Urinary incontinence (or incontinence) is perceived by many as a typical pathology old age. Indeed, this disease affects more than half of women after 70-80 years. However, a similar problem occurs not only in older women, but also after childbirth, in late pregnancy, after some operations, and even in stressful situations.
The problem causes many inconveniences and restrictions in Everyday life leads to self-doubt depressive states, isolation, violations in sexual relations. Unfortunately, not all women decide to apply for medical care, hushing up about the disease or looking for dubious means traditional medicine. Pathology can be overcome only with the help of competent treatment.
Causes of the disease
There are many factors that can cause incontinence. There are several main reasons among them:
- the period of pregnancy and after the birth of a child, when the enlarged uterus has high blood pressure on the pelvic organs;
- prolonged stressful conditions;
- age-related changes that cause a decrease in the elasticity of the ligaments and muscle tone;
- surgical operations on the pelvic organs (uterus, bladder, rectum), complicated by the appearance of fistulas or.
It should be noted a number of diseases in which urinary incontinence is one of the symptoms. This diabetes the presence of stones in the bladder, multiple sclerosis, stroke. provoke pathological condition some medications (for example, diuretics), abuse of strong tea, coffee and alcoholic beverages, smoking, overweight. Even healthy woman high estrogen drugs or antidepressants can cause problems with keeping the urge to urinate. After discontinuation of these drugs, this condition disappears without treatment.
In women over 50, urinary incontinence can be hereditary. Availability in childhood Enuresis years later can also be a predisposing factor for senile incontinence.
Types of pathology
IN modern medicine There are several types of urination disorders. Their classification reflects the features of various cases that make it impossible for the patient to control the process.
- stress urinary incontinence
This condition is one of the most common. Uncontrollable discharge occurs during even minor physical exertion, when coughing and sneezing, when jumping and running, lifting weights, laughing. The main reason is the weakening of the pelvic floor muscles.
- Urgent urinary incontinence
Or urgent - can be caused by hyperactivity Bladder. Its nerve endings instantly react to the slightest external stimuli: the sound of water, bright light. The desire to urinate occurs suddenly when a woman cannot keep the process under control. Incontinence can be caused by diseases of the brain, hormonal disorders, inflammatory processes in the bladder.
- Bedwetting (enuresis)
It is more common among young children suffering from excessive nervous excitability. But there are frequent cases of the development of pathology in women of advanced age, as well as in younger representatives of the weaker sex.
Mild urinary incontinence that occurs at night can be caused by hormonal changes, psychological trauma, diseases of the urinary system. Enuresis can occur after childbirth at the birth of twins or a baby with a large weight.
The inability to control the process of urination does not always indicate a full bladder. A small amount of urine may squirt or drip.
- mixed incontinence
Occurs in about a third of cases of pathology. This type disorders combines the symptoms of incontinence during physical exertion and an urgent urge to urinate. More frequent urge to urinate is characteristic - more than 8-10 times in the daytime and more than once at night. This pathology often appears after childbirth or after suffering traumatic lesions of the pelvic organs.
- Permanent incontinence
With this type of incontinence, the outflow of a few drops (leakage) occurs with small interruptions during the day, regardless of physical stress.
The manifestation of the disease during menopause
Surgical treatment
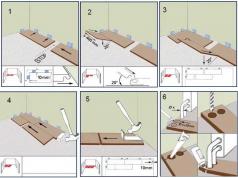
What to do, if conservative treatment did not give effective results? In these cases, sling operations are prescribed. The main indicators for surgical intervention are urgency and stress incontinence. A number of contraindications should be taken into account. The operation is not performed for pregnant women, in the presence of inflammatory processes in the organs of the urinary system, for patients who take medications to thin the blood.
After a preliminary consultation with a urologist and a therapist, the sling operation is performed under local anesthesia. On the front wall of the vagina, a loop is installed that will support the bladder in correct position. The procedure lasts no more than 30 minutes. To control the process of urination, a catheter is installed, which is removed a day or two after the manipulation. After removing the catheter, a number of women report minor pain, which are easily eliminated by painkillers.
The recovery period lasts from two weeks to a month. A woman should be in a state of physical and sexual rest, avoid lifting weights, intense sports, driving a car. sex life allowed no earlier than one month.
Sometimes there may be complications:
- bladder injury;
- bleeding;
- development inflammatory process, for its prevention, a course of antibiotics is prescribed;
- problems with urination immediately after surgery;
- intestinal disorders.
Carrying out the operation in medical institution with a good reputation eliminates the risk of complications and makes surgical intervention absolutely safe for health.
laser therapy
Laser exposure is one of the most effective methodologies to normalize urination. With the help of pulses, the walls of the vagina are processed and urethra. Laser urinary incontinence treatment tightens the walls of the bladder, making them more elastic. The method has many advantages. It is painless, safe for the patient, does not require a long recovery period.

