1. General information
A. Insulin-dependent is most common in children and adolescents diabetes(type I), caused by absolute insulin deficiency. Insulin-dependent diabetes mellitus - chronic progressive autoimmune disease, in which destruction of beta cells of the islets of Langerhans occurs. By the time of appearance clinical symptoms 90% of beta cells have already been destroyed. Susceptibility to insulin-dependent diabetes mellitus is at least partly due to genetic factors. In first-degree relatives, the risk of diabetes is 5%, while among the general population it does not exceed 0.1-0.25%. The risk of diabetes in an identical twin reaches 40%.
b. A small number of adolescents develop non-insulin-dependent diabetes mellitus (type II). In non-insulin-dependent diabetes mellitus, ketoacidosis occurs only under stress. Most patients suffer from obesity, which often results in insulin resistance. This may be the cause of impaired glucose tolerance.
V.Secondary diabetes mellitus caused by diseases of the pancreas (cystic fibrosis, pancreatectomy) or excess glucocorticoids.
2. Survey
A.Flow
1) Onset of the disease. Eighty percent of patients see a doctor no later than 3 weeks after the onset of symptoms. The most common complaints are polyuria, thirst, urinary incontinence, weight loss (despite polyphagia), lethargy, fatigue, blurred vision, and in girls - perineal candidiasis. Almost a third of patients are diagnosed with diabetic ketoacidosis at the first visit to the doctor.
2) Remission. A few weeks or months after starting insulin therapy, approximately 2/3 of patients experience partial or complete remission. In case of partial remission to ensure normal level blood glucose requires relatively small doses of insulin (less than 0.5 IU/kg/day). With complete remission, observed in approximately 3% of patients, normal plasma glucose levels are maintained without insulin therapy for at least 3 months. Partial or complete remission can last from several months to 1-2 years, but is eventually replaced by an increase in the need for insulin. Typically, within 5 years of diagnosis, almost all beta cells are destroyed.
3) Exacerbation. Typically, an exacerbation begins gradually: over several weeks or months, the need for insulin increases, and blood glucose levels are unstable. Sometimes remission is interrupted due to infection, emotional stress or physical activity.
4) Stage of complete destruction of beta cells- this is a condition in which C-peptide is absent in the blood; patients are completely dependent on exogenous insulin - a break in its administration for a day or more leads to severe hyperglycemia and ketoacidosis.
b.Laboratory research
1) Fasting and random plasma glucose levels are elevated. Ketonuria does not always happen.
2) It must be remembered that transient hyperglycemia and glycosuria occur in healthy people under stress.
3) Oral glucose tolerance test It has diagnostic value only in the absence of stress. At least 3 days before the test, a diet high in carbohydrates (200-300 g/1.73 m2 per day) is prescribed. In the morning on an empty stomach, give 1.75 g/kg (maximum 75 g) of glucose. A blood sample to determine plasma glucose and insulin is taken immediately before glucose intake and then every 30 minutes for 2 hours.
4) Antibodies to beta cells or insulin indicate high risk insulin-dependent diabetes mellitus. If the first phase of insulin secretion is missing during an IV glucose tolerance test, diabetes mellitus is almost inevitable.
3. Diagnostics
A. Asymptomatic diabetes mellitus is detected using an oral glucose tolerance test: 1) fasting plasma glucose level more than 140 mg%; 2) plasma glucose level 2 hours after taking glucose and in another sample more than 200 mg%.
b. Impaired glucose tolerance is diagnosed when the fasting plasma glucose level is less than 140 mg% and the plasma glucose level 2 hours after ingestion is more than 140 mg%.
V. In case of glycosuria without hyperglycemia, renal glycosuria must be excluded. To do this, the level of glucose in the urine is determined simultaneously with the glucose tolerance test.
4. Treatment
A.Goals. Treatment is aimed at eliminating symptoms, providing wellness, full physical and mental development.
1) The immediate goal is to restore glucose metabolism close to normal, avoiding ketoacidosis and severe hypoglycemia.
2) The long-term goal is to prevent chronic complications of diabetes. According to modern data, maintaining normal plasma glucose levels inhibits the development of late complications, reduces their severity, increases life expectancy and improves its quality.
3) Intensive insulin therapy. Continuous subcutaneous administration or multiple injections of insulin make it possible, subject to medical recommendations, to maintain plasma glucose at a level close to normal. However, such treatment requires discipline from the patient and is rarely used.
b. Compensation for diabetes mellitus is considered satisfactory when:
1) fasting plasma glucose level - 70-140 mg%;
2) plasma glucose level after meals - less than 180-200 mg%;
3) in at least three out of four urine samples the glucose content does not exceed 1%;
4) daily urinary glucose excretion is less than 5-10% of daily carbohydrate intake;
5) the level of glycosylated hemoglobin is no more than 1.35 times higher than upper limit norms;
6) there is no ketonuria;
7) Plasma lipid levels are within normal limits.
V.Patient education- the basis of successful therapy.
1) Education for parents and children begins immediately after the diagnosis of diabetes mellitus. Since in most cases parents are too frustrated to absorb much information, teaching should be gradual. First, they are limited to basic information about the nature of the disease and methods of its treatment, necessary for the child to be discharged from the hospital, treated at home and attending school.
2) Over the next few weeks, basic knowledge about caring for a person with diabetes is supplemented with practical skills training at home. During this time, frequent contact with a doctor or nurse who works with patients with diabetes is necessary.
3) Once the initial shock is over, family members tend to be more receptive to learning about the details of caring for a sick child, what to do about comorbidities, changes in appetite and exercise, and other everyday situations.
4) Training includes not only theoretical knowledge and practical skills; it helps the child adapt to a chronic incurable disease.
5) The curriculum must be appropriate to the child's developmental level. It is compiled individually. Parents bear full responsibility for the patient, but as the child grows older, he learns to independently follow the treatment regimen.
G.Insulin
1) Insulin preparations are divided into three groups depending on the onset, maximum and duration of action after subcutaneous administration. The effect of human insulin NPH (neutral protamine Hagedorn insulin) begins earlier and reaches a maximum faster than the effect of drugs of other types or human insulin Lente, and the duration of the effect is significantly shorter (usually no more than 18 hours; after 12 hours the effect is significantly weakened).
2) During the period of remission, in most cases, a single injection of an intermediate-acting insulin preparation (sometimes in combination with a small dose of short-acting insulin) before breakfast is effective.
A) For persistent nocturnal hyperglycemia, manifested by nocturia or urinary incontinence, as well as for hyperglycemia at bedtime or on an empty stomach, an additional injection of insulin is required before dinner or at night (if short-acting insulin is not administered before dinner).
b) If a single morning dose of intermediate-acting insulin is significantly increased to extend the effect of the drug into the night and early morning hours, then during the period of maximum effect (usually in the afternoon and evening), hypoglycemia and severe hunger usually develop.
3) At the stage of complete destruction of beta cells, a satisfactory result is obtained by administering a combination of short-acting drugs (simple insulin) and medium-acting drugs (NPH insulin or Lente insulin). The drugs are administered in one syringe subcutaneously 2 times a day (30 minutes before breakfast and dinner).
4) The dose of insulin is selected individually. On average, 60-75% of the total daily dose is administered before breakfast, 25-40% before dinner. About a third of a single dose is simple insulin; The optimal ratio of short-acting and intermediate-acting drugs is selected based on plasma glucose monitoring before meals, before bedtime, and between 2 and 3 a.m.
5) With moderate hyperglycemia without ketonuria, initial daily dose insulin is 0.3-0.5 IU/kg s.c. To restore normal plasma glucose levels and eliminate symptoms, a single injection of a medium-acting drug (without short-acting insulin) is sufficient.
A) For ketonuria without acidosis and dehydration, start with 0.5-0.7 IU/kg intermediate-acting insulin in combination with 0.1 IU/kg short-acting insulin subcutaneously every 4-6 hours, maintaining fasting plasma glucose within 80 -150 mg%. The dose is adjusted daily until the desired plasma glucose level is achieved.
b) After normalization of plasma glucose, the dose is adjusted no more than once every 3 days, changing it by approximately 10%. In case of acute disorders of glucose metabolism, the dose is adjusted more often.
