A B heart block is private option violations of contractility of the heart muscle. At its core, this is a weakening or complete cessation of the conduction of an electrical impulse through the atrioventricular node.
Treatment is not always required. In the early stages, recovery is not carried out at all; dynamic observation is indicated.
As it progresses, drug therapy is prescribed. The duration of the full development cycle of the deviation is approximately 3-10 years.
Symptoms appear much earlier than the terminal phase. They are quite pronounced. Therefore, there is time for diagnosis and treatment.
All activities are carried out under the supervision of a cardiologist and, as necessary, related specialists.
The division is carried out on three grounds.
Depending on the nature of the flow:
- Spicy. It is relatively rare and occurs as a result of severe external factors. Injuries, vomiting, sudden changes in body position, the course of somatic pathologies, all these are moments in the development of the process. Risks of cardiac arrest are greatest. Correction of the condition and stabilization of patients is carried out in inpatient conditions, under the supervision of a group of doctors.
- Chronic form. Diagnosed in every second case of the total number of AV blocks. It is a lightweight option. Manifestations are minimal, and the likelihood of death is also not high. Restoration is carried out as planned. Treatment is medicinal or surgical, depending on the stage.
According to the degree of impairment of the functional activity of fibers:
- Complete AV block. There is no conduction of the electrical impulse from the sinus node to the atrioventricular node at all. The result is cardiac arrest and death. This emergency, is eliminated in intensive care conditions.
- Partial blockade of the atrioventricular node. It occurs more easily and accounts for the majority of clinical cases. But we must remember that progression may be abrupt, but this is relatively rare.
It is possible to subdivide the process according to the duration of the flow:
- Constant blockade. As the name suggests, it does not go away on its own.
- Transient (transient). The duration of the episode is from a couple of hours to several weeks and even months.
- Paroxysmal or paroxysmal. Duration about 2-3 hours.
Four degrees of severity
Generally accepted clinical classification carried out according to the severity of the current. Accordingly, there are 4 stages in the development of the process.
1st degree (mild)
It occurs against the background of other cardiac and extracardiac pathologies. Manifestations of the subjective plan are minimal or completely absent. At the level diagnostic techniques There are minor deviations in the ECG picture.

Recovery is possible within 6-12 months, but is not always required. Dynamic observation is indicated, and, if necessary, the use of medications.
2nd degree (medium)
It is further divided into 2 types, depending on electrocardiographic data.
- AV block 2nd degree Mobitz 1 characterized by a gradual lengthening of the PQ interval. Symptoms are also uncharacteristic. Minimal manifestations occur that are practically unnoticeable if you do not overload the body. Provocative tests are quite informative, but can pose a danger to health and even life. Treatment is identical, with more emphasis on medication.
- AV block 2nd degree Mobitz 2 is determined by the loss of ventricular complexes, which indicates incomplete contraction of cardiac structures. Because the symptoms are much brighter, it’s difficult not to notice them.

3rd degree (severe)
It is determined by pronounced deviations in the functioning of a muscular organ. Changes on the ECG are easy to detect, the manifestations are intense - an arrhythmia occurs, such as a slowdown in contractions.
Such signs do not bode well. Against the background of complex organic defects, weakening of hemodynamics, tissue ischemia occurs, and multiple organ failure is possible in the initial phase.

4th degree (terminal)
Determined by complete blockade, heart rate 30-50. As a compensatory mechanism, the ventricles begin to contract at their own rhythm, separate areas of excitation arise.

All cameras work in their own way, which leads to fibrillation and. The death of the patient is the most likely scenario.

Clinical classifications are used to identify a specific type of disease, stage, determine treatment tactics and diagnosis.
Causes of 1st degree AV block
These are mainly external factors. They can be eliminated by the patient himself, with rare exceptions.
- Intense physical activity, excessive activity. There is such a thing as a sports heart. Conduction disorders are the result of the development of cardiac structures. Such causes account for up to 10% of all clinical situations. But such a diagnosis can be made after long-term observation and exclusion of organic pathologies.
- Excess medicines. Cardiac glycosides, psychotropic drugs, calcium channel blockers, antispasmodics, muscle relaxants, narcotic analgesics, corticosteroids.
- Violation of braking processes nervous system. A relatively harmless factor. Usually it is part of a symptom complex of a disease.
Causes of 2-3 degree blockade
Much more serious. Possible factors include:
- Myocarditis. Inflammatory pathology of the muscular layers of an organ of infectious or autoimmune (less commonly) origin. Occurs as a consequence in most cases.
Treatment in a hospital, the clinical picture is clear. A terrible complication - destruction of the ventricles is determined in every tenth case.
Especially without special antibacterial and supportive effects.

- Heart attack. Acute disturbance of trophism of cardiac structures. Occurs at any age, mainly in elderly patients. Also against the background of current ischemic heart disease, as a complication.
It ends with necrosis of cardiomyocytes (heart cells), replacement of active tissue with scar tissue. It is unable to contract and conduct a signal. Hence the AV block.
Depending on the extent, we can talk about the degree of severity. The more structures damaged, the more dangerous the consequences.

- Rheumatism. Autoimmune process affecting the myocardium. The treatment is long-term, lifelong maintenance therapy is the result.
It is possible to slow down the destruction and prevent relapses, but complete relief is unlikely.
The neglected phenomenon ends with damage to the His bundles and conduction disturbances.
- Ischemic disease. It is similar in nature to a heart attack, but the process does not reach a certain critical mass, since the blood supply still remains at an acceptable level. However, necrosis of the muscle layer will not take long to occur without treatment. This logical conclusion.

- Coronary insufficiency. As a result of atherosclerosis with narrowing or occlusion of the corresponding arteries supplying cardiac structures. Manifestations occur on late stages. Blockade is one of the organic disorders. Read more about coronary insufficiency.

