Tick-borne encephalitis- it's quite common infection. It usually has an acute course. Intoxication leads to damage nervous system which can lead to paralysis.
It is a mistake to assume that, based on the name, tick-borne encephalitis can affect a person only after a tick bite. This is the prevailing version. However, the virus of this disease can also be located in the organisms of rodents and insectivores.
The most unpleasant thing is that domestic goats, cows or sheep can have the virus. They may have the virus, but they may not have symptoms of the disease. That is, these pets can be simple carriers. Human infection can occur through raw milk.
Tick-borne encephalitis is a viral pathology characterized by a transmissible mechanism of infection (with insect bites), as well as accompanied by febrile symptoms and damage to the tissues of the central nervous system.
Encephalitis is a disease of the brain. The suffix -it directly indicates that the disease is inflammatory in nature. Often, in the general case, the cause of encephalitis (inflammation of the brain) is difficult to establish.
However, in the case of a tick bite, the cause is obvious. It remains only to make sure that the bite was (here it is a tick that was removed from the skin) and establish the symptoms.
Here, in the case of receiving the tick-borne encephalitis virus through the infected milk of a pet, it will be more difficult to verify the cause.
The disease has a pronounced natural foci. The conditions for the existence of ticks are:
- favorable climate,
- essential vegetation,
- landscape.
Also, tick-borne encephalitis is characterized by seasonality.
A sick person is not a source of infection for others.
According to ICD10, tick-borne encephalitis is classified as A84.
Tick-borne encephalitis - causative agent
Tick-borne encephalitis viruses belong to the group of RNA-containing flaviviruses.
According to the genotype, tick-borne encephalitis viruses are divided into five types:
- Far Eastern
- western,
- Greek-Turkish,
- East Siberian
- Ural-Siberian.
For reference. The most common type of virus is the Ural-Siberian genotype of the pathogen.
The virus is quickly destroyed by boiling (within two to three minutes), during pasteurization, and also when treated with disinfectant solutions.
When dried and under freezing conditions, viral particles are able to retain their activity for a long time.
Attention. It should be noted that pathogens can persist for a long time in food products(especially in milk, butter, etc.).
Infection with tick-borne encephalitis
 Tick-borne encephalitis is carried by ixodid ticks. Infection occurs mainly in a transmissible way: when biting a tick, as well as when combing the bite site, improper removal of the tick, etc.
Tick-borne encephalitis is carried by ixodid ticks. Infection occurs mainly in a transmissible way: when biting a tick, as well as when combing the bite site, improper removal of the tick, etc.
Given that pathogens are resistant to of hydrochloric acid, in isolated cases, alimentary (food) infection with tick-borne encephalitis may occur when consuming products containing viruses.
It should be noted that not all tick bites are accompanied by the development of an infectious process. According to statistics, the development of the disease after tick bites is recorded in approximately two to four percent of cases.
For reference. Infection of the ticks themselves with the encephalitis virus is observed when biting animals in which the viremic phase of the virus circulation is observed (the virus is in the blood).
In this regard, infection with viral particles is observed in approximately five percent of ticks. However, after a tick is infected with a virus, this type of virus circulates in its body for life and, in the future, is transmitted to the next generation of ticks. It is due to this that ixodid ticks are able to act as a natural reservoir of pathogens of tick-borne encephalitis.
The period of incubation of viruses in the human body is on average from ten to fourteen days (sometimes from one to thirty days).
For reference. A person cannot act as a source of infection (the virus is not transmitted from person to person).
risk factors for infection
The maximum activity of ticks is observed from mid-spring to the end of summer. In this regard, the maximum risk of infection is observed during these months.
For reference. Most often, tick-borne encephalitis affects people from twenty to sixty years old. The level of natural susceptibility to the disease is high and has no gender differences.
City dwellers, often resting in nature, get sick more often than rural dwellers.
Definition of disease. Causes of the disease
Tick-borne encephalitis- This is an acute and chronic natural focal infectious disease caused by the tick-borne encephalitis virus, which leads to an acute fever, damage to various parts of the nervous system in the form of flaccid paresis and paralysis. As a rule, it is transmissible, that is, it is transmitted by blood-sucking insects.
Etiology
The tick-borne encephalitis virus was first isolated in 1937 by L. Zilber.
Group - arboviruses
Family - Togaviruses
Genus - Flavivirus (group B)
The species is a tick-borne encephalitis virus, which is divided into six genotypes (the most significant are the Far Eastern, Ural-Siberian and Western).
Tick-borne encephalitis is an RNA virus that is localized in the nervous tissue. It has a spherical shape 40-50 nm in diameter. It contains a nucleocapsid surrounded by an outer lipoprotein membrane with glycoprotein spines embedded in it (capable of sticking together red blood cells).

At low temperatures well preserved, resistant to drying (at low temperatures), in milk (including in the refrigerator) it lasts up to two weeks, in butter and sour cream - up to two months, at room temperature it is inactivated for 10 days, it dies after boiling two minutes, at a temperature of 60°C loses its properties after 20 minutes. Household disinfectants and ultraviolet light also lead to its rapid death. Antibiotics have no effect.
Epidemiology
Natural focal disease. The distribution area covers Siberia, Far East, Ural, European part Russia, as well as Europe.

The main reservoirs of infection are ticks Ixodes persulcatus (taiga ticks) and Ixodes ricinus (dog ticks), sometimes other representatives of ticks.
The secondary reservoir of the virus in nature is warm-blooded mammals (hares, squirrels, chipmunks, mice, foxes, wolves, goats and others) and birds (thrush, bullfinch, black grouse and others).
Female ticks are able to transmit the acquired pathogens of the virus to their offspring, which ensures a constant level of infectivity of these arthropods and the circulation of the pathogen.
One tick can contain up to 10 10 viral particles, and the ingestion of only 1: 1,000,000 shares in the human body may well lead to the development of the disease. The fatter the tick, the greater the concentration of the virus in it.
The main circulation of the virus: ticks - hosts (animals and birds) - ticks. When a person is infected, the cycle is interrupted, because after the virus enters the human body, it stops spreading (biological impasse).