6) Injection sites need to be changed to avoid lipohypertrophy, which alters insulin absorption. For subcutaneous injections, the extensor surface of the arms, the anterior surface of the thighs, buttocks and the anterior abdominal wall are used.
7) Parents, and eventually children, are taught how to select, mix and administer insulin. As a rule, a child over 12 years of age can and should be able to inject himself with insulin under parental supervision.
8.) Dose adjustment
A) Insulin requirements change during different periods of illness, as growth and sexual development progress, and as physical activity changes (in most children, activity increases significantly in the spring and summer, and smaller doses of insulin are required at this time). Therefore, the insulin therapy regimen is periodically reviewed.
b) During the period of remission, the need for insulin is less than 0.5 IU/kg/day; Sometimes insulin administration can be stopped altogether for several months.
V) During the period of exacerbation and at the stage of complete destruction of beta cells, the daily dose of insulin in prepubertal children ranges from 0.5-1 IU/kg; in the puberty period it is 0.8-1.5 IU/kg.
G) Doses of insulin exceeding those indicated are rarely required. In such cases, post-hypoglycemic hyperglycemia due to insulin overdose (Somogyi syndrome) should be suspected. We should not forget about the extremely rare occurrence of insulin resistance, which occurs due to dysfunction of insulin receptors.
d.Diet
1) General principles
A) Need in nutrients ah in diabetes mellitus is the same as in healthy children. The total amount of calories and nutrients in the diet should be sufficient for normal growth and compensation of energy costs.
V) The diet is periodically reviewed to achieve the ideal weight and ensure normal growth and development of the child.
G) The main goal of diet therapy for non-insulin-dependent diabetes mellitus against a background of obesity is to reduce weight and maintain it at this level.
d) Meals should be coordinated with the administration of insulin. Food must be taken strictly at the same time of day, and the daily amount of calories and the ratio of carbohydrates, proteins and fats in the diet must be constant. Because insulin is constantly released from the injection site, hypoglycemia may develop in the absence of additional snacks between meals and may worsen during exercise. Therefore, most children receiving two insulin injections per day need to eat something between breakfast, lunch and dinner, and before bed. A light snack should also precede intense physical activity (unless plasma glucose levels are very high).
2) Product interchangeability
A) The diet is prepared with the participation of a nutritionist. Using a list of interchangeable products (“replacement lists”) allows you to take into account ethnic and religious traditions, the economic capabilities of the family, as well as the tastes of the child.
b)“Replacement lists” include six basic foods: milk, fruits, vegetables, bread, meat and fats. Products included in the “replacement list” contain approximately the same amount of carbohydrates, fats and proteins (the weight or serving size of each product is indicated). The menu should include interchangeable products from all main groups.
3) Fat consumption. Since patients with diabetes are predisposed to atherosclerosis, the amount of fat in the diet should not exceed 30% of the daily energy requirement, and cholesterol intake should not exceed 300 mg/day. The content of polyunsaturated fatty acids in the diet is increased, and the content of saturated fatty acids is decreased, including less beef and pork in the diet and more lean meat, chicken, turkey, fish, skim milk and vegetable proteins.
4) Cellulose reduces the increase in plasma glucose levels after meals. Soluble fiber helps reduce serum cholesterol levels. Therefore, it is recommended to eat raw or minimally processed foods - vegetables, wholemeal flour, legumes.
5) Fruits. To prevent sharp increase plasma glucose levels, you need to eat fresh fruits and avoid drinking fruit juices. Fruit juices are only indicated for hypoglycemia.
e. The effect of physical activity on diabetes can be different.
1) Physical activity, depending on its intensity and duration, as well as the level of insulin in the blood, sharply reduces plasma glucose levels. The physical activity of children is usually unpredictable, which makes it practically impossible to dose the load. Therefore, increased energy consumption is compensated by additional food intake before physical activity, and sometimes during it (if the exercise is long-term). A rule of thumb is to compensate for every 30 minutes of intense physical activity with 15 grams of carbohydrate. Significant physical activity in the afternoon or evening requires a reduction in the dose of average-acting insulin administered before dinner by 10-20%, as well as a larger snack before bed. These measures prevent nighttime and morning hypoglycemia.
2) With hyperglycemia and ketonuria, a sharp increase in physical activity can increase hyperglycemia and stimulate the formation of ketone bodies. Therefore, physical activity is limited until satisfactory compensation of diabetes mellitus is achieved.
3) The work of the muscles of the limb into which insulin was injected accelerates its absorption. Therefore, if physical activity is to be performed, it is recommended that the injection be made in that part of the body whose muscles will not be involved in the work.
4) Physical training increases tissue sensitivity to insulin. For adolescents who regularly engage in sports, the dose of insulin administered before physical activity is reduced to 70-90% of the usual.
and.Monitoring
1) Blood glucose determination
A) The preferred method of monitoring is self-monitoring of blood glucose levels. Patients with insulin-dependent diabetes mellitus need to be taught how to test blood glucose and ensure that they get accurate results. Frequent self-monitoring of blood glucose levels in combination with urine ketone testing is important during concomitant illnesses. In addition, it helps prevent ketoacidosis. Blood glucose levels measured at home using various devices with a digital display differ from the results obtained in a clinical laboratory by no more than 10%.
b) Ideally, patients should measure their blood glucose levels before each meal and at bedtime. If for some reason this is not possible, glucose levels are measured before each insulin injection and at least 2 times a week before lunch and before bed. If patients are unable to monitor as frequently or are unable to purchase test strips, it is possible to test glucose levels for just a few days in a row before visiting the doctor (before each meal, before bed, and between 2 and 3 a.m.). This information is sufficient to assess the effectiveness of treatment and its correction.
V) Monitoring may be inaccurate due to incorrect recording of results or incorrect research methodology. The most common causes of errors are the following: a drop of blood does not completely cover the test strip; the time required to complete the reaction is not observed; Too much blood is wiped off the test strip. Modern measuring instruments avoid some of these difficulties.
2) Urine tests
A) Urinary glucose levels are rarely used to assess the effectiveness of therapy. This is due for the following reasons: it correlates weakly with plasma glucose levels; the absence of glucosuria does not make it possible to distinguish hypoglycemia from normal or even slightly elevated plasma glucose levels, so parents, fearing hypoglycemia, often reduce the dose of insulin.
b) Determination of ketone bodies in urine is indicated when concomitant disease, plasma glucose levels above 250 mg% and plasma glucose levels too high before breakfast. In the latter case, nocturnal hypoglycemia with “rebound” hyperglycemia can be suspected.
3) Glycosylated hemoglobin. Assess the effectiveness of therapy based on symptoms, urine tests and rare blood tests at home or outpatient setting inaccurate Therefore, in order to objectively assess the average plasma glucose level for 3 months, the level of glycosylated hemoglobin, which is formed by the non-enzymatic addition of glucose to the hemoglobin molecule, is determined quarterly. This indicator is directly proportional to the average plasma glucose level over the previous 2-3 months.
5. Acute complications diabetes mellitus
A.Hypoglycemia
1) Attacks of hypoglycemia during insulin therapy are almost inevitable. It is necessary to treat in such a way that the frequency and severity of hypoglycemia attacks is minimal.
2) The most common causes of hypoglycemia are increased physical activity that is not compensated by previous food intake; long-term intense physical activity without reducing the insulin dose; increasing the intervals between meals or not eating the usual portion; accidental insulin overdose and wrong mode insulin therapy.
3) Patients and their families must learn to recognize early symptoms hypoglycemia and quickly eliminate them with concentrated carbohydrates. In most cases, attacks of hypoglycemia are eliminated by taking 10-20 g of glucose. For children under 2 years old, 5 g is enough. Glucose can be given in the form of tablets (5 g each), sugar, orange or apple juice.
