MRI of the pelvis in men is prescribed to identify pathologies of organs in this area and is intended to confirm the diagnosis made based on the patient’s symptoms or based on the results of other examinations, and also helps in the prevention of diseases.
What does an MRI of the pelvis show in men?
Examination of the pelvis is quite difficult. This method allows you to examine the pelvic organs without harm to the body. The pelvic cavity in men includes sigmoid colon, bladder, prostate gland, pubic bones. MRI in the study of this area is mostly used in the diagnosis of cancer. Possibilities ultrasound examination and are limited and require additional study of organs. MRI allows you to find the source of the disease. Acute, chronic inflammatory diseases, vascular pathology, tumors that need immediate attention surgical intervention, are detected and diagnosed very accurately.
Since, during the study, sections one millimeter thick are obtained. Due to a thorough examination with an MRI scanner, the detection of a tumor can be recognized at the very beginning of its development.
Symptoms for prescribing magnetic resonance imaging:
- swelling or swelling of the testicles or scrotum
- ectopia of the testicle (if it is not possible to detect the testicle using ultrasound)
- pain in the abdomen and pelvic area, the causes of which are unknown
- difficulty urinating, urinary retention
MRI of the pelvic organs in men is also prescribed for the following indications:
- identifying pathologies as a result
- availability birth defects hip development
- injury or wound to this area
- sensations of pain in the hip area for unknown reasons.
In the diagnosis of diseases prostate gland MRI is also indispensable. As with all other human organs, tomography is typically used to detect prostate cancer. In addition, MRI is used to diagnose other diseases of the prostate gland and seminal vesicles.
Tomography is carried out using powerful magnets and small sensors. This involves taking several pictures of the area being studied. No X-rays are used during the procedure. That is, the study does not in any way affect human health.
Tomography with contrast is usually ordered to confirm the presence oncological diseases prostate gland, urinary tract and other organs of this cavity.
Preparing for the examination
 Preparation for the study is not particularly different from other types of MRI. To complete the study you are required to follow a diet. Three days before the examination, exclude gas-forming foods (vegetables, fruits, sweets, spicy seasonings, carbonated drinks). You should not eat food four hours before the procedure.
Preparation for the study is not particularly different from other types of MRI. To complete the study you are required to follow a diet. Three days before the examination, exclude gas-forming foods (vegetables, fruits, sweets, spicy seasonings, carbonated drinks). You should not eat food four hours before the procedure.
It is often recommended to take the No-Spa or Espumisan tablet. When examining the prostate gland, an enema is given before the procedure. the obstacle is allergic reaction for specific drugs.
are similar when performing procedures on other internal organs. This is the presence in the body of pacemakers, insulin pumps, metal braces or implants other than titanium. Metal dentures can also interfere with the examination. Contraindications will also be renal failure and claustrophobia.
Systemic lupus erythematosus (SLE) is a chronic autoimmune rheumatic disease. The diagnosis of SLE can only be made by a specialist with sufficient experience. Difficulties in diagnosing the disease are associated with a varied clinical picture, when throughout the course of the disease new signs of the disease appear, reflecting damage various organs and systems.
When diagnosing SLE, MEDSI specialists are based on a combination of clinical manifestations of the disease and data laboratory diagnostics, in addition, blood tests, urine tests, ultrasound, X-ray examination make it possible to accurately determine the nature and extent of damage to internal organs and the phases of disease activity.
In the Clinic of Innovative Rheumatology of the Clinical Diagnostic Center MEDSI on Belorusskaya, diagnostics are carried out using modern laboratory and instrumental methods research - determination of autoantibodies, complement, rheumatoid factor titer, biochemical analysis blood, MRI, MSCT, ultrasound, radiography, functional tests are performed. Treatment of the disease is carried out according to international standards and recommendations of rheumatological associations of Europe and the USA together with specialists from the Center for Diagnostics and Innovation medical technologies MEDSI and the only one in Russia that uses the world's best innovative methods of diagnosis and treatment. Specialists of the EML Department developed their own high-tech method treatment of lupus erythematosus - immunosorption, which has no analogues in the world.
At the Clinical Diagnostic Center on Belorusskaya, a famous Doctor of Medical Sciences, Honored Doctor is receiving treatment. Russian Federation. Sergei Konstantinovich - creator of the national school intensive care rheumatic diseases, expert in the diagnosis and treatment of systemic lupus erythematosus, severe forms rheumatoid arthritis, systemic vasculitis and other connective tissue diseases.