The disease is characterized by autumn-summer-spring seasonality in the middle lane, due to peaks in tick activity, depending on natural and climatic conditions. Sometimes there are cases of activation of ticks and diseases in winter during thaws.
Tick habitats are deciduous and mixed deciduous-coniferous forests with a pronounced shrub and grass cover, as well as paths of animals that feed ticks.
Infection occurs when ticks attack people in the suburban area, fields, forests, summer cottages during the holidays, collecting the gifts of the forest. Often, cases of infection are also recorded in the cities themselves: in park areas, lawns. Mechanical transfer of ticks on clothes, things, products and their crawling to people who have never visited nature is possible.
Transmission mechanisms:
If you experience similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Symptoms of tick-borne encephalitis
The clinical picture of the disease may vary depending on the serotype of the virus: as a rule, the Far East and Siberian variants are more severe; the course of the disease in the European part of the Russian Federation and Europe is marked by a milder and more favorable course.
The incubation period is from 1 to 35 days (on average 2-3 weeks), there is no clear relationship between the severity of the disease and the incubation period.
Schematically the course of the disease in acute period can be divided into six stages:
- infection;
- incubation period;
- prodromal period (the appearance of precursors of the disease);
- feverish period;
- early convalescence (recovery);
- recovery period.
Most often, the disease occurs in a latent or mild form, manifested by a slight increase in body temperature, a mild headache without a clear localization, general malaise and sleep disturbances (up to 90% of all cases).
Sometimes, in cases of a more pronounced course, the disease begins with prodromal phenomena in the form of chilling, weakness, heaviness in the head, diffuse headaches of low intensity for 1-2 days. Then the disease manifests itself with a sharp increase in body temperature up to 38-39 ° C, a sharp chill, sweating, severe headaches of a bursting nature, often accompanied by nausea, vomiting and impaired coordination. The patient is inhibited, apathetic, sluggishly reacts to external stimuli. His face, neck and chest are hyperemic. Perhaps the appearance of pain in various parts of the body, muscles and joints, sometimes there are fascicular twitches. In the future, weakness, increased sweating, fluctuations (lability) blood pressure, paresthesia (numbness) of certain parts of the body without impaired motor functions. There are symptoms of damage to the meninges, such as stiff neck, symptoms of Kernig and Brudzinski.
With alimentary infection (through food), abdominal pain, diarrhea, the appearance of a dense white coating on the tongue, as well as a two-wave febrile reaction are possible:
- short first wave of fever within 2-3 days;
- the second rise in temperature after a week-long "break" (usually more severe and prolonged).
With a favorable course, these signs gradually regress, sometimes leaving behind residual (residual) phenomena of varying severity and duration.
In some cases, the symptomatology increases and manifests itself in the form of severe toxicosis, the appearance of focal symptoms, paresis, impaired consciousness, breathing and activity. of cardio-vascular system. The prognosis in such cases is serious.
In the chronic course of the disease a wide polymorphism of clinical manifestations is possible, but the following signs are more often observed:
The pathogenesis of tick-borne encephalitis
The entrance gate is the skin damaged by the tick, the mucous membranes of the intestines, stomach, rarely the conjunctiva of the eye (when the tick is smeared and the hands are not washed).
Viremia - the entry of the virus into the blood and its spread in the body - goes through two stages.
By hematogenous route, the virus enters the brain, where it actively multiplies, along the way, moving more slowly along the lymphatic pathways, sensitizes (increases sensitivity) segmental tissue areas - often more significant neurological changes are detected in these places.
After the multiplication phase in the nervous tissue, the virus enters the blood again and causes re-sensitization of already previously sensitized tissues. This leads to specific allergic reaction, alterations (functional damage) nerve cells and impaired microcirculation. In various parts of the nervous system, foci of micronecrosis are formed, supported by a generalized inflammatory process in the nervous tissue (with predominant involvement of the central sections), which determines the severity of the symptoms of the disease.

Due to the cytopathic action of the tick-borne encephalitis virus (degenerative change), there is a depression in the production and a decrease in the content of circulating T-lymphocytes, as well as a delayed reaction of the proliferation of B-lymphocytes (sometimes only by three months), i.e., an immunodeficiency state develops that supports the development of pathological changes in the brain brain. The developing immune response deactivates viral particles first in the intercellular space, then destroys infected cells when the complement system is attached.
In some cases, the virus triggers mechanisms to evade the immune response (features of individual strains of the virus, antigenic drift, individual characteristics human immunological reactivity, etc.), which causes the possibility of its long-term presence in the body and the formation of chronic forms.
After an infection with recovery, a stable (possibly lifelong) immunity remains.
Classification and stages of development of tick-borne encephalitis
According to the clinical form:
- Acute tick-borne encephalitis:
- Inapparent (hidden) form - detection of specific markers of infection in the blood in the absence or minimal severity of clinical manifestations.
- Feverish form - a sudden increase in body temperature up to 38-39С, nausea, sometimes vomiting, increased tone of the occipital muscles without changes in the composition of the cerebrospinal fluid (meningismus), general weakness, sweating lasting about a week. As a rule, it ends favorably, after it is possible medium duration asthenovegetative syndrome.
- Meningeal form (the most common manifest form) - the occurrence of all manifestations of the febrile form with the addition of pathological symptoms of irritation of the meninges, severe toxicosis. Sometimes, with the addition of transient scattered neurological symptoms, there is a change in tendon reflexes, anisoreflexia (dissimilar reflexes), facial asymmetry, and more. CSF changes are characterized by an increase intracranial pressure up to 300 mm w.c. Art., lymphocytic pleocytosis is detected up to 300-900 cells in 1 μl, the protein level rises to 0.6 g/l, the sugar content does not change. In general, the duration of the disease is about 20 days, more often it proceeds favorably, residual effects are possible in the form intracranial hypertension, headaches, subfebrile condition up to 2-3 months.
- Meningoencephalitic (focal and diffuse) form is a severe, life-threatening form of the disease. With a diffuse lesion, toxic and cerebral symptoms, the development of seizures, and impaired consciousness come to the fore. of varying severity sometimes to coma. With a focal lesion against the background of cerebral and toxic symptoms, motor disorders develop - central paresis(usually completely reversible).
- Polioencephalitic form - violations of swallowing, drinking, speech, various visual impairments, sometimes twitching of the tongue, when trying to drink water pours out through the nose, paresis of the soft palate is possible. Characteristic manifestations are central respiratory disorders, vascular collapse and cardiac paralysis, which leads to lethal outcome. With a favorable course, a long (sometimes more than a year) asthenic syndrome is characteristic.
- The polioencephalomyelic form is an extremely severe course, characterized by damage to the cranial nerves, paralysis of the heart and breathing with a mortality rate of up to 30%. In other cases, there is a high probability of paralysis and the transition of the disease to a chronic form.
- Poliomyelitis form - flaccid paralysis of the muscles of the neck, shoulder girdle and upper limbs, periodic disturbances in the sensitivity of these areas, atony. Very indicative of the so-called. drooping head syndrome, when the patient cannot hold his head in vertical position. Sometimes breathing is affected due to damage to the diaphragm, which is quite dangerous. The course of this form is long, the restoration of the function of the affected departments does not always occur in full.
- Two-wave course with an indication of the form of the second wave - the first wave of fever within a week with a complex of cerebral and intoxication disorders, then a period of imaginary well-being lasting 1-2 weeks, and the onset of the second wave of fever, accompanied by the development of meningeal and focal symptoms, usually without severe consequences.
- Chronic tick-borne encephalitis:
- Hyperkinetic form - Kozhevnikov's epilepsy, myoclonus epilepsy, hyperkinetic syndrome.
- Amyotrophic form - poliomyelitis and encephalopoliomyelitis syndrome, as well as syndrome of disseminated encephalomyelitis and amyotrophic lateral sclerosis.
- Rare syndromes.
In the course of the disease is:
- acute - 1-2 months;
- acute protracted (progredient) - up to 6 months;
- chronic - more than 6 months,
Chronic tick-borne encephalitis is caused by a long stay in the body of the tick-borne encephalitis virus. It usually develops in childhood and young age. There are four forms:
- initial - continuation of the acute process;
- early - during the first year;
- late - after a year from an acute form;
- spontaneous - without an acute period.
The severity of tick-borne encephalitis:
Complications of tick-borne encephalitis
Tick-borne encephalitis itself is serious illness which sometimes leads to death. However, against the background of its course, additional complications are possible, significantly aggravating the prognosis:
Diagnosis of tick-borne encephalitis
Laboratory diagnostics:


Differential diagnosis:
Treatment of tick-borne encephalitis
With the development of the disease, there is no specific highly effective etiotropic treatment.
In the acute period, strict bed rest, detoxification therapy, rational nutrition, the use of vitamins, means of improving cerebral circulation, hormone therapy. If necessary, the patient can be transferred to the ward intensive care prescribe the use of antispasmodic and relaxing drugs.
Sometimes in practice, immunotherapy agents, specific immunoglobulins, gamma globulins are used - their use to some extent can reduce the severity of the manifestations of tick-borne encephalitis and the severity of long-term consequences, but these drugs cannot radically affect the outcome of the disease.
In the chronic phase of the disease, it is possible to use vitamin and immunostimulating therapy, the use of antihypoxants and adaptagens.
For those who have been ill, regardless of the severity of the disease, dispensary observation is established for up to three years with periodic examination by a neurologist and examinations (according to indications).
Forecast. Prevention
With inapparent, mild forms of the disease, the prognosis is usually favorable. With the development of more serious forms of the disease, the formation of sufficiently long, sometimes lifelong residual effects accompanied by astheno-neurotic manifestations, headaches of varying intensity, decreased mental and physical performance. In severe forms, the prognosis is unfavorable.
Vaccination is the most effective preventive measure to prevent the development of the disease. It is carried out using any registered tick-borne encephalitis vaccine. As a rule, it is performed first in the fall, then in the spring, then the next spring a year later, after which a subsequent revaccination is shown every three years (it is possible to determine the level protective antibodies and graph correction). Such a scheme provides almost guaranteed protection against the development of the disease during infection. There are emergency vaccination schemes, but their effectiveness is lower than the main ones.
When an infected tick bites an unvaccinated person in Russia, they resort to the introduction of immunoglobulin, but its effectiveness and safety are in doubt.
Measures of non-specific prevention are similar to the prevention of tick-borne borreliosis:
- when visiting the forest park zone, it is worth wearing protective tight clothing, as well as using repellents that repel ticks;
- periodically examine the skin and clothing (every two hours);
- carry out centralized treatment of forest and park lands with means of combating ticks.
If a stuck tick is found, you should immediately contact the trauma department to remove the tick and send it for examination. Also, in parallel, it is necessary to contact an infectious disease specialist for observation, examination and recommendations for preventive therapy.
Tick-borne encephalitis is a severe infectious disease that is transmitted to humans from encephalitis ticks. The virus sneaks into the brain and spinal cord of an adult or a child, causes severe intoxication and affects the central nervous system. Severe encephalitic forms without timely treatment can lead to paralysis, mental disorders and even death. How to recognize the symptoms dangerous pathology what to do if you suspect a tick-borne infection and what is the importance of vaccination in the prevention and treatment of a deadly disease?
General description of the disease
Tick-borne encephalitis is classified as a natural focal disease that occurs in certain areas. The carriers of the pathogen are wild animals, in this case the encephalitic tick. The main foci of tick-borne pathology are Siberia and the Far East, the Urals, the Kaliningrad region, Mongolia, China, some areas of the Scandinavian Peninsula and Eastern Europe. Every year about 5-6 thousand cases of encephalitic tick infection are registered in our country.
The severity of the course and the form depend on the immunity of the bitten person, the amount of the virus in the body, the number of bites, and also on the geographic location. Specialists divide the encephalitic tick virus into 3 subspecies: Far Eastern, Siberian and Western. The most severe forms of the disease - after the attack of ticks in the Far East, 20-40% of death. If an encephalitic tick attack occurred in the European part of Russia, the chances of avoiding complications are much higher - the mortality rate here is only 1-3%.
Forms of the disease
Symptoms after an encephalitic tick attack are very diverse, but in each patient the period of the disease traditionally proceeds with several pronounced signs. In accordance with this, 5 main forms of tick-borne encephalitis are distinguished.
- Feverish, or erased (the most successful prognosis with treatment).
- Meningeal (diagnosed most often).
- Meningoencephalitic (occurs in 15% of the country as a whole, in the Far East 2 times more often).
- Poliomyelitis (diagnosed in a third of those affected by encephalitis ticks).
- Polyradiculoneuritis.
A special form of tick-borne infection - with a two-wave course. The first period of the disease is characterized by febrile symptoms and lasts 3-7 days. Then the virus penetrates the meninges, neurological signs appear. The second period lasts about two weeks and is much more severe than the febrile phase.
Causes and ways of transmission of the virus

The causative agent of lethal encephalitis is an arbovirus from the genus Flaviviruses. It is very small (2 times smaller than the influenza virus!), so it easily and rapidly passes through human immune defenses. Arbovirus is unstable to UV radiation, disinfection and heat: when boiled, it dies after a few minutes. But at low temperatures, it maintains vital activity for a very long time.