According to statistics, more than 90% of patients report positive results after laser therapy sessions. The laser is not used for severe prolapse of the vagina, prolapse of the uterus, if present in the body malignant tumors and bleeding. One of the contraindications is age over 60 years.
Traditional medicine
You can fight the problem of urinary incontinence with the help of folk remedies. Using the usual medicinal herbs, it is easy to prepare decoctions and infusions that will help reduce the activity of symptoms without the use of drug treatment.
Folk remedies will be effective for urinary incontinence with their regular use and compliance with the rules of nutrition. However, it should be borne in mind that the use of infusions and decoctions is not effective for urgent incontinence that occurs during menopause, age-related changes or the presence of inflammatory processes.
- Dill seeds
Two tablespoons of seeds are poured into 0.5 liters of hot water and left to infuse overnight. In the morning, the resulting infusion is filtered and drunk before meals. The duration of treatment is 10 days. After a ten-day break, the treatment is repeated.
- Cowberry
To prepare the medicine, dry berries and leaves of the plant are taken. They are crushed, the same amount of St. John's wort is added, poured with boiling water and kept in a water bath for 10-15 minutes. Take a decoction should be a glass three times a day.
- Elecampane
The root of the plant is poured with boiling water, kept on low heat for at least a quarter of an hour, insisted in a dark place for several hours, a small amount of honey is added. The resulting mixture is drunk before going to bed 2-3 times a day.
- Corn silk
2-3 teaspoons of corn stigmas are poured with boiling water, kept for a quarter of an hour or more, filtered. Take the resulting broth several times a day, about half a glass with the addition of a teaspoon of honey.
- Shepherd's bag
Two tablespoons of chopped herbs insist in a glass of cool boiled water, filter. Take a tablespoon several times a day. This remedy is effective for nighttime incontinence.
Many patients also note the effectiveness of the following home remedies:
- cold decoction prepared from the bark of viburnum, elm, ash;
- taking a glass of fresh carrot juice before breakfast;
- eating several times a day a pinch of crushed dill seeds;
- inclusion in the menu of tea made from young twigs of cherries or sweet cherries.
Treatment folk remedies has been proving its effectiveness for many years. However, if a woman does not see a significant improvement after taking the course, she should consult a doctor in order to prescribe more effective methods or surgical treatment. Self-medication for a long time can be hazardous to health.
Lifestyle changes and prevention
When such a problem appears, a woman has to make certain adjustments to her lifestyle. First of all, you need to pay attention to personal hygiene. To avoid irritation and infection of the skin, after a shower, the affected areas should be treated with moisturizing anti-inflammatory creams or medicines. Well, if they contain petroleum jelly, lanolin or cocoa butter. When taking a shower, use warm, but not hot, water.

