopsy. Bladder biopsy is indicated to diagnose specific pathology and in some cases to assess response to treatment. Contraindications include hemorrhagic diathesis and acute tuberculous cystitis. Preoperative antibiotic therapy is only necessary if there is an active UTI. The biopsy instrument is inserted into the bladder through a cystoscope; rigid or flexible instruments can be used. The biopsy site is coagulated to prevent bleeding. A drainage catheter is left in place to facilitate healing and drainage of clots.
Biopsy prostate gland . A prostate biopsy is usually performed to diagnose prostate cancer. Contraindications include bleeding diathesis, acute prostatitis and UTI. Patient preparation includes stopping aspirin a week before the biopsy, taking a preoperative antibiotic (usually a fluoroquinolone), and a cleansing enema. In the lateral position, the position of the prostate is determined by palpation, or, more preferably, with an ultrasound probe. The tissues overlying the prostate (perineum or rectum) are anesthetized, then a spring-driven biopsy needle is inserted into the prostate tissue and usually 12 columns of tissue are obtained.
Complications include the following:
- Urosepsis.
- Bleeding.
- Urinary retention.
- Hematuria.
- Hemospermia (often up to 3-6 months after biopsy).
Bougienage of the urethra
Urethral dilation is performed to treat the following conditions:
- Urethral stricture.
- Urethral syndrome (with urge urinary incontinence).
- Meatostenosis.
Contraindications include untreated infection, bleeding diathesis, extended strictures, and severe urethral scarring. In case of stricture, a thin thread-like guide is passed, then bougies of successively increasing diameter are attached to distal end filamentous conductor and are carried out behind it until the urine stream becomes adequate. Usually the procedure is performed in several sessions.