The virus usually lives in the body of ixodid encephalitic ticks and attacks not only humans, but also livestock: cows, goats, etc. Therefore, there are 2 main ways to get encephalitis: through an insect bite and alimentary (fecal-oral method). In this regard, we can name 4 main causes of encephalitic tick infection:
- Immediately after the bite of an infected insect;
- If tick feces get on the skin and penetrate into the blood through scratching;
- If, when trying to remove a stuck encephalitic tick, it bursts, and the virus gets inside;
- After drinking unpasteurized milk infected with an animal tick.
Symptoms

While the latent period of infection lasts, the virus multiplies at the site of the bite or in the walls of the intestine, then penetrates into the bloodstream and scatters throughout the body. Regardless of the form of the disease, the initial symptoms of tick-borne encephalitis in adults are the same:
- A rapid rise in temperature to 39-40º and chills;
- Head and lumbar pain;
- Muscle aches;
- Lethargy with lethargy;
- Cutting in the eyes and photophobia;
- Nausea, vomiting and convulsions (in isolated cases);
- Redness of the skin on the face and down to the collarbones;
- Rapid breathing and slow pulse;
- Plaque on the tongue.
If the virus has time to penetrate into meninges, there are separate signs of damage to the nervous system: the skin becomes numb, muscles weaken, goosebumps run through the body, sometimes convulsions.
Children experience similar symptoms after being attacked by a tick infected with encephalitis. The main difference is that the disease develops more rapidly and is more severe. Children especially often have convulsive seizures against the background of high temperature.
Feverish form
The febrile form of the infection develops if the virus circulates in the blood and does not penetrate the lining of the brain.
At first, the disease looks like a classic: fever begins (high temperature alternates with chills), constant weakness, the bitten person is tormented by pain in the head, nausea, and sometimes vomiting. Mild neurological symptoms may be observed: mild muscle pain, backache. Sometimes - goosebumps in separate attacks.
After recovery, within a month, individual signs may appear: weakness, poor appetite, sweating, palpitations.
meningeal form
This is the most common form of the disease after the bite of an encephalitic tick. Arbovirus in this form affects the membranes of the brain and spinal cord. The disease begins with classic signs: high temperature, then intolerable headache, which instantly increases with the slightest movement, dizziness, nausea and vomiting, pain in the eyes from bright light, lethargy, weakness and lethargy.
After infection with an encephalitis tick, rigidity occurs (the muscles of the neck are so tense that the head constantly tips back), tension in the muscles of the lower leg and the inability to straighten the leg at the knee, heightened skin sensitivity (even clothes bring pain).

This period lasts 7-14 days, after recovery, lethargy, photophobia, and depressive mood may persist for about 2 months.
Meningoencephalitic form
With this form of infection, the bites of encephalitis ticks and the penetration of the virus cause damage directly to the brain cells. The symptoms of pathology depend on which part of the brain is affected by the arbovirus and what is the size of this lesion.
If the meningoencephalitic form of encephalitis develops, neurological symptoms will come first: disturbances in movements and facial expressions, loss of orientation in time and space, clouding of consciousness, sleep problems, delirium and hallucinations, muscle twitching, shaking arms and legs, damage to the facial muscles (strabismus, double vision, problems with swallowing, slurred speech, etc.).
Specialists divide meningoencephalitis into 2 forms: diffuse and focal. Diffuse infection causes disorders of consciousness, epileptic seizures, breathing problems, central paresis of facial expressions and language, that is, a decrease in muscle strength. Focal tick-borne encephalitis is manifested by weakness in the muscles after convulsions, monoparesis, seizures.
Polio form
Poliomyelitis tick-borne encephalitis is a disease of cells exclusively in the spinal cord. In the prodromal period of such a pathology, for a couple of days, the patient feels weak, gets tired very quickly. Then difficulties with movement begin: first they suffer facial muscles, then arms and legs, after which certain areas of the skin begin to go numb and lose sensitivity.
A person infected with an encephalitic tick cannot hold his head in the usual position, make normal movements with his hands, suffer from severe pain in the back of the neck, shoulder girdle and arms. Muscles can significantly decrease in volume. All signs of other encephalitic forms may also appear.

Polyradiculoneuritic form
With this type of tick-borne infection, peripheral nerves and roots suffer. The main manifestations are pain throughout the body, tingling and crawling on the skin, Lasegue symptoms (pain along the way sciatic nerve when lifting a straight leg) and Wasserman (pain in the front of the thigh when lifting a leg).
The danger of the polyradiculoneuritis form is the development of Landry's ascending paralysis. In this case, flaccid paralysis starts from the legs, rises up the torso, covers the arms, then the facial muscles, pharynx, tongue, and can lead to respiratory failure. Paralysis can also start from the muscles of the shoulder and move upward, involving the muscles of the neck.
Two-waveform
Some experts classify such tick-borne encephalitis as febrile, but most scientists distinguish it as a separate type.
After the bite and the incubation period, the temperature jumps sharply, the patient feels dizzy, nausea and vomiting begin, pain in the arms and legs, sleep and appetite disturbances. Then, for 3-7 days, a feverish period lasts, which is replaced by a calm for one to two weeks.
The second wave of encephalitis begins just as abruptly, to the listed symptoms are added signs of meningeal and focal meningoencephalitic forms. The prognosis for recovery with this type of encephalitis is favorable, as with a normal febrile infection.
Diagnostics

