Staphylococcus in a child's nose is a very common infectious disease that is becoming more common every year. The good news is that science has already studied staphylococcus well and can easily cope with the manifestations of infection in children and their parents.
is a very stable and tenacious bacterium; it can retain its abilities and infect humans even in a favorable environment. Bacteria do not die when exposed to sun rays and low temperatures. In drought conditions they can live up to 8 months. Staphylococcus can withstand heating up to 70°C. However, for all its stability, it dies from banal boiling. By treating the products with boiling water, a person will protect himself from this infection. Staphylococcus is sensitive to brilliant green; if you treat a cut with it, you can completely avoid infection. Of course, in the case of an infection that has developed in the nose, brilliant green will not help; more serious drugs are needed here.
I would like to note that staphylococcus is a conditionally pathogenic microorganism; in small quantities, the bacteria do not harm the human body. According to statistics, 70% of the population is infected with staphylococcal infection. Treatment should begin when Staphylococcus aureus becomes the cause of chronic or recurrent inflammatory processes in the body. Most people have a certain amount of infection, as mentioned above, but the bacterium is activated only under the influence of certain factors, such as, for example, a decrease, emotional shock, lack of vitamins or respiratory viral diseases.
Staphylococcus can appear in a child’s throat or nose in several ways:
- contact method of transmission;
- airborne droplets;
- while breastfeeding;
- through the placenta during childbirth;
- due to insufficient food processing.
There are many ways of infection, as can be seen from the above facts, so you should not be careless about this disease and ignore its symptoms.
Symptoms of staphylococcal infection
Staphylococcus in children in the nose has pronounced symptoms, among them the following can be noted:
- dark green nasal discharge, prolonged rhinitis;
- redness of the skin around the nose;
- impaired sense of smell;
- voice changes;
- itching and discomfort in the nose;
- headache;
- increased body temperature;
- the appearance of ulcers if staphylococcus lives in the throat;
- dysfunction of the gastrointestinal tract, which manifests itself in diarrhea, constipation and nausea;
- in hypersensitive children, staphylococcal infection is accompanied by a skin rash;
- abdominal pain, possible intestinal pain;
- decreased blood pressure;
- general weakness and intoxication of the body.

The symptoms are most intense in newborns, since their body has not yet had time to adapt to the influence of the external environment. A baby who has contracted staphylococcus epidermidis sleeps poorly, loses appetite, and is very moody. Parents often confuse this condition in their children with intestinal colic or signs of teeth cutting, thereby complicating the situation. If a parent notices such signs, it is better to visit a doctor who can accurately diagnose. It is much wiser to play it safe and rule out staphylococcal rhinitis or tonsillitis than to deal with its consequences later.
Diagnosis of staphylococcus
In order to begin treatment, a diagnosis is initially required. Many doctors never cease to assert that a correct diagnosis is the key to effective and Get well soon. First of all, the doctor, based on the complaints of the patient or his parents, will conduct a visual examination of the skin. The analysis by which in most cases the presence of infection is diagnosed is bacterial culture on a nutrient medium. A swab is taken from the child’s nose or throat if there is a suspicion that it is located in this part of the body. It is very important to prepare your child. Before taking a smear in the morning, you should not eat or drink tea, you should not use toothpaste or gargle. These seemingly unrelated procedures can affect the reliability of the analysis. Before taking the test, you should not take medications; if they cannot be stopped, you should inform your doctor.
Principles of treatment of staphylococcus in the nose
Few people know how to treat staphylococcus, so when they hear the diagnosis, they begin to panic, but this is not worth doing. Modern pharmacology offers great amount drugs sensitive to this infection. It is important to note that the drug should only be prescribed by the attending physician. It is prohibited to prescribe medications to a child on your own. You should not listen to the advice of friends and neighbors who have encountered similar diagnoses, because the remedies that cured them can harm your baby.

After a detailed diagnosis, the doctor must decide exactly how the treatment will be carried out, and whether antibacterial or sulfonamide medications will be used. The selection of medications is carried out on an individual basis, taking into account the patient’s age, body weight and other characteristics of his body. Most often, to eliminate staphylococcal infections from the nose and throat, the following remedies are chosen:
- Flemoclav;
- Ankomycin;
- Oxacillin;
- Amoxiclav;
- Vancomycin;
- Unazine;
- Clindamycin;
- Erythromycin;
- Azithromycin;
- Cephalothin;
- Cephalexin.
Treatment can be carried out with local means, for example, rinsing the nose using saline solutions Miramistin or Chlorhexidine. An excellent solution would be such as:
- Polydex;
- Isofra;
- Chlorophyllipt;
- Protargol.
If nasal congestion is very severe, then taking vasodilating drops is recommended.
Tetracycline and erythromycin ointments will help relieve pustular lesions of the nasal mucosa. If ulcers large sizes, then the doctor will open them and treat them with antiseptic agents. You cannot delete them yourself. The fact is that the liquid contained in the abscess is precisely the source of staphylococcal infection if it gets on healthy areas skin, it can affect them too. For staphylococcal infections in the throat, frequent gargling with hydrogen peroxide, Furacilin, Miramistin is prescribed.
Treatment will also include general restoratives, since an integrated approach is required to eliminate pathogenic bacteria. Among these drugs are:
- Taktivin;
- Immunorix;
- Poludan;
- Immudon;
- Supradin;
- Alphabet;
- Vitrum.

The use of strengthening agents allows one to increase the patient’s immunity, because as is known, an organism with stable immunity copes better with pathogenic processes. To speed up the action of antibiotics and other medications, you need to eat more foods containing vitamins and beneficial micro- and macroelements. You should also try to reduce physical activity child, let him rest more.
If there is swelling of the wings of the nose and a skin rash, then treatment with antihistamines is required, such as:
- Tavegil;
- Diazolin;
- Zyrtec.
If side effects from the above drugs are observed or they do not produce results, then you must inform your doctor about this, and he will change the treatment regimen.
The duration of treatment and dosage of the drug are prescribed individually by the doctor. Before using the product, it would be a good idea to read the instructions and exclude possible contraindications applications.
Traditional medicine
Staphylococcus aureus can also be eliminated using traditional methods of treatment. Of course, preference must first be given traditional ways, but there are a number of cases when it is not possible to seek qualified help, then home recipes will come to the rescue.
A decoction is prepared from dried chamomile flowers, left for half an hour, and then dropped into the nose. Chamomile is a well-known anti-inflammatory and antiseptic agent, so its use is completely justified.
Dried sage herb is prepared in the same way as chamomile, but the decoction is used to gargle if there are pustules.
Burdock root is crushed and mixed with a small amount of boiled water. The resulting juice and water are placed in the nose, 5 drops every 3 hours.

To gargle, use an alcohol tincture of propolis diluted in boiled water. It allows you to remove the pustular rash and make it easier to swallow with a sore throat.
Compresses are used to eliminate staphylococcus. To do this, they usually use a cotton swab dipped in water diluted with apple cider vinegar. Similar lotions are applied to each nostril for half an hour. According to people who tested the product, the effect will be noticeable after just three uses.
A plant such as aloe has proven itself very well; the juice from this plant not only improves immunity, but also removes staphylococcal infections. You need to instill juice from fresh leaves of the plant 3 times a day. It is important to note that this gives results very quickly, since aloe provokes a sneezing attack in the child. Green clots that interfere with the child’s breathing come out very quickly.
You should not get carried away with traditional medicine, and if it does not give results, then it is better to stop using ancient treatment recipes. Sometimes they can only worsen the child’s well-being and provoke a number of complications, which will be more difficult to deal with than treating the infection itself.
The best effect is achieved when traditional medicine combined with folk. In such a case, the main treatment is synthetic drugs, and as a supplement, general strengthening agents on a natural basis, as traditional medicine advises.
It is strictly forbidden to warm the nose or use hot baths to warm the body. If you apply heat to a sick body, staphylococcus begins to multiply even faster, affecting new areas, because favorable conditions are created for its life. You should not use folk remedies that include honey, sweet fruit juices, dairy products, they also provoke the proliferation of staphylococcus.

You should not insert tampons soaked in alcohol into your child, as pseudocylitologists advise. Bacteria of this group are not at all sensitive to alcohol; such treatment will only irritate the mucous membrane and lead to dry nose and burning.