- Cardiomyopathy. The generic name of a group of processes. Arises as a consequence of severe somatic pathologies.
The essence lies in dystrophy of the muscular layer of the heart. Contractility decreases, the signal damaged tissues performed worse than in the normal position.
Weakened hemodynamics, ischemia, multiple organ failure as a consequence. Types of cardiomyopathy, causes and treatment methods are described.

The presence of pathologies of the adrenal glands of the deficient type also affects thyroid gland, vessels, including the aorta.
Symptoms depending on the degree
Clinical picture depends on the stage of the pathological process.
Stage 1:
Manifestations are completely or mostly absent. The patient feels normal, there are no deviations in his vital functions.
Functional defects can be detected only by electrocardiography results. Often this is an accidental finding, discovered during a preventive examination of a person.
Mild shortness of breath is possible during intense physical activity (work, running, exhausting sporting events).
Attention:
First degree atrioventricular block is clinically favorable. If detected early there is a chance of complete cure without consequences.
Stage 2:
- Chest pain unknown origin. Occurs in most cases. This is a non-specific sign. The duration of the episode is no more than a few minutes.
- Shortness of breath due to intense physical activity. IN calm state she's not there.
- Weakness, drowsiness, lack of performance. Apathy and reluctance to do anything are possible.
- . Change in heart rate downwards. It is not yet threatening.
Stage 3:
- Shortness of breath with little physical activity. Even with simple walking.
- Headache. Determined by ischemic disorders in cerebral structures. The duration varies from a few minutes to hours and even days. It is necessary to differentiate from migraine.
- Vertigo. Up to uncoordination of movements, inability to navigate in space.
- Arrhythmia of several types at once. The slowdown in cardiac activity is accompanied by a change in the time intervals between contractions.
- Fainting.
- Demotion blood pressure to critical levels.
- A sharp drop in heart rate.
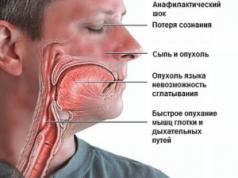
All three symptoms presented above are included in the structure of the so-called. This is an emergency. It lasts a few minutes, but poses an enormous danger to life.

Injury, stroke, heart attack or cardiac arrest are possible. If this kind of manifestation occurs, it is necessary surgery the essence of which is the implantation of a pacemaker.
Stage 4:
It is not always called. It is a variation of the previous one, but is characterized by even more severe symptoms. Massive organic disturbances are noted in all systems.
Death with 4th degree AV block becomes inevitable, it’s a matter of time. However, in order to trigger pathology in this way, you need to try and consciously ignore all the signals from your own body.
Diagnostic methods
Management of persons with abnormalities in the conduction of cardiac structures is under the supervision of a cardiologist. If the process is complicated and has dangerous character- specialized surgeon.
An approximate survey scheme includes the following elements:
- Questioning the patient about complaints, their age and duration. Objectification of symptoms and fixation.
- Anamnesis collection. Including family history, determination of lifestyle, presence of bad habits and others. Aimed at early detection source of the problem.
- Blood pressure measurement. Against the background of an advanced process, by the second stage, or even more so the third, jumps in blood pressure are likely. It is difficult to catch such a condition using routine techniques.
- 24-hour Holter monitoring. More informative way. Blood pressure and heart rate are assessed every half hour or more often, depending on the program. Can be performed repeatedly to improve accuracy.
- Electrocardiography. Allows you to identify functional disorders from the side of the heart. Plays a key role in early diagnosis.
- EFI. Modified version of the previous survey. However, it is invasive. Through femoral artery a special probe is inserted. The activity of individual areas of cardiac structures is assessed. Quite a difficult study, but sometimes there are no alternatives to it.
- Echocardiography. In order to identify organic disorders. The classic option as a result of a long course of blockade is cardiomyopathy of varying severity.
- Blood analysis. For hormones, general and biochemical. For a comprehensive assessment of the body’s condition, in particular endocrine system and metabolism in general.
As necessary, if previous methods do not provide answers to questions, CT, MRI, coronography, and radioisotope studies are used. The decision is made by a group of leading specialists.
Variants of deviations on the ECG
Among the characteristic features:
- Prolongation of the QT interval by more than 0.2 s. At the first stage this is a typical finding.
- PQ extension. Changes in the frequency of occurrence of ventricular complexes. The so-called Mobitz 1.
- Complete loss of contractions of the lower chambers of the heart. Or alternately, in a symmetrical order.
- Decreased heart rate (bradycardia) of varying severity. Depends on the stage of the pathological process.
AV block is specifically noted on the ECG, and the more severe the phase, the easier it is to diagnose the problem.
Treatment depending on the degree
The therapy is complex.
1st degree.
Long-term follow-up is indicated. Such tactics can be repeated for more than one year. If there is no progression, gradually the frequency of consultations with a cardiologist becomes less frequent.
Against the background of deterioration, medications from several pharmaceutical groups are prescribed:
- Antihypertensive drugs. Different types.
- Antiarrhythmic.
If there is an inflammatory infectious pathology, antibiotics, NSAIDs and corticosteroids are used. Treatment is strictly in a hospital.
Transient 1st degree AV block (transient) is the only dangerous case requiring therapy, provided it is of viral or bacterial origin.
2nd degree
The same type of drugs are used. If the condition quickly worsens, there is no point in waiting. The installation of a pacemaker is shown.
Regardless of age. The only exception is older patients who may not be able to withstand surgery. The issue is resolved individually.