Many women have to give up some of the pleasures of life because of the fear of leakage and odor. Absorbent protective pads are used to protect and eliminate these problems. Also in pharmacies you can buy special underwear. It should be changed and washed regularly.
Prevention of urinary incontinence involves the following measures:
- It is strictly forbidden to lift weights exceeding 5 kg, this causes excessive tension in the muscles of the pelvic region and serves as a provoking factor in the development of pathology.
- Under any circumstances, monitor the complete emptying of the bladder, do not postpone the process "for later."
- Watch your diet, do not overeat.
- Early detection and treatment inflammatory diseases urinary system.
- Be active, follow the daily routine, including sports, swimming, walking.
- Monitor timely bowel movements, fight constipation.
- Provide yourself with a favorable emotional atmosphere, avoid stressful situations, chronic lack of sleep, increased physical and psychological stress.
- Control the amount of fluid you drink (1.5-2 liters per day).
- Make sure you empty your bladder before bed.
- Do not abuse sweet carbonated drinks, packaged juices, strong tea, coffee and alcohol.
- Visit your urologist regularly.
- Perform for prevention.
Particular attention should be paid to the listed preventive measures for expectant mothers and women with menopause. A positive emotional attitude is of great importance.
Urinary incontinence is a disease that requires careful long-term treatment. Only complex therapy together with changes in the daily routine and nutrition, it will eliminate the pathology and return the opportunity to lead a normal life.
The condition in which there is an involuntary release of urine in women is called "incontinence" or urinary incontinence. R There are several main types of pathology: stressful, urgent (imperative) and combined.
More often, urologists are faced with a stressful form of urinary incontinence.
At the same time, involuntary urination is associated with an increase in pressure in the bladder, which occurs when sneezing, laughing, coughing, lifting weights, a sharp change in body position in space, the sound of running water, hypothermia, etc.
Mixed urinary incontinence has signs and stress form, and urge incontinence with an overactive bladder.
Table of contents:note
Girls and nulliparous women rarely suffer from this delicate issue, mainly, women over the age of 40 and during menopause face the disease.
stress urinary incontinence
There are many predisposing factors to this form of pathology:
- In the first place, experts unanimously attribute complicated independent childbirth during which the muscles and tissues of the pelvic floor were traumatized and significantly stretched.
- Congenital pathology of the sphincter of the bladder and muscle fibers can also be the cause of stress urinary incontinence.
- Surgical interventions on the organs of the genitourinary sphere of a woman, iatrogenic injuries during medical manipulations.
- Hormonal disorders associated with insufficient production. More often - this is the cause of urinary incontinence during the period of natural fading of ovarian function in. With the onset of menopause, the pathology progresses, as there is a change in the structure connective tissue, decreased collagen production against the background of hypoestrogenism.
- Work involving heavy lifting.
- Diseases of the broncho-pulmonary system, in which debilitating leads to almost constant high intra-abdominal pressure.
Stress urinary incontinence develops due to anatomical disorders or due to changes in the work of the sphincter and urethra.
The degree of incontinence is determined by the amount of urine lost:
- drip (up to 50 ml);
- light (from 50 to 100 ml);
- medium (from 100 to 200 ml);
- severe (from 200 to 300 ml);
- very heavy (over 300 ml).
How to treat stress urinary incontinence in women
Treatment is always individual, and depends on the location of the bladder relative to the pubic symphysis, the amount of urine lost, the age of the patient and concomitant extragenital pathology. So, surgery older woman c in history is not shown, even with severe urinary incontinence. In this case, if there are no contraindications to conservative therapy, it is possible to prescribe medicines, wearing a vaginal ring, physiotherapeutic effects and physiotherapy exercises aimed at strengthening the muscles of the pelvic floor.
So, the methods of treatment of stress urinary incontinence:
- drug therapy;
- physiotherapy;
- physiotherapy;
- wearing assistive devices that change the angle of the urethra.
- surgical treatment.
Note that the above methods are used alone or in combination, at the discretion of the attending physician.
What medications are available to treat stress urinary incontinence?
Of course, the treatment regimen depends on the cause that led to the pathology.
Hormone treatment
If stress urinary incontinence has developed against the background, it is possible to use hormones as replacement therapy both systemic and local.
Sometimes hormones with systemic treatment are taken for 5 to 7 years, and with local therapy, indefinite use of hormonal drugs is possible. This is relevant only with positive dynamics from the use of hormone replacement therapy.
 Against the background of taking estrogens, collagen synthesis increases, blood circulation improves, muscle tone is restored, contractility detrusor and tissues that enter the ligamentous apparatus.
Against the background of taking estrogens, collagen synthesis increases, blood circulation improves, muscle tone is restored, contractility detrusor and tissues that enter the ligamentous apparatus.
Due to the inhibitory effect of calcium channels, the overactivity of the bladder decreases.
Estrogens stimulate local immune response, so organ resistance can be expected genitourinary system women to various infections.
Hormone replacement therapy with estrogen is not suitable for everyone, there are a number of contraindications, for example, hormone-dependent breast tumors, therefore, before taking hormones, it is necessary to undergo a complete laboratory and instrumental examination.
The disadvantages of hormone replacement therapy include the fact that the effect persists only during the treatment period, in the future, the symptoms of urinary incontinence reappear.
Good reviews of urogynecologists about herbal medicine Klimadinon (active substance- Cimicifuga plant). It contains plant estrogens, which causes a mild effect.
Treatment with drugs that affect the tone of the smooth muscles of the urinary tract
There is a sufficient choice of drugs from this group on the pharmaceutical market:
- Spasmex;
- Urotol;
- Driptan;
- Vesicar.
 It should be noted that the effect of taking these drugs in stress urinary incontinence is weak, so it is unreasonable to call them drugs of choice.
It should be noted that the effect of taking these drugs in stress urinary incontinence is weak, so it is unreasonable to call them drugs of choice.
Adrenomimetic Gutron affects the tone of smooth muscles and urethra, but has many side effects, one of which is an increase in blood pressure. The effectiveness of the reception is currently questioned.
Ubretide(a group of anticholinesterase agents) is used for confirmed bladder hypotension. Do not prescribe to women suffering from the gastrointestinal tract, etc.
There is evidence of positive dynamics in the state on the background of taking, in particular the drug Duloxetine(Symbalta). The opinions of experts are divided, since a positive effect is recorded only in half of the cases.
Surgery for stress urinary incontinence
We list all types of major surgical interventions for this pathology:
- Sling operations . The angle of the urethra changes due to the passage of a synthetic loop under it, which retains urine even in cases of increased intra-abdominal pressure. If the cause of stress incontinence lies in the pathology of the sphincter, the effectiveness of sling operations is very problematic. Some women may relapse after a certain period.
note
Sling surgeries are performed more often than others, and are recognized as the most reasonable in stress urinary incontinence.

