The prevalence is estimated at 1.4 cases per 100,000 and accounts for 1% of all surgically removed melanocytic nevi. It is usually acquired. 1/3 of patients are children under the age of 10 years, in 36% it is found between the ages of 10 and 20 years, and only in 31% - over the age of 20 years. There is no familial predisposition.
The etiology and pathogenesis are unknown. Spitz nevus develops from neural crest cells. No pathogenetic associations have been reported. It is possible that this nevus and cutaneous malignant melanoma are stages of the same continuous pathological process.
| It is a single, moderately dense palpation, clearly circumscribed, hairless, asymptomatic, dome-shaped or flat papule (nodule) with a diameter of 0.2 to 2 cm (average 0.6 cm) with a smooth or warty surface. The coloring of the lesion is uniform. The color of the neoplasm depends on the degree of vascularization and the amount of melanin in its structure. Therefore, they distinguish:
Most often, the tumor is located on the head (face, ears, less often hairy part, periorbital region) and neck, less often on the lower extremities. Casuistic cases of localization on the mucous membrane of the mouth and genitals have been described. Cases of multiple or grouped nevi have been noted. |
Atypical nevus Spitz
Clinical variants of Spitz nevus
 |
 |
 |
| hyperpigmented | hyperpigmented flat | polypoid |
 |
 |
 |
| target-shaped | halonevus | mucous membranes |
 |
 |
 |
| disseminated | grouped | combined with macular nevus |
Course of nevus Spitz
The course of the disease is unpredictable. In most cases, the nevus occurs de novo (on unchanged skin). Usually, the history shows an unexpected onset and rapid growth (can reach 1 cm within 6 months), after which the process stabilizes and becomes static. It can develop into a common complex melanocytic nevus, in some cases undergoes fibrosis. Very rarely it can spontaneously regress. In 6% of cases, malignant melanoma of the skin can occur within the nevus.
The diagnosis is made on the basis of anamnesis, clinical picture, dermatoscopy and histological examination
Dermatoscopy
Hypopigmented form
Vascular manifestations predominate - pinpoint vessels, comma-shaped vessels and glomeruli, located on a uniform pink background. Pale brown globules or pale pigment spots may be observed
Pigment form
Brown formations with dark central part and a slightly lighter peripheral one, in which spherical globules are located, forming a characteristic chain at the border with healthy skin. The pattern of the central part is variable. Homogeneous pigmentation and globules are most often found. In some cases, Spitz nevus may not have characteristic features and looks like an unevenly pigmented gray-blue or gray-black spot. Reed's nevus is characterized by the presence of uniform radial radiance (pseudopodia), an intensely pigmented center and the frequent presence of a blue-white veil.
Histological examination
Histologically, nevus can be borderline, mixed (most often) and intradermal. Nevus cells are predominantly spindle-shaped, but may be epithelioid. Nevus cells are located mainly in limited nests extending from the hyperplastic epidermis into the reticular layer of the dermis in the shape of an inverted triangle. Edema and telangiectasias are very often observed in the stroma. Melanin in many cases is either practically absent or very little. Sometimes mitoses and inflammatory infiltrates occur. Epithelioid cells often contain many large, hyperchromatic nuclei.
An atypical Spitz nevus is characterized by pronounced cellular and increased mitotic activity. The greater the atypicality, the more difficult it is to differentiate between Spitz nevus and malignant melanoma skin.
Complete surgical excision of the lesion is recommended (with a margin of 5 mm to 1 cm in the case of atypical variants), followed by re-excision of positive border areas if present. Incomplete excision often leads to recurrence. Periodic monitoring is recommended at intervals of 6-12 months.
One of the types of moles is Spitz nevus - not malignancy, differing from the others in the evenness of the edges. Bleeds heavily at the slightest injury. They appear in the first 10 years of life, but may increase at an older age. This is a congenital tumor with an unknown exact nature of occurrence. Appears abruptly and asymptomatically. It is often located on the patient’s face, so it can cause external discomfort. A spindle cell nevus is removed using laser therapy, surgery, destruction by radio waves, liquid nitrogen or heat. You must first diagnose the tumor.
Spitz nevus is characterized by hypersensitivity and bleeding.
What does it represent?