3-4 degrees
Implantation artificial driver rhythm is required. Once the terminal phase occurs, the chances of cure are minimal.
Throughout the entire period of therapy, lifestyle changes are indicated:
- Quitting bad habits.
- Diet ( treatment table No. 3 and No. 10).
- Adequate sleep (8 hours).
- Walks, exercise therapy. The main thing is not to overwork. The duration is arbitrary.
- Avoiding stress.
Traditional recipes can be dangerous, so they are not used.
Prognosis and possible complications
Typical consequences:
- Heart failure. Resuscitation in such a situation is minimally effective; as soon as it is restored, the rhythm will change again. A relapse is likely within a few days.
- Cardiogenic shock. Potentially fatal consequence. Moreover, death occurs in almost 100% of cases.
- Fainting and, as a result, injury may be incompatible with life.
- Heart attack or stroke. Acute malnutrition of cardiac structures and brain, respectively.
- Vascular dementia.
Forecasts depend on the stage of the pathological process:
In the terminal phase, death is inevitable. Therapy is ineffective.
Radical surgery with the installation of a pacemaker significantly improves the prognosis.
Finally
Atrioventricular block is a disorder of conduction from the sinus node to the atria and ventricles. The result is total dysfunction of the muscular organ. The mortality rate is high, but there is enough time for treatment and diagnosis. This is encouraging.
First degree atrioventricular block is a pathology in which the conduction function of the heart muscle is disrupted, which is manifested by a slowdown in the conduction of impulses from the atria to the ventricles.
1st degree AV block on the ECG looks like an increase in the PR interval of more than 0.20 seconds. This leads to disruption of blood flow through the vessels and failure heart rate. This condition body is extremely dangerous and, under certain conditions, can lead to a sharp deterioration in the patient’s health and even to fatal outcome. ICD code 10 AV block 1st degree – I44.0.
The cause of AV block is most often a disturbance in the functioning of the adductor system of the heart muscle, which is responsible for the contraction of the atria and ventricles.
Predisposing factors may be increased physical activity or the use of certain medications (for example, papaverine or drotaverine).
This pathology can occur due to the following reasons:
- Sports activities associated with increased physical activity. In professional athletes, first-degree AV block may occur as a result of increased vagal tone.
- Myotonic dystrophy.
- IHD. First degree AV block during myocardial infarction occurs in approximately 15% of patients undergoing therapy.
- Infiltrative diseases (for example, sarcoidosis or amyloidosis).
- Angina pectoris.
- Systemic collagenoses, the course of which is accompanied by vascular damage.
- Some infectious diseases.
- Degenerative pathologies of the conduction system of unknown etiology. Some medications(Digoxin, beta blockers, Amiodarone and a number of others).
- Lev's disease. Its course is characterized by calcification and degenerative fibrosis of cardiac structures (base of the aorta, septum, mitral annulus, etc.).
Kinds
The following types of blockade are distinguished:
- persistent;
- transient 1st degree AV block (another name is 1st degree transient AV block);
- intermittent.
According to the location, 1st degree AV block can be distal and proximal, as well as combined.
Symptoms
The clinical picture depends on the degree and type of blockade. Incomplete 1st degree AV block is in most cases characterized by an asymptomatic course. If severe bradycardia is observed, symptoms such as shortness of breath and weakness (rarely angina attacks) may appear.
If there is a pronounced decrease in blood flow, dizziness and fainting are possible. As blockages progress, they may appear. additional symptoms(arrhythmia, general weakness, darkening of the eyes).
1st degree AV block in children is a consequence of pathological intrauterine development. Most often, this disease occurs when the fetus is affected by various infections (chlamydia, staphylococci, streptococci, and so on). In some cases, AV block is a consequence of a genetic failure. The disease can also develop after surgery for heart defects.
Clinically, AV block manifests itself in children as loss of concentration, heart pain, shortness of breath, weakness, and headaches. If the child is in critical condition (which is rare with first-degree AV block), then implantation of a pacemaker is indicated.
Diagnostics
The main way to diagnose this pathology is an ECG, which not only detects the disease, but also determines its degree. In addition to the ECG, there are a number of additional research, which help to create a more accurate clinical picture of the disease.
Diagnosis of AV block includes:
1. History taking. The doctor conducts a survey of the patient, finds out what complaints the patient has, whether he has had myocarditis or a heart attack in the past, whether the patient has taken drugs that impair the function of the atrioventricular node (beta blockers, digitalis and others).
2. Examination of the patient(physical examination). With first-degree AV block, the first heart sound is weakened, sometimes an irregular rhythm and bradycardia are observed.
3. First degree atrioventricular block on ECG:
- P-Q intervals are prolonged (more than 0.16 seconds in children and more than 0.20 seconds in adults);
- the size of the intervals is constant, each P is followed by a QRS complex.
4. Additional research:
- for hyperkalemia - determination of the content of electrolytes in the blood;
- in case of overdose of drugs that affect heart rate, determine their concentration in the blood.
Treatment of 1st degree AV block is most often not required. It is necessary to eliminate the causes of the blockade and correct electrolyte metabolism.
Prevention of the disease consists of undergoing regular preventive examinations, this is especially true for older people. If a disease is detected, you must follow your doctor’s recommendations, eat right, and consume foods containing magnesium and potassium.
Cardiologist
Higher education:
Cardiologist
Kuban State Medical University (KubSMU, KubSMA, KubGMI)
Level of education - Specialist
Additional education:
“Cardiology”, “Course on magnetic resonance imaging of the cardiovascular system”
Research Institute of Cardiology named after. A.L. Myasnikova
"Course on functional diagnostics"
NTsSSKh them. A. N. Bakuleva
"Course in Clinical Pharmacology"
Russian medical Academy postgraduate education
"Emergency Cardiology"
Cantonal Hospital of Geneva, Geneva (Switzerland)
"Therapy course"
Russian State Medical Institute of Roszdrav
With transient 2nd degree AV block, the conduction of electrical impulses from the atria to the ventricles is partially disrupted. Atrioventricular block sometimes occurs without visible symptoms, may be accompanied by weakness, dizziness, angina pectoris, and in some cases loss of consciousness. The AV node is part of the conduction system of the heart, which ensures the sequential contraction of the atria and ventricles. When the AV node is damaged, the electrical impulse slows down or does not arrive at all and, as a result, a malfunction of the organ occurs.
Causes and extent of the disease
Second degree atrioventricular block can also be observed in healthy trained people. This condition develops during rest and goes away with physical activity. The most susceptible to this pathology are elderly people and people with organic diseases hearts:
- ischemic disease;
- myocardial infarction;
- heart disease;
- myocarditis;
- heart tumor.