4) Family members are taught glucagon injections (the drug should be kept in your home medicine cabinet). It is given for severe hypoglycemia when the child is unconscious or unable to take carbohydrates. The dose is 0.02 mg/kg (maximum 1 mg) IM or SC; Plasma glucose levels rise 5-15 minutes after injection. Glucagon may cause nausea and vomiting. If hypoglycemia is caused by an overdose of insulin, then after regaining consciousness, it is necessary to take carbohydrates to prevent a recurrence of the attack.
5) If taking sugar-containing solutions is not possible, administer 5-10 g of glucose intravenously, after which a long-term infusion is established at a rate of at least 10 mg/kg/min, monitoring plasma glucose levels.
6) A person with diabetes must wear an identification bracelet or medallion.
b.Diabetic ketoacidosis
1) Survey.
A) To make a diagnosis, identify the cause of diabetic ketoacidosis (especially infection), and assess the degree of dehydration, a physical examination, weight and height are measured (the examination should be prompt).
b) Plasma glucose levels (using a test strip) and plasma ketone bodies are determined at the patient's bedside.
V) A blood sample is taken to determine hemoglobin, hematocrit, leukocyte formula, levels of electrolytes (including calcium and magnesium) and phosphate, plasma CO 2, BUN, pH, pCO 2, pO 2. The anion gap is calculated using the formula: Na + – (Cl – + CO 2 plasma); normally it is 12 ± 2.
G) Conduct a urine test; They take material for culture - blood, urine and throat swabs.
d) Plasma potassium levels are determined and an ECG is recorded.
e) A neurological examination is performed.
2) Supportive measures
A) If consciousness is depressed, the contents of the stomach are removed through nasogastric tube to prevent aspiration.
b)For fever after taking material for culture, antibiotics are prescribed wide range actions.
V) In case of shock, cyanosis, p a O 2 is below 80 mm Hg. Art. Oxygen is prescribed.
G) Diuresis is determined as accurately as possible. If necessary, catheterize bladder or use condom catheters.
d) Careful monitoring of clinical and biochemical parameters is required to allow timely adjustment of therapy. To do this, a special card is created in which the results of clinical and laboratory tests (including diuresis), details of infusion therapy, and insulin administration are recorded.
e) Severe patients are placed in intensive care or another department where continuous monitoring of clinical and laboratory parameters is possible.
3) Correction water and electrolyte disturbances . In diabetic ketoacidosis, there is always dehydration and deficiency of sodium, potassium, magnesium, chloride and phosphate. In mild to moderate diabetic ketoacidosis, approximately 5% of weight is lost, and in severe diabetic ketoacidosis, about 10% is lost.
A) First of all, saline solution is administered, 10-20 ml/kg IV over 60 minutes through a large-diameter catheter. If arterial hypotension or shock persists, another 10-20 ml/kg of physiological or colloidal solution is administered over the next 60 minutes.
b) After normalization of hemodynamics, water loss is replenished with a 0.45% NaCl solution. Half the volume is administered in the first 8-16 hours, the rest in the next 16-20 hours.
V) As soon as the plasma glucose concentration drops to 250-300 mg%, 5% glucose is added to the infusion solutions. Sometimes 10% glucose is used to prevent hypoglycemia.
G) At the beginning of treatment, continued water loss is largely due to osmotic diuresis. They are compensated by 0.45% NaCl with added potassium. After a positive water balance has been established, the volume of injected solutions is reduced to the minimum water requirement (1500-2000 ml/m2/day).
4) Several insulin therapy regimens for diabetic ketoacidosis have been developed.
A) The preferred method is continuous IV administration of low doses of insulin using an infusion pump. Simple insulin at a dose of 50 IU is diluted in 50 ml of saline. After an intravenous injection of 0.1-0.25 IU/kg of insulin, its infusion is established at a rate of 0.1 IU/kg/h. In most cases, these measures are sufficient to eliminate diabetic ketoacidosis. If, due to insulin resistance, plasma glucose levels and anion gap do not decrease, the infusion rate is increased until an effect is achieved. Rarely, in severe insulin resistance, low-dose insulin is ineffective; in such cases, the dose is increased 2-3 times. Long-term infusion allows you to regulate the rate of insulin administration, reducing the risk of hypoglycemia and hypokalemia. The disadvantage of this method is the rapid cessation of insulin action after the drug stops entering the blood. The fact is that T1/2 of insulin is approximately 5 minutes, that is, after stopping the infusion, its level in the serum drops by 50% every 5 minutes. Therefore, careful monitoring is necessary during low-dose continuous infusion of insulin.
b) After elimination of diabetic ketoacidosis, when the pH of the venous blood is more than 7.32 and plasma CO 2 is more than 18 meq/l, they switch to subcutaneous administration of insulin. The first subcutaneous injection is carried out at least 1-2 hours before the end of the intravenous infusion, so that the insulin has time to be absorbed into the blood.
V)IM injection Insulin also reduces plasma glucose levels and eliminates acidosis. It does not require special equipment, however, IM injections must be frequent and, in addition, with arterial hypotension, insulin absorption fluctuates greatly. First, administer 0.1-0.5 IU/kg IV bolus, and then 0.1 IU/kg IM every hour until the plasma glucose level drops to 300 mg%. After this, they switch to subcutaneous administration.
5) Compensation for potassium deficiency
A) All patients with diabetic ketoacidosis develop hypokalemia (potassium deficiency - 3-10 mEq/kg), although plasma potassium levels may be normal or even elevated before treatment. The administration of infusion solutions and insulin can cause severe hypokalemia and, as a consequence, cardiac arrhythmias. If plasma potassium levels were reduced before treatment, hypokalemia worsens; in this case, potassium is administered immediately after diuresis is restored and insulin is administered, and its plasma level is determined hourly.
b) Plasma potassium levels are maintained within 4-5 mEq/L. If the results of measuring the initial (before treatment) potassium level are not obtained within an hour, and insulin has already been administered and diuresis has been restored, potassium administration is continued.
V) Half of the potassium dose is administered in the form of chloride, and the other half in the form of phosphate, which reduces the dose of chloride administered and partially compensates for the phosphate deficiency. For hyperchloremia, potassium acetate is administered instead of chloride.
G) To assess the results of treatment, an ECG is recorded at intervals of 30-60 minutes, paying attention to the configuration of the T wave in lead II and V2.
J. Gref (ed.) "Pediatrics", Moscow, "Practice", 1997
If parents from an early age teach their child to healthy image life, in the future diabetes will not prevent him from achieving heights. The main thing is to accept the diagnosis and not give up.
Video to the text:
School of Doctor Komarovsky
Live healthy
Diabetes mellitus in children: how the disease develops, recommendations for prevention and treatment
Diabetes mellitus in children is not so much a physical problem as a psychological one. Sick children have a harder time adapting to a group environment; unlike adults, it is more difficult for them to change their usual lifestyle.
A disease such as diabetes mellitus is part of the group of endocrine disorders with signs of hormone deficiency thyroid gland– insulin. The pathology is accompanied by a constant increase in the amount of glucose in the blood.
The mechanism of the disease is characterized chronic form, provokes the appearance of symptoms characteristic of the disease alarming symptoms and is accompanied by a failure of all types of metabolism - protein, mineral, fat, water, salt, carbohydrate.
Diabetes mellitus in children has no age restrictions and can appear at the most unexpected moment. Presence of disorders endocrine system present in infants, preschoolers and adolescents.
Childhood diabetes is in second place on the list of the most common chronic diseases.
Just as in adult diabetics, this form of the disease in children is aggravated by additional symptoms. With timely detection of pathology and hasty adoption of the necessary measures to prevent the consequences of diabetes, it is possible to achieve positive results and significantly alleviate the child’s suffering.
 Impaired carbohydrate metabolism is the main cause of diabetes in children at any age. Scientists were able to track other factors influencing the development of the disease in children. Some of them have been studied in detail, but some reasons still remain classified as unknown.