Spitz nevus is called juvenile, juvenile spindle cell and epithelioid mole. This is a nodular neoplasm with a round shape, slightly protruding above the surface. Nevus of this type mainly manifests itself in children and adolescents, young people under 20 years of age. Juvenile nevus has clear edges that are clearly visible in contrast to the skin. Has pink or brown, different tones. Often such a spindle-shaped mole is small in size, the diameter does not exceed 2 cm. The color of the surface of the nevus is uniform, scaliness is possible. Selects any area on the human body, mainly on the head. Hair doesn't grow on her. Any changes in size, color and surface skin are a reason to consult a doctor for advice.
Etiology and epidemiology
Medicine does not name the exact reason for the appearance of Spitz’s mole. The basis for the manifestation of a nevus is the embryonic rudiment of neural crest cells. The child has a congenital formation. Possible growth of growth at any age, but after 40 years it is rare. One of the reasons for the appearance of a nodule is hereditary factor. The nevus was identified by pathologist Sophie Spitz, after whom the fusiform nevus was named in 1948.
Often appears in a single copy, only in 2% of cases several epitheloid compactions are observed. Hormonal imbalances, during the formation of the body, can become the nature of the occurrence of juvenile moles. The risk of degeneration into a malignant formation is very low, but you should undergo systematic diagnosis by a dermatologist, especially if there are patients with any type of oncology in the family. This is the view birthmarks prone to malignancy.
 Spitz nevus is characterized by a dense nodular structure and possible peeling.
Spitz nevus is characterized by a dense nodular structure and possible peeling.
Symptoms and course options
The appearance of Spitz nevus is asymptomatic. The patient does not feel pain, there is no swelling of the tissue, itching or burning. Similar to warts, but with a smooth surface. Clarity of boundaries is one of the distinctive symptoms of a neoplasm. According to the clinical picture of the disease, there are:
- nevus Pink colour, the consistency is soft, the formation is slightly pigmented;
- light knot of dense structure;
- a strongly pronounced dark-colored compaction with a dense structure, sometimes with a flaky surface;
- several nevi of bright or dark color.
A Spitz mole appears suddenly, without prior redness. A feature of this type of nevus is its ability to bleed heavily with minor damage and injury. Only a doctor can diagnose a spindle cell nevus using dermatoscopy, which is the main analysis. An inexperienced doctor, upon visual examination, may confuse a Spitz mole with melanoma.
 “Metamorphoses” of a nevus may indicate degeneration into malignant form.
“Metamorphoses” of a nevus may indicate degeneration into malignant form. Complications of spindle cell nevus
Epitheloid nevus rarely develops into melanoma, but the risk is not minimal due to the rapid trauma of the formation. A complication from such a mole can be its degeneration into a non-cellular formation, which, if ignored, leads to fibroma. In case of metastasis cancer cells located on lymph nodes. You should show a nevus to a doctor immediately when:
- the form of education has changed;
- pigmentation has appeared - darker or lighter zones in the overall color;
- happened sharp increase at the rate of;
- the boundaries have become uneven;
- discharge from the epidermis appeared;
- The skin around the nevus turned red.
Atypical behavior of a Spitz mole is a signal for immediate diagnosis. Changes in the appearance of the tumor may indicate a problem.
 Diagnosis for a threat from Spitz nevus includes testing and hardware examination.
Diagnosis for a threat from Spitz nevus includes testing and hardware examination. Event diagnostics
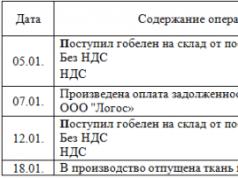
To determine the exact picture of the disease, you should seek help from a doctor. The initial examination can be carried out by a general practitioner who subsequently refers the patient to a dermatologist or oncologist. Diagnostics includes the use of several research methods to complete the clinical picture. A table with methods for studying the disease is provided.
Diagnostics are carried out for precise definition disease, so as not to mistake it for dermofibroma, granuloma, hemangioma, nodular melanoma or molluscum contagiosum. Only after appropriate analyzes can it be established accurate diagnosis and prescribe appropriate treatment. A Spitz mole is similar in manifestations to melanoma, so only a dermatologist or oncologist can give an accurate description.
 The most justified treatment for Spitz nevus is professional surgery.
The most justified treatment for Spitz nevus is professional surgery. At some times, people considered this a mark of belonging to a higher caste; among other peoples, moles and especially birthmarks were a mark of evil spirits, and an epidermal nevus on the face in medieval Europe was quite a death sentence. It was considered a “mask of the devil,” and its owner was subject to purification by fire and burning, regardless of social status or age. A little more than a hundred years passed, aristocrats and people close to aristocratic circles ordered artificial black moles - flies, which they literally pasted over their faces. True, even then there were gossips who claimed that man-made moles covered scars after one of the crowned persons suffered black smallpox. Nowadays, enlightened contemporaries also tend to see a certain danger in the presence of nevi. And this is completely justified, because such familiar and seemingly harmless moles may well become the first signs of the body’s tendency to cancer.