Sometimes the disease develops against the background of an overdose of drugs, less common congenital pathology. The cause of atrioventricular block can be surgical interventions: insertion of a catheter into the right side of the heart, valve replacement, organ plastic surgery. Diseases of the endocrine system and infectious diseases contribute to the development of 2nd degree blockade.
In medicine, atrioventricular blocks are divided into 3 degrees. The clinical picture at stage 1 of the disease does not have pronounced symptoms. In this case, the passage of impulses in the organ area slows down.
Stage 2 is characterized by slowing down and partial passage of sinus impulses; as a result, the ventricles do not receive a signal and are not excited. Depending on the degree of loss of impulses, there are several options for 2nd degree blockade:
- Mobitz 1 is characterized by a gradual lengthening of the P-Q interval, where the ratio of P waves and QRS complexes is 3:2, 4:3, 5:4, 6:5, etc.
- Another variant, Mobitz 2, is characterized by incomplete blockade with a constant P-Q interval. After one or two pulses, the conductivity of the system deteriorates, and the third signal no longer arrives.
- Option 3 implies a high degree of blockade 3:1, 2:1. During diagnosis, every second pulse that does not pass through is lost on the electrocardiogram. This condition leads the patient to a slow heart rate and bradycardia.
AV block (grade 2) with further deterioration leads to complete blockage, when not a single impulse passes to the ventricles. This condition is typical for stage 3 of the disease.
Symptoms and treatment
Symptoms of the pathology develop against the background of a rare heartbeat and circulatory disorders. Due to insufficient blood flow to the brain, dizziness occurs and the patient may lose consciousness for a while. The patient feels rare powerful tremors in the chest, and the pulse slows down.
When assessing the patient’s condition, the specialist finds out whether he has had previous heart attacks, cardiovascular diseases, list of medications taken. The main research method is electrocardiography, which allows you to capture and graphically reproduce the work of the cardiac system. Daily monitoring Holter allows you to assess the patient’s condition at rest and during light physical exertion.

Additional studies are carried out using echocardiography, multispiral computed cardiography and magnetic resonance imaging.
If AV block (grade 2) occurs for the first time, the patient is prescribed a course of drug therapy. All medications that slow down impulse conduction are discontinued. Drugs are prescribed that increase the heart rate and block the influence of the nervous system on the sinus node. These drugs include: Atropine, Isadrine, Glucagon and Prednisolone. In cases of chronic disease, Belloid and Corinfar are additionally prescribed. Teopek is recommended for pregnant women and people suffering from epilepsy. The dosage is prescribed by the doctor depending on the patient’s condition.
Long-term heart failure contributes to the accumulation of fluid in the body. To eliminate congestion, take the diuretics Furosemide and Hydrochlorothiazide.
A severe form of the disease with 2nd degree AV block of the Mobitz type 2 requires radical treatment. For this purpose, an operation is performed to install a pacemaker - a device that controls the rhythm and frequency of the heart. Indications for surgery:
- clinical picture of the patient’s condition with frequent fainting;
- AV block (degree 2) Mobitz type 2;
- Morgagni-Adams-Stokes attack;
- heart rate less than 40 beats per minute;
- heart failures with a frequency of more than 3 seconds.
Modern medicine uses the latest devices that work on demand: electrodes release pulses only when the heart rate begins to fall. The operation causes minimal damage and is performed under local anesthesia. After installing the stimulator, the patients' pulse normalizes and disappears. painful sensations and your well-being improves. Patients must follow all doctor's instructions and visit a cardiologist. The operating life of the device is 7-10 years.

Forecast and prevention of the disease
At chronic course pathology, serious complications are possible. Patients develop heart failure, kidney disease, arrhythmia and tachycardia, and there are cases of myocardial infarction. Poor blood supply to the brain leads to dizziness and fainting, and may impair intellectual activity. A Morgagni-Adams-Stokes attack, the symptoms of which are fever and pallor, becomes dangerous for a person. skin, nausea and fainting. In such cases, the patient needs urgent help: cardiac massage, artificial respiration, calling intensive care. The attack can result in cardiac arrest and death.
Prevention of the disease consists of timely treatment heart pathologies, hypertension, blood sugar control. It is necessary to avoid stress and overexertion.
In case of second degree AV block, the following is prohibited:
- engage in professional sports;
- be exposed to excessive physical exertion;
- smoke and drink alcohol;
- After installing a pacemaker, avoid electrical and electromagnetic fields, physiotherapeutic procedures and injuries to the chest area.
A routine electrocardiogram will help identify the disease in the early stages and carry out conservative treatment, which will contribute full restoration person and his return to a normal lifestyle.
When the conduction of electrical impulses through the AV node is impaired, atrioventricular block develops, the degree of which can vary. Her ECG and clinical manifestations change accordingly. In most cases, the pathology does not cause a serious deterioration in well-being. It requires mandatory diagnosis using daily ECG monitoring.
Normally, the impulse generated in the sinus node travels along the atrial pathways, exciting the atria. Then it enters the atrioventricular (AV), that is, the atrioventricular node, in which its conduction speed drops sharply. This is necessary so that the atrial myocardium contracts completely and blood enters the ventricles. The electrical signal then travels to the ventricular myocardium, where it causes them to contract.
At pathological changes in the AV node, caused by heart disease or tension in the autonomic nervous system, the passage of the signal through it slows down or stops altogether. A conduction block occurs from the atria to the ventricles. If the impulses still pass into the ventricular myocardium, this is an incomplete atrioventricular block.
A complete blockade, when the atria contract normally, but not a single impulse penetrates the ventricles, is much more dangerous for health. The latter are forced to “connect backup sources” of impulses lying below the AV connection. Such pacemakers operate at a low frequency (from 30 to 60 per minute). At this rate, the heart cannot provide the body with oxygen, and clinical signs of pathology arise, in particular, fainting.
The incidence of AV block increases with age. Complete blockade is observed mainly in people over 70 years of age, in 60% of men. It can also be congenital, and then the ratio of girls to boys is 3:2.
Classification of pathology
AV block is classified according to ECG signs that reflect electrical processes in the heart. There are 3 degrees of blockade. The 1st degree is accompanied only by a slowdown in the conduction of the impulse through the AV node.