Impaired carbohydrate metabolism is the main cause of diabetes in children at any age. Scientists were able to track other factors influencing the development of the disease in children. Some of them have been studied in detail, but some reasons still remain classified as unknown.
This does not change the essence of diabetes and comes down to the main conclusion - problems with insulin will forever change the life of a sick child.
The first symptoms of diabetes in children: how to recognize them
Understanding that a child has diabetes is always difficult at the initial stage. The symptoms are almost invisible. The speed of manifestation of the disease depends on its type - first or second.
With type I diabetes, symptoms progress rapidly, and the child changes during the first week. Type II diabetes is characterized by severity; symptoms appear less quickly and less clearly. Parents do not notice them and do not take the child to the doctor until complications occur. In order not to aggravate the situation, it would be a good idea to find out how diabetes mellitus manifests itself in children.
Let's look at the most common symptoms of childhood diabetes:
 So that the child’s body receives an energy reserve for proper organization vital activity, insulin must convert part of the glucose entering the blood. If diabetes has already begun to develop, the need for sweets may increase. This is due to the hunger of the body cells, because in diabetes there is a disturbance in carbohydrate metabolism and not all glucose is transformed into energy.
So that the child’s body receives an energy reserve for proper organization vital activity, insulin must convert part of the glucose entering the blood. If diabetes has already begun to develop, the need for sweets may increase. This is due to the hunger of the body cells, because in diabetes there is a disturbance in carbohydrate metabolism and not all glucose is transformed into energy.
For this reason, the child is always reaching for sweets. The adult's task is to distinguish pathological process from the love of sweets.
 A child with diabetes often experiences a feeling of hunger. Even if children eat enough food, they find it difficult to wait next appointment food.
A child with diabetes often experiences a feeling of hunger. Even if children eat enough food, they find it difficult to wait next appointment food.
This can cause headaches and even trembling legs and arms. Children constantly ask for food and choose high-carbohydrate foods - flour and fried foods.
Decreased motor ability.
A diabetic child experiences an overwhelming feeling of fatigue and lacks energy. He gets irritated for any reason, cries, and does not even want to play his favorite games.
If you notice frequent recurrence of one or more symptoms, consult your doctor and get a blood glucose test.
Children are not always able to objectively assess their needs and weaknesses, so parents must be vigilant.
Signs of diabetes in a child: what precedes the disease

In addition to the symptoms of the first stage, the disease is subsequently accompanied by more obvious signs
 One of the most striking manifestations of diabetes. Adults need to monitor the child's fluid intake. With diabetes, children experience a constant feeling of thirst. A sick baby can drink more than 3 liters of water per day, but his mucous membranes will remain dry and the feeling of thirst will not be dulled.
One of the most striking manifestations of diabetes. Adults need to monitor the child's fluid intake. With diabetes, children experience a constant feeling of thirst. A sick baby can drink more than 3 liters of water per day, but his mucous membranes will remain dry and the feeling of thirst will not be dulled.
2. Polyuria, or frequent and increased urination.
Due to constant thirst and large amounts of fluid drunk, children suffering from diabetes urinate more often than their healthy peers.
 A large amount of urine excreted is associated with the amount of fluid consumed. In one day, a child can go to the toilet about 15-20 times, and at night the child can also wake up due to the desire to urinate. Parents confuse these signs with a problem associated with frequent urination - enuresis. Therefore, for diagnosis, the signs should be considered together.
A large amount of urine excreted is associated with the amount of fluid consumed. In one day, a child can go to the toilet about 15-20 times, and at night the child can also wake up due to the desire to urinate. Parents confuse these signs with a problem associated with frequent urination - enuresis. Therefore, for diagnosis, the signs should be considered together.
 Even despite increased appetite and consumption of sweets, children with diabetes may experience weight loss. Although initially the weight, on the contrary, may increase slightly. This is due to physiology during times of insulin deficiency. Cells do not have enough sugar to generate energy, so they look for it in fats, breaking them down. This is how weight decreases.
Even despite increased appetite and consumption of sweets, children with diabetes may experience weight loss. Although initially the weight, on the contrary, may increase slightly. This is due to physiology during times of insulin deficiency. Cells do not have enough sugar to generate energy, so they look for it in fats, breaking them down. This is how weight decreases.
 You can also understand that a child has diabetes based on this sign. Even minor abrasions and scratches heal very slowly. This is due to impaired functioning of the vascular system due to a sustained increase in blood glucose levels. In this critical situation, contacting an endocrinologist is inevitable.
You can also understand that a child has diabetes based on this sign. Even minor abrasions and scratches heal very slowly. This is due to impaired functioning of the vascular system due to a sustained increase in blood glucose levels. In this critical situation, contacting an endocrinologist is inevitable.
5. Dermopathy, or skin lesions.
Children often suffer from diabetes due to skin diseases. Rashes, sores and spots may appear on various parts of the body. This occurs due to decreased immunity, disturbances in metabolic processes and blood vessels.
 If there is no energy, the child has no strength to play or move. He becomes weak and anxious. Diabetic children lag behind their friends academically and are not as active in physical education classes.
If there is no energy, the child has no strength to play or move. He becomes weak and anxious. Diabetic children lag behind their friends academically and are not as active in physical education classes.
After coming home from educational institution the child wants to sleep, looks tired, does not want to communicate with anyone.
 Another characteristic sign of diabetes. The air near the child smells of vinegar or sour apples. This is clear evidence that the amount of ketone bodies in the body has increased. It is worth going to see a doctor immediately, otherwise the child may fall into a ketoacidotic coma.
Another characteristic sign of diabetes. The air near the child smells of vinegar or sour apples. This is clear evidence that the amount of ketone bodies in the body has increased. It is worth going to see a doctor immediately, otherwise the child may fall into a ketoacidotic coma.
Knowledge is your power. If you are familiar with the symptoms of diabetes in children, you can avoid severe consequences pathologies and alleviate childhood pain.

The clinical picture of the disease differs in children of different age categories. We invite you to familiarize yourself with the differences in the development of diabetes in accordance with age-related changes.
Signs of diabetes in infants
It is not easy to detect the disease in newly born children. It is very difficult to understand whether a baby is experiencing polyuria (increased urination) or polydipsia (thirst) from his usual state of health. Pathology may be accompanied by other signs: vomiting, intoxication, dehydration and even coma.
 If diabetes develops slowly, the baby slowly gains weight, sleeps poorly and does not want to eat, often cries, and suffers from bowel problems. For a long time Babies may suffer from diaper rash. Skin problems begin: prickly heat, allergies, pustules. Another thing that should attract attention is the stickiness of urine. Once dry, the diapers become hardened, and when they come into contact with the surface, the stain sticks.
If diabetes develops slowly, the baby slowly gains weight, sleeps poorly and does not want to eat, often cries, and suffers from bowel problems. For a long time Babies may suffer from diaper rash. Skin problems begin: prickly heat, allergies, pustules. Another thing that should attract attention is the stickiness of urine. Once dry, the diapers become hardened, and when they come into contact with the surface, the stain sticks.
Causes of diabetes mellitus in young children
The development of diabetes occurs at an accelerated rate in children older than 1 year. The onset of a precomatose state will be preceded by the following signs:

Type I diabetes mellitus in children of this age is associated with genetic disposition and heredity.
Cases of type II diabetes mellitus in preschool children are observed more often than type I. This happens due to uncontrolled consumption of unhealthy foods, fast food, rapid weight gain, and lack of exercise.
How diabetes mellitus manifests itself in schoolchildren
Detection of diabetes in children school age will be preceded by signs:

All these physical factors combined with psychological, so-called atypical manifestations of diabetes mellitus:
- Anxiety and depression;
- Fatigue and weakness;
- A drop in academic performance;
- Reluctance to contact peers.
If you notice at least one of these signs, do not ignore the situation.
At first, parents attribute diabetic symptoms to fatigue from school. Moms and dads, love your children, do not ignore their problems and worries.