Like any disease, staphylococcal infection is easier to prevent than to deal with its consequences. As a preventive measure, we can recommend:
- constantly monitor the child’s hand hygiene;
- give food only from clean dishes;
- carefully process food before cooking;
- regularly carry out wet cleaning in the house;
- constantly strengthen the immune system;
- humidify the air, ventilate the rooms where the child is;
- avoid contact with sick people.
Sticking to such simple preventive measures, it will be possible to protect the baby from exposure to bacteria and the development of unpleasant diseases.
Staphylococcus in the nose is not just an unpleasant condition that causes discomfort, but also quite dangerous illness, causing complications. This is the most unpleasant problem that an ENT patient can encounter. It affects the mucous membranes of the nose, and it is almost impossible to completely rid the body of the presence of these bacteria.
Staphylococcal infection: nature and features
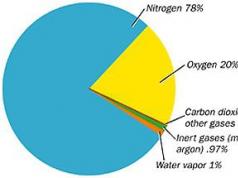
Staph in the nose (staphylococcus aureus) is not such a surprising occurrence. These gram-positive bacteria are found in all types of environments. They can be found in water, soil, air. Bacteria of the Staphylococcaceae family are facultative aerobic. Cocci have many types - up to 30 varieties. Most of them are not dangerous to humans; they are representatives of opportunistic microflora. But some are pathogenic and fraught with danger.
Non-hazardous types of staphylococcus do not cause infections and are often found on the surface of the mucous membrane of the nose and throat. The immune system of a healthy person is able to resist the action of these bacteria. Up to 70% of the world's population periodically become carriers of staphylococcus, and for 20% it will be a constant companion in life.
If the concentration of the pathogen increases and becomes an infection, effective control methods are used. In particular, aqueous solutions of silver salts and liquid compositions containing this substance are used. Antibiotics and a special bacteriophage are also effective. However, there are dangerous pathogenic varieties that are very difficult to combat due to their excessive survivability and resistance to many antibiotics:
- Golden - this pathogen is considered the most dangerous. It can easily affect all tissues human body. Staphylococcus aureus in the nose can lead to a severe inflammatory process with subsequent provocation of pneumonia and even meningitis. It is characterized by increased sensitivity to antibiotics - the use of penicillins and cephalosporins does not give the desired effect, which complicates treatment.
- Saprophytic – less dangerous pathogen compared to the previous one, but it always leads to severe infectious diseases organs genitourinary system. Its consequences are cystitis and urethritis.
- Epidermal - is a frequent guest on the mucous membranes and skin. It can be found in the mouth, nasal passages, and eyes. Children are especially susceptible to its effects. The result of infection is conjunctivitis, infection open wounds, damage to the genitourinary system. Also, pathogenic staphylococcus provokes severe infection of the bloodstream and endocarditis.
The severity of damage by staphylococci is determined by the fact that, having settled in the body in excessive quantities, they begin to produce a number of enzyme components and toxins. They actively destroy cells and provoke other ailments.
Causes and methods of transmission
Staphylococcus aureus in the nasopharynx will begin to actively develop only if certain conditions coincide:
- a sharp increase in the number of bacteria in the body and exceeding the threshold level, after which the immune system cannot resist microbes;
- falling protective barriers immune system body;
- the formation of wounds, scratches, damage to the mucous membrane, through which the infection begins to penetrate.
How is the infection transmitted?
You can become infected with staphylococcus in any conditions. All people are susceptible to it, regardless of age. The main routes of entry of the pathogen include:

Provoking factors
Staphylococcus aureus (aureus) can penetrate through the consumption of unwashed food, through wounds, due to the “revival” of the pathogen located in the intestines. Factors that provoke infection are:
- Hypothermia of the body, because when cold air passes through the nose, the cilia of the epithelium freeze. The lack of their movement reduces the quality of cleansing of the nasal cavity, which leads to the settling of bacteria on the mucous membranes and their active development.
- Respiratory infections and influenza provoke rhinitis of the staphylococcal type, which leads to a decrease in immune defense.
- Excessively long-term use of nasal drops with a vasoconstrictor effect causes drug-induced rhinitis. It facilitates the penetration and proliferation of bacteria.
- Uncontrolled use of antibiotics, abuse of cytostatics and corticosteroids causes hypersensitivity of the body to staphylococcus.
- Staph infections in the nose may affect certain populations at higher rates. This applies to newborns, children, older people, and patients with chronic illnesses.
- Increased activity in foci of infection - infection may result from chronic tonsillitis, pharyngitis or adenoiditis.
- Mental stress and long-term stressful situations.
Symptoms of infection
The appearance of a staphylococcal infection requires immediate treatment in adults and children. This is especially true for severe cases with damage from the golden type of pathogen. Signs of staphylococcus in the nose are as follows:

A feature of staphylococcal infection in children is the presence of a rash on the body. Rashes in the form of pustules, as well as the discharge of pus, leading to the formation of crusts, require prompt medical intervention.
Scratching or otherwise disturbing wounds in the affected areas leads to the transfer of infection to other parts of the body.
Why is staphylococcus in the nose dangerous?
When infected with staphylococcus, inflammation can quickly turn to Airways, organs located in close proximity to the source of infection. The sinuses and larynx are affected, the tonsils and trachea are affected. The infection can spread to the lungs or heart.
An ordinary runny nose, which is often ignored, can develop into a sore throat, otitis media or sinusitis in a matter of days. In severe cases, bronchitis or tracheitis may be provoked. Certain categories of patients are at risk: infants and the elderly. It is in them that staphylococcal infection can cause abscesses, serious disruption of the lungs, damage to the bone structure, brain and heart. The spread of infection to the kidneys and liver is also dangerous. Cases of septic-type blood infection should not be excluded.
Staphylococcus aureus is extremely tenacious. It is not easy to get rid of it even with the help of powerful medications - it is poorly susceptible to penicillins. This feature requires timely initiation of hospital treatment and an antibiogram.
Diagnostic specifics
Staphylococcus aureus in the nose in adults is not so easy to diagnose, as a more in-depth examination is required. After a general examination of the patient by an ENT specialist, the following types of studies are prescribed:
How to treat staphylococcus in the nose
The therapeutic intervention program is prescribed by specialists on an individual basis, taking into account the characteristics of the clinical case. The typical parameters of the infectious agent, the patient’s condition and the development of the disease are taken into account, and the potential effectiveness of the use of medications is assessed.
In case of infection without complications, the method of symptomatic therapeutic treatment is used, but in severe forms it is required complex treatment with the use of drugs that have a general antibacterial or specific antistaphylococcal effect.
Antibiotic therapy
For each clinical picture patients require individual program treatment, because there are no universal ways to combat it. This is explained by the presence of specific sets of pathogens in people susceptible to this infection. The selection of an antibiotic is made based on the results of the antibiogram. The doctor forms the course and dosage. You cannot deviate from them - incomplete cure is fraught with the transition of the disease to chronic form. In this case, the slightest action of the provoking factor will intensify the disease.
Staphylococcus in the nose of an adult, if the pathogen is not of the aureus type, can be treated with antibiotics belonging to the penicillin class. For example, doctors often prescribe Ampicillin.
Staphylococcus aureus is very insidious - it has developed resistance to penicillin drugs. These medications will not help cure the infection. Risk self-treatment due to the possibility of provoking pneumonia with these drugs. There is a risk of sepsis of staphylococcal origin and osteomyelitis.
Sulfonamide drugs and some antibiotics will help destroy Staphylococcus aureus bacteria. The following drugs provide high effectiveness of therapy:
If severe purulent formations are observed, then drugs of this class of antibiotics can be used to treat areas where open ulcers are located.
During the therapy, emphasis is placed on components that can suppress the action of microbes and overcome their resistance to medications. The dosage is determined by a specialist individually. In cases where it is impossible to adjust pathological changes in the nose due to the use of antibiotics, a decision is made to introduce immunoglobulin with an antistaphylococcal effect or toxoid into the course of therapy. These medications will help prevent complications.
Local treatment of affected areas
To rinse the nasal cavity, medications with an antiseptic effect are prescribed - Miramistin or Chlorhexidine. In the process of complex therapy, a combination of vasoconstrictor and antibacterial effects is often required. Effectiveness is demonstrated by nasal instillation:
- Protargol;
- Polydexa;
- Isophroy.
It is also advisable to rinse your nose with a solution of Chlorophyllipt or use drops of an oil consistency based on this drug. Mupirocin anti-staphylococcus ointment is used twice a day as prescribed by a doctor.