Urgent urinary incontinence

In the first place, as the cause of urge urinary incontinence, consider the overactivity of the bladder, in particular, its uncontrolled contractions. This condition can be provoked by tumors and injuries of the spinal cord or brain, infections of the urogenital tract, hypoestrogenism (the longer the period of postmenopause with a decrease in estrogens, the more likely it is to develop pathology), circulatory disorders of the cerebral vessels, and a number of other reasons.
The main symptoms on the basis of which the diagnosis is made are as follows:
- , including nocturia (from 8 times a day);
- irresistible urge to urinate;
- urinary incontinence;
- the ability to control urination when laughing, coughing, etc.
Treatment of urge urinary incontinence in women
Estrogen hormone replacement therapy is carried out with confirmed hypoestrogenism. We talked about its positive effect above.
In overactive bladder, in contrast to stress urinary incontinence, the following drugs are effective:
- spasmex,
- Vesicar,
- Urotol,
- Detrusitol,
- Driptan.
The action is carried out by blocking muscarinic receptors in the walls of the bladder against the background of suppression of acetylcholine.
According to the results of ongoing research, combined application M - anticholinergic and substitution hormone therapy allows you to quickly achieve improvement in well-being.
note
A number of authors consider it reasonable to include alpha-adrenergic blockers, for example, Omnik, Fokusin, Proflosin, in the syndrome of abrupt urination in the scheme. Tamsulosin (active ingredient) at a dosage of 0.4 mg / day. prevents the onset of ischemic disorders, relaxes the muscles and increases the capacity of the bladder.
 most efficient and safe drug – Vesicar. Side effects when taking it, they are less common than when using similar drugs, and the frequency of administration is 1 time per day, 5 mg. Vesicar can be taken for a long time.
most efficient and safe drug – Vesicar. Side effects when taking it, they are less common than when using similar drugs, and the frequency of administration is 1 time per day, 5 mg. Vesicar can be taken for a long time.
More recently, the drug Betmiga (Mirabegron) has appeared on the pharmaceutical market. The main indication for the appointment is an overactive bladder with symptoms of urinary incontinence, sudden urges and frequent urination. Take orally 50 mg.
As a rule, urge urinary incontinence responds well to conservative therapy. In cases where the medication has not been effective, resort to surgical treatment.
Recently, the introduction of botulinum toxin into the detrusor is gaining popularity, as effective method treatment of urge urinary incontinence in women.
The intervention is considered minimally invasive, the effect of the application develops quite quickly. The drug is administered during cystoscopy.
Mixed form of urinary incontinence in women
Depending on the prevalence of symptoms, they are determined with the tactics of management. It is possible to carry out surgical treatment followed by drug therapy.
Urinary incontinence during pregnancy
Urinary incontinence in a pregnant woman can occur for several reasons:
- hormonal changes,
- a constant increase in pressure on the bladder by a growing uterus,
- overstretching of the pelvic floor muscles.
Predisposing factors include the following:
- large weight of the fetus, its position in the uterus;
- mother/large gain during pregnancy;
- several pregnancies and childbirth in history, including complicated ones.
Urinary incontinence during pregnancy is usually not a pathology, and many women experience it in the third trimester.
To exclude inflammation, check.
Urinary incontinence is a fairly common problem. More than half of all representatives of the weaker sex face it at least once in their lives. Incontinence can occur both in young women after childbirth or surgery, and in mature women after menopause. Statistics show that every fifth girl in her reproductive age suffers from urinary incontinence, in early period every third lady faces this problem, and after 70 years - every second elderly woman.
Urinary incontinence is a serious problem that significantly impairs the quality of life, leads to disorders in the sexual and psychological sphere, can provoke depression, and becomes an obstacle to the successful building of a personal life and career. Enuresis should be considered from the point of view of not only a hygienic aspect - this disease also has medical and social significance, as it causes a wide variety of problems in women: sexual dysfunctions, neuroses, etc.
You can also come across such a term as incontinence, which also means urinary incontinence, but is more often used by urologists and gynecologists when making a diagnosis. Enuresis is the name given to a urinary incontinence that is accompanied by an inability to control the emptying of the bladder. Leakage volumes can vary from a few drops to almost the entire contents of the organ. The disease is treated by gynecologists, urologists, surgeons and psychotherapists.
The problem of urinary incontinence is so global that even a special international medical organization, dealing with the study of the causes of enuresis and the development of new effective methods of treating this disease.

There are the following types of urinary incontinence:
stressful;
Imperative (urgent);
iatrogenic;
mixed;
Other forms, for example, enuresis with overflow of the bladder, continuous leakage of urine, unconscious incontinence, etc.
In women, it is the first three types of urinary incontinence that are most common, so it is worth dwelling on them in more detail.

Stress urinary incontinence is the inability to control the process of emptying the bladder during stress. The word "stress" in this context means "load" or "effort".
Symptoms of stress urinary incontinence:
Passing urine when laughing, coughing, sneezing, physical activity, sexual intimacy.
If there is no voltage abdominal cavity, no urine is excreted.
Not every cough or sneeze results in the involuntary release of urine. On early stages the development of incontinence, this occurs only with a crowded organ, and the volume of lost urine is equal to a few drops.
As the disease progresses, even minor physical activity, such as brisk walking, can lead to loss of urine.
Irresistible urge to urinate in a woman is absent.
Together with urine, involuntary excretion of feces and gases from the intestines can occur.
Normally, physical activity, as well as coughing and laughing, should not lead to the release of urine. This is prevented by the pelvic floor muscles and the sphincter. However, when they are weakened, they become unable to fully cope with their function. Urine overcomes their resistance and flows out.
There may be several reasons:
Difficult childbirth. In this regard, childbirth is especially dangerous, accompanied by the release of a large fetus, perineal incisions, the application of forceps and other manipulations. Women with a narrow pelvis are at risk.
Surgical interventions on the pelvic organs. Any intervention on the bladder, rectum, uterus can lead to stress urinary incontinence. Fistulas that form between organs are dangerous, since these defects also lead to urinary incontinence.
Hormonal changes in a woman's body that occur with age. The less estrogen is produced, the worse becomes the elasticity of the ligaments and the lower will be muscle tone.
In addition to the main causes that lead to stress urinary incontinence, we can additionally highlight the following factors risk:
Overweight, especially in combination with diabetes;
Sharp weight loss;
Hard work associated with high physical exertion;
Passage of radiation therapy;
Prolapse and prolapse of the uterus;
Weight lifting;
Burdened heredity;
Belonging to the Caucasian race;
Neurological diseases, including heart attacks, spinal injuries;
Taking certain medications.

Urgent urinary incontinence is characterized by an unbearable urge to empty the bladder. These urges are imperative, and it is almost impossible to restrain them. And they occur when the bladder is only partially filled. While normally, a woman experiences an urge to urinate when a sufficiently impressive amount of urine accumulates in the bladder.
Symptoms of urge urinary incontinence include:
The urge to empty the bladder is very frequent and occurs more than 8 times a day.
They almost always appear suddenly.
The urge to urinate is irresistible.
There are frequent trips to the toilet at night.
The urge to urinate is often dictated by external factors, among which, for example, the sound of water pouring from a tap, a bright light, a loud sound, etc.
When urge urinary incontinence occurs against the background of a prolapsed bladder, a woman may experience pain and discomfort in the lower abdomen.
Urine leakage may be accompanied by the development of dermatitis in the groin area, and urinary infections such as vulvovaginitis, cystitis, etc. may occur.
The cause of urge urinary incontinence in women lies in the violation of neuromuscular transmission in the detrusor of the bladder (muscular frame), which leads to its increased activity. Therefore, even when a small amount of urine accumulates in the cavity of the organ, the woman experiences the urge to urinate. As for the risk factors that can lead to the development of urge urinary incontinence, they are similar to the risk factors for stress incontinence. Often these two types of incontinence are combined with each other.