The first signs of diabetes in adolescents
Adolescent diabetes is a phenomenon that occurs after 15 years of age. Symptoms of diabetes mellitus in adolescents are typical and, if left untreated, get worse.
The most common symptoms of diabetes in adolescents are:

The clinical picture of adolescent diabetes is as follows: high level glucose in the blood provokes thirst, which does not decrease even after drinking a large amount of liquid; and frequent visits to the toilet for minor needs - both during the day and at night.
Diabetes mellitus in girls during adolescence manifests itself in disorders menstrual cycle. This serious disorder can lead to infertility. When a girl develops type II diabetes, polycystic ovary syndrome may begin.
Diabetes mellitus of both types in adolescents occurs with symptoms of vascular disorders, blood pressure may increase, and there is an increase in cholesterol in the blood. Blood microcirculation in the legs is disrupted, the teenager experiences a feeling of numbness and suffers from cramps.
 With late diagnosis of diabetes mellitus in adolescents, the clinical picture of the disease is associated with accumulation of ketone bodies in the blood. This happens due to a significant increase in blood glucose levels and a simultaneous energy deficit.
With late diagnosis of diabetes mellitus in adolescents, the clinical picture of the disease is associated with accumulation of ketone bodies in the blood. This happens due to a significant increase in blood glucose levels and a simultaneous energy deficit.
The body strives to compensate for this deficiency by producing ketones.
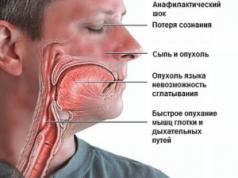
Primary signs of ketoacidosis are abdominal pain and nausea, secondary signs are weakness and vomiting, frequent difficulty breathing, the smell of acetone when exhaling. The progressive form of ketoacidosis is loss of consciousness and coma.
Causes of ketoacidosis in adolescents include:
- In the first place among preventive measures is the organization of proper nutrition. It is necessary to maintain water balance at all times, because in addition to insulin, the pancreas produces water solution bicarbonate, a substance that stabilizes the process of glucose penetration into the body's cells.

Children suffering from diabetes should make it a rule to drink a glass of clean drinking water before each meal. And this is the minimum requirement. Coffee, sweet drinks, and carbonated water do not count toward your fluid intake. Such drinks will only do harm.
If the child excess weight(most often with type II diabetes), reduce calories in food as much as possible. Calculate not only carbohydrates, but also vegetable and animal fats. Your child needs to eat more often, but not a lot. Follow the recommendations for proper nutrition with your child. It is easier to overcome difficulties with company.
Include vegetables in your children's diet and prepare original dishes from them. Let your child fall in love with beets, zucchini, cabbage, radishes, carrots, broccoli, onions, garlic, beans, rutabaga, and fruits.
Treatment of diabetes mellitus in children
The main areas of treatment for childhood diabetes include:
Self-medication of diabetes can lead to unpredictable scenarios. Influence traditional medicine not fully studied. Therefore, you should not conduct experiments with your child, you should not seek help from traditional healers. Treatment of the disease in adults and children is different.
Many of the advertised drugs contain large amounts of hormones; when they enter the body, they can behave in any way. A large number of side effects will only worsen the condition of the sick child and adversely affect the function of the pancreas.
If your child has been diagnosed with diabetes, do not despair. The situation you and your baby find yourself in is serious. You shouldn't expect magic from medications.
Diabetes mellitus is a chronic disease that occurs when there is a lack of the pancreatic hormone insulin. Diabetes is one of the most frequent illnesses endocrine system in children. The prevalence of diabetes mellitus among the pediatric population (including children at an early age) has currently increased. Newborn children rarely get diabetes; it often appears during puberty.
Types of diabetes
In most cases, children develop type 1 diabetes.To ensure all functions, the body needs energy. It mainly receives this energy from processing glucose (or sugar) when it enters the cell. Insulin takes part in the process of converting sugar into energy.
It is this that ensures the flow of sugar into the cell for further conversion into energy. The amount of insulin in the body changes: food intake promotes the synthesis and release of the hormone, and less is produced during sleep and under the influence of certain medications.
After eating carbohydrates, your blood sugar levels rise. But under the influence of insulin, glucose is absorbed by the cells of the whole body, and therefore its level gradually (over about 2 hours) decreases to normal indicators(3.3-5.5 mmol/l). After this, the pancreas stops secreting insulin.
When there is not enough insulin, blood glucose levels are elevated because it is not absorbed by cells, and diabetes develops. There are types 1 and 2 of this disease (insulin-dependent and insulin-independent, respectively). In type 1, the disease is the result of damage to the pancreas.
With type 2, iron synthesizes insulin in sufficient quantities, but the body's cells (their receptors) do not respond to it and do not use sugar from the blood; its level remains high.
Children more often develop insulin-dependent type 1 disease.
Causes
There are many reasons for the occurrence of this disease in children:
- Predisposition to disease plays a significant role, that is, a hereditary factor. If both parents suffer from this disease, then 80% of their children will have underdevelopment or damage to pancreatic cells. They will be at high risk of developing the disease, which may appear soon after birth or years or decades later. The presence of diabetes may predispose to the disease not only in the child’s parents, but also in other, less close relatives.
- Increased glucose levels in a woman during pregnancy are also an unfavorable factor for the child: glucose freely passes through the placental barrier. Its surplus (the child has little need for it) is deposited in subcutaneous fat layer, and babies are born not only with a large body weight (5 kg, and sometimes higher), but also with a risk of developing diabetes in the future. Therefore, a pregnant woman should adhere to the recommended diet, and parents should not rejoice (as is usually the case) when a child is born with a large weight.
- Feeding children with plenty of easily digestible foods carbohydrates (chocolate, sweets, sugar, confectionery and flour products) leads to excessive load on the pancreas and its depletion: insulin production decreases.
- Excess body weight of a child leads to the deposition of fat in the body. Fat molecules contribute to changes in cell receptors, and they stop responding to insulin; Sugar is not utilized even if there is sufficient insulin.
- A child's sedentary lifestyle contributes to excess body weight. In addition, physical activity itself causes increased work of all tissues in the body, including pancreatic cells. Thus, with active movements, blood sugar levels decrease.
- Parents who are addicted to unreasonable stimulation of the immune system in children should keep in mind that by doing so they cause a disruption in the interaction of two systems: activation and inhibition immune reactions. At the same time, the body begins to constantly produce antibodies. If antibodies "do not detect » microorganisms, they destroy the cells of the body itself, including the cells of the pancreas. The occurrence of such a pathological immune reaction may also be associated with the child’s frequent colds or viral infections. Particularly unfavorable in this regard are the mumps and hepatitis viruses.
- The trigger for the development of diabetes in childhood may be allergic reaction(including cow's milk), exposure to harmful chemical factors, the use of certain medications (etc.), stress or excessive physical activity.
Symptoms
 Constant thirst in a child may indicate increased blood sugar.
Constant thirst in a child may indicate increased blood sugar. Diabetes in children has several stages:
- There is a predisposition to the disease.
- The pancreatic tissue is already affected, but there are no manifestations of the disease yet; it can only be diagnosed with the help of special examinations.
- Diabetes has clinical manifestations, and its diagnosis at this stage is not difficult.
Specifics of the course of diabetes mellitus in children:
- correct treatment in the initial, hidden form gives a good result;
- if left untreated, the disease progresses rapidly;
- more severe course than in adults.
In the initial stage of the disease, blood sugar levels can increase only under certain circumstances or stress, and in later stages, even in the morning on an empty stomach. Not only carbohydrate metabolism is disrupted, but also other metabolic processes, protein synthesis, etc.
Acetone and under-oxidized metabolic products accumulate in the child’s body, which have a detrimental effect on the nervous and cardiovascular systems. Diabetes leads to problems in immune system, liver.
You can suspect this insidious disease in children based on the following signs:
- increased thirst: children can drink several liters of water per day, they wake up even at night to drink water.