Methods for the treatment of autoimmune rheumatic diseases developed by the Professor using methods of extracorporeal therapy and genetic engineering biological drugs provide not only maximum survival, but also high level quality of life, the ability to minimize intake hormonal drugs or even their complete abolition. Early recognition of the disease, timely and personalized therapy, professional monitoring are the main principles that guide Sergei Konstantinovich in his daily practice.
Systemic lupus erythematosus– chronic systemic disease, with the most pronounced manifestations on the skin; The etiology of lupus erythematosus is unknown, but its pathogenesis is associated with a violation of autoimmune processes, as a result of which antibodies are produced to healthy cells of the body. Middle-aged women are more susceptible to the disease. The incidence of lupus erythematosus is not high - 2-3 cases per thousand people. Treatment and diagnosis of systemic lupus erythematosus is carried out jointly by a rheumatologist and a dermatologist. The diagnosis of SLE is made based on typical clinical signs, laboratory test results.
General information
Systemic lupus erythematosus– a chronic systemic disease, with the most pronounced manifestations on the skin; The etiology of lupus erythematosus is unknown, but its pathogenesis is associated with a violation of autoimmune processes, as a result of which antibodies are produced to healthy cells of the body. Middle-aged women are more susceptible to the disease. The incidence of lupus erythematosus is not high - 2-3 cases per thousand people.
Development and suspected causes of systemic lupus erythematosus
The exact etiology of lupus erythematosus has not been established, but most patients have antibodies to the Epstein-Barr virus, which confirms the possible viral nature of the disease. Features of the body that result in the production of autoantibodies are also observed in almost all patients.
The hormonal nature of lupus erythematosus has not been confirmed, but hormonal disorders worsen the course of the disease, although they cannot provoke its occurrence. Women diagnosed with lupus erythematosus are not recommended to take oral contraceptives. In people who have genetic predisposition and identical twins have a higher incidence of lupus erythematosus than other groups.
The pathogenesis of systemic lupus erythematosus is based on a violation of immunoregulation, when protein components of the cell, primarily DNA, act as autoantigens and, as a result of adhesion, even those cells that were initially free from immune complexes become targets.
Clinical picture of systemic lupus erythematosus
 Lupus erythematosus affects connective tissue, skin and epithelium. Important diagnostic sign is a symmetrical lesion of large joints, and if joint deformation occurs, it is due to the involvement of ligaments and tendons, and not due to lesions of an erosive nature. Myalgia, pleurisy, pneumonitis are observed.
Lupus erythematosus affects connective tissue, skin and epithelium. Important diagnostic sign is a symmetrical lesion of large joints, and if joint deformation occurs, it is due to the involvement of ligaments and tendons, and not due to lesions of an erosive nature. Myalgia, pleurisy, pneumonitis are observed.
But most clear symptoms lupus erythematosus is noted on the skin and it is based on these manifestations that the diagnosis is made in the first place.
On initial stages The disease lupus erythematosus is characterized by continuous flow with periodic remissions, but almost always becomes systemic. Erythematous dermatitis of the butterfly type is most often observed on the face - erythema on the cheeks, cheekbones and always on the dorsum of the nose.  Hypersensitivity to solar radiation appears - photodermatoses are usually round in shape and multiple in nature. In lupus erythematosus, a feature of photodermatoses is the presence of a hyperemic corolla, an area of atrophy in the center and depigmentation of the affected area. The pityriasis scales that cover the surface of the erythema are tightly fused to the skin and attempts to separate them are very painful. At the stage of atrophy of the affected skin the formation of a smooth, delicate alabaster-white surface is observed, which gradually replaces the erythematous areas, starting from the middle and moving to the periphery.
Hypersensitivity to solar radiation appears - photodermatoses are usually round in shape and multiple in nature. In lupus erythematosus, a feature of photodermatoses is the presence of a hyperemic corolla, an area of atrophy in the center and depigmentation of the affected area. The pityriasis scales that cover the surface of the erythema are tightly fused to the skin and attempts to separate them are very painful. At the stage of atrophy of the affected skin the formation of a smooth, delicate alabaster-white surface is observed, which gradually replaces the erythematous areas, starting from the middle and moving to the periphery.
In some patients with lupus erythematosus, the lesions extend to scalp scalp, causing complete or partial alopecia. If the lesions affect the red border of the lips and the mucous membrane of the mouth, then the lesions are bluish-red dense plaques, sometimes with pityriasis-like scales on top, their contours have clear boundaries, the plaques are prone to ulceration and cause pain while eating.