Iatrogenic urinary incontinence is incontinence that develops while taking medications. As a rule, enuresis becomes side effect one medication or another.
You should be aware that medications such as:
Adrenomimetics (Pseudoephedrine), which are used to treat bronchial diseases. First, such drugs provoke urinary retention, and then cause incontinence.
Any diuretic drugs.
Adrenoblockers.
Hormonal preparations containing estrogen in their composition.
Colchicine, which is used in therapy.
Antidepressants.
Sedative medicines.
When the course of treatment with the listed drugs is completed, urinary incontinence will pass on its own and will not require any therapeutic measures.

Diagnosis of urinary incontinence should begin with keeping a diary. You need to fix the data in it for several days. At this time, a woman should write down how much liquid she drinks, how many times she goes to urinate. It is important to measure the volume of urine released, as well as display in the diary all episodes of urinary incontinence and what she was doing at that time. To understand exactly how much urine goes into episodes of incontinence, you can use the so-called PAD test. For a certain time, the patient wears urological pads, weighing them before and after use.
A conversation in the doctor's office is of no small importance. It allows you to find out the symptoms of the disease, the time of its manifestation.
A woman must visit a gynecologist. During the examination on the chair, the doctor assesses the condition of the muscles and tissues of the pelvic floor, the presence or absence of prolapse of the vaginal walls and uterus.
A cough test is performed in the gynecologist's office. The woman is asked to cough while her bladder is full. If urine is expelled during exertion, stress urinary incontinence may be suspected.
As a rule, the diagnosis is not difficult in most cases. However, additional tests may be required, such as:
Cystoscopy. This study involves examining the bladder from the inside. For this purpose, a thin cystoscope is inserted inside through the urethra. The procedure for a woman is painless, for which the doctor uses a special anesthetic gel. Cystoscopy makes it possible to assess the condition of the bladder, to exclude the presence of tumor formations.
Urodynamic examination evaluates the process of filling and emptying the bladder. To carry it out, special sensors are inserted into the bladder itself and into the vagina, which provide the information necessary for the doctor.
Ultrasound of the pelvic organs. This examination allows you to assess the state of the organs of the female reproductive system, which makes it possible to determine the further therapeutic tactics.
As for laboratory research methods, a woman is prescribed a general and bacterial analysis of urine, a microscopic examination of a smear. Thanks to the above methods of examination, the doctor will be able to make the most accurate diagnosis and prescribe the necessary treatment.

Most often, in older women over the age of 50, a mixed form of urinary incontinence predominates, that is, there is both a stress and an urgent component.
There can be many reasons that lead to the disease, so the doctor during the examination must find out the following points:
Does the woman suffer from neurological pathologies.
Does she have mental disorders?
Does the woman suffer from diabetes?
Does she have problems with being overweight.
Are there hernias intervertebral discs or other degenerative diseases spinal cord that can affect the functioning of the bladder.
Did the woman have a history of surgery on the pelvic organs. If there were any, then it is important to find out if they provoked the formation of adhesions and fistulas.
All these diseases can be the cause of urinary incontinence, as in one way or another they can affect the functionality of the bladder. It is possible that the woman has “overfilling incontinence”, that is, due to the reduced sensitivity of the organ, the signal to empty it is transmitted to the brain too weakly, or not at all.
It is important to find out which medications a woman is taking. Special attention give sedative and antihypertensive drugs, diuretics.
In elderly patients diagnosed with stress incontinence, prolapse is detected in 30% of cases. pelvic organs, namely, the prolapse of the bladder. Therefore, the approach to both diagnosing an existing problem and treating older women must necessarily be individualized. We should also not lose sight of the fact that urinary incontinence can develop against the background of relative health due to a lack of estrogen production in the postmenopausal period.
A comprehensive urodynamic examination for elderly women complaining of urinary incontinence is prescribed without fail.

Therapeutic tactics largely depend on what exactly caused the urinary incontinence and how far the problem has gone. The disease is treated by gynecologists, urologists and surgeons (if surgery is required).
Treatment of any type of urinary incontinence should be started according to the principle “from simple to complex”.
First, you should definitely try the most accessible methods, including:
Getting rid of excess weight in the presence of obesity. The fact is that excess body weight affects the condition internal organs that are subjected to overpressure. As a result, their location is disturbed, functioning suffers, which leads to problems with urination. Obesity can be treated with diet, drugs, psychotherapy, or surgical intervention on the stomach.
Any drinks that contain caffeine should be limited. This primarily applies to coffee and tea. The ban on caffeine is due to its diuretic effect on the body. With excessive intake of this substance, the risk of urinary incontinence increases significantly. As for the use of the usual clean water, then it cannot be limited, otherwise the situation can be aggravated.
Refusal of cigarettes. So far, no clear relationship has been established between tobacco smoking and the problem of urinary incontinence. However, it has been proven that women suffering from smoker's bronchitis are many times more likely to develop stress urinary incontinence. In general, any disease respiratory system must be treated promptly.
Imperative urinary incontinence is perfectly treated when the patient manages to correct the urination regimen. The essence of this method boils down to the fact that you need to accustom your body to urinate by the hour. The initial interval can be set to 30 minutes and then increased to an hour or more.
In order to increase the tone of the pelvic floor muscles, you should exercise regularly. Special exercises will allow you to correct the work of the sphincter and the walls of the bladder.
All chronic diseases must be treated in a timely manner in order to prevent their exacerbation.
It is equally effective to create a psychological attitude that distracts from the desire to empty the bladder.