- Frequent urination (sometimes even up to 20 rubles per day); Normally, children urinate approximately every 6 p.m. per day; enuresis or bedwetting may occur; urine is almost colorless and odorless, but on diapers or underwear it can leave sticky marks or stains reminiscent (after drying) of starch.
- Dryness of mucous membranes and skin due to the excretion of fluid in the urine; Diaper rash, itching and inflammation of the external genitalia may appear in girls.
- Loss of body weight with a good (and sometimes even increased) appetite; only in more late stages disease and in newborns with diabetes, absence or sharp deterioration of appetite is observed.
- Decreased visual acuity is associated with clouding of the lens due to the deposition of sugar in it; The retinal vessels are also affected due to the toxic effect of glucose.
- Unreasonable fatigue and general weakness in a child occurs due to insufficient energy supply to the body; children begin to study worse, they are inactive, may lag behind in physical development, and complain of a headache at the end of the day; The child is characterized by apathy and drowsiness.
- With a decrease in immune reactions, pustular and fungal infections skin, scratches that do not heal for a long time.
- The muscle layer becomes flabby.
- Bones are brittle and do not heal well during fractures due to...
Severe drowsiness of the child, abdominal pain and vomiting, the smell of acetone or pickled apples from the mouth: this condition requires immediate medical attention and examination of the child.
 Incidence chart for the Moscow region in 2008
Incidence chart for the Moscow region in 2008 In some cases, children are admitted to the hospital already in a condition requiring resuscitation measures. In severe cases of diabetes, the the cardiovascular system:, the rhythm of cardiac activity is disturbed, pain in the heart area may bother you.
Diabetes mellitus leads to disruption of the structure and function of the kidneys, and inflammatory processes often occur in them. It is also affected digestive system: it is possible to develop a disease of any of its organs.
The liver is enlarged, and even development may occur.
Diagnostics
Clinical manifestations of the disease can be confirmed by blood sugar testing. Normal blood sugar levels are from 3.3 to 5.5 mmol/l. An increase in glucose levels up to 7.5 mmol/l can be observed with latent diabetes mellitus. Blood sugar levels above this level indicate confirmation of diabetes.
There is also a diagnostic glucose tolerance test. First, the fasting blood sugar level is determined, then 75 g of glucose is given to drink (dissolved in water); Children under 12 years of age are given 35 g. After 2 hours, a finger prick blood test for glucose is repeated. If the indicator is 7.5-10.9 mmol/l, then there is hidden form diseases; a reading of 11 mmol/l or higher confirms the diagnosis of diabetes mellitus.
In addition, an ultrasound of the organs is performed abdominal cavity in order to exclude the inflammatory process in the pancreas.
Treatment
 Proper nutrition is the basis of diabetes treatment.
Proper nutrition is the basis of diabetes treatment. Treatment is selected for the child by a pediatric endocrinologist depending on the type of diabetes mellitus.
For type 1 diabetes mellitus(it accounts for 98% of cases of “childhood” diabetes) is carried out replacement therapy, that is, insulin is injected, which is not available or is not sufficiently secreted by the pancreas.
At the same time, the child must be provided with proper nutrition, avoiding starvation. In addition to the main meals, include intermediate ones (mainly the consumption of fruits and vegetables).
This is necessary to avoid the development of complications of diabetes in the form of hypoglycemic coma, which develops when a larger dose of insulin is administered than is needed for food processing. In this case, the entire supply of sugar in the body is consumed and energy starvation of the brain develops first. This condition sometimes even requires resuscitation measures.
Hypoglycemic coma develops very quickly, in 20-30 minutes. Suddenly there is a sharp weakness, severe sweating, trembling in the body, and a feeling of hunger. Headache, double vision, palpitations, nausea, vomiting, numbness of the tongue and lips may occur. The mood changes: from depressed to excited and even aggressive. If help is not provided, then visual and auditory hallucinations, unmotivated actions, then convulsions and loss of consciousness occur.
The child should always have a chocolate candy with him, which he could eat if a larger dose of insulin is administered than necessary at that time, and prevent the development of coma. But in daily menu The child should be limited in carbohydrates.
For children, short-acting insulins are used, most often Actrapid and Protophan. They are administered subcutaneously using a syringe pen. Such a syringe allows you to clearly determine the dose prescribed by the endocrinologist. Often children themselves can fill it and administer the drug.
It is mandatory to monitor blood sugar levels daily using a glucometer. His readings, as well as the foods eaten, are recorded in a diary, which helps the doctor choose the correct insulin dose.
For type 1 diabetes, pancreas transplantation is also possible as one of the treatment methods.
In the treatment of type 2 diabetes great importance It has . An endocrinologist will dwell in detail on the child’s nutrition depending on age. The principle of the diet is that it is necessary to completely eliminate the child’s consumption of easily digestible carbohydrates (chocolate, sugar, flour products) and significantly limit other carbohydrates in the diet. These recommendations must be followed in order to prevent a sharp increase in blood glucose.
To cope with this task, it is necessary to calculate the so-called “bread units”. A bread unit is the amount of a product containing 12 g of carbohydrates, which increases blood glucose levels by 2.2 mmol/l.
In European countries, nowadays every product has an indication of the grain units in it. This helps diabetic patients choose foods for their diet. In Russia there is no such information, but parents can calculate bread units on their own.
To do this, you need to divide the amount of carbohydrates in 100 g of product (this information is on each product) by 12. The resulting number of bread units should be recalculated by the weight of the product that will be consumed by the child.
Consequences (complications) of diabetes
Diabetes can lead to damage to the blood vessels of many organs with the development of irreversible consequences:
- damage to the retinal vessels will result in a decrease (or even complete loss) of vision;
- renal failure may occur as a result of damage to the renal vessels;
- encephalopathy develops due to damage to the blood vessels of the brain.
To avoid such severe complications it is necessary to ensure regular monitoring of blood sugar levels, careful and constant adherence to the diet (table No. 9), and strictly follow all the recommendations of the endocrinologist for the treatment of the disease.
Prevention
Prevention of diabetes in children should be carried out from birth. Here are a few provisions.
– a chronic metabolic disease characterized by impaired insulin secretion and the development of hyperglycemia. Diabetes mellitus in children usually develops rapidly; is accompanied by rapid weight loss in the child with increased appetite, uncontrollable thirst and excessive urination. In order to identify diabetes mellitus in children, a detailed examination is carried out laboratory diagnostics(determination of sugar, glucose tolerance, glycated hemoglobin, insulin, C-peptide, Ab to pancreatic β-cells in the blood, glycosuria, etc.). The main directions in the treatment of diabetes mellitus in children include diet and insulin therapy.

General information
Diabetes mellitus in children is a disorder of carbohydrate and other types of metabolism, which is based on insulin deficiency and/or insulin resistance, leading to chronic hyperglycemia. According to WHO, every 500th child and every 200th adolescent suffers from diabetes. Moreover, in the coming years, the incidence of diabetes mellitus among children and adolescents is predicted to increase by 70%. Considering the wide distribution, the tendency towards “rejuvenation” of the pathology, the progressive course and severity of complications, the problem of diabetes mellitus in children requires an interdisciplinary approach with the participation of specialists in the field of pediatrics, pediatric endocrinology, cardiology, neurology, ophthalmology, etc.

Classification of diabetes mellitus in children
In pediatric patients, diabetes doctors in most cases have to deal with type 1 diabetes mellitus (insulin-dependent), which is based on absolute insulin deficiency. Type 1 diabetes mellitus in children is usually autoimmune in nature; it is characterized by the presence of autoantibodies, destruction of β-cells, association with the genes of the major histocompatibility complex HLA, complete insulin dependence, a tendency to ketoacidosis, etc. Idiopathic diabetes mellitus type 1 has an unknown pathogenesis and is more often recorded in people of non-European race.
In addition to the dominant type 1 diabetes mellitus, rarer forms of the disease also occur in children: type 2 diabetes mellitus; diabetes mellitus associated with genetic syndromes; diabetes mellitus MODY type.