Lupus erythematosus has a seasonal course, and in the autumn-summer periods the skin condition worsens sharply due to more intense exposure to solar radiation.
 When under acute course lupus erythematosus, psoriasis-like lesions are observed throughout the body, telangiectasia is pronounced on the skin lower limbs a reticular livedio (tree-like pattern) appears. Generalized or focal alopecia, urticaria and itchy skin observed in all patients with systemic lupus erythematosus.
When under acute course lupus erythematosus, psoriasis-like lesions are observed throughout the body, telangiectasia is pronounced on the skin lower limbs a reticular livedio (tree-like pattern) appears. Generalized or focal alopecia, urticaria and itchy skin observed in all patients with systemic lupus erythematosus.
In all organs where there is connective tissue, over time they begin pathological changes. With lupus erythematosus, all membranes of the heart, renal pelvis, gastrointestinal tract and the central nervous system.
If, in addition to skin manifestations, patients suffer from periodic headaches, joint pains unrelated to injuries and weather conditions, and disturbances in the functioning of the heart and kidneys are observed, then based on the survey, we can assume deeper and systemic disorders and examine the patient for the presence of lupus erythematosus. A sharp change in mood from a euphoric state to a state of aggression is also a characteristic manifestation of lupus erythematosus.
In elderly patients with lupus erythematosus, skin manifestations, renal and arthralgic syndromes are less pronounced, but Sjogren's syndrome is more often observed - this is an autoimmune lesion connective tissue manifested by hyposecretion salivary glands, dryness and pain in the eyes, photophobia.
Children with the neonatal form of lupus erythematosus, born from sick mothers, have an erythematous rash and anemia already in infancy, so they should be differential diagnosis with atopic dermatitis.
Diagnosis of systemic lupus erythematosus
If systemic lupus erythematosus is suspected, the patient is referred for consultation with a rheumatologist and dermatologist. Lupus erythematosus is diagnosed by the presence of manifestations in each symptomatic group. Criteria for diagnosis from the skin: butterfly erythema, photodermatitis, discoid rash; from the joints: symmetrical damage to the joints, arthralgia, “pearl bracelet” syndrome on the wrists due to deformation of the ligamentous apparatus; from the internal organs: various localizations serositis, persistent proteinuria and cylindruria in urine analysis; from the central nervous system: convulsions, chorea, psychoses and mood swings; In terms of hematopoietic function, lupus erythematosus is manifested by leukopenia, thrombocytopenia, and lymphopenia.
The Wasserman reaction can be false-positive, like other serological tests, which sometimes leads to the prescription of inadequate treatment. If pneumonia develops, an X-ray of the lungs is performed; if pleurisy is suspected,
Patients with lupus erythematosus should avoid direct sun rays, wear clothing that covers the entire body, and apply creams with a high UV protective filter to exposed areas. Corticosteroid ointments are applied to the affected areas of the skin, since the use of non-hormonal drugs has no effect. Treatment must be carried out intermittently so that hormone-related dermatitis does not develop.
In uncomplicated forms of lupus erythematosus to eliminate pain in muscles and joints, non-steroidal anti-inflammatory drugs are prescribed, but aspirin should be taken with caution, as it slows down the blood clotting process. It is mandatory to take glucocorticosteroids, and the doses of the drugs are selected in such a way that while minimizing side effects protect internal organs from defeats.
A method when stem cells are collected from a patient, and then immunosuppressive therapy is carried out, after which for recovery immune system stem cells are reintroduced, effective even in severe and hopeless forms of lupus erythematosus. With this therapy, autoimmune aggression in most cases stops, and the condition of the patient with lupus erythematosus improves.
Healthy lifestyle, giving up alcohol and smoking, adequate exercise stress, balanced diet and psychological comfort allow patients with lupus erythematosus to control their condition and prevent disability.
(systemic lupus erythematosus) is a systemic connective tissue disease that develops on the basis of a genetically determined imperfection of immunoregulatory processes, leading to the formation of antibodies to one’s own cells and their components and the occurrence of immune complex inflammation, which results in damage to many organs and systems.
The etiology of the disease is unknown.
Suggested etiological role the following factors: 1. Chronic viral infection 2. Genetic factor.
Clinic (symptoms) of systemic lupus erythematosus
Mostly women are affected, most often aged 14-40 years.