It is recommended to introduce immunomodulators into the course of therapy. They are applied topically. These drugs include IRS-19 or Immudon. Sanitation of the nasopharynx with a special bacteriophage is effective - tampons are moistened in it and left for 15-20 minutes. inserted into the passages of the nose. Bacteriophage should not be used simultaneously with alcohol-based Chlorophyllipt due to the risk of mutual neutralization.
Treatment of the nasopharynx is also provided through the use of lozenges, for example Lizobakt. These products help to have a positive effect on the condition of the throat, which is additionally gargled with Miramistin, Chlorophyllipt, soda or hydrogen peroxide in solution.
Folk recipes
Treatment of staphylococcus is carried out by taking medications prescribed by specialists. Do not refuse or skip doses. But in addition to the developed therapy program, you can use folk remedies that will alleviate the patient’s condition.
Treatment will help remove staphylococcal infection from the nasopharynx folk remedies:
- Herbal infusion, for which you need to take sage with plantain and burdock root. You can put it in your nose or use it to gargle.
- It is recommended to eat 2 apricots before meals, the pulp of which is natural antibiotic from such a disease as staphylococcus.
- Prepare an infusion from natural ingredients - walnut leaves, tricolor violet root and wheatgrass. After standing for 2 hours in a dark place, drink 0.5 cups of the product in between meals.
- Consume foods rich in copper, which has an antiseptic effect, within the daily norm of 2 mg. Spinach, buckwheat or salad are suitable for treatment at home.
Treatment rules in special cases
Treatment of staphylococcal infections in pregnant women has its own specifics. Firstly, most antibiotics should not be used during this period. Secondly, there is a huge risk of transmitting the infection to the baby during intrauterine development, during childbirth or during breastfeeding. This necessitates a very attentive attitude to women's health.
During the treatment process, drugs are prescribed that do not have the ability to pass through the placenta or do not have a teratogenic effect on the unborn child. The course of treatment includes bacteriophages and immunomodulators. The procedure for immunizing a woman with staphylococcal type antitoxins is also recommended. It is also acceptable to use relatively safe products such as Chlorophyllipt.
Staphylococcal infection is the result of weak immunity, so a pregnant woman should eat well, lead a healthy lifestyle, walk more and avoid stress.
Detecting an infection in a child is fraught with many complications, so prompt consultation with a doctor is required. The specialist prescribes gentle antibiotics, folk remedies, vitamin complexes and immunomodulators. Treating the affected areas with Chlorophyllipt is suitable. A feature of the treatment of this category of patients is the need for all family members to undergo tests and, if necessary, undergo complex therapy.
Prevention means
 When diagnosing a staphylococcal infection, you must strictly follow your doctor's recommendations. Warming procedures that contribute to the spread of germs are not allowed. You should not consume milk and dairy dishes; you should exclude honey and juices from your diet. Alcohol solutions must be used carefully - they may not have the desired effect and will lead to increased dryness of the mucous membrane. After taking antibiotics, it is advisable to undergo a course of therapy using probiotics.
When diagnosing a staphylococcal infection, you must strictly follow your doctor's recommendations. Warming procedures that contribute to the spread of germs are not allowed. You should not consume milk and dairy dishes; you should exclude honey and juices from your diet. Alcohol solutions must be used carefully - they may not have the desired effect and will lead to increased dryness of the mucous membrane. After taking antibiotics, it is advisable to undergo a course of therapy using probiotics.
However, it is important to prevent the disease from activating, for which a set of preventive measures should be implemented:
- compliance with hygiene rules, avoiding the use of other people's objects;
- active pastime, increased immunity;
- avoiding stress;
- treatment of runny noses only with medications prescribed by a specialist;
- ventilation of the room and wet cleaning;
- maintaining hygiene when feeding your baby.
Staphylococcal infection is a very complex and dangerous disease. The situation should not be underestimated. It is important to quickly consult a doctor and promptly begin therapy. This is especially true for risk groups that are susceptible to complications.
Staphylococcus is an opportunistic bacterium, which, when immunity is weakened, can lead to a number of serious diseases. As long as a person is healthy, staphylococcus is not dangerous for him, and he may not even suspect that he is a carrier of this bacterium. But during exacerbation chronic diseases, colds, after injuries and operations, staphylococcus begins to actively manifest itself. Therefore, it is important to know the symptoms of staphylococcus in the nose in order to identify it in time and take measures to quickly eliminate it.
Risk factors
Anyone can become infected with staphylococcus. It is enough to touch the surface on which the bacteria is located with your hands, and then any open area of skin. It spreads no less easily through airborne droplets. Therefore, it is almost impossible to get rid of this bacterium. She is a permanent resident of public catering establishments, toilets, hospitals and child care institutions.
The risk of contracting an infection increases significantly if:
failure to comply with basic hygiene rules; weakened immune system; vitamin deficiency and insufficient amounts of minerals and trace elements; frequent or chronic respiratory diseases; long-term use of vasoconstrictor nasal drops; long history of smoking; unreasonable use of antibiotics; looseness or inflammation of the mucous membranes of the nose; scratches, injuries and other damage to the skin.
There is a high probability of infection during medical procedures and manipulations with poor sterility or dirty hands. Children are especially easily infected with staphylococcus, since their immunity is not yet developed enough to resist the bacteria, and their skin and mucous membranes are very delicate and sensitive.
Main symptoms
The easiest place for staphylococcus to end up in the nasal cavity. You can bring it there with unwashed hands, simply inhale the saliva of a person sneezing or coughing nearby, etc. The mucous lining of the nasal passages is very delicate and constantly moisturized, which creates almost ideal conditions for the active proliferation of bacteria.
Staphylococcus in the nose usually manifests itself with the following symptoms:
redness, inflammation, sometimes swelling of the mucous membrane; slight persistent increase in body temperature; increased secretion mucus from the nose, often purulent runny nose; weakness, dizziness, nausea and other signs of intoxication; multiple small pustular rashes on the mucous membrane and skin of the nose.
If the nasopharynx is affected, a purulent sore throat can quickly develop, which will give a sharp rise in temperature, sore throat, and severe cough. When it gets into the nasal sinuses, sinusitis, sinusitis, and otitis media are added to the overall picture.
Sometimes the first symptoms of staphylococcus in the nasal cavity are not pronounced and are easy to miss. And the disease is detected only when the respiratory symptoms for some time do not respond to conventional treatment. This can complicate the situation, since during this time staphylococcus actively increases its numbers and spreads further and further.
Possible complications
The main danger is that, having settled into the body and actively developing, staphylococcus is not limited to the internal cavity. It spreads further along the mucous membrane, affects the nasopharynx, larynx and reaches the internal organs. Therefore, in the absence of treatment or the use of the wrong drugs, very serious complications can occur:
Gastrointestinal disorders. Accompanied loose stools(leads to dysbacteriosis and dehydration), complete lack of appetite, frequent vomiting, constant nausea, are not uncommon severe pain in the abdominal area. Skin diseases: inflammation of the hair follicles, dermatitis, eczema. Purulent pimples, boils, and carbuncles appear on the affected areas of the skin, not individually, but in whole groups. Pneumonia. Fortunately, it rarely develops, more often in children or adults who are weakened after surgery or have previously suffered serious illnesses. If not noticed in time, purulent pneumonia and obstructive syndrome are possible. ENT diseases. Getting staphylococcus into the sinuses or eustachian tube can provoke purulent sinusitis, frontal sinusitis, chronic rhinitis, otitis. At the same time, there is severe inflammation and swelling of the nasal mucosa. Staphylococcal endocarditis. Serious heart disease that can cause very severe damage to the heart and brain and even fatal outcome. Ritter's disease. These complications are also more common in children, since their skin is more delicate and thin and is easily affected by bacteria. The disease manifests itself by the appearance of clearly defined red spots on the body. Toxic shock. It occurs only in patients with severely weakened immunity due to poisoning of the entire body with toxins produced by staphylococcus. It looks like very severe poisoning: a sharp increase in temperature, severe vomiting, weakness, loss of consciousness, drop in blood pressure.
Curing such complications is much more difficult than neutralizing staphylococcus at an early stage. The situation is worsened by the fact that serious damage to internal organs and severe inflammatory processes reduce immunity, and this, in turn, contributes to the further proliferation of staphylococci.
Therefore, if there is even a suspicion of the presence of this bacterium in the body, it is necessary to immediately get tested and begin active treatment.