Causes of diabetes in children
The leading factor determining the development of type 1 diabetes mellitus in children is a hereditary predisposition, as evidenced by the high frequency of familial cases of the disease and the presence of pathology in close relatives (parents, siblings, grandparents).
However, to initiate the autoimmune process, exposure to a provoking factor is necessary. external environment. The most likely triggers leading to chronic lymphocytic insulitis, subsequent destruction of β-cells and insulin deficiency are viral agents (Coxsackie B, ECHO, Epstein-Barr, mumps, rubella, herpes, measles, rotavirus, enterovirus, cytomegalovirus, etc.) viruses. .
In addition, the development of diabetes mellitus in children with a genetic predisposition can be facilitated by toxic effects, nutritional factors (artificial or mixed feeding, cow's milk feeding, monotonous carbohydrate foods, etc.), stressful situations, surgical interventions.
The risk group for the development of diabetes mellitus includes children with a birth weight of over 4.5 kg, those who are obese, who lead an inactive lifestyle, who suffer from diathesis, and who are often ill.
Secondary (symptomatic) forms of diabetes mellitus in children can develop with endocrinopathies (Itsenko-Cushing syndrome, diffuse toxic goiter, acromegaly, pheochromocytoma), diseases of the pancreas (pancreatitis, etc.). Type 1 diabetes mellitus in children is often accompanied by other immunopathological processes: systemic lupus erythematosus, scleroderma, rheumatoid arthritis, periarteritis nodosa, etc.
Diabetes mellitus in children can be associated with various genetic syndromes: Down syndrome, Klinefelter syndrome, Prader-Willi syndrome, Lawrence-Moon-Bardet-Biedl syndrome, Wolfram syndrome, Huntington's chorea, Friedreich's ataxia, porphyria, etc.
Symptoms of diabetes in children
Manifestations of diabetes mellitus in a child can develop at any age. There are two peaks of manifestation of diabetes mellitus in children - at 5-8 years and in puberty, i.e. during periods increased growth and intensive metabolism.
In most cases, the development of insulin-dependent diabetes mellitus in children is preceded by a viral infection: mumps, measles, ARVI, enterovirus infection, rotavirus infection, viral hepatitis, etc. Type 1 diabetes mellitus in children is characterized by an acute, rapid onset, often with the rapid development of ketoacidosis and diabetic coma. From the moment of the first symptoms to the development of a coma, it can take from 1 to 2-3 months.
Diabetes mellitus in children can be suspected based on pathognomonic signs: increased urination (polyuria), thirst (polydipsia), increased appetite (polyphagia), and weight loss.
The mechanism of polyuria is associated with osmotic diuresis, which occurs with hyperglycemia ≥9 mmol/L, exceeding the renal threshold, and the appearance of glucose in the urine. Urine becomes colorless, it specific gravity increases due to high sugar content. Daytime polyuria may go unrecognized. More noticeable is nocturnal polyuria, which in diabetes mellitus in children is often accompanied by urinary incontinence. Sometimes parents pay attention to the fact that urine becomes sticky, and so-called “starch” stains remain on the child’s underwear.
Polydipsia is a consequence increased secretion urine and dehydration of the body. Thirst and dry mouth can also plague your child at night, causing him to wake up and ask for something to drink.
Children with diabetes experience a constant feeling of hunger, but along with polyphagia, they experience a decrease in body weight. This is due to energy starvation of cells caused by the loss of glucose in the urine, impaired glucose utilization, and increased processes of proteolysis and lipolysis under conditions of insulin deficiency.
Already at the onset of diabetes mellitus, children may experience dry skin and mucous membranes, the appearance of dry seborrhea on the scalp, flaking of the skin on the palms and soles, seizures in the corners of the mouth, candidal stomatitis, etc. Pustular skin lesions, furunculosis, mycoses, diaper rash, etc. are typical. vulvitis in girls and balanoposthitis in boys. If the debut of diabetes mellitus in a girl occurs during puberty, this can lead to menstrual irregularities.
With decompensated diabetes mellitus, children develop cardiovascular disorders(tachycardia, functional murmurs), hepatomegaly.
Complications of diabetes mellitus in children
The course of diabetes mellitus in children is extremely labile and is characterized by a tendency to develop dangerous conditions hypoglycemia, ketoacidosis and ketoacidotic coma.
Hypoglycemia develops as a result of a sharp decrease in blood sugar caused by stress, excessive physical activity, insulin overdose, poor diet, etc. Hypoglycemic coma is usually preceded by lethargy, weakness, sweating, headache, feeling severe hunger, trembling in the limbs. If measures are not taken to increase blood sugar, the child develops convulsions, agitation, followed by depression of consciousness. In hypoglycemic coma, body temperature and blood pressure are normal, there is no smell of acetone from the mouth, the skin is moist, the blood glucose level
Diagnosis of diabetes mellitus in children
In identifying diabetes, an important role belongs to the local pediatrician, who regularly monitors the child. At the first stage, the presence of classic symptoms of the disease (polyuria, polydipsia, polyphagia, weight loss) and objective signs should be taken into account. When examining children, attention is drawn to the presence of diabetic blush on the cheeks, forehead and chin, a crimson tongue, and decreased skin turgor. Children with characteristic manifestations of diabetes mellitus should be referred for further management to a pediatric endocrinologist.
The final diagnosis is preceded by a thorough laboratory examination of the child. Basic tests for diabetes mellitus in children include determination of blood sugar levels (including through daily monitoring), insulin, C-peptide, proinsulin, glycosylated hemoglobin, glucose tolerance, blood CBS; in urine - glucose and ketone bodies. The most important diagnostic criteria for diabetes mellitus in children are hyperglycemia (above 5.5 mmol/l), glucosuria, ketonuria, acetonuria. For the purpose of preclinical detection of type 1 diabetes mellitus in groups with high genetic risk or for the differential diagnosis of type 1 and type 2 diabetes, determination of Abs to pancreatic β-cells and Abs to glutamate decarboxylase (GAD) is indicated. An ultrasound examination is performed to assess the structural condition of the pancreas.
Differential diagnosis of diabetes mellitus in children is carried out with acetone syndrome, diabetes insipidus, nephrogenic diabetes. Ketoacidosis and who needs to be distinguished from acute abdomen (appendicitis, peritonitis, intestinal obstruction), meningitis, encephalitis,.
Treatment of diabetes mellitus in children
The main components of treatment for type 1 diabetes mellitus in children are insulin therapy, diet, proper lifestyle and self-control. Dietary measures include excluding sugars from the diet, limiting carbohydrates and animal fats, split meals 5-6 times a day, taking into account individual energy needs. An important aspect of the treatment of diabetes mellitus in children is competent self-control: awareness of the seriousness of one’s disease, the ability to determine the level of glucose in the blood, and adjust the dose of insulin taking into account the level of glycemia, physical activity, and dietary errors. Self-control techniques are taught to parents and children with diabetes in “diabetes schools.”
Replacement therapy for children suffering from diabetes mellitus is carried out with drugs of human genetically engineered insulin and their analogues. The dose of insulin is selected individually, taking into account the degree of hyperglycemia and the age of the child. Basis-bolus insulin therapy has proven itself well in pediatric practice, providing for the administration of long-acting insulin in the morning and evening to correct baseline hyperglycemia and the additional use of short-acting insulin before each main meal to correct postprandial hyperglycemia.
A modern method of insulin therapy for diabetes mellitus in children is an insulin pump, which allows insulin to be administered in a continuous mode (imitation of basal secretion) and bolus mode (imitation of post-alimentary secretion).
The most important components of the treatment of type 2 diabetes mellitus in children are diet therapy, sufficient physical activity, and the use of oral hypoglycemic drugs.
With the development of diabetic ketoacidosis, infusion rehydration, administration of an additional dose of insulin taking into account the level of hyperglycemia, and correction of acidosis are necessary. If a hypoglycemic state develops, it is necessary to urgently give the child sugar-containing products (a lump of sugar, juice, sweet tea, caramel); if the child is unconscious, it is necessary intravenous administration glucose or intramuscular injection glucagon.