When making a diagnosis of tick-borne encephalitis, it is necessary to take into account a combination of three factors: clinical manifestations(symptoms), epidemiological data (time of the year, whether the vaccine was given, whether there was a tick bite) and laboratory tests (analysis of the tick itself - optional, analysis cerebrospinal fluid and etc.).
The first thing to do if a tick attacked is to inspect sore spot. The bite of an infected insect is just a red, inflamed wound, and the encephalitic tick itself looks like a normal one. Therefore, in any case, emergency prevention of tick-borne encephalitis is needed - to introduce immunoglobulin against the virus, and then do an analysis. The main diagnostic methods that must be done after a tick bite are:
- Analysis of patient complaints and medical history;
- General examination (analysis of all symptoms in order to identify typical manifestations of tick-borne encephalitis);
- Virological analysis of blood and cerebrospinal fluid;
- Analysis of arbovirus and determination of its particles in physiological fluids;
- Immunoenzymatic analysis (level of antibodies in the blood);
- General and biochemical blood tests to determine the severity and characteristics of the CNS lesion.
Treatment
Today, tick-borne encephalitis is treated exclusively in a hospital, the main medicine against the disease is immunoglobulin ( special solution from serum or plasma donated blood with antibodies to the virus). Immunoglobulin has practically no adverse reactions, but when used against tick-borne encephalitis, it can cause a serious allergy, therefore it is used strictly for its intended purpose and under the supervision of a doctor.
What to do if a person is attacked by a tick? The first step is to remove it and urgently go to the hospital.

Regardless of whether the attacked tick was encephalitic, the victim is given a specific immunoglobulin against tick infection for 3 days. Immunoglobulin is injected strictly intramuscularly: with a febrile form daily for 3-5 days, meningeal - every 10-12 hours for 5 days, the dose is 0.1 ml / kg. In more severe forms, for the treatment of tick-borne encephalitis, immunoglobulin against the disease is prescribed in increased doses.
The doctor prescribes further treatment for tick-borne encephalitis depending on the encephalitis form and the severity of symptoms:
- Detoxification and restorative therapy;
- resuscitation measures ( artificial ventilation lungs, oxygen mask, etc.);
- Decreased cerebral edema;
- symptomatic treatment.
In addition, after recovery, the patient remains under the supervision of a neurologist for up to 3 years.
Prevention
Prevention of tick-borne encephalitis is carried out in two directions: vaccination ( specific prophylaxis against tick-borne encephalitis) and preventive measures (non-specific).

Emergency prophylaxis against the encephalitic tick virus is an immunoglobulin that is administered within 3 days after the bite. Immunoglobulin is also administered to unvaccinated individuals in dangerous (endemic) areas. The protective effect lasts about 4 weeks, if the danger persists, immunoglobulin can be re-administered.
If immunoglobulin is more often used for emergency vaccination, then a routine vaccination against an infection is a special vaccine of a killed virus. With the standard vaccination schedule, the first vaccination is carried out from November, the second should be done after 1–3 months, and the third after 9–12 months. In an emergency scheme, the second vaccination can be done after 14 days, the third - after 9-12 months.
What should be done to avoid an insect attack? Non-specific prophylaxis includes the following measures:
- When hiking in the forests, wear thick clothing and use repellents;
- Upon returning, do a thorough examination of exposed areas of the body;
- Boil raw milk from domestic goats and cows;
- If you find a stuck tick, immediately remove it or go to the nearest hospital.
For complete protection against encephalitis ticks in dangerous areas, it is necessary to combine vaccination against dangerous infection and the usual preventive measures.
viral infection, of natural origin, appearing during the period of spring, summer and early autumn.
Infection occurs during absorption into the skin and suction of blood from the human body (in the first minutes of suction) by a tick affected by the encephalitis virus.
Studies have shown that the duration of blood sucking from the human body is about several days, and the body weight of the insect, at the same time, increases many times over.
Infection with this infection is also possible when taking raw milk affected by the infection, or by-products made from a contaminated ingredient (milk).
The presence of the virus in the tissues of the human brain is determined, a few days after the bite (data from a clinical study), and is maximally observed on day 4.
The incubation period of tick-borne encephalitis depends on the method of infection (with a bite of 7-20 days, through food 4-7 days). Not everyone bitten by a tick gets sick. It all depends on immune system organism.
How and when the disease occurs
Infection with tick-borne encephalitis affects people whose activities are carried out in the forest area (workers of timber industry enterprises, geologists, tourists, hunters), less, but still at risk, and urban residents visiting recreation parks, with forest plantations, dachas (garden and garden plots).
For infection, plant branches brought into the house from the forest, parks, summer cottages may also come up.
Ticks are considered carriers. living in the forest expanses, and affected by the infection. Clinical studies conducted on animals have shown that the affected animal (by a tick bite) experienced malaise, lethargy.
And after about 5 days, all the tissues of the organs were damaged by the virus. The accumulation of the virus was observed in the genital tract, intestines and salivary glands.
Pathogenesis
Differs in two reproductions:
- The virus, when bitten by a tick, enters the blood cells. In them (inside) its development takes place, and when fully formed, it moves to the cell membrane, subsequently leaving it.
- Lymph nodes, liver cells, spleen cells are affected, and then the virus enters the motor neurons of the spinal cord, the pia mater and the cells of the cerebellum.
Disease types
In modern medical literature, domestic authors, depending on the period and form of the course of the disease, and the number of deaths, it is permissible to divide infection viruses into the following types as dangers:
- west;
- Siberian;
- Far Eastern.
General signs of the disease
After a trip to an area dominated by a large number of deciduous trees and vegetation, the first signs of tick-borne encephalitis can be suspected when appearance:

Signs of tick-borne encephalitis in of people:
- the appearance of weakness in the limbs;
- the appearance of convulsions, numbness of the facial joints and necks;
- paralysis of individual parts of the muscles, then completely of the limbs.
The development of the disease is acute with distinctive signs:
- chills of the body and fever lasting from 2 to 10 days;
- general malaise of the patient;
- clouding of consciousness;
- different stages of deafness (different degrees).
As the body is covered by the infection, such symptoms of tick-borne encephalitis:
- severe headaches, accompanied by loss of consciousness, vomiting;
- mucosal lesions of the body oral cavity, eye (conjunctivitis develops));
- development coma with loss of time interval and space.
At the same time, patients observed:
- malfunctions of the cardiac system, cardiovascular insufficiency and arrhythmia appear;
- malfunctions of the digestive tract, stool retention is observed, can be detected during an internal check of the organs;
- enlargement of the liver and spleen.
However, throughout the development infectious period, the patient has an elevated temperature in the range of 40 degrees.
Despite severe consequences this disease The disease most often occurs in mild form characterized by slight fever.
Clinical forms of the disease
Experts distinguish between several forms of the disease, depending on the severity of its symptoms:
- feverish;
- meningeal;
- meningoencephalitic;
- polio;
- polyradiculoneuritic.
Symptoms depending on the form of the disease
The symptoms of infection are characterized appearance:
- fever;
- intoxication of the brain (damage to its gray matter), subsequently the development of encephalitis;
- damage to the brain and spinal cord, in particular its membranes, as a consequence of the development of diseases of meningitis and meningoencephalitis.
These diseases are dangerous because, if they are not treated in time, they lead to complications of a neurological and psychiatric nature, as well as to a lethal outcome (death).
Each form of the disease has its own specific first symptoms of tick-borne encephalitis.
Feverish form
Due to the mild course of the disease and a quick cure. Signs of an infection are:
- headache, weakness, nausea;
- the presence of fever, which fluctuates within 3-5 days.

meningeal form
A common form of the disease. The febrile state occurs with increased symptoms (listed below) and lasts from 7 to 14 days:
- headache (at the slightest movement), dizziness;
- nausea with single or repeated vomiting;
- pain in the eyes;
- there is lethargy and lethargy.
Meningoencephalitic form
Often found in the Far Eastern part of the country. It leaks and is heavy. Patients observed:
- delusional state with hallucinations;
- loss of orientation in time and place.
Missed treatment for this type of disease, leads to:
- damage to the brain by reference to the respiratory reflexes of the body;
- numbness of the facial muscles and muscles of the tongue;
- epileptic seizures (possible);
- stomach bleeding with bloody vomit(on rare occasions).
 How is it different from the disease in adults. Special symptoms and methods of treatment of pathology in infants.
How is it different from the disease in adults. Special symptoms and methods of treatment of pathology in infants.
A severe and severe illness is alcoholic polyneuropathy, the treatment of which must be started in a timely manner, otherwise.
Polio form
observed in a third of patients. It begins with a general lethargy of the whole organism, observed for 1-2 days. Accompanied by:
- weakness in the limbs, which can later lead to numbness;
- characterized by pain in the neck.
Subsequently, with rapid, increasing violations of the motor functions of the body. The result is muscle atrophy.
Polyradiculoneuritic form
The patient's nervous system is damaged. Paralysis develops, starting from the legs and subsequently spreading to the entire body, covering the hands of the infected person.
Diagnostics
It is carried out by methods worn in medical literature and reference books titles:
Encephalitis as a disease is more common in children than in adults, occurring against the background of infectious diseases, may occur as a complication after vaccination.
The main symptoms and signs of tick-borne encephalitis in children include:
- the first sign of tick-borne encephalitis is a headache, expressed by a rise in body temperature;
- sleep disorders;
- disorders of the eyeball;
- disorders of the vestibular apparatus.
Treatment of the disease
 There is no specific treatment for tick-borne encephalitis in humans. Applies drug therapy in which antiviral drugs are prescribed.
There is no specific treatment for tick-borne encephalitis in humans. Applies drug therapy in which antiviral drugs are prescribed.
In case of damage to the nervous system, with the development of meningitis or encephalitis, the patient should be urgently hospitalized.
In the treatment of this disease, one can distinguish two ways:
- treatment of tick-borne encephalitis independently;
- help of a specialist.
Help self
It is carried out through traditional medicine.
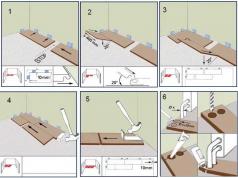
When a tick is found on the body (it looks like a dark bulge, with a substance sticking out from under the skin (the back of the body of the insect)), traditional healers it is recommended to drop a drop on it vegetable oil or any alcohol, and leave for 15-20 minutes.
Under the paws sticking out above the skin of a person, bring a loop-like thread, and with smooth, slow, swaying movements, try to pull it out. The thread can be replaced with tweezers.
The extracted tick must be placed in any container and taken to medical clinic, to determine the presence or absence of infection in it.
Preferably after removing the insect from the skin, contact a specialist in the same hospital to undergo tests for the presence of infection in your body. Infectionists recommend, even if no infection is detected, to be observed by a doctor during the incubation period.
With the appearance of fever, skin rash, itching, an urgent consultation with a specialist is necessary.
Help from a specialist
If, nevertheless, due to a tick bite, an attempt to extract the insect was unsuccessful a positive result, or there was a fear of doing something wrong  action, specialist assistance is needed.
action, specialist assistance is needed.
In the hospital, the tick will be removed from the skin of the patient, and the patient will be given an injection, intramuscularly, against the development of the disease.
Immunoglobulin is an expensive drug, due to the content of antibodies obtained from donated blood, previously vaccinated against tick-borne encephalitis. In addition to this medicine, there are a number of other antiviral drugs, which can be prescribed by a doctor, for preventive and therapeutic purposes.
- drug therapy;
- bed rest;
- rational diet.
Forecast
Data are based on 100 people - 100%:
- Out of a hundred infected patients, complications (neurological and psychiatric) develop in 10-20 people.
- Lethal outcome occurs for the European type: 1-2 people, for the Far Eastern type: 20-25 people. As a rule, death occurs after the appearance neurological symptoms for 5-7 days.
Preventive measures
- The preparatory process is carried out in two stages. The first is in autumn, the second is in winter.
- In case of sudden (extreme) cases, also in two stages, with breaks of two weeks. Immunity, as clinical studies show, develops 14-20 days after vaccination. After 9-12 months, 3 injections should be given.
Everyone, in order to prevent (prevention) must remember:
To date, tick-borne encephalitis is not incurable and, if detected in time, does not cause significant damage to the body.
The key in this case is timely detection of ticks and, therefore, you should especially carefully examine the surface of the skin (especially in children) after visiting the forest.
It should also be remembered that tick-borne encephalitis is not transmitted from one patient to another, it is not dangerous, as viral disease surrounding.
Video: What to do if you have had tick-borne encephalitis
A neurologist talks about what to do next if you were bitten by a tick and the patient suffered tick-borne encephalitis. Very useful advice the doctors.
Ixodid ticks carry dangerous diseases, one of which is tick-borne encephalitis. In order to protect yourself from it, to recognize the onset of infection in time, it is important to know the mechanism of infection, what signs you should pay attention to, how symptoms develop, what consequences occur, how the disease is treated and what are the preventive measures.
What is tick-borne encephalitis
Tick-borne encephalitis is an infectious disease with natural foci. Ticks are carriers. It is isolated from 14 species of the genus Ixodes, and the main role is played by: Ixodes persulcatus and Ixodes ricinus.
Endemic areas: Siberia, Urals, Far East, Arkhangelsk, Leningrad, Irkutsk regions, about. Crimea, Perm, Primorsky Krai, rep. Tatarstan and others.