Diagnostic methods
Staphylococcus is not a diagnosis that can be made by eye. The only way to detect it is a laboratory test of nasal mucus taken for analysis. The sample is placed under sterile conditions in a clean nutrient medium, where ideal conditions are created for unhindered reproduction. This test is called bacterial culture.
After about a day, the sample is carefully examined under a microscope, and a specialist can determine: the type of staphylococcus, the growth rate of the colony, the degree of damage, and also test the strain for resistance to various antibacterial drugs. Based on this analysis, the doctor will choose the most effective treatment method.
Unfortunately, quite often staphylococcus in the nose does not show typical symptoms, but still affects internal organs and provokes the development of diseases. In this case, it can only be detected by chance or when the concomitant disease does not respond to treatment for a long time, and the doctor decides to test the patient for staphylococcus.
In some cases, a blood test can help identify staphylococcus, in which a certain type of antibody can be detected. You can suspect his presence if general analysis blood indicates a greatly reduced immunity, and purulent rashes periodically appear on the skin and nose.
Treatment options
There are two main ways to treat staphylococcus - this is a course antibacterial therapy or staphylococcal bacteriophage. Which of them is most effective in this case can only be decided by a doctor based on the results of the examination. Antibiotics can cause an allergic reaction and have a number of contraindications, but they are guaranteed to cope with the bacteria.
Staphylococcal bacteriophage is essentially a temporary vaccination against staphylococcus. It is a liquid in which microorganisms hostile to bacteria are present. They destroy pathogenic bacteria while dying themselves. There are no contraindications to this drug. But for some time it can increase the symptoms of general intoxication.
At the same time, be sure to take medications to strengthen the immune system. These can be plant extracts: echinacea, eleutherococcus, ginseng or special preparations: “Immunal”, “Immunex”, etc. Avitaminosis can significantly slow down the healing process, so it is advisable to drink a good multivitamin complex at the same time.
The external manifestations of staphylococcus also need to be combated in order to prevent its spread to other areas of the skin and mucous membranes. It is insensitive to alcohol solutions and hydrogen peroxide. But chlorophyllipt copes well with it, both oil and alcohol based.
The second worst enemy of staphylococcus is ordinary brilliant green, which should be applied to the affected areas 2-3 times a day. It quickly dries out the pustules and prevents the disease from progressing further.
It is very important to complete your treatment. This means that the doctor’s orders must be followed until a repeat analysis shows that the problem has been completely eliminated. Otherwise, the remaining microorganisms will adapt to the drugs used and will stop responding to them. And at the next exacerbation it will be much more difficult to fight them.
Preventive measures
No amount of prevention can completely guarantee that you will not become infected with one of the types of staphylococcus. As already mentioned, this bacterium is very tenacious, and creating conditions close to sterile in everyday life is simply unrealistic, and even unnecessary, since many beneficial microorganisms live on our skin and mucous membranes.
Therefore, preventive measures should be aimed primarily not at avoiding infection, but at strengthening the body and giving it the ability to independently restrain the proliferation of pathogenic microflora. This means that all efforts must be directed towards:
Strengthening the immune system. Of course, not in the acute stage of staphylococcus or chronic diseases. An active lifestyle, sports, hardening procedures will help with this. cold and hot shower, swimming. Healing from chronic diseases. Any chronic disease greatly weakens the body’s immune defense, which means that it is easier for any infection to harm the body. Therefore, not only staphylococcus can provoke a chronic disease, but the disease can also create conditions for the proliferation of staphylococcus. Proper Use household chemicals. Nowadays, many people are addicted to strong household chemicals. Of course, they greatly facilitate the process of cleaning the room, but at the same time they kill not only pathogenic, but also beneficial microorganisms, weakening the natural protection of the skin. Therefore, you need to work with them with gloves and use them sparingly. Maintaining hygiene rules. You should always wash your hands before eating and after using the toilet, not just in public places. It is advisable to always have antibacterial wet wipes or a pocket bottle of antiseptic with you and use them if necessary. Proper storage and processing of products. Staphylococcus from the surface of unwashed vegetables and fruits can get not only into the stomach, but also end up first on the hands, and then in the nose, mouth, and throat. Therefore, in the hot season, it is advisable not only to wash them, but also to pour boiling water over them, in which the bacteria die instantly. Timely consultation with a doctor. Contact for medical care It is necessary as soon as you have discovered signs in yourself that allow you to suspect the presence of pathogenic bacteria, and not when you have already tried to treat them yourself and failed. As a last resort, immediately tell the doctor how you acted, so that he understands which treatment methods will no longer be effective. Rejection of bad habits. Smoking tobacco, alcohol abuse, and the use of narcotic drugs systematically poison the body and weaken the immune system. And smoking also loosens and thins the nasal mucosa, facilitating the penetration of pathogens.
Remember that staphylococcus lives in the nose in 9 out of 10 adults. This is only an opportunistic bacterium that can do a lot of harm. healthy person I just can't. Therefore, a healthy lifestyle and strong immunity - best protection from staphylococcus and the complications caused by it.
Often people turn to ENT specialists with complaints of discomfort in the nose or throat, and after a series of tests and studies, staphylococcus may be detected in their nose.
This is a bacterium that is called the "killer" for the reasons that it hides very well and is very difficult to destroy. What is it, what danger does it pose and what specific symptoms are this infection characterized by?
What is staphylococcus in the nose: symptoms
Almost all staphylococci, with the exception of Staphylococcus aureus, are gram-positive opportunistic bacteria, that is, those which are constantly present on the mucous membranes and skin of humans, but cause the development of diseases only when favorable conditions are created for their reproduction.
In general, there are more than 20 types of staphylococci, but the most common are:
Epidermal. Such microorganisms prefer to live exclusively in a humid environment, so they mainly affect the epidermis (upper layer of skin and mucous membranes) of the genital and ENT organs.
Saprophytic. The bacterium usually settles in the organs of the genitourinary system.
Hemolytic. It differs from other representatives of the class in that its virulence (ability to cause diseases) increases when it penetrates the blood.
Staphylococcus aureus or, as is often called, golden staphylococcus (Staphylococcus aureus). Most dangerous representative this group of bacteria, since it is capable of causing the development of extremely life-threatening diseases. Its favorite habitat is the mucous membranes of the nasal cavity, from where it eventually penetrates the bloodstream and spreads throughout the body.
You can get infected with them absolutely everywhere: at home, on the street, in hospitals, in public places, etc., because there are a lot of ways in which the bacteria are transmitted. These are airborne, contact-household, and oral routes of infection.
However, it is difficult to call this an infection, since staphylococci in larger or smaller quantities constantly live in the body of every person, and for the first time settle on the mucous membranes and skin literally immediately after birth.
Therefore, a staphylococcal infection in the nose is diagnosed only when the number of microorganisms exceeds the norm, which is observed against the background of a weakened immune system. This may result in:
sore throat; pharyngitis; tonsillitis; stomatitis; gingivitis; sinusitis, etc.
Most often, the reasons for this lie in:
weakened immunity due to various diseases; stress; poor nutrition; untimely treatment of teeth affected by caries; long-term use of vasoconstrictor sprays, corticosteroids, cytostatics, etc. Thus, there are a lot of factors that contribute to what causes staphylococcal infection. In addition, due to physiological characteristics and a natural decrease in immunity, the following are often hostages of these bacteria: pregnant women; aged people; children; people suffering from immunodeficiencies; patients who have undergone chemotherapy; patients undergoing long-term treatment in hospitals.
During their life, bacteria produce toxins and enzymes that poison the body and destroy cells. Moreover, how the disease manifests itself directly depends on the specific type of bacteria that has managed to multiply and infect the ENT organs.
Staphylococcus aureus makes itself felt most clearly, however, the main signs of infection are:
formation of purulent wounds in the nose area (not always); prolonged persistence of elevated body temperature; congestion; redness of the mucous membrane in the nasopharynx; persistent runny nose that cannot be treated traditional means; nausea, vomiting, headaches, that is, signs of poisoning.
Despite the seeming harmlessness of the manifestations of staphylococcal infection, it cannot be ignored, because it can lead to the development of:
chronic sinusitis; meningitis; pneumonia; phlegmon; sepsis, etc. Therefore, when identifying an excessive number of staphylococci, it is necessary to remember how dangerous the microbe is, and start treatment immediately, which will be aimed at eliminating the cause of its increase and eliminating signs of malaise.