Forecast and prevention of diabetes mellitus in children
The quality of life of children with diabetes mellitus is largely determined by the effectiveness of disease compensation. If you follow the recommended diet, regimen, and therapeutic measures, life expectancy corresponds to the average in the population. In case of gross violations of doctor's instructions, or decompensation of diabetes, specific diabetic complications develop early. Patients with diabetes mellitus are monitored for life by an endocrinologist-diabetologist.
Vaccination of children with diabetes mellitus is carried out during the period of clinical and metabolic compensation; in this case, it does not cause deterioration in the course of the underlying disease.
Specific prevention of diabetes mellitus in children has not been developed. It is possible to predict the risk of the disease and identify prediabetes based on an immunological examination. In children at risk for developing diabetes, it is important to maintain optimal weight, daily physical activity, increase immunoresistance, and treat concomitant pathologies.
Dr. Komarovsky argues that diabetes in children is most often insulin-dependent, in which the pancreas stops producing the hormone that converts glucose into energy. This is a chronic autoimmune progressive disease during which the beta cells of the islets of Langerhans are destroyed. It is worth noting that during the period of primary symptoms, most of these cells have already undergone destruction.
Often type 1 diabetes is caused by hereditary factors. So, if someone close to the child had chronic hyperglycemia, then the probability that the disease will be detected in him or her is 5%. And the risk of developing the disease in 3 identical twins is about 40%.
Sometimes, in adolescence, a second type of diabetes, also called insulin-dependent, can develop. Komarovsky notes that with this form of the disease, ketoacidosis appears only due to severe stress.
Also, a large proportion of people with acquired diabetes are overweight, which often causes insulin resistance, which can contribute to impaired glucose tolerance. In addition, the secondary form of the disease can develop due to a malfunction of the pancreas or an excess of glucocorticoids.
Signs of diabetes in children
Talking about the symptoms of chronic hyperglycemia in a child, Komarovsky focuses the attention of parents on the fact that the disease manifests itself very quickly. This can often lead to the development of disability, which is explained by the peculiarities of child physiology. These include instability nervous system, increased metabolism, strong physical activity, underdevelopment of the enzymatic system, due to which it cannot fully fight ketones, which causes the appearance of diabetic coma.
However, as mentioned above, a child sometimes develops type 2 diabetes. Although this violation is not common, because most parents try to monitor the health of their children.
The symptoms of type 1 and type 2 diabetes are similar. The first manifestation is the consumption of copious amounts of fluid. This is explained by the fact that water passes from the cells into the blood to dilute the sugar. Therefore, a child drinks up to 5 liters of water per day.
Also, one of the leading signs of chronic hyperglycemia is polyuria. Moreover, in children, urination often occurs during sleep, because the day before they drank a lot of liquid. In addition, mothers often write on forums that if their child’s underwear dries out before washing, it becomes as if starched to the touch.
Many more diabetics lose weight. This is explained by the fact that when there is a deficiency of glucose, the body begins to break down muscle and fat tissue.
If there is diabetes, the symptoms in children, Komarovsky claims, can manifest themselves as vision problems. After all, dehydration of the body is reflected in the eye lens.
As a result, a veil appears before the eyes. However, this phenomenon is no longer considered a sign, but a complication of diabetes, which requires immediate examination by an ophthalmologist.
In addition, a change in the child’s behavior may indicate endocrine disorders. This is explained by the fact that the cells do not receive additional glucose, which causes energy hunger and the patient becomes inactive and irritable.
Ketoacidosis in children
Sugar level
Another characteristic sign of diabetes is refusal to eat or, conversely, constant hunger. This also occurs against the background of energy starvation.
In diabetic ketoacidosis, appetite disappears. This manifestation is quite dangerous, which requires immediately calling an ambulance and subsequent hospitalization of the patient, because this is the only way to prevent the development of disability and other serious consequences.
In type 2 diabetes, a typical manifestation is often frequent fungal infections. And with an insulin-dependent form of the disease, it is even difficult for a child’s body to fight ordinary acute respiratory viral infections.
Diabetics may smell acetone on their breath, and ketone bodies are sometimes found in the urine. These symptoms, in addition to diabetes, may accompany others serious illnesses, for example, rotavirus infection.
If the child only smells acetone from the mouth, and there are no other signs of diabetes, then Komarovsky explains this by glucose deficiency. This condition occurs not only against the background of endocrine disorders, but also after active physical activity.
This problem can be solved simply: the patient needs to be given a glucose tablet or offered to drink sweet tea or eat candy. However, you can get rid of the acetone smell in diabetes only with the help and adherence to a diet.
Moreover, the clinical picture of the disease is confirmed by laboratory tests:
- increased blood glucose levels;
- the presence in the blood of antibodies that destroy the pancreas;
- Occasionally, immunoglobulins to insulin or enzymes involved in the production of the hormone are detected.
The children's doctor notes that antibodies are found only in insulin-dependent diabetes, which is considered autoimmune disease. And the second type of disease manifests itself increased level Blood pressure, high cholesterol levels in the blood and the appearance of dark spots in the armpits and between the fingers.
Hyperglycemia in the insulin-dependent form of the disease is also accompanied by pallor skin, tremors of the limbs, dizziness and malaise. Sometimes diabetes develops covertly, which is dangerous due to late detection of the disease and the development of irreversible consequences.
Occasionally, diabetes appears in the first year of life, which significantly complicates diagnosis, because the child cannot explain what symptoms are bothering him. In addition, it is quite difficult to determine the daily volume of urine from diapers.
Therefore, parents of newborns should pay attention to a number of manifestations such as:
- anxiety;
- dehydration;
- increased appetite, due to which weight is not gained, but rather lost;
- vomit;
- the appearance of diaper rash on the surface of the genital organs;
- the formation of sticky spots on surfaces where urine has entered.
Komarovsky draws the attention of parents to the fact that earlier child If you get diabetes, the more difficult the disease will be in the future.
Therefore, if there is hereditary factor It is important to control glycemic levels from birth, carefully monitoring the behavior of children.
How to reduce the likelihood of developing diabetes and what to do if the diagnosis is confirmed?
 Of course, it is impossible to cope with a hereditary predisposition, but it is possible to make the life of a child with diabetes easier. Thus, for preventive purposes, infants who are in the risk category should especially carefully select complementary foods and use adapted formulas if breastfeeding is impossible.
Of course, it is impossible to cope with a hereditary predisposition, but it is possible to make the life of a child with diabetes easier. Thus, for preventive purposes, infants who are in the risk category should especially carefully select complementary foods and use adapted formulas if breastfeeding is impossible.
At an older age, the child needs to be accustomed to an active life with moderate activity. No less important in preventive and medicinal purposes teach children to adhere to a special diet.
The general principles of proper nutrition are that the ratio of nutrients and calories in a child’s menu should be such that he can compensate for energy costs and grow and develop normally. So, 50% of the diet should be carbohydrates, 30% should be fats, and 20% should be proteins. If a diabetic is obese, then the goal of diet therapy is to slowly lose weight and then maintain weight at the same level.
In the insulin-dependent form, it is important to coordinate meals with the administration of insulin. Therefore, it is necessary to eat in same time, and you should always maintain the ratio of proteins, carbohydrates and fats.
Since insulin flows from the injection site, in the absence of additional snacks between the main meal, the patient may develop pain, which will intensify with physical activity. Therefore, children who receive 2 injections per day must have a snack between breakfast, lunch and dinner.
The child’s menu includes 6 main types of products that can be replaced with each other:
- meat;
- milk;
- bread;
- vegetables;
- fruits;
- fats.
It is noteworthy that diabetics often develop atherosclerosis. Therefore, the daily dose of fat for such a disease should be no more than 30%, and cholesterol - up to 300 mg.
Preference should be given to polyunsaturated fatty acids. For meat, it is better to choose fish, turkey, chicken, and the consumption of pork and beef should be limited. Dr. Komarovsky himself in the video in this article will talk about diabetes and sugar in children.