Closed injuries should be understood as damage to tissues and organs caused by exposure to external factors without violating the integrity of the skin and visible mucous membranes.
In wartime, with the use of thermonuclear weapons, the number of closed injuries will increase to 50%, mainly due to direct and indirect (by flying logs, bricks, fragments, etc.) impact of the shock wave. Closed injuries will occur in soft tissues, bones, joints, organs of the chest and abdominal cavities, in the brain, and organs of the genitourinary system.
Allocate closed injuries of soft tissues; closed injuries of organs located in the cavities; closed injuries of bones and joints.
The severity of a closed injury depends on the traumatic force, the direction and duration of its impact, the area of the injured area of the body, the state of the body at the time of injury, the injured tissue, and other factors.
A bruise is a type of injury that occurs when direct impact a mechanical damaging factor, such as hitting an object or hitting an object. As a result of the direct destructive effect of the object and its kinetic energy during the impact, tissue cells are damaged. This triggers a local reaction to a traumatic agent.
Signs of a bruise
At the site of the bruise, a slight swelling and short-term pain first appear. Later, depending on the volume of the damaged tissue, the swelling increases significantly, there is an intense constant pain at the site of the injury. Perhaps in response to pain, the development of muscle contraction, which leads to dysfunction of these muscles. The focus of bruising can significantly increase compared to the original - a site of secondary damage occurs. If the vessels passing at the site of injury are affected, then a hematoma is formed - an accumulation of blood in the thickness and loose spaces of soft tissues. If the integrity of small vessels is violated, small-point hemorrhages or continuous bruises appear.
The increase in pain and swelling continues during the first two days, then the slow resorption of the focus begins, which can include from two to three weeks. If there is a hematoma, then complete resorption takes a period of up to a month or more. Bruises of soft tissues in the abdomen, lower back, and chest deserve special attention. With such localizations, it is important to exclude damage to internal organs that can lead to internal bleeding. Therefore, it is very important to consult a doctor in such a situation.
First aid for bruises.
As a rule, bruises are subject to the head, arms and legs. Moreover, muscles, blood vessels and nerves are usually damaged. Due to its elasticity, the skin is less likely to suffer from injury. The blood poured out from the wounded vessels impregnates the surrounding tissues, and a bruise (hematoma) is formed. As a result, swelling appears at the site of the bruise, pain occurs. Often even violated normal function injured limb. The pain is particularly aggravated when the injured area is abundantly supplied with nerves.
Ice, snow or a bubble filled with cold water should be immediately applied to the site of injury. Suitable for this purpose also dipped in cold water towel. Massage, thermal procedures, hot baths and compresses are contraindicated for 4-5 days, as such measures increase hemorrhage.
If the bruise was accompanied by abrasions or scratches, an infection can penetrate into the contaminated wound. Therefore, the wound should be cauterized with alcohol or iodine and tied with a bandage.
When, with a bruised leg, the foot turned up and a sprain occurred, in addition to hemorrhage, swelling and severe pain, the mobility of the joint may be limited. In such cases, the victim needs bed rest, cold on the joint area, and a bandage to limit joint mobility. (Usually, such bandages are also resorted to when the knee and elbow joints are damaged.)
Particular attention should be paid to head contusion, which may be accompanied by a concussion. Symptoms of this disease: sharp headache, nausea and dizziness. The victim needs complete rest and urgent medical advice.
Under all circumstances, after giving him first aid, the victim must be shown to the doctor in order to, if necessary, administer anti-tetanus serum to him, exclude bone fractures, and in case of bruises of the abdomen and chest- damage to internal organs.
So, after the occurrence of a bruise, it is important to assess the force of the blow, the localization of the site of the bruise. This is necessary to exclude the possibility of damage to the main vessels, internal organs, the brain with bruises in the head area, bone fractures.
The first hours and the first or second day, cold objects are applied to the site of injury, for example, an ice pack, a bottle of frozen water. For athletes use special sprays. Ice must be applied through a cloth, such as a towel, which should then be slowly unrolled.
When exposed to cold, vasospasm occurs and tissue reactions to damage slow down. This allows you to reduce the area of secondary damage.
To prevent thrombosis and reduce the inflammatory response in the first hours and the next day, aspirin is allowed at a dose of 0.5 g 1-2 times a day. It is better to use its soluble forms.
For pain relief, it is advisable to take analgin, ketorol both in the form of tablets and injection forms. In the same period, it is good to use ointments based on anti-inflammatory drugs, such as diclofenac (Voltaren), ibuprofen, ketorol. A good effect is achieved by using a quick gel.
From the end of the second and on the following day, dry heat is applied to the site of injury, physiotherapy. It is possible to use warming ointments: espol, finalgon, fastum gel, capsicam. Applicable pepper tinctures, bile, cabbage leaves, etc., sometimes Wobenzym is recommended.
In the event of the formation of hematomas at the site of injury, in no case should they be opened. This contributes to infection and subsequent suppuration. These hematomas will perfectly decrease on their own during the first day.
With severe bruises of the limbs, fixation is sometimes resorted to to reduce pain when moving.
Emergency care for injuries of the skull and brain
Injuries to the skull and brain occur with a direct blow to the head, by the type of acceleration (road accidents of a fall from a height), with compression of the head between two solid objects. Depending on the strength of the impact of the traumatic agent, either reversible (concussion) or irreversible changes (bruises of varying degrees) occur in the brain. Importance has the formation of intracranial hematomas and foci of crushing of the brain, which, in the absence of specialized neurosurgical care, lead to an increase in cerebral edema, the development of dislocation and, as a result, to death. For practical work, it is advisable to distinguish three degrees of traumatic brain injury at the prehospital stage: mild, moderate and severe.
Light traumatic brain injury (concussion, brain contusion mild degree).
Symptoms. Characterized by switching off consciousness for several minutes, some confusion, disorientation after the restoration of consciousness, retro- and anterograde amnesia Vomiting is often observed. Patients complain of severe headache, general weakness, dizziness, tinnitus, pain in eyeballs Oh. Focal neurological symptoms slight or absent.
Urgent Care. Immediately at the scene of the incident, the patient must be laid on his back or on his side. Transportation is carried out only in the supine position. Patients are administered analgesics (2 ml of a 50% solution of analgin in / m), decongestants (20-40 mg of lasix in / m), 20 ml of a 40% solution of glucose in / in.