The emergence and development of such neoplasms today is one of the main issues that are being comprehensively addressed by physicians of different specializations. Due to the significant deterioration of the environmental situation in the world, there has been a surge in manifestations of skin destruction of various etiologies, with a tendency to malignant degeneration. What an epidermal nevus actually is and what are its features that make it possible to distinguish it from a number of similar pathologies.
Modern classical medicine uses a variety of sources and methods to determine the essence and nature of skin tumors. As is known, the founders of medical science dealt with problems of this order. But even with the use modern technologies It is difficult to talk about the scope of the reasons that potentiate the appearance of neoplasms at various levels of the skin, including how and why epidermal nevus is formed. The latter can be considered as a kind of negative genetic mutation, developmental defect skin varying levels of depth and localization, to one degree or another inherent in almost all people. Neoplasms of this nature are usually congenital in nature or manifest themselves in at different ages. The name determines the specifics when the development of a nevus occurs in the epidermis - the very top layer skin. During the rest period, when the mole is in a stable dormant state, it does not manifest itself in any way. A special feature is that epidermal nevi most rarely of all atypical neoplasms degenerate into a malignant type. Despite such an outwardly harmless nature, a certain species is still subject to transformation into cancerous tumor. This is a nevus sebaceous gland or a sebaceous sac, which, according to statistics, in the range from 5% to 8% degenerates into basalioma - a cancerous growth of the basal layers of the skin.
Causes of congenital nevi

What you need to know about this type of neoplasm is that it is the most common developmental disorder of the skin that occurs in the perinatal period. For certain reasons, a small area of skin becomes a site of accumulation of cells with a high content of melanin. Epidermal nevus is a pathologically developed tissue with an excess of pigment. The result of the process is a dark-colored spot on the skin.
The reasons for its appearance at birth may be various factors, among which the most often diagnosed when collecting anamnesis are:
- Large-scale impact of unfavorable environmental factors. In this case, most often a flat nevus occurs, which appears at a very early age.
- Negative impact is important intrauterine infections during fetal development, among which the most dangerous are viral diseases– herpes, smallpox, cytomegaloviruses, pathogens of toxoplasmosis and other dangerous infections.
- Particular attention should be paid to the presence ionizing radiation. Serious consequences for a child’s skin can be the uncontrolled use of various medications by a pregnant woman, hypervitaminosis of groups “A” and “B,” and work in the presence of mercury vapor and metal salts. Typically, in this case, hemangiomas appear - capillary nodes of various sizes.
- Manifestations of significant iodine or zinc deficiency, pregnancy due to diabetes mellitus or phenylketanuria also entails such consequences as subcutaneous formation - juvenile nevus in a child.
Causes of acquired moles
But this all applies to birthmarks that a person received at birth or upon reaching a certain age. As for the other type, which is classified as acquired epidermal nevus, the reasons for its appearance are somewhat different.

- First of all, experts consider the impact of age-related changes hormonal status. This surge of hormones in adolescents or their age-related attenuation in adulthood, pregnancy or menopause leads to the fact that juvenile, pink or brown vascular nevus most often appears. Most often it does not differ in pronounced texture and large sizes, multiple neoplasms occur.
- Significant injuries to the deep layers of the skin lead to the appearance of a junctional or, as it is called, “borderline” nevus in the form of a flat, smooth, pigmented neoplasm somewhat raised above the surface of the skin, on which there is no hair. They have a tendency to degenerate into a malignant tumor - melanoma.
- Severe organic lesions at the level of metabolic disorders, dysfunction internal organs and systems, the consequences of operations, injuries, severe infections also lead to the appearance cutaneous nevi. Especially often, vascular pigment spots remain “as a keepsake” after hepatitis, pancreatitis, or liver failure. Nevi of this type are often called liver stars; they are a fairly accurate confirmation of the presence of liver disease.
Sunny or fake tan – good activity, but not for those who already have a variety of moles, pigmented or depigmented spots. Exposure to the ultraviolet spectrum for a long time on open skin leads to burns, potentiating the degeneration of cells containing melanin into cancerous structures. Constant deep burns of the skin lead to the appearance of combined epidermal and dermal nevi, growing from the superficial layers into the deeper layers of the skin.