At the same time, any self-medication is unacceptable, since it can significantly aggravate the situation and provoke the development of resistance in pathogenic microorganisms to most modern drugs. Then it will be much more difficult to cope with the infection.
To diagnose the disease, a swab is taken from the throat and nose for the presence of pathogenic staphylococcus, and a blood test is also performed. There is no need to be afraid of the research, because the way samples are taken does not provide the patient with any pain.
For this purpose sterile cotton swab carried out along the internal surfaces of the nasopharynx. The rinsing from it is sown on nutrient media, that is, an in vitro analysis is carried out (in a test tube).
After several days, the grown colonies are assessed by the nature of the edges and surface, size, color and quantity, since each type of microorganism is characterized by the formation of colonies with strictly defined parameters.
It is worth noting
If a culture from the throat and nose shows staphylococcus, laboratory assistants immediately assess the sensitivity of the detected microorganisms to various antibiotics.
This is extremely important, because today, due to the frequent and unreasonable use antibacterial drugs Many pathogens are resistant to them.
Therefore, if staphylococcus is found, the study allows you to immediately determine which medicine will give the maximum result in each specific case.
Thus, how the infection is treated is determined individually in each individual case. Moreover, therapy is started only when the normal indicators number of microorganisms, and the norm of staphylococcus in the nose is 10 to 3 degrees.
But this is true for all types of these microorganisms, except Staphylococcus aureus. If it is detected, even in minimal quantities, treatment begins immediately.
Let us note once again that any self-medication is unacceptable because:
bacteria quickly become insensitive to the action of antibiotics; incorrect dose selection and untimely interruption of the course of antibiotic therapy leads to the development of resistance in microbes; an irrational choice of drug will entail the suppression of other types of microorganisms that inhibit the proliferation of staphylococci, which will result in their active reproduction; an erroneous combination of medications leads to the development of complications, intoxication, etc.
Therefore, only a competent specialist can decide how to get rid of a staphylococcal infection.
In the vast majority of cases, treatment is carried out at home. Hospitalization is required only in extreme, very severe cases, when, due to the lack of timely intervention, microorganisms have affected internal organs.
Patients are prescribed:
Antibiotics. These medications destroy all microorganisms sensitive to them. To suppress staphylococcal infections, agents based on:
amoxicillin (Amoxiclav, Flemoxin, Augmentin) ceftriaxone (Sulbatomax, Blitsef, Tercef, Medakson), neomycin (Actilin, Neomin, Sofrana, Mycerin), erythromycin (Eritrocin, Eracin, Ilozon), vancomycin (Vankoled, Vanmiksan), azithromycin (Sumamed, Azitral, Hemomycin), cephalexin (Ospexin, Keflex, Flexin) and their combinations.
In the presence of a pustular rash, ointments with antibiotics are prescribed: erythromycin, tetracycline, Bactroban, Fusiderm, Baneocin and others.
In mild forms of sinusitis and some other isolated lesions of the nose and throat, drops with antibacterial compounds can come to the rescue. local application: Bioparox, Isofra, Polydexa.
Sulfonamide drugs. The main task of drugs in this group is to suppress the growth and reproduction of various bacteria. Therefore, patients are advised to take Ofloxacin and Unazine.
Gargles and nasal drops for staphylococcus. There are no specific pharmaceuticals in the form of nasal drops to eliminate these microbes. Nevertheless, many otolaryngologists recommend that their patients instill oil solution chlorophyllipt or vitamin A.
You can also often find advice to rinse with solutions of Miramistin or Chlorhexidine, as well as an alcohol solution of chlorophyllipt.
If the oral cavity is affected, rinsing with these medications or furatsilin solution, propolis tincture and herbal decoctions is recommended.
Immunomodulators. Medicines such as Immunorix, Taktivin, IRS-19, Immudon and others are designed to activate the body’s own defense mechanisms and thereby speed up the healing process.
Antiallergic drugs. Prescribed to eliminate swelling and prevent the development of allergic reactions to other medications used. These include Zyrtec, Erius, Diazolin, Loratadine and others.
Vitamin and mineral complexes. The purpose of these drugs is to eliminate the deficiency necessary for the body substances and increased immunity. Most often, patients are advised to take Alphabet and Supradin due to their high bioavailability and rich composition.
Folk remedies
It is very important for patients to drink a lot of water so that waste products and decay of microbes do not poison the body.
In some cases, patients are prescribed probiotics, for example, Bifiform, Linex, Lactovita Forte and others, to restore the normal composition of the intestinal microflora.
But there is still heated debate about the advisability of using these drugs. Some doctors consider them useless, since almost all beneficial microorganisms die in the aggressive environment of the stomach, and the remaining ones are unable to take root on the intestinal walls.
Other experts are confident that special capsule shells protect bacteria from the action of hydrochloric acid, allowing the release of the contents dosage form occurs precisely in the intestines and beneficial microbes quickly take root.
Patients are strictly prohibited from performing any warming procedures, since local thermal exposure promotes even more active growth of bacteria and their spread.
Therefore, applying, on the advice of loved ones and relatives, bags of salt, eggs and other heated objects can become cause the development of life-threatening complications.
You should not expect that therapy will lead to the complete destruction of microbes. This is only required if Staphylococcus aureus is detected.
In mild cases, 3-4 weeks are enough to normalize the number of microorganisms on the mucous membranes of the ENT organs, and all symptoms of infection usually disappear within 7 days, but the course cannot be interrupted at this point.
For the remaining 2–3 weeks, you should regularly take the medications prescribed by your doctor to consolidate the results achieved and prevent a relapse of the disease.
During the entire treatment period, a nasal test for staphylococcus is performed several times in order to monitor its effectiveness and, if necessary, make timely adjustments to the prescription.
Diet
Oddly enough, the success of the therapeutic measures largely depends on proper nutrition. It is known that simple carbohydrates are necessary for the growth and reproduction of bacteria, so for the entire duration of treatment it is necessary to completely abandon:
sweets, including chocolate and confectionery; carbonated drinks; fast food; ready-made breakfast cereals, etc.
all kinds of cereals; whole wheat bread; lots of fresh vegetables and fruits; greenery.
Otherwise, the patients’ diet does not require correction.
Folk remedies
Cure the disease with strength traditional medicine impossible. Any such attempts can lead to the development of complications due to the uncontrollably rapid proliferation of pathogenic microflora.
Nevertheless, with the permission of the otolaryngologist, the following folk remedies can be used as auxiliary measures:
Rose hip decoction. It is drunk twice a day, 100 ml.
A decoction of echinacea and burdock roots. Plant materials are crushed, 2 tsp. Brew the resulting powder in 4 cups of boiling water and cook over low heat for 10 minutes. The decoction is taken 200 ml three times a day.
Birch buds, string grass, yarrow, wild rosemary and thyme are taken in equal quantities. 1 tbsp. l. The resulting mixture is poured with two glasses of boiling water and left for a couple of hours. The finished infusion is taken ½ cup 4 times a day.
Daily use is also believed to have a beneficial effect on the speed of recovery. eating 100 g of black currant and 0.5 kg of apricot.
If a microorganism is detected, especially if it has already managed to provoke the occurrence of certain pathologies, you should as soon as possible contact your doctor to develop the optimal treatment regimen.
Considering the question of how to remove the infection in each individual case, the specialist will prescribe a number of medications from those listed above, recommend sticking to a diet and recommend folk remedies that are suitable for the case.
also in mandatory Symptomatic therapy is carried out, the nature of which directly depends on what pathology has developed and what symptoms it is accompanied by.
In severe cases, the use of bacteriophages may be necessary. They are specific viruses that are active against certain types of bacteria. The bacteriophage penetrates the staphylococcus cell and destroys it from the inside, without causing any harm to human tissue.
If an increase in the number of bacteria leads to the formation of large pustules on the mucous membranes of the mouth and nasal cavity, the doctor may decide to open them.
In such cases, the procedure is performed under local anesthesia. Each element of the rash is incised, the contents are carefully removed and washed with a solution of an antibiotic selected based on the results of bacterial culture.
The most dangerous infection is for babies in the first year of life, since due to their weak immunity, infection can lead to rheumatic changes in the body, in particular, damage to the heart and joints, as well as “scalded baby” syndrome, in which the upper layers of the skin peel off.
Therefore, if an increased number of staphylococci is detected in a baby, treatment should be started immediately, but you should be prepared for the fact that it will be long. As a rule, therapy takes 3 months, during which several breaks in taking medications are taken for up to 6 days.