Kegel exercises are a gymnastic complex that is very easy to implement. First, a woman must decide what the pelvic floor muscles are and where they are located. To do this, you need to imagine the process of emptying the bladder and try to stop it with muscle power. It is these muscles that should be involved during training.
Three times a day you need to strain and relax the muscles of the pelvic floor. The tension time ranges from a few seconds at the initial stages of training to 3 minutes later. Kegel exercises can be performed almost anywhere and anytime, as they are completely invisible to others.
When the muscles are sufficiently trained, you can try to strain them during coughing and sneezing, during physical exertion. The more varied the exercises, the higher their effectiveness.
You can use techniques such as fast and slow contractions, pushing out like pushing during childbirth, holding the jet during emptying of the bladder.
biofeedback therapy
Exercises with biological feedback(BFB) are superior in effectiveness to Kegel exercises, as they allow you to strain only the right muscles. To implement the complex, specialized equipment is required. It is designed not only to control the process of muscle tension, but also to additionally stimulate them with the help of electrical impulses.
It has been proven that biofeedback training allows you to achieve control over urination in quite short time. However, exercises are prohibited for implementation in the presence of malignant formations, inflammatory diseases in acute stage, pathologies of the heart, liver and kidneys.
The use of simulators for the treatment of urinary incontinence
There are a lot of devices that allow you to train the muscles of the pelvic floor. Many of them are very compact and easy to use. For example, the PelvicToner simulator allows you to competently increase the load on the muscles, gradually strengthening them. The device is very easy to use, and its effectiveness has been proven in clinical studies.
Psychotechnics
When you have the urge to urinate, you can try to distract yourself from them by moving your thoughts in a different direction. For example, think about upcoming plans for life, read interesting literature, etc. The main task that a woman faces is to delay urination, at least for a short time.
Medications
Vitafon for urinary incontinence

The Vitafon device is a vibroacoustic device that allows you to strengthen muscles and rejuvenate the body. Treatment with Vitafon refers to physiotherapeutic methods of exposure that can be used at home. The device is a housing block connected to the mains. Attached to it are two round diaphragms that emit acoustic vibration in several programmable ranges. It is these membranes that need to be applied to problem areas to provide a therapeutic effect.
Mechanism of action. Phonation with Vitafon allows you to massage the desired area, and the effect is carried out at the cellular level, which improves the nutrition of tissues, both muscle and nerve.
In case of urinary incontinence, phonation of the following zones is carried out:
Perineum area - 10 minutes;
The area of the muscular sphincter of the bladder (slightly above the pubis) - 10 minutes;
Kidney area - 10-30 minutes;
Liver area - up to 15 minutes;
Lumbo-sacral zone - 5 minutes.
Each zone is treated 1-3 times a day. The course of treatment continues until a stable result is obtained.
Vitafon can be used by women who have gone through a difficult labor that has led to urinary incontinence. Physiotherapy with its use will allow you to recover faster, accelerate the healing of injuries.
Vitafon is used to treat enuresis in children.
Contraindications:
Malignant neoplasms in the affected area.
Infectious diseases in the acute stage.
Pregnancy.
Reviews. Doctors speak of the Vitafon device as an effective device that allows you to get rid of urinary incontinence. However, you should not expect a miracle, so before you start using the device for the treatment of enuresis, you should consult a doctor and find out the causes of incontinence. Reviews of people who have used the device for the treatment of urinary incontinence are mostly positive. Often it is used to get rid of this problem in all family members.

If a woman suffers from stress urinary incontinence, consultation and medical assistance she will need. The fact is that with the help of conservative methods, it is most often not possible to achieve an effect in this type of disease.
Drug treatment is indicated when stress incontinence has mild degree expressiveness, and the muscles and ligaments have not lost their integrity. Medical correction is possible with the following drugs:
Gutron (adrenomimetic). The drug increases the tone of the urethra and sphincter. It is prescribed quite rarely, as it has a negative effect on the condition vascular wall and contributes to high blood pressure.
Ubretide (anticholinesterase drug). Medicine increases muscle tone. It is indicated for those patients who suffer from hypotension of the bladder.
Duloxetine or Cymbalta (antidepressant). The drug helps in 50% of cases, however, it has a negative effect on the digestive tract.
In general, drugs for the treatment of stress urinary incontinence are prescribed infrequently, as they have low efficacy, but a sufficient number of side effects.