Diagnosis and elimination
If you are the owner of moles, for you mandatory procedure There should be regular examinations by a dermatologist and oncologist. It is especially important not to waste precious time if the element begins to change, pain, itching or burning appears, bleeding or lymph discharge, or redness around. Complex diagnostic measures allows us to establish the nature of changes in the neoplasm quite qualitatively.

- A visual examination for growth, changes in color, and appearance is most effective if the black nevus has begun to degenerate.
- When cracks, ulcers or fluid are visible on the surface, the doctor must order a smear for clinical examination. cytological examination. This method helps determine whether there are modified cells in tissues.
- Investigation using epiluminescent microscopy and more modern method– computer research after digital photography of the object.
Biopsy is not recommended due to high tissue trauma; histology is taken exclusively during the process surgical removal element. At the end of the research, the doctor makes a decision to eliminate the tumor. The most popular and practically painless methods are applications of liquid nitrogen. Electrocoagulation and laser removal are no less often used, and radiosurgery is a popular method. In situations where there is no special equipment, traditional surgery is used against the background of local local anesthesia.
Pigment formations on the skin are a very common phenomenon. Everyone has moles on their body, but in some cases other elements also appear. Some may experience a benign condition called Spitz nevus (Spitz) or juvenile melanoma. What it is, how it manifests itself and how it is eliminated – these questions remain to be answered.
Causes and mechanisms
Why juvenile nevus occurs is not fully established. The most likely mechanism for its development is considered to be hormonal changes in the body. Scientists made this conclusion based on data on the prevalence of the disease. It is known that such formation most often occurs during certain periods of life:
- Childhood.
- Puberty.
- Pregnancy.
Thus, people are most susceptible to juvenile melanoma young. After 40 years, such nevi occur only in isolated cases. They may also be congenital, but the fact is not denied genetic predisposition to the development of such formations.
Classification
There are several terms suitable for the same process. The pigmented lesion may also be called juvenile benign melanoma, juvenile or atypical spindle cell nevus. Usually this is a single tumor, but there are also multiple forms. In their structure, according to the classification, there are several types:
- The first is widespread (grouped) nevi on various parts of the body.
- The second is that the lesions are located on unchanged skin.
- Third, nevi occupy an area with reduced pigmentation.
- Fourth, the formations are grouped against a hyperpigmented background.
These criteria are necessary for making a diagnosis, because the patient’s specific symptoms fit into the framework of one of the presented options.
Spitz nevus has several names reflecting its nature and origin. And the classification presents four types of its course.
Morphology

Great importance is given to the histological structure of the nevus. As stated earlier, this is a benign formation. It is mainly represented by spindle-shaped or epithelioid cells. Depending on the location, the following nevi are distinguished:
- Intradermal.
- Borderline.
- Mixed.
The latter variety is more common. In the structure of the formation, the cells are arranged in groups, the tissues are swollen, and the capillaries are dilated. Inflammatory infiltrates may also occur. The basal layer of the epithelium may contain specific eosinophilic particles, and in the stroma of the nevus, a so-called desmoplastic reaction (proliferation of connective tissue) is sometimes observed.
Symptoms
The tumor-like formation is mainly localized on the scalp and face; other parts of the body (limbs, torso) are less commonly involved. A nevus looks like a small node measuring from 2 to 20 mm, but most often with a diameter not exceeding 1 cm. The color varies from pink to dark brown, the color is homogeneous or uneven. The nature of the surface can be smooth or rough (with warty or papillomatous growths). The pigment formation is devoid of hair.
The course of Spitz nevus has several clinical variants, which was described in the classification. The first is characterized by the appearance of an elastic, slightly pigmented tumor (pink or light brown), which loses color when pressed. The second type is represented by a more dense formation with the development of telangiectasia. A smooth or lumpy tumor with a flaky surface and intense coloring is a sign of the third clinical option. If many red-brown nodes appear on the background age spots, then they talk about the fourth type of nevus.
The clinical symptoms of nevus are represented only by external changes on the skin. The patient does not experience any discomfort other than cosmetic.
Course and prognosis

Education arises quite suddenly and has rapid growth. But soon the nevus becomes flat and long time remains unchanged. If injured, it may bleed. In the future, there are several options for the development of pathology:
- Spontaneous involution (reverse development).
- Transformation into melanocytic nevus.
- Malignancy (transformation into melanoma).