Information for your information
In such situations, all family members must be examined for carriage of staphylococcal infection, and if the source of infection is identified, both him and the child are treated simultaneously.
But how to treat the disease should be decided solely by the doctor, based on the research data obtained.
If the mouth is affected in children, especially small ones, it is not possible to rinse. Therefore, they are often replaced by wiping the mucous membranes with gauze soaked in an antiseptic solution chosen by the doctor.
Otherwise, treatment is carried out according to the same scheme as in adults, but with drugs appropriate to the child’s age. In severe cases, as well as when Staphylococcus aureus is detected in an infant, patients must be hospitalized.
All women registered for pregnancy are prescribed a smear test for staphylococcus.
Detection of an increased content of microorganisms is a reason to begin full-fledged treatment, since the toxins released by bacteria can negatively affect the condition of the fetus.
But at the same time, each medicine for expectant mothers is selected with special scrupulousness, Moreover, they try to give preference to products for topical use.
Since the main reason why opportunistic microflora is activated in pregnant women is a decrease in immunity, they are always advised to:
walk more in the fresh air; take vitamins; eat well.
Thus, there are a lot of reasons why fungus appears in the nose, but at the same time it is not possible to talk about whether it is contagious. After all, every person can be a carrier of one or another type of this bacterium, without even realizing it.
In each individual case, how to cure the infection should be decided individually, and the choice of tactics and direction of therapy should be trusted only to a qualified ENT specialist, so as not to aggravate the current situation.
ratings, average:
About 70% of all inhabitants of the Earth are carriers of staphylococci. Currently, 27 varieties of these bacteria are known, and 14 of them are always found on human skin or mucous membranes.
Location of the pathogenic environment
Staphylococcus is quite common in the nose and throat. Treatment must be comprehensive. But it is important to pay attention not to the very fact of the presence of these microorganisms, but to their concentration. It is also necessary to look at which type of staphylococcus is most active. In addition, this microorganism is always located in the intestines. When diagnosing, it is necessary to look at the detected number of bacteria.
With the development of a staphylococcal infection in the throat, diseases such as sore throat, gingivitis, stomatitis and others may appear. An excessive amount of bacteria in the nose leads to nasal congestion and a constant runny nose. Also, such a lesion may be characterized by general malaise.
Symptoms of infection development
In many cases, people don't even know they have staph. Reviews from ordinary patients indicate that only after special examinations was it possible to identify this bacterium. But there are certain external signs, indicating that a staphylococcal infection is developing in the body. Such manifestations include:
- unreasonable elevated body temperature;
- the appearance of ulcers, pimples, ulcers on the skin;
- flatulence;
- abdominal pain, dysfunction of the digestive system;
- appearance of signs of general intoxication of the body.
However, it is not necessary to have all the symptoms to suspect that staphylococcus has appeared in the nose and throat. Treatment should be prescribed after the examination. In some cases, the disease may be asymptomatic. But this does not always mean that there are no problems. For example, if Staphylococcus aureus is detected, treatment will be mandatory.
Signs of bacterial growth in the nose and throat
You can understand that you have begun to develop a staphylococcal infection by a number of signs. But in most cases, people do not even suspect that they do not just have a lingering runny nose, but are infected with the staphylococcus bacteria. A photo of this microorganism, which looks like a bunch of grapes, does not convey the full danger.
Signs of staphylococcus in the nose include:
- persistent runny nose;
- temperature increase;
- manifestations of general intoxication.
If a test for staphylococcus shows that the microorganism has infected the throat, then the following symptoms may be present:
- discomfort and pain in the throat area;
- swelling of the tonsils, their redness, the appearance of pustules or purulent plaque;
- temperature increase;
- increase lymph nodes;
- intoxication.
Staphylococcus aureus is considered one of the most dangerous. It causes pustules to appear on the skin. Children often develop a rash. If such a staphylococcal infection is not treated, then damage to other organs and systems will begin. Malfunctions in the gastrointestinal tract appear, they manifest themselves in the form of abdominal pain and flatulence. At the same time, children's bodies are the least protected. The staphylococcus bacteria spreads faster throughout their body, causing the development of various inflammatory processes in organs and tissues.
It is customary to distinguish four degrees of staphylococcus. Moreover, each of them is characterized by a certain degree of activity and requires different treatment. It is necessary to distinguish between staphylococci that are definitely pathogenic, which are destructive to blood cells, and opportunistic, which contribute to the development of a minor inflammatory reaction. In addition, there are also saprophytes that cause virtually no damage.
Routes of infection
There are several ways a staph infection can get into your body. One of the most common is the contact-household route. Therefore, you need to be careful about hygiene issues. Even minor scratches or splinters must be treated with bactericidal disinfectants.
It is also worth knowing that Staphylococcus aureus is also transmitted through stale food (see photo below).
We must not forget that this bacterium is part of the normal microflora. But with a decrease in immunity, it can begin to become more active and lead to serious illnesses. Even the seemingly harmless habit of licking your lips on the street is a risk factor. The risk of infection with pathogenic staphylococcus also increases in those who are accustomed to biting their nails.
But this bacterium is most dangerous for HIV-infected people and cancer patients. The defenses of their bodies are noticeably reduced, so staphylococcus does not encounter barriers.
Diagnosis of the disease
Only in specialized laboratories can a test for staphylococcus be done. For these purposes, biomaterial is taken from the mucous membranes of the nose and throat. It's called bacterial culture. It is important to maintain high sterility and take the analysis according to the established scheme. After all, it is necessary to prevent situations in which other microorganisms can get into the material under study.
Samples taken from the mucous membranes are delivered to a special laboratory, where they can determine whether there is staphylococcus in the nose and throat. Treatment, ideally, should be prescribed only after receiving test results. After all, in the laboratory they not only determine which bacteria have infected the body, but also perform an antibiogram. You need to be guided by it when selecting medications. The antibioticogram shows which antibacterial agents the bacteria are sensitive to. After all, some of them cannot cause staphylococcus any harm.
Treatment tactics
Once it has been determined that staphylococcus is the cause of your problems, you can begin therapy. You should not expect the immune system to cope with pathogenic microorganisms on its own. This can only lead to complications. For example, with primary damage to the nasopharynx and lack of treatment, the infection can affect the central nervous system and lead to the development of intracranial phlebitis and the formation of abscesses. Pneumonia or even meningitis can be a complication.
As a rule, treatment is aimed at removing the causative agent of staphylococcus and carrying out complete sanitation of the nasopharynx area. Antibiotics such as Ceftriaxone, Amoxiclav, Ciprofloxacin, Oxacillin and other drugs are often prescribed wide range actions. But you need to focus on test results that will show which drugs the bacteria are sensitive to.
Simultaneously with the use of antibacterial agents, it is necessary to take drugs that should support normal level microflora in the gastrointestinal tract. You can use products such as Linex, Laktovit, Biolact and other similar medications.
Treatment of throat and nose infections
Having determined the type and antibiotic resistance of the pathogen that has affected the body, you can begin therapy. If the concentration of bacteria is insignificant, the infection can be destroyed using local means. Staphylococcus is treated with special antimicrobial solutions, sprays, decoctions, and infusions. In more severe cases, it is necessary to use special antistaphylococcal agents.
An addition to the main treatment can be the prescription of vitamin complexes that can strengthen the immune system and improve vitality. Do not forget about traditional methods of treatment. Of course, they alone will not be enough to fight the infection, but they will help speed up recovery and eliminate Staphylococcus aureus in adults. Using traditional methods One must be careful when treating children, because decoctions of many herbs can only be given from the age of 12.
You can instill Chlorophyllipt oil drops into your nose, and you can rinse its cavity with an alcohol solution of the same name. You can also use the well-known antiseptic “Furacilin”. You can increase the immunity of the mucous membranes with the help of IRS-19.
The throat can be gargled with Chlorophyllipt solution, herbal or salt infusions, and herbal decoctions. If necessary, symptomatic therapy is recommended: painkillers and antipyretics, drinking increased amounts of fluid. By the way, doctors say that Chlorophyllipt helps enhance the local effect of antibacterial agents on staphylococcus.
During pregnancy, a special approach to treatment is required. After all, not all antibacterial drugs are allowed for expectant mothers, so a therapist should select medications.