The peak incidence is in warm time of the year. This is due to the active visits by people to natural foci against the background of an increase in the activity of ticks.
Few people know what an encephalitic tick looks like. In outline, it resembles a spider. However, the structure is more primitive: instead of the typical division into cephalothorax and abdomen, the body consists of a trunk and mouth. The tick moves thanks to 4 pairs of short limbs. There is a hard shield on the back.

There are 2 mechanisms of human infection:
- Transmissible - when biting. It has major epidemiological significance.
- The alimentary mechanism is recorded extremely rarely. Infection occurs through unboiled milk from a diseased goat or cow with viremia.
The causative agent of encephalitis is a small RNA flavivirus coated with a protein coat. Its small size helps it penetrate various body barriers. ultraviolet irradiation and high temperatures cause its destruction, and in the refrigerator, the encephalitis virus remains in products for up to 2 months. In the body of the ixodid tick, the pathogen quickly penetrates into all its organs with maximum accumulation in digestive system. That's why main danger for a person it is precisely the bite of an encephalitic tick.
Entering the ovaries of females leads to the possibility of transmission of tick-borne encephalitis virions to offspring. Favorable conditions of the tick's body provide transphase transmission: the virus passes along with the tick, retaining the ability to infect. This mechanism is important for maintaining the focus of infection.
Spread of the virus in the body
The tick-borne encephalitis virus penetrates through the skin or mucous membranes. gastrointestinal tract. The cells of the immune system are the first to meet it - macrophages, which are found in almost all organs. They specialize in capturing and digesting infectious, foreign agents, dead body cells.

The virus uses macrophages to recreate its own genetic material and assembly, then leaves them, spreading throughout the body hematogenously. The ability of the encephalitis virus to integrate into the DNA of host cells can lead to prolonged asymptomatic carriage, and immune suppression leads to chronic course diseases. Also, the encephalitis virus can cause a dangerous slow infection with a long incubation, after which the first symptoms of the disease rapidly appear with a sharp deterioration.
The circulation of a virus in the blood is called viremia. It has 2 peaks: the first occurs during the initial propagation from the entrance gate. It does not last long, leads to the formation of foci of secondary reproduction in the liver, spleen, blood vessels, lymph nodes. The second peak falls at the end of the incubation period, when the encephalitis virus leaves the internal organs.
The first signs of the disease
The incubation period for tick-borne encephalitis is up to 30 days. When drinking milk, it is the shortest - up to several days. This period of time is dangerous with imaginary well-being, as well as the fact that it is subsequently difficult to associate the symptoms of an encephalitis tick bite with an infection. Painless redness can be seen on the skin - a trace of suction. The development of annular erythema indicates the presence of two tick-borne infections: encephalitis and borreliosis.

In some patients, the incubation period of encephalitis is replaced by nonspecific symptoms - a prodrome. These will be the first signs of encephalitis after a tick bite. They are often mistaken for the development of SARS. This:
- headache;
- weakness;
- fatigue;
- rise in temperature;
- irritability;
- sleep disorders;
- muscle pain;
- weakness in arms, legs;
- paresthesia of the skin of the neck, face.
Symptoms
Symptoms of tick-borne encephalitis indicate the spread of virions and help recognize the disease:
- hyperpyretic fever;
- chills;
- muscle pain;
- headache;
- redness of the face;
- slowing of the heartbeat;
- eye vascular injection;
- drop in blood pressure.
- abdominal pain, bloating, tongue with a white coating;
- hepato-, splenomegaly develop with the penetration of the pathogen into the organs.
- meningeal signs (symptoms of irritation of the meninges).
With damage to the central nervous system are added:
- symptoms of shutdown, clouding of consciousness%
- episyndrome;
- malignant hyperthermia;
- symptoms of local brain involvement.
The first signs of infection with damage to the motor neurons of the spinal cord look like flaccid paresis, paralysis.
Forms of tick-borne encephalitis
With what symptoms tick-borne encephalitis will develop, the set of conditions will determine:- place of introduction of the virus;
- duration of tick suction;
- the total number of ticks per person;
- properties of the encephalitis virus strain;
- properties of the human immune system.
The division of the disease into forms is conditional, since cases are known that begin with clinical signs of one form and then have an atypical development. Also, the symptoms of encephalitis after a bite may not be due to an asymptomatic course.
Let us consider in more detail the main forms of the disease:
feverish
Most victims of a tick bite develop a so-called febrile form of tick-borne encephalitis. It has the following features:
- sudden onset without prodrome;
- pale skin;
- muscle pain;
- pain in eyeballs;
- a sharp rise in temperature to 39 degrees;
- severe intoxication;
- the appearance of symptoms of irritation of the membranes of the brain without inflammation (meningismus).

The elevated temperature persists for 6 days. CSF analysis is not indicative. This is the best quality option. At the exit, asthenic phenomena remain.
Minengial
The meningeal form is often diagnosed. The virus does not cross the membranes of the brain. Signs of tick-borne encephalitis are as follows:
- headache, dizziness;
- pain in the eyeballs, photophobia;
- cerebral vomiting without subsequent relief.