Initial manifestations. Weakness, weight loss, increased body temperature.
General symptoms: fatigue, weakness, fever, lack of appetite, weight loss, nausea
Symptoms from the musculoskeletal system: arthralgia, myalgia; nonerosive polyarthritis; deformation of the joints of the hands; myopathy, myositis; aseptic bone necrosis.
Skin manifestations: “butterfly”; discoid lupus; photosensitivity; sores in the mouth; skin rashes- maculopapular, urticarial, bullous, subacute cutaneous lupus; alopecia; vasculitis; panniculitis.
Rice
Hematological manifestations: anemia (secondary); hemolytic anemia; leukopenia (less than 4x10 5
l); lymphopenia (less than 1.5x10 9
l); thrombocytopenia (less than 100x10 9
l); circulating anticoagulant; splenomegaly; lymphadenopathy.
Neurological manifestations: organic brain damage syndrome; psychoses; seizures; peripheral neuropathy; other manifestations of the central nervous system.
Cardiac manifestations: pericarditis; myocarditis; Libman-Sachs endocarditis.
Clinical classification
| Nature of the disease |
Acute, subacute, chronic Recurrent polyarthritis Discoid lupus syndrome Raynaud's syndrome Werlhoff's syndrome Sjögren's syndrome Antiphospholipid syndrome |
|
|
Activity level |
Missing (0) |
|
|
process |
Minimum (I) Moderate (II) High (III) |
|
|
Moth symptom |
||
|
Capillarites |
||
|
Discoid lupus |
||
|
Reticular livedo, etc. |
||
|
joints |
Arthralgia |
|
|
Polyarthritis (acute, subacute, chronic) |
||
|
serous |
Pleurisy, pericarditis (effusion, dry, |
|
|
shells |
adhesive), perihepatitis, perisplenitis, by |
|
|
lyserositis |
||
|
Myocarditis, endocarditis, failure |
||
|
mitral valve, myocardiofibrosis, |
||
|
myocardial dystrophy |
||
|
Acute, chronic pneumonitis |
||
|
Pneumosclerosis |
||
|
Lupus nephritis nephrotic or mixed |
||
|
pyelonephritic syndrome, |
||
|
urinary syndrome |
||
|
Meningoencephalopolyradiculoneuritis, according to |
||
|
lineuritis, strokes and cerebral infarction, cerebral vasculitis |
||
Pulmonary manifestations: pleurisy; effusion in pleural cavity; lupus pneumonia; interstitial fibrosis; pulmonary hypertension; hemorrhages.
Renal manifestations: proteinuria (more than 500 mg per day); shadows of red blood cells (and other cells); nephrotic syndrome; renal failure.
Gastrointestinal manifestations: nonspecific symptoms (loss of appetite, nausea, diarrhea, mild pain); vasculitis with gastrointestinal bleeding or perforation; ascites; increased activity of serum liver enzymes.
Thrombosis: venous; arterial.
Ocular pathology: retinal vasculitis; conjunctivitis, episcleritis; dry syndrome.
Clinical options. V.A. Nasonova identifies variants of the course of SLE (acute, subacute, chronic) according to the onset of the disease and further progression.
In the acute course, the onset of the disease is sudden, the body temperature is high, acute polyarthritis with severe pain in the joints, severe skin changes, severe polyserositis, damage to the kidneys, nervous system, trophic disorders, weight loss, sharp increase ESR, pancytopenia, a large number of LE cells in the blood, high titers antinuclear factor. The duration of the disease is 1-2 years.
Subacute course characterized by gradual development, articular syndrome, normal or low-grade fever body, skin changes. The activity of the process is minimal for a considerable time, remissions are long (up to six months). However, the process gradually generalizes, and multiple damage to organs and systems develops.
Chronic course manifests itself as mono- or low-syndromic syndrome for many years. General state remains satisfactory for a long time. In the early stages, skin changes and joint syndrome are observed. The process progresses slowly, and many organs and systems are subsequently affected.
Drug treatment of systemic lupus erythematosus
Glucocorticoids: high doses of prednisolone (1-1.5 mg/kg/day) until activity decreases, then maintenance doses; pulse therapy with methylprednisolone (1000 mg/day, once a day for 3 days) - with high activity of the process (active lupus nephritis, generalized vasculitis, other organ lesions), followed by high doses of prednisolone (1 mg/kg per day). Immunosuppressants (with high process activity, in combination with prednisone): cyclophosphamide (50-100 mg per day for 10 weeks, then maintenance doses - 25-50 mg/day); methotrexate 10-15 mg/week (4-6 weeks); azathioprine 50-200 mg/day for at least 10 weeks. Aminoquinolone drugs (with low process activity in combination with glucocorticoids): Delagil 0.5 g/day; Plaquenil 0.4 g/day.