Features of getting rid of infection in pregnant women and babies
When selecting medications, expectant mothers and young children need to be especially careful. After all, not all medications can be taken by them. But we should not forget that staphylococcus during pregnancy can cause irreparable damage to the health of both the woman and her unborn baby. After all, the infection can be transmitted intrauterinely.
If treatment with antibiotics is unavoidable, then the doctor, as a rule, chooses the most gentle ones. Also, at the same time, the duration of treatment is adjusted downwards. The emphasis should be on approved folk remedies and local therapy.
To prevent infection, it is necessary to pay sufficient attention to preventive measures. These include not only personal hygiene, monitoring the quality of the products consumed, but also the fight against bad habits. You need to take care of yourself and stop licking or biting your lips or biting your nails. The leading role is given to strengthening the immune system and combating the manifestations of the disease. So, it is necessary to gargle and rinse your nose with herbal or saline solutions several times a day.
Alternative Methods
In combination with the treatment prescribed by the doctor, folk remedies therapy can also be used. Of course, it is impossible to say that the staphylococcus bacillus is sensitive to them. But they help enhance the effect of traditional medications and strengthen the immune system.
You need to choose the most suitable local remedies. So, to treat staphylococcus that has settled in the nasopharynx, you can use the following collection of herbs: burdock root, sedge buds, walnut leaves, roots of tricolor violet, wheatgrass, and white cherry. These plants are crushed and poured with boiling water. Drink half a glass of the infusion between meals.
It is also important to saturate the body with vitamin C. For these purposes, you can eat currants in unlimited quantities and drink rosehip decoction.
Among folk methods, rinsing with water fir extract is popular. Also, many recommend eating half a kilogram of apricot pulp daily. The specified volume of fruit can be divided into several times.
Propolis solution has proven itself well. One teaspoon of pharmaceutical infusion is diluted in a glass of warm boiled water. The prepared solution is used to gargle. Various herbal preparations can also be used for these purposes. For example, you can prepare an infusion of calendula, St. John's wort and chamomile if staphylococcus was found in the nose and throat. Treatment consists of a combination of traditional therapy and rinses.
You can take the following collection internally: thyme, wild rosemary, string, birch buds, yarrow. Half a liter of the prepared infusion is drunk in four stages throughout the day.
Doctors often prescribe inhalations and quartz treatment of the nasal and oral cavity as an addition to complex therapy. These methods allow you to weaken bacteria and get rid of infection in a short time.
Drugs used
In order to get rid of a staphylococcal infection, in some cases it is necessary long-term treatment. This is especially true in cases where the golden strain has been identified.
Therapy will be effective in cases where only those drugs to which the bacterium is sensitive are used. It is important to pay attention to its quantity. If only carriage has been identified, then treatment is not required. Therefore, you should not try to understand the test results and choose medications for yourself. The use of antibiotics at low concentrations of staphylococci will only harm the microflora.
But if your health deteriorates and symptoms of infection appear, you cannot do without antibacterial drugs. Depending on the results, drugs such as Amoxicillin, Ciprofloxacin, Unasin, Ofloxacin, Vancomycin, Ceftriaxone, Amoxiclav, Oxacillin and other broad-spectrum agents may be prescribed.
Also, if indicated, the doctor may prescribe a special staphylococcal bacteriophage. This product is intended to destroy the specified opportunistic microflora. It can be prescribed without combination with antibacterial agents in case of detection of Staphylococcus aureus. But such treatment is possible provided that the patient has no complications and only this strain was detected. This therapy should last 21 days. Sorbents are prescribed in combination with a bacteriophage. You can use the following drugs “Smecta”, “Enterosgel”. The use of special immunostimulants is also desirable.
After completing the course of treatment, it is necessary to take repeated tests. If it is determined that the expected effect of therapy could not be achieved, then another repetition is necessary. But at the same time, medications need to be changed. After all, the specified opportunistic microflora can develop resistance to the action of the same medications.
After successful therapy, it is necessary to restore the microflora. For these purposes, you can use the drug "IRS-19", universal vitamin complexes, dietary supplements.
β-toxin or sphingomyelinase is detected in approximately a quarter of all pathogenic staphylococci. β-toxin is capable of causing the destruction of red blood cells ( red blood cells), and also lead to the proliferation of fibroblasts ( migration of fibroblasts into the inflammatory focus). This toxin becomes most active at low temperatures.
γ-toxin is a two-component hemolysin that has moderate activity. It is worth noting that the bloodstream contains substances that block the action of γ-toxin ( sulfur-containing molecules are capable of inhibiting one of the components of the γ-toxin).
δ-toxin is a low molecular weight compound with detergent properties. Exposure of a cell to δ-toxin leads to disruption of cell integrity by various mechanisms ( basically there is a disruption of the relationship between lipids cell membrane ).
- Exfoliative toxins. In total, there are 2 types of exfoliative toxins – exfoliant A and exfoliant B. Exfoliative toxins are detected in 2–5% of cases. Exfoliants are capable of destroying intercellular connections in one of the layers of the skin ( granular layer of the epidermis), and also lead to detachment of the stratum corneum ( the most superficial layer of skin). These toxins can act locally and systemically. In the latter case, this can lead to scalded skin syndrome ( the appearance of areas of redness on the body, as well as large blisters). It is worth noting that exfoliants are able to bind several molecules involved in the immune response at once ( exfoliative toxins exhibit properties of superantigens).
- Toxic shock syndrome toxin (formerly called enterotoxin F) is a toxin that causes the development of toxic shock syndrome. Toxic shock syndrome refers to acutely occurring multisystem organ damage ( several organs are affected at once) with fever, nausea, vomiting, stool disorders ( diarrhea), skin rash. It is worth noting that toxic shock syndrome toxin can only be produced in rare cases by Staphylococcus aureus.
- Leukocidin or Panton-Valentine toxin capable of attacking some white blood cells ( neutrophils and macrophages). The effect of leukocidin on the cell leads to disruption of the water-electrolyte balance, which increases the concentration of cyclic adenosine monophosphate in the cell ( cAMP). These disorders underlie the mechanism of occurrence of staphylococcal diarrhea in food poisoning from products infected with Staphylococcus aureus.
- Enterotoxins. In total, there are 6 classes of enterotoxins - A, B, C1, C2, D and E. Enterotoxins are toxins that attack human intestinal cells. Enterotoxins are low molecular weight proteins ( proteins), which tolerate elevated temperatures well. It should be noted that it is enterotoxins that lead to the development food poisoning by type of intoxication. In most cases, these poisonings can be caused by enterotoxins A and D. The effect of any of the enterotoxins on the body manifests itself in the form of nausea, vomiting, pain in the upper abdomen, diarrhea, fever and muscle spasm. These disorders are caused by the superantigenic properties of enterotoxins. In this case, excessive synthesis of interleukin-2 occurs, which leads to this intoxication of the body. Enterotoxins can lead to an increase in the tone of intestinal smooth muscles and increase motility ( contractions of the intestines to move food along) gastrointestinal tract.
Enzymes
Staphylococcal enzymes have a diverse effect. Also, the enzymes that staphylococci produce are called “aggression and defense” factors. It should be noted that not all enzymes are pathogenicity factors.The following staphylococcal enzymes are isolated:
- Catalase is an enzyme that can destroy hydrogen peroxide. Hydrogen peroxide is capable of releasing the oxygen radical and oxidizing the cell wall of the microorganism, leading to its destruction ( lysis).
- β-lactamase is able to effectively combat and neutralize β-lactam antibiotics ( a group of antibiotics that are united by the presence of a β-lactam ring). It is worth noting that β-lactamase is very common among the population of pathogenic staphylococci. Some strains of staphylococci exhibit increased resistance to methicillin ( antibiotic) and other chemotherapy drugs.
- Lipase is an enzyme that facilitates the attachment and penetration of bacteria into the human body. Lipase is capable of destroying fat fractions and, in some cases, penetrating through sebum into the hair follicle ( location of the hair root) and into the sebaceous glands.
- Hyaluronidase has the ability to increase tissue permeability, which contributes to the further spread of staphylococci in the body. The action of hyaluronidase is aimed at the breakdown of complex carbohydrates ( mucopolysaccharides), which are part of the intercellular substance connective tissue, and are also found in bones, in vitreous body and in the cornea of the eye.
- DNAase is an enzyme that cleaves double-stranded DNA molecule ( Deoxyribonucleic acid) into fragments. During exposure to DNase, the cell loses its genetic material and the ability to synthesize enzymes for its own needs.