Patients are lethargic, positive persistent signs of irritation of the meninges are inhibited. The duration of the fever is about 3 weeks. Liquor contains a large number of lymphocytes, the content of proteins is increased.
Meningoencephalitic
The meningoencephalitic form appears when the tick-borne encephalitis virus crosses the blood-brain barrier. It is more severe due to the involvement of brain tissue. The fever reaches 40 degrees, its increase is accompanied by severe general somatic symptoms. The duration of the fever reaches 2-3 weeks. Meningoencephalitis can be diffuse or focal.
With diffuse lesions, the clinic is determined by cerebral disorders: epileptic seizures, dysphagia, violent crying, reflexes of oral automatism, delirium.

With a focal lesion, the cranial nerves are involved, unilateral paresis, episyndrome occur. The clinic appears on the 3rd - 5th day of illness.
Poliomyelitis
The poliomyelitis form affects the motor parts of the spinal cord. It begins with a prodromal period, after which the following symptoms of encephalitis appear:- muscle twitches;
- weakness in arms, legs;
- numbness;
- soreness;
- cerebral manifestations;
- flaccid paresis of the neck, muscles of the shoulder girdle, arms.

CSF analysis will show lymphocytosis. There are persistent consequences of tick-borne encephalitis: paresis, atrophy, malnutrition.
Tick-borne encephalitis with a two-wave course begins acutely, with meningeal and general somatic manifestations against the background of the first wave of fever. Analysis of the cerebrospinal fluid is not indicative, leukopenia, an increase in ESR are detected in the blood. The duration of the wave is up to 1 week. This is followed by a fever-free period of up to 2 weeks. The second wave of hyperthermia that follows is more severe. Lethargy, cerebral vomiting, meningeal signs, local manifestations are noted. A blood test will show leukocytosis; CSF pressure is increased, lymphocytosis is pronounced. This option often ends happily.
Polyradiculoneuritis
The polyradiculoneuritic form of tick-borne encephalitis occurs with a lesion peripheral nerves: pain in the arms, legs, numbness, paresthesia. Landry's palsy may join, starting in the legs or shoulder girdle, with involvement of the brain stem.
The severity of the infection can be mild, moderate, or severe. The type of course of tick-borne encephalitis is determined by the properties of the human body and the virus.
Few people know how encephalitis manifests itself in children. The infection manifests as fever. Children's propensity for generalized reactions leads to difficulty timely diagnosis diseases. This means that the child's body cannot localize infectious process due to underdeveloped barriers. Therefore, everything is involved more organ systems with the appearance of bright, but not allowing the correct diagnosis of symptoms:
- stomach ache;
- urinary retention;
- fever that is not relieved by medication;
- vomit;
- sore throat;
- various neurological symptoms.
The course is severe, with frequent mental disorders. Encephalitis is dangerous due to the development of episyndrome, status epilepticus (epistatus). Episyndrome - the appearance of epileptic seizures due to damage to the brain by a virus.
Epistatus is a series of epileptic seizures, going one after another. In the interval between them, a person does not regain consciousness. This condition can cause swelling of the brain and lead to death. Due to the immaturity of the immune system, cases of a chronic course are frequent.
Consequences of tick-borne encephalitis
Some patients do not fully recover from the disease. Then various neurological disorders come to the fore.
The main consequences of encephalitis are:
- persistent headache;
- dizziness;
- ataxia;
- pathology of speech, hearing, vision;
- the formation of paresis, paralysis;
- impaired memory, attention;
- asthenic symptoms;
- psychotic disorders;
- heart failure;
- pneumonia.
Diagnostics
Diagnosis of tick-borne encephalitis includes a set of measures:
Important! If several ticks have been removed, they should be transported separately in signed jars.
- Collection of complaints, medical examination data.
- Laboratory research methods will help establish the diagnosis.

A general blood test will show leukocytosis, an increase in ESR.
With meningeal focal symptoms spinal tap with the study of cerebrospinal fluid will allow you to find signs of inflammation: lymphocytosis, increased protein.
The diagnostic standard is a method (ELISA) that allows you to evaluate the appearance of Ig G, M and track the growth of titer in paired sera (at the beginning and end of the disease).
Detecting viral DNA fragments is possible thanks to the polymerase chain reaction (PCR) method. The material is blood, liquor.
Differential diagnosis is carried out with other neuroinfections, tuberculous meningitis, borreliosis.
Treatment
Important! A tick found on the body must be urgently removed and taken to the laboratory.
In the case of verification of the diagnosis, the etiotropic treatment of tick-borne encephalitis is carried out with the help of injections of a special immunoglobulin. It is used in people examined in the first few days after the tick is sucked. The scheme of administration is selected by the infectious disease specialist.
Patients need to be monitored, so the examination and treatment of encephalitis must be carried out in a hospital. Especially important is constant monitoring in children due to the danger of a sharp deterioration in the condition and death.
In the infectious diseases department, patients are provided with strict bed rest. Treatment includes:
- interferons;
- antipyretic;
- detoxification;
- vitamin preparations;
- neuroprotectors.
If necessary, the treatment is connected:
- hormones, diuretics to prevent cerebral edema;
- anticonvulsants;
- tranquilizers, neuroleptics;
- oxygen therapy.
Disease prevention
Disease prevention measures are divided into specific and non-specific.
Specific planned prevention of tick-borne encephalitis consists in timely vaccination. Vaccination is given to adults and children.
Emergency prevention of encephalitis is carried out by the introduction of immunoglobulin to all persons who applied after a tick bite before laboratory confirmation of the diagnosis.
Non-specific methods include:
- The use of repellents.
- When visiting a forested area, choose light-colored clothing that covers arms and legs, with tight-fitting cuffs, wearing a headdress with fields.
- It is not recommended to sit on the grass, arrange parking, spending the night in areas with tall grass.
- Regular inspections during walks for the timely detection of tick bites.
- Mandatory boiling of milk.
Even a single and short contact with an encephalitis tick can provoke the development of the disease. Attentive attitude to your health will help to avoid terrible consequences and death.