NSAIDs (for bursitis, arthritis, polymyalgia): diclofenac sodium 150 mg/day; indomethacin 150 mg/day. Antiplatelet agents and anticoagulants: heparin 5000-10000 units 4 times a day (for vasculitis, disseminated intravascular coagulation syndrome); dipyridamole 75-210 mg per day; pentoxifylline 100-200 mg 3 times a day.
This article will be long, since there are practically no organs and organ systems that are not affected by systemic lupus erythematosus (SLE). Unfortunately... For ease of reading, I will describe lesions in lupus by organ system. SLE is characterized by multiple organ damage. Symptoms and clinical manifestations vary greatly among different patients. The course of the disease is usually undulating with alternating exacerbations and remissions.
General symptoms
- weakness,
- increase in body temperature,
- weight loss,
- increased weakness, fatigue, drowsiness.
Damage to skin, hair and nails
 Skin lesions are observed in a significant proportion of patients - 50-90%. In about a third of patients, lupus debuts with skin lesions; in the rest, certain skin manifestations occur later, as the disease progresses. The main types of skin lesions are presented below:
Skin lesions are observed in a significant proportion of patients - 50-90%. In about a third of patients, lupus debuts with skin lesions; in the rest, certain skin manifestations occur later, as the disease progresses. The main types of skin lesions are presented below:

Damage to mucous membranes
 Data on the prevalence of mucosal lesions range from 10 to 40% according to various sources. Most often the mucous membranes of the nose and mouth are affected, much less often the conjunctiva and mucous membranes of the genital organs. Long-term damage to the nasal mucosa can even lead to perforation of the nasal septum.
Data on the prevalence of mucosal lesions range from 10 to 40% according to various sources. Most often the mucous membranes of the nose and mouth are affected, much less often the conjunctiva and mucous membranes of the genital organs. Long-term damage to the nasal mucosa can even lead to perforation of the nasal septum.
- Aphthous stomatitis- sores.
- Lupus cheilitis- damage, swelling, redness of the red border of the lips with the development of ulceration and erosion (see photo).
Damage to the musculoskeletalapparatus
Joint damage in one form or another occurs in the vast majority of patients - 90%. In addition, in approximately half of patients the disease may begin with joint damage. Most often affected small joints hands, wrists, elbows, knee joints. Arthritis is often symmetrical in nature and can even be “masked” as.
- However, pain and stiffness are more common than serious destructive joint damage. Morning stiffness is usually short-lived, and joint deformity is relatively rare.
- In some patients it can be observed defeat skeletal muscles , which manifests itself in the form of pain and weakness of muscles up to their atrophy, discomfort upon palpation of the affected muscles.
- Often there are so-called aseptic necrosis bones, which are most often observed in the heads of the hip bones.
- Of course, systemic lupus erythematosus is associated with an increased likelihood of developing . The incidence of spontaneous fractures in such patients is approximately 5 times higher than in the general population.
Respiratory system damage
IN pathological process In SLE, almost all parts of the respiratory system can be involved.
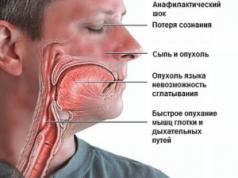
- Larynx is affected relatively infrequently, in no more than 5% of cases. Most often, clinically this is manifested by inflammation of the mucous membrane of the larynx, swelling of the larynx.
- Pleurisy develop in approximately 50% of cases. Often accompanied by pain in chest, shortness of breath, cough, fever.
- Increased pressure in pulmonary artery(pulmonary hypertension) most often develops only several years after the onset of the disease.
- Acute lupus pneumonitis (lupus pneumonitis) fortunately, it is rare, but it is very severe with fever, shortness of breath, cough, hemoptysis and severe pain in the chest.
Damage to the cardiovascular system
Clinically, these or those are much less common than they are detected at autopsy. However, it is already known that damage to the heart and blood vessels in lupus is one of the leading causes early mortality with this disease.
- Pericardial lesion observed in approximately 50-80% of patients. In some patients, we see only thickening of the pericardial layers on echocardioscopy (EchoCS), while in others there is effusion into the pericardial cavity, which sometimes leads to a rare but dangerous complication - pericardial tamponade. Usually the amount of effusion is small or moderate. Often pericarditis is combined with pleurisy (then it is called “polyserositis”).