Operations are indicated in the case when it is not possible to achieve an effect by other methods of correction of urinary incontinence. Selecting a specific surgical technique depends on features female body, as well as the degree of enuresis.
However, there are general contraindications for any type of transaction, including:
Identified malignant tumor.
Inflammation in the pelvic organs, which is in the acute stage.
Blood clotting disorders.
The following operations are possible:
Sling operations (TVT,TVT-O). These operations are less traumatic and quite effective. During their conduct, a special loop is carried out under the neck of the bladder, which is fixed in the desired position. This loop supports the urethra and prevents urine from flowing out. After such an intervention, the woman recovers very quickly, however, the risk of relapse remains.
Bulk injections. This method of treatment boils down to the fact that a special substance is injected into the urethra, which is designed to fill the deficit of missing soft tissues and maintain the urethra in the desired position. The operation is performed in an outpatient setting and does not require general anesthesia. However, the risk of relapse remains.
Colporrhaphy. This method boils down to the fact that the vagina is sutured with special threads. The procedure is indicated for prolapse of the pelvic organs and has a number of complications. It is possible that a relapse will occur after a few years.
Laparoscopic colposuspension according toBurch. This operation aims to suspend the tissues located around the urethra to inguinal ligaments. The procedure requires the introduction of general anesthesia, has many contraindications and more complications than sling operations. Therefore, colposuspension according to Birch is implemented only when the operation using the loop did not bring the desired effect.

Clover plowed. An herb called plowed clover can be used to treat urinary incontinence. It should be brewed like tea and drunk as a weak solution. This herb can be purchased at a pharmacy.
Honey water. Honey has the ability to retain water. That's why traditional healers use it to treat enuresis. To get rid of urinary incontinence, before going to bed, you should drink half a glass of warm water, in which a teaspoon of honey is first diluted. The course of treatment is 3 days. Alternatively, you can drink 30 ml of honey water three times a day.
Dill seeds for enuresis in children. To save a child from enuresis, you can use the seeds. You will need to take a tablespoon of seeds and pour them with a glass of boiling water, insist for an hour, strain. Use this infusion on an empty stomach. Children under 10 years old are given 1/2 cup each, and children over 10 years old are given a whole glass of drink.
3 effective exercises for urinary incontinence
The following exercises can be used to treat urinary incontinence and should be done every day:
You need to squat down and connect your palms with each other at chest level. The back should be straight. Stay motionless in this position for at least 30 seconds.
It is necessary to lie on your back, spread your knees to the sides, while connecting the feet together. The arms are stretched along the body with palms up. In this position, you need to hold out for a minute.
You need to kneel and lower your buttocks to your feet. Stretch your arms forward, your face should look down. In this position, stretch the spine for a minute.
What to do if you suffer from urinary incontinence?