- Fibrinolysin or plasmin. Fibrinolysin is a staphylococcal enzyme that is capable of dissolving fibrin threads. In some cases, blood clots are performed protective function and prevent bacteria from entering other tissues.
- Staphylokinase is an enzyme that converts plasminogen to plasmin ( when exposed to staphylokinase, the proenzyme plasminogen transforms into its active form - plasmin). Plasmin can extremely effectively break down large blood clots, which act as an obstacle to the further advancement of staphylococci.
- Phosphatase is an enzyme that accelerates the breakdown of phosphoric acid esters. Staphylococcal acid phosphatase is generally responsible for the virulence of the bacterium. This enzyme can be located on the outer membrane, and the location of the phosphatase depends on the acidity of the environment.
- Proteinase staphylococcus is capable of breaking down proteins into amino acids ( protein denaturation). Proteinase has the ability to inactivate certain antibodies, suppressing the body's immune response.
- Lecithinase is an extracellular enzyme that breaks down lecithin ( fat-like substance that is part of the cell wall) into simpler components ( phosphocholine and diglycerides).
- Coagulase or plasmacoagulase. Coagulase is the main factor in the pathogenicity of staphylococcus. Coagulase can cause blood plasma clotting. This enzyme can form a thrombin-like substance that interacts with prothrombin and envelops the bacterium in a fibrin film. The formed fibrin film has significant resistance and serves as an additional capsule for staphylococcus.
Groups of staphylococci depending on the presence of coagulase
| Pathogenicity | Coagulase-positive staphylococci | Coagulase-negative staphylococci |
| Opportunistic staphylococci that live on the skin and mucous membranes of humans and animals | S. intermedius, S. hyicus | S. capitis, S. warneri, S. cohnii, S. xylosis, S. sciuri, S. simulans, S. arlettae, S. auricularis, S. carnosus, S. caseolyticus, S. gallinarum, S. kloosii, S. caprae, S. equorum, S. lentus, S. saccharolyticus, S. schleiferi, S. lugdunensis, S. chromogenes. |
| Pathogenic staphylococci that cause diseases in humans | S. aureus ( Staphylococcus aureus) | S. saprophyticus ( saprophyticstaphylococcus), S. epidermidis ( epidermalstaphylococcus), S. haemolyticus ( hemolytic staphylococcus). |
Adhesins
Adhesins are surface layer proteins that are responsible for attaching staphylococcus to mucous membranes and connective tissue ( ligaments, tendons, joints, cartilages are some of the representatives of connective tissue), as well as to the intercellular substance. The ability to attach to tissues is associated with hydrophobicity ( property of cells to avoid contact with water), and the higher it is, the better these properties are manifested.Adhesins have specificity for certain substances ( tropism) in organism. So, on the mucous membranes this substance is mucin ( a substance that is part of the secretion of all mucous glands), and in connective tissue – proteoglycan ( intercellular substance of connective tissue). Adhesins are capable of binding fibronectin ( complex extracellular substance), thereby improving the process of attachment to tissues.
It is worth noting that most of the components of the cell wall of pathogenic staphylococci, as well as their toxins, can lead to delayed and immediate allergic reactions ( anaphylactic shock, Arthus phenomenon, etc.). Clinically this manifests itself in the form of dermatitis ( inflammatory skin disease), bronchospastic syndrome ( spasm of bronchial smooth muscles, which manifests itself as shortness of breath) etc.
Method of infection with staphylococcus
 Diseases caused by staphylococci can be of the nature of autoinfection ( entry of bacteria into the body through damaged areas of the skin and mucous membranes), since staphylococci are permanent inhabitants of human skin and mucous membranes. Infection can also occur through contact with household items or by eating contaminated food. This method of infection is called exogenous.
Diseases caused by staphylococci can be of the nature of autoinfection ( entry of bacteria into the body through damaged areas of the skin and mucous membranes), since staphylococci are permanent inhabitants of human skin and mucous membranes. Infection can also occur through contact with household items or by eating contaminated food. This method of infection is called exogenous. It is worth noting that important In the mechanism of transmission of staphylococci, they are attributed to the carriage of pathogenic staphylococci. The term “carrier” refers to the presence of pathogenic bacteria in the body that do not cause any clinical manifestations diseases. There are two types of carriage of pathogenic staphylococci - temporary and permanent. The main danger is posed by people who are constant carriers of pathogenic staphylococcus. In this category of people, pathogenic staphylococci are detected in large quantities, which are present for a long time on the mucous membranes and in the skin. It is still not entirely clear why long-term carriage of pathogenic staphylococcus occurs. Some scientists associate this with a weakening of local immunity with a decrease in the titer of immunoglobulin A ( a decrease in the concentration of one of the types of antibodies that are responsible for the immune response). There is also a hypothesis that explains the long-term carriage of pathogenic staphylococcus with impaired functioning of the mucous membrane.
The following mechanisms of transmission of staphylococci are distinguished:
- contact and household mechanism;
- air-droplet mechanism;
- air-dust mechanism;
- nutritional mechanism;
- artificial mechanism.
Contact and household mechanism
The contact-household mechanism of transmission of infection occurs due to the transfer of bacteria from the skin and mucous membranes to various household and household items. This route of transmission of infection is associated with the use of common household items ( towel, toys, etc.). To implement the contact-household route of transmission, a susceptible organism is required ( When bacteria are introduced, the human body reacts with a clinically significant disease or carriage). The contact-household mechanism of transmission is a special case of the contact route of transmission of infection ( direct contact with skin).Airborne mechanism
The airborne transmission mechanism is based on inhalation of air containing microorganisms. This transmission mechanism becomes possible if bacteria are released into the environment along with exhaled air ( for diseases of the respiratory system). Pathogenic bacteria can be released through breathing, coughing and sneezing.Air-dust mechanism
The airborne dust mechanism of transmission of staphylococcal infection is a special case of the airborne droplet mechanism. The air-dust mechanism is realized when bacteria remain in dust for a long time.Nutritional mechanism
With the alimentary mechanism ( fecal-oral mechanism) transmission, the release of staphylococci occurs from an infected organism through bowel movements or vomiting. Penetration of bacteria into a susceptible organism occurs through the oral cavity when consuming contaminated food ( presence of microorganisms in food). After this, the staphylococcus again colonizes the digestive tract of the new host. As a rule, contamination of food products with staphylococci occurs due to non-compliance with personal hygiene rules - insufficient hand washing. Also, this mechanism can be carried out as a result of carriage of a staphylococcal infection in a food industry worker.Artificial mechanism
The artificial transmission mechanism is characterized by the penetration of pathogenic staphylococcus into the human body through insufficiently sterilized ( sterilization is a method of processing medical instruments and equipment to completely destroy all microorganisms) medical instruments. As a rule, this can occur during the use of various instrumental diagnostic methods ( for example, bronchoscopy). Also, in some cases, the penetration of staphylococcus into the body is observed during surgical operations.It is worth noting that medical equipment and instruments may not be completely sterile due to the fact that staphylococcus is resistant to some types of disinfectants ( chemical substances with antimicrobial action). Also, the cause of the artificial transmission mechanism may be the incompetence or negligence of medical personnel.
What diseases does Staphylococcus aureus cause?
 Staphylococcus aureus is capable of infecting most tissues of the human body. In total, there are more than a hundred diseases that are caused by staphylococcal infection. Staphylococcal infection is characterized by the presence of many different mechanisms, routes and transmission factors.
Staphylococcus aureus is capable of infecting most tissues of the human body. In total, there are more than a hundred diseases that are caused by staphylococcal infection. Staphylococcal infection is characterized by the presence of many different mechanisms, routes and transmission factors. Staphylococcus aureus can penetrate extremely easily through minor damage skin and mucous membranes into the body. Staphylococcal infection can lead to various diseases, ranging from acne ( acne) and ending with peritonitis ( inflammatory process peritoneum), endocarditis ( inflammation of the inner lining of the heart) and sepsis, which has a mortality rate of around 80%. In most cases, staphylococcal infection develops against the background of a decrease in local or general immunity, for example, after an acute respiratory viral infection ( ARVI).
The following symptoms are characteristic of staphylococcal sepsis:
- increase in body temperature to 39 – 40°C;
- intense headache;
- loss of appetite;
- nausea;
- vomit;
- increased sweating;
- skin pustular rash;
- increase in heart rate to 140 beats per minute;
- an increase in the size of the liver and spleen;
- loss of consciousness;
- rave.