 1st degree AV block
1st degree AV block With the 2nd degree of blockade, the signals are increasingly delayed in the AV node until one of them is blocked, that is, the atria are excited, but the ventricles are not. With the regular loss of every 3rd, 4th, and so on, contractions speak of AV block with Samoilov-Wenckebach periodicity or Mobitz-1 type. If the impulse block occurs irregularly, it is AV block without the specified periodicity or Mobitz-2 type.

 AV block II degree, Mobitz type I (Samoilov-Wenckebach block)
AV block II degree, Mobitz type I (Samoilov-Wenckebach block) With the loss of every 2nd complex, a picture of 2nd degree AV block appears with 2:1 conduction. The first digit in this regard indicates the number of sinus impulses, and the second - the number of signals transmitted to the ventricles.

 Second degree AV block, Mobitz type II
Second degree AV block, Mobitz type II Finally, if electrical signals from the atria do not travel to the ventricles, third degree atrioventricular block develops. It is characterized by the formation of replacement rhythms, causing the ventricles to contract, albeit slowly.
First degree blockade
All impulses emanating from the sinus node enter the ventricles. However, their conduction through the AV node is slow. In this case, the P-Q interval on the ECG is more than 0.20 s.

 AV blockade, first degree
AV blockade, first degree Second degree blockade
Atrioventricular block of the 2nd degree with Wenckebach periodicity manifests itself on the ECG as progressive extension P-Q followed by the appearance of a single non-conducted P-wave, resulting in a pause being recorded. This pause is shorter than the sum of any two consecutive R-R intervals.
An episode of Mobitz-11 type blockade usually consists of 3 to 5 contractions with the ratio of impulses generated and conducted into the ventricles as 4:3, 3:2, and so on.
The ventricles contract under the influence of the replacement rhythm, which is generated in the upper part of the His bundle, either in its legs, or in even smaller pathways. If the source of the rhythm is in the upper part of the His bundle, then the QRS complexes are no wider than 0.12 s, their frequency is 40 - 60 per minute. With an idioventricular rhythm, that is, formed in the ventricles, the QRS complexes have an irregular shape, they are widened, and the heart rate is 30 - 40 per minute.
Diseases associated with infiltration of the heart muscle by pathological tissues that impede conduction through the AV node:
- sarcoidosis;
- hypothyroidism;
- hemochromatosis;
- Lyme disease;
Systemic diseases can also affect the degree of AV conduction: ankylosing spondylitis and Reiter's syndrome.
Iatrogenic causes of AV block (related to medical intervention):
- prosthetics aortic valve;

 Aortic valve replacement
Aortic valve replacement - surgeries for hypertrophic cardiomyopathy;
- correction birth defects hearts;
- some medications: digoxin, beta blockers, adenosine and other antiarrhythmics.
Symptoms

 Clinical signs atrioventricular block depend on its degree.
Clinical signs atrioventricular block depend on its degree.
With a 1st degree block, there are no symptoms, and conduction disturbances are detected only on an ECG. In addition, it can occur exclusively at night.
2nd degree blockade is accompanied by a feeling of interruptions in the heart. With complete AV block, the patient experiences weakness, dizziness, fainting, and a rare heartbeat.
The patient also experiences symptoms of the underlying disease (chest pain, shortness of breath, swelling, instability of blood pressure, and others).
Treatment
AV block is not a disease, but only one of the manifestations of any cardiac pathology. Therefore, therapy begins with treatment of the underlying disease (myocardial infarction, etc.).
First degree AV block and asymptomatic second degree block do not require treatment. You just need to stop using medications that impair AV conduction.


If atrioventricular block on the ECG is accompanied by signs of oxygen starvation of the brain, medical attention is needed.
A remedy for quickly accelerating heart rate, but it is not always effective. In these cases, temporary cardiac pacing is used.
Treatment of atrioventricular block III degree consists of . Depending on the type of blockade, atrial-dependent ventricular pacing or on-demand ventricular pacing may be used.
In the first case, the device is adjusted in such a way that contraction of the atria is artificially carried out to the ventricles. In the second, the stimulator impulse is applied directly to the ventricular myocardium, causing them to contract rhythmically at the desired frequency.
Forecast
This conduction disorder can cause the following complications:
- sudden death due to cardiac arrest or ventricular tachycardia;
- cardiovascular failure with fainting, exacerbation of coronary artery disease or congestive heart failure;
- head or limb injuries during...
When a pacemaker is implanted, all these unpleasant consequences are eliminated.
Scientists have proven that first degree AV block is associated with increased risk occurrence, the need for pacing, heart failure and mortality from any cause.
With congenital AV block, the prognosis depends on the heart defect that caused the disorder. With timely surgical intervention and implantation of a pacemaker, the child grows and develops normally.
About what AV block is, symptoms, complications, watch this video:
Prevention
Prevention of AV block is associated with general measures to prevent heart disease:
- healthy eating;
- maintaining normal weight;
- daily physical activity;
- control blood pressure, cholesterol and blood sugar levels;
- cessation of alcohol abuse and smoking.
Patients with 1st degree blockade should avoid medications that worsen AV conduction, primarily beta blockers (, atenolol, metoprolol and others).
Secondary prevention of blockade complications is the timely installation of a pacemaker.
Atrioventricular block is a violation of the conduction of impulses from the atria to the ventricles. In mild cases it is asymptomatic. However, the 3rd degree of such blockade can lead to fainting and injury, as well as complicate the course of cardiac pathology. The main treatment method for advanced AV block is. This device causes the heart to pump normal rhythm, and all manifestations of conduction disturbances disappear.
Read also
The detected bundle branch block indicates many abnormalities in the functioning of the myocardium. It can be right and left, complete and incomplete, branches, anterior branch, two- and three-bundle. Why is blockade dangerous in adults and children? What are the ECG signs and treatment? What are the symptoms in women? Why was it detected during pregnancy? Is bundle block block dangerous?



The heart obeys the rhythm set by the sinus node. Arrhythmias and heart blocks occur due to the fact that the impulse does not pass correctly through the conduction system of the heart. The ventricles and atria cannot contract rhythmically and coherently, so disruptions occur in the functioning of the myocardium, blood supply to the brain and other organs. Such arrhythmia can cause serious illnesses or testify to existing ones.
The mechanism of development of the problem
A healthy heart obeys a clear rhythm, which is set by electrical impulses. The impulse appears in the sinus node, first contracts the atria, then the ventricles, providing an optimal rhythm with a frequency of 60-80 beats/min. At the same time, optimal blood pressure and oxygen saturation of organs are maintained. Heart block occurs when an impulse does not pass through. full path along the conductive system. Then an extra blow occurs or, conversely, the contraction “falls out”. Consequently, blockade is a subtype of arrhythmia, which characterizes conditions with disruption of the excitability, conductivity and rhythm of heart contractions.
If the pulse increases due to arrhythmia, tachycardia occurs; if it decreases, bradycardia occurs. There are several types of heart blockades, depending on how and where the impulse conduction is disrupted. The types of disease are presented in the table:
| Type of blockade | Description |
| Chronic | Constant failure of impulse transmission. |
| Transitional | Periodic disturbance of impulse transfer. |
| Partial | The momentum slows down. |
| Full | The signal cannot be transmitted completely. |
| Atrioventricular | The signal does not pass through all three branches from the sinus node in three types:
|
| Sinoatrial | There is no full contraction of the heart muscle due to overexcitation of the vagus nerve. |
| Intraventricular | The impulse to the ventricles is not transmitted or is very delayed. |
| Intraatrial | Pathology of signal transmission within the atria. |
Return to contents
Reasons for the development of arrhythmia and blockade
Most often, arrhythmia is caused by the consequences of an unhealthy lifestyle (alcoholism, smoking, abuse of strong caffeine-containing drinks, frequent stress, uncontrolled use of medications), diabetes, heart diseases. After suffered a heart attack myocardium, due to residual scars, the impulse cannot be transmitted correctly, which also causes arrhythmia.
 Sometimes arrhythmia is congenital and inherited.
Sometimes arrhythmia is congenital and inherited.
If a person is healthy and there are no external factors that provoke arrhythmia, this disease itself cannot appear. However, there are certain risk factors. For example, some types of arrhythmias are congenital and are transmitted genetically. Thyroid disease affects the level of hormones in the blood, which changes metabolism. When combined complete blockade and atrial fibrillation or atrial flutter develops severe Frederick's syndrome, in which the rhythm decreases to 20 beats/min. The attack is characterized by fainting and convulsions against the background of cerebral ischemia. Such attacks are called Adams-Morgagni-Stokes phenomena. In the absence of help, the outcome is fatal.
Return to contents
Diagnostic methods
Arrhythmia and heart block are diagnosed using an electrocardiogram (ECG). For each type and type of disease ECG waves look different, which allows the doctor to assess the state of systoles (contractions). Rhythm disturbances are audible when measuring pressure with a mechanical tonometer. The automatic device will indicate the number of heart contractions, which normally should be from 60 to 80 beats/min.
First degree blockade and partial blockade manifest themselves only on the ECG. They may be accompanied by some weakness and dizziness. As it develops, rhythm disturbances, freezing or fluttering of the heart, nausea, dark spots or dots before the eyes are felt. Such deterioration may occur suddenly, rapidly changing periods wellness. The following symptoms may be felt long time. With complete blockade, loss of consciousness is possible, which is preceded by a rare pulse, pallor and cold sweat. Epileptiform seizures are possible. If they occur regularly, they lead to brain hypoxia and death. It is important not to delay visiting a doctor if symptoms appear.
Return to contents
Treatment of arrhythmia and heart block
For partial blockades of the 1st and 2nd degree drug treatment, is generally not used. Most often, this disease is concomitant, so the underlying disease is treated. The recommendations are aimed at organizing healthy image life, moderate physical activity. Walking in the fresh air is beneficial. You definitely need to give up alcohol, smoking, and strong coffee. Treatment of arrhythmia is prescribed only by a specialist. If drug treatment does not help, pacing may be necessary.
If symptoms of 3rd degree blockade appear, you should immediately call ambulance. At this time, it is important to place the patient on a hard, flat surface; if there is no pulse, do indirect massage hearts. If you lose consciousness, perform artificial respiration. Brigade emergency care carries out resuscitation measures, the doctor will decide on the need for constant stimulation. Surgery may be needed.
A comment
Nickname
- Why is the crisis developing?
- What crises are there?
- Clinical picture
- First aid
- Necessary activities
- Means for emergency assistance
- What to do in severe cases
- Conclusion
Every person prone to high blood pressure has a chance to find out from his own experience what it is. hypertensive crisis. It is also called hypertensive. This is understood as a sharp rise in pressure, which is accompanied by characteristic clinical symptoms. This condition is dangerous and requires an urgent but controlled reduction in pressure. Otherwise, vital organs may be damaged.
The diagnostic criterion for this condition is an increase in pressure above 180/120 mm Hg. Art. Sometimes one of the indicators reaches high numbers. But there are cases when the corresponding symptoms are observed at lower values.
Why is the crisis developing?

The reasons why a hypertensive crisis develops are divided into external (exogenous) and internal (endogenous).
TO external factors include:
- sudden cessation of medications that control blood pressure;
- excessive salt consumption;
- strong psycho-emotional stress - stress;
- excessive drinking of alcohol;
- changing weather conditions accompanied by changes in atmospheric pressure;
- reception hormonal contraceptives, NSAIDs, glucocorticoids, B-adrenergic agonists and other drugs that increase blood pressure;
- acute cerebral hypoxia as a result sharp decline pressure caused by the action of drugs;
- resuscitation measures during and after operations.
Endogenous reasons may be the following:
- sudden disruption of kidney function, which is accompanied by increased production of renin;
- hormonal changes in women during menopause;
- progressive deterioration of the condition in patients with coronary artery disease, which is manifested by the development of heart attack, cardiac asthma;
- cerebral ischemia leading to compensatory hypertension;
- disorders in the organs of the urinary system (kidneys) against the background of prostatic hyperplasia;
- secondary hyperaldosteronism;
- psychogenic hyperventilation – breathing disorders;
- crisis in sickle cell anemia;
- sleep apnea syndrome - stopping breathing during sleep.
Hypertensive crises are usually associated with sudden increase vascular tone - arterioles - under the influence of vasoconstrictor factors or as a result of sodium retention. Another reason may be an increase in heart rate, myocardial contractility, or a change in the volume of circulating blood towards its increase.
The severity of the condition is largely determined by the rate of increase in pressure, and not by its numbers. If the pressure grows quickly, then the mechanisms responsible for its stabilization do not have time to turn on.
A hypertensive crisis is accompanied by an increase in pressure in the blood vessels of the brain. Reflex narrowing of the arteries helps compensate for this. And normal blood flow is maintained for some time. A rapid increase in pressure may be accompanied by rupture vascular wall and hemorrhage. Arterial spasm is dangerous for the development of cerebral ischemia. Vessels cannot for a long time to be in good shape, so the spasm is replaced by their dilatation (expansion). Vascular permeability increases, fluid rushes into the brain tissue, and brain edema develops. Symptoms of encephalopathy appear.
Hypertensive crises do not pass without leaving a mark on the heart and large arterial vessels. Increased load and increased myocardial oxygen demand with concomitant ischemic heart disease can be accompanied by attacks of anginal pain up to the development of a heart attack. Acute left ventricular failure may occur. Heart rhythm may be disturbed.
Against the background of high pressure, vascular rupture is possible and symptoms such as nosebleeds and the formation of a dissecting aortic aneurysm may appear. With repeated crises, the kidneys may also suffer.
What crises are there?
Depending on the features clinical manifestations Hypertensive crises are divided into two types:
- Hyperkinetic (neurovegetative, adrenal, type 1) - develops due to activation of the sympathoadrenal system. It is characterized by a sudden onset, violent vegetative symptoms: redness of the face, rapid heartbeat, sweating. Frequent urination may occur. This is a more favorable option, although the appearance of chest pain typical of angina, rhythm disturbances and the development of myocardial infarction are possible. The duration of the attack is from 2 to 4 hours.
- Hypokinetic (edematous, norepinephrine, type 2) – the clinical picture increases gradually, the skin is pale, patients are adynamic. In this case, there is a significant increase lower pressure. Symptoms of brain and heart damage come to the fore. They flow hard. This condition can persist for several days. Such crises are observed in the later stages of the disease and with initially higher blood pressure values.
Currently, the generally accepted classification is that a hypertensive crisis can be complicated or uncomplicated.
The first option includes crises that are accompanied by the development of:
- acute necrosis of the heart muscle (infarction);
- hypertensive encephalopathy;
- ischemic stroke;
- acute left ventricular failure with symptoms of cardiac asthma and pulmonary edema;
- dissecting aortic aneurysm;
- hemorrhages under the membranes of the brain or in the brain;
- transient ischemic attacks.
Crises of any type are considered complicated in pregnant women with eclampsia and preeclampsia (late toxicosis), with traumatic brain injuries, bleeding, and with the use of drugs and amphetamines. Requires hospitalization and treatment in a hospital setting.
An uncomplicated hypertensive crisis is milder and usually does not pose a serious threat to life. No emergency transport to hospital is required. Treatment should result in a slow decrease in blood pressure over several hours.
Clinical picture

The signs of a hypertensive crisis, regardless of the cause and variant, are quite typical. This is a relatively unexpected start. Blood pressure may rise within minutes or hours. The pressure level is individually high.
Signs of brain distress:
- intense headaches and dizziness;
- nausea, sometimes ending in vomiting;
- visual disturbances: there is often double vision, temporary blindness is possible, but more often flies flash before the eyes or a veil appears;
- sensitivity disorders: the face may become numb, pain sensitivity in the face, lips, tongue decreases, a feeling of goosebumps appears;
- movement disorders: possible mild weakness in distal sections hands, transient (up to a day) hemiparesis - paralysis of one side of the body;
- possible temporary speech difficulty - aphasia;
- Rarely, but there are seizures.
Most of these symptoms are due to the development of hypertensive encephalopathy.
A hypertensive crisis also adversely affects the heart. The following symptoms are characteristic:
- pain in the precordial region;
- rhythm disturbances - rapid heartbeat, interruptions in heart function;
- shortness of breath appears.
Autonomic disorders are often observed:
- chills or feeling of heat appear;
- there is tremors in the limbs;
- characterized by irritability;
- a feeling of fear appears;
- sweating and thirst are possible;
- After an attack, copious amounts of urination often occur.
The main signs of a hypertensive crisis are a triad of symptoms: headache, dizziness and nausea. Other symptoms may be observed in various combinations or absent altogether. But every person should know what to do in such a situation.
First aid

Hypertensive crisis must be treated promptly. This should be done correctly, otherwise you may get severe complications. If the crisis is uncomplicated, then you can try to cope with it yourself. Medicines in tablets are used for treatment. A slow decrease in blood pressure, by an average of 25% during the first two hours, is considered optimal. It should stabilize within 24 hours.
Necessary activities
- Calm down. Panic can only make an already difficult situation worse.
- It is better to sit down or take a half-sitting position.
- You can prepare a basin of hot water and put your feet in it. As an alternative, you can use mustard plasters, which are fixed in the area calf muscles. You can use a heating pad.
- Open a window to provide fresh air.
- Take medicine to lower your blood pressure. It is advisable to use the remedy that the doctor recommends in this case.
- Call an ambulance.
Emergency supplies
If a person suffers from hypertension, then medications to quickly lower blood pressure should always be on hand. The same tools are used by emergency doctors in similar cases. You need to take the pills as soon as your blood pressure reaches critical values and the corresponding symptoms appeared.
- Captopril is an ACE inhibitor. Begins to act in 5 minutes. The effect lasts on average about 4 hours, rarely longer. A 25 mg tablet is placed under the tongue and kept there until completely absorbed. Some patients report an unpleasant tingling sensation under the tongue. The dose can vary from half a tablet to 2. It all depends on the blood pressure. The drug is indicated for any type of crisis. Not for use in pregnant women, for the treatment of nursing women and persons under 18 years of age.
- Nifedipine is a calcium channel blocker. It can also be found under other names: phenigidine, corinfar, cordaflex, cordipin. The effect occurs 15–20 minutes after oral administration and 5 minutes after sublingual (under the tongue) use. The drug is effective for a maximum of 6 hours, with an average of 4 hours. Tablets have a standard dose of 10 mg. They can be placed under the tongue or simply chewed. To relieve high blood pressure, you may need from 1 to 4 tablets. It is undesirable to use the drug during type 1 crises, since nifedipine causes tachycardia, characterized by redness of the facial skin. In case of severe atherosclerosis, it is better not to take the drug.
- Clonidine (clofedine) – drug central action. After sublingual administration, the pressure begins to decrease within 10–15 minutes. The action ends after 2–4 hours. The recommended dose is 0.15 or 0.075 mg. It is permissible to take no more than 2.4 mg per day. The use of the drug is not recommended for significant atherosclerotic vascular damage, which is especially common in older people. Contraindications are: severe bradycardia, heart block, pregnancy and lactation.
- Propranolol (anaprilin) is a drug from the group of non-selective B-blockers. After oral administration, the hypotensive effect is observed within 30–60 minutes and lasts up to 4 hours. Tablets come in 10 or 40 mg. It's better to start with a lower dose. This is the most effective remedy during crises of type 1, accompanied by tachycardia and severe vegetative symptoms. The drug is contraindicated in severe heart failure, bradycardia and heart block.
- Moxonidine is a centrally acting drug. Other names of the medicine: physiotens, moxonitex, moxarel, tenzotran. It is an excellent alternative to clonidine, since the latter can only be obtained with a special doctor’s prescription. A 0.2 or 0.4 mg tablet is used on the tongue. It acts quickly and for a long time, more than 12 hours. Contraindications are similar to clonidine, but the list can be supplemented with conditions such as Parkinson's disease, epilepsy and glaucoma.
When using medications, individual intolerance should be taken into account.
When the pressure stabilizes, treatment for hypertension continues by usual means. After a hypertensive crisis has occurred, you should definitely consult your doctor. In consultation with the doctor, treatment can be changed.
What to do in severe cases

If symptoms appear that indicate the development of complications, then the ambulance team is involved in treatment. Before starting treatment, the doctor will definitely do an electrocardiogram to rule out acute cardiac pathology, talk to you and provide first aid.
Medicines are administered intravenously. This may be clonidine, enalaprilat, propranolol, furosemide (Lasix), urapidil (Ebrantil). Nitroglycerin is used according to indications. It is extremely rare to resort to drugs such as sodium nitroprusside or phentolamine. Such patients should not stay at home.
Indications for hospitalization:
- the first crisis;
- if crisis conditions are repeated many times;
- crisis, which began to be treated at prehospital stage, but this did not bring a positive effect;
- the appearance of symptoms of hypertensive encephalopathy;
- development of complications requiring intensive treatment and constant medical supervision;
- malignant arterial hypertension.
Patients are hospitalized in the therapy or cardiology department. If a stroke develops, treatment is carried out in the neurology department.
Conclusion
Every person who suffers arterial hypertension, as well as his relatives, must clearly understand the dangers of a hypertensive crisis. You need to be prepared for this. However, it is much more important to prevent exacerbations of hypertension, manifested in the form of such pressure surges.
To do this, you need to remember the reasons that provoke an increase in pressure in order to exclude them. It is necessary to understand the basic symptoms and first aid methods. But most importantly, you should regularly follow the recommendations of your doctor and do not try to experiment with medications. You cannot cancel treatment on your own. Any mistake can cost your life.