- Heart valve damage. The “classic” lesion of the valvular apparatus in SLE is Libman-Sachs verrucous endocarditis. Most often affected mitral valve. Endocarditis is more often observed in young patients with a high degree of disease activity.
- Myocardial damage(heart muscle) manifests itself in the form of myocarditis, myocardial dystrophy, myocardial hypertrophy,
- Arterial hypertension is observed in 10-50% of patients.
Damage to the digestive system
- P infection of the oral mucosa, as I wrote above, occurs on average in a quarter of patients. Sometimes there are painful, extensive ulcers that make it difficult to fully swallow food. About a third of patients develop varying degrees severity of digestive disorders: anorexia, nausea, vomiting.
- Intestinal pathology often associated with damage to the serous membranes. A serious complication is damage to the vessels of the mesentery, which can lead to the development of intestinal infarction.
- Liver damage may occur in the form of a slight increase in its size, in some patients up to the development of severe hepatitis.
Kidney damage
 Kidney damage has varied and numerous manifestations.
Kidney damage has varied and numerous manifestations.
- In most patients, lupus nephritis (lupus nephritis) develops during the first years from the onset of the disease, and only in 5% of patients lupus begins with kidney damage. Active forms of lupus nephritis usually develop in young patients against a background of high disease activity. In middle-aged and elderly patients, nephritis occurs more “mildly”. The course of lupus nephritis is characterized by frequent exacerbations. Approximately 10-30% of patients with nephritis develop severe renal failure, which is the cause of their death. Unfavorable factors for the progression of kidney damage are: male gender, early onset of the disease and early development of nephritis.
- Nephritis against the background of SLE can also be complicated by various infectious diseases of the kidneys, for example, pyelonephritis.
- Toxic kidney damage due to therapy (NSAIDs, cyclophosphamide) has also been described.
Damage to the nervous system
Neurological symptoms in systemic lupus erythematosus are very, very diverse. It is so varied and diverse that it is quite difficult to somehow systematize all the symptoms encountered.
- Characteristic tin pains according to the type of migraines that do not stop or practically do not stop when taking conventional painkillers. Moreover, sometimes headaches and some other neurological signs occur long before the full picture of the disease and diagnosis.
- Transient ischemic attacks may appear epileptic seizures, speech impairment, swallowing, vomiting, dizziness.
- Strokes usually occur with parallel developing antiphospholipid syndrome.
- Syndrome pseudotumors brain is observed, as a rule, against the background of high activity and aggressive course of lupus. Manifests itself as persistent headache, nausea, vomiting, dizziness, and lethargy.
- Epileptic seizures, as a rule, accompany exacerbations of the disease.
- Defeat spinal cord develops quite rarely and can manifest itself as muscle weakness, numbness of the arms and legs, loss of sensitivity, paralysis, dysfunction pelvic organs(involuntary urination and defecation, impotence).
Mentalviolations quite common in patients with systemic lupus erythematosus. They can manifest themselves as hallucinations, disorientation, depression, and suicidal attempts.
Endocrine disorders. There is a more frequent development of diabetes, autoimmune thyroiditis, hyper- and hypothyroidism in these patients.
Classification of systemic lupus erythematosus
The classification is based on identifying variants of the course of the disease.
Acute course of the disease: There is a rapid development of damage to many organs, including the nervous system, kidneys, and heart.
Subacute course: the disease proceeds in waves, with alternating periods of remission and exacerbations, but usually after each exacerbation there is involvement of new organs and organ systems in the process.
Chronic course: characterized by rather slow damage to organs, most often a detailed picture of the disease with damage to many organs and organ systems is noted only after 5-10 years from the onset of the disease.
Special clinical options
- Onset of the disease in childhood and adolescence: characterized by an acute, sometimes even violent onset of the disease.
- SLE in the elderly has a more favorable prognosis and a mild course.
- SLE in men. It has already been mentioned that lupus is predominantly a “female” disease. Men get sick much less often, but they are obviously more severe and have a more unfavorable prognosis.
- Neonatal lupus syndrome (neonatal lupus) is associated with transmission of maternal autoantibodies. Includes damage to the skin, lungs, and heart. As a rule, all symptoms are temporary and disappear a few weeks after the natural removal of maternal immunoglobulins from the child’s body.