The greatest danger is the malignancy of a juvenile nevus during puberty, although such cases are quite rare. External signs dangerous formations may be big size and the presence of ulcerations. Histologically, malignant Spitz nevus is characterized by a dense arrangement of cells with atypia and a significant number of mitoses. Sometimes metastasis occurs to regional lymph nodes.
Additional diagnostics
Histological examination is of decisive importance for diagnosis. With its help, it is possible to differentiate nevus from melanoma, since there is a certain similarity with malignant tumor on early stages development. Typical differences in the condition under consideration will be:
- Presence of spindle cells.
- Low pigment content.
- Surface location.
- Less pronounced atypia.
In addition to melanoma, juvenile nevus is also differentiated from other changes on the skin, among which it is necessary to note juvenile xanthogranuloma, mastocytoma, and hemangioma.
Treatment
The only treatment method is surgery. According to the traditional instrumental technique, the nevus is completely excised within the boundaries healthy skin(at once). Laser resection can also be performed, the advantage of which is coagulation of adjacent tissues and the absence of bleeding. After the operation, the doctor monitors the patient’s condition for 12 months.
Since there is a risk of malignant transformation of the nevus, it must be removed surgically.
The nevus may disappear on its own, but there is a risk of its malignant transformation. Therefore, if suspicious changes appear on the skin, you should consult a doctor in time and carry out appropriate correction.
In modern dermatology, a large number of different benign formations skin. They are often called moles or nevi and most of them do not pose a threat to human life and health. However, in some cases they can degenerate into such dangerous disease like melanoma. Nevus Spitz- this is one of such formations, which, despite its benign nature, still has a tendency to malignant transformation and therefore requires increased attention.
Clinical picture
Nevus Spitz has a dome-shaped shape and is small in size (up to 1 cm). His outer surface, as a rule, smooth, without hair, with clear boundaries and uniform coloring. In the vast majority of cases, these are single formations that are located on the skin of the face or neck and very rarely on the torso or limbs.
In dermatology, it is customary to distinguish 4 variants of the manifestation of formation:
- The nevus has an elastic consistency and a low pigment content. Its color is pink or light brown.
- Education with low level pigmentation, but with a dense consistency.
- A skin formation with a large amount of pigment with a smooth or flaky dark-colored surface.
- Manifestation of multiple nodules.
The first two options are the most common.
Period of occurrence
More often nevus Spitz manifests itself in childhood or adolescence, as well as from birth (10%). Much less often after 20 years and, in isolated cases, after 40 years. In this case, the tumor grows quite quickly and within a few months can reach its natural size. Often rapid growth forces you to seek advice from a dermatologist. It is because of this peculiarity of its manifestation that Spitz nevus is also called “juvenile melanoma,” as well as spindle cell or juvenile nevus. This pathology occurs with equal frequency in both men and women.
In what cases should you consult a doctor?
In its structure, the formation is very similar to melanoma, but is not it. At the same time, the presence of such a mole indicates increased risk skin cancer diseases. Also, according to recent observations, the likelihood of malignancy increases significantly with the onset of puberty.
You should definitely consult a doctor if the following changes become noticeable: appearance nevus:
- After being in a stable state for a long time, the mole suddenly increases in size.
- The nevus begins to change its shape, irregular contours and asymmetry appear.
- Changes in color are noticeable: it becomes uneven or the entire color changes.
- The formation bleeds or wet masses of a different nature are released from it.
- , pain or other unpleasant sensations appear.
Such manifestations may indicate the beginning of the process of malignancy (malignancy). Even if there is one of listed signs It is imperative to visit a dermatologist, as this may indicate a precancerous condition or initial stage melanoma.
Features of diagnosis and treatment of Spitz nevus
Primary diagnosis and examination is carried out by a dermatologist using. This device increases the visibility of the nevus tens of times, which allows you to draw conclusions about the clinical condition of the skin formation.
Sometimes nevus Spitz it is very difficult to distinguish from manifestations of melanoma, since their structure can be very similar. In this case, a biopsy procedure is prescribed for histological studies. Taking these factors into account, you should consult an experienced dermatologist for a correct diagnosis.
Treatment of such a nevus is carried out by simultaneous excision of the tumor with the capture of healthy adjacent tissue. It is advisable to perform the operation when, as a result of examination or histological examination, malignancy of the formation is confirmed. Usage laser scalpel leaves minimal post-operative marks on the skin. Therefore, in this way it can be carried out in for cosmetic purposes. This, in turn, can prevent the development of complications such as fibrosis.
Excised tissues are necessarily sent for histological examination. After the operation, periodic monitoring by a doctor is required over the next 12 months.