Drink at least 1.5-2 liters of water without gas per day.
It is important to create your own urination routine. You need to accustom your body to defecate at the same time, for example, in the morning, before leaving the house, at lunchtime and at evening time, upon returning home.
Obesity is not allowed.
All bad habits should be abandoned.
Constipation must not be allowed. To prevent them, you should eat right, consume enough fiber and fluids. Before going to bed, it is recommended to drink a sour-milk drink.
Training the pelvic floor muscles should begin at the stage of pregnancy planning. This will avoid breaks.
You should always try to stay in high spirits and enjoy life.
Education: A diploma in the specialty "Andrology" was obtained after completing residency at the Department of Endoscopic Urology of the RMAPO at the Urological Center of the Central Clinical Hospital No. 1 of Russian Railways (2007). Postgraduate studies were completed here in 2010.
Treatment of urinary incontinence in women is prescribed by a doctor after a preliminary examination and examination. The choice of technique in this case directly depends on the form of the disease, comorbidities and wishes of the patient.
Urinary incontinence (or incontinence) is a pathology that is manifested by involuntary leakage of urine from the urethra. “Not serious” at first glance, the disease has a negative impact on the psychological state of a woman, and also causes her hygienic inconvenience.
Statistics say: urinary incontinence to one degree or another is observed in approximately 35% of the beautiful half of humanity. With age (especially after 40 years), the likelihood of encountering this problem increases.
Why is incontinence a female ailment, and why does it rarely bother men? It's all about the physiology of the woman's body. Hormonal disruptions during menopause, childbirth, pelvic inflammatory disease and "unfeminine" physical activity are often factors that provoke the development of urinary incontinence.
Causes
Urinary incontinence in women can be caused by several reasons:
- Uncontrolled excretion of urine can be a complication of a number of pathologies, as a result of which the normal functioning of the pelvic organs is disrupted. These include: diabetes mellitus, inflammatory diseases of the spinal cord, anomalies in the development of the pelvic organs, tumors, etc.
- Age after 40, when the muscles of the bladder begin to lose their elasticity. This is due to hormonal changes.
- Traumatic injuries of the perineum and ruptures of the pelvic muscles as a result of labor activity. At the same time, urinary incontinence is observed more often in women with a history of two or more births, rapid or long births.
- Hormonal failures as a consequence of the onset of menopause.
- Urinary incontinence can trigger a pregnancy condition. And this happens for two reasons: under the influence of a changed hormonal background, or as a result of the pressure of the uterus on the bladder.
- Surgical operations on the genitals (for example, extirpation of the uterus), in which the integrity of the nerves that control the work of the sphincter and detrusor may be disturbed. As a result - a violation of innervation urinary tract leading to urinary incontinence.
- Work involving heavy lifting.
- Weightlifting, running, jumping, etc.
- Overweight, obesity.
- Diseases of the peripheral part nervous system and the central nervous system, manifested by disorders in the functioning of the pelvic organs (spinal cord injuries, multiple sclerosis, etc.).
- Injuries to the perineum, leading to damage to the nerves that control the process of urination. Urinary incontinence can also be observed when the integrity of the pathways responsible for the excretion of urine is violated.
Classification
There are several forms of urinary incontinence:
- Stress incontinence is a pathological condition in which the involuntary release of urine occurs during sneezing, physical exertion, laughter, etc. This form of the disease is associated with atrophy of the pelvic muscles or cicatricial changes at the site of injury. muscle tissue during childbirth.
- Urgent (imperative) incontinence - involuntary discharge of urine as a result of a sudden urge to urinate. Usually this condition occurs with an overactive bladder or is a symptom of cystitis.
- Paradoxical ischuria is a form of urinary incontinence in which leakage occurs when the bladder is full. It is more common in older men with prostate adenoma.
- Mixed incontinence is a combination of urgency and stress incontinence.
Manifestations of urinary incontinence
This pathology is accompanied by the following symptoms:
- inability to control the process of urination;
- nocturia - excretion of the main daily volume of urine at night;
- complaints about the feeling in the vagina of something extraneous;
- imperative urge - a strong urge to urinate that is difficult to contain;
- involuntary passage of urine when coughing, exertion, sneezing, etc.
Each of the above symptoms gives the patient constant discomfort.
Complications
Urinary incontinence can lead to unpleasant and serious complications, including:
- , urethritis and other infectious lesions of the urinary system;
- dermatitis, diaper rash and other infections skin resulting from constant irritation of the skin by excreted urine.
In addition, constant, uncontrollable leakage of urine does not make it possible to lead an active life: fully engage in sports, relax, work, meet friends.
Diagnostics
The diagnostic methods used for urinary incontinence make it possible to determine the form and severity of the disease, identify the causes, and assess the state of the urinary system. This will allow the doctor to choose an effective method of treatment, resorting to conservative therapy or surgery.
- Clinical examination includes: gynecological examination, history taking to identify all complaints, determine the causes of incontinence. The doctor learns from the woman about everything chronic diseases, surgeries, allergies.
- Laboratory methods: general urinalysis, urine culture for microflora.
- Ultrasound examination - is carried out in order to study the condition of the urethra and genitals of a woman.
- X-ray examination.
- Cystoscopy - examination of the bladder (examination of the internal surface) using a cystoscope.
- Urodynamic study - study functional state lower urinary tract during emptying and filling.
Treatment Methods
Urinary incontinence is treated by a urologist. However, there is no single pattern. It is selected strictly individually after determining the cause of the disease.
Non-drug therapy
The first thing a woman should do is to adjust her lifestyle:
- completely exclude from the diet foods that have a laxative effect on the body;
- during the day to visit the toilet "on schedule" - every 3-4 hours;
- do not use laxative drugs;
- give up alcohol, coffee, stop smoking;
- limit daily fluid intake (no more than 2 liters).
Performing a specially designed set of exercises will help strengthen the pelvic floor muscles involved in the process of urination. Kegel exercises are especially effective if the incontinence is mild or moderate.
Medical therapy
The choice of drugs directly depends on the form of pathology. With urge incontinence, there is an increase in the muscle tone of the bladder. In this case, anticholinergic drugs cholinesterase inhibitors are indicated:
- oxybutin,
- tolterodine,
- solifenacin,
- diclomin hydrochloride.
In the treatment of stress incontinence, when sphincter insufficiency is observed, Gutron is used, which increases the muscle tone of the sphincter of the bladder and distigmine bromide.
With atrophic colpitis, a course is carried out (1.5-2 months) hormonal treatment(estrogen therapy). If urinary incontinence occurs in a patient during menopause, hormone replacement therapy is performed. Strictly prescribed by a doctor hormonal preparations(in tablets, in the form of vaginal gels and ointments).
Surgery
With inefficiency conservative methods treatment indicated surgical intervention. During the operation, excessive mobility of the urethra is eliminated.
Today, the most popular are minimally invasive sling operations using synthetic prostheses - free synthetic loop urethropexy (TVTO, TVT). This procedure does not cause postoperative pain in the patient. pain. And later, the tension of the loop can be adjusted.
Prevention
WHAT DO THE DOCTOR'S SAY?
 Doctor of Medical Sciences, Honored Doctor Russian Federation and honorary member of the Russian Academy of Sciences, Anton Vasiliev:
Doctor of Medical Sciences, Honored Doctor Russian Federation and honorary member of the Russian Academy of Sciences, Anton Vasiliev:
“I have been treating diseases of the genitourinary system for many years. According to the statistics of the Ministry of Health, cystitis in 60% of cases becomes chronic.
The main mistake is tightening! The sooner treatment for cystitis is started, the better. There is a tool that is recommended for self-treatment and prevention of cystitis at home, as many patients do not seek help due to lack of time or shame. This is Ureferon. It is the most versatile. It does not contain synthetic components, its effect is mild, but noticeable after the first day of administration. It relieves inflammation, strengthens the walls of the bladder, its mucosa, and restores general immunity. It suits both women and men. For men there will be nice bonus- increased potency. »
To prevent the development of urinary incontinence, the following recommendations should be followed:
- timely eliminate foci of inflammation in the urinary tract;
- avoid hypothermia, dress according to the season;
- maintain a normal weight;
- do not allow heavy lifting;
- give up alcohol;
- quit smoking;
- limit the consumption of soda, coffee;
- perform special exercises to strengthen the muscles of the pelvic floor.
Conclusion
Urinary incontinence is a condition in the treatment of which you should not rely on your knowledge and traditional medicine recipes. Effective treatment can only be prescribed by a doctor after a preliminary diagnosis. A timely appeal for help to a specialist will allow a woman to get rid of this “trouble” in the shortest possible time and return to a full-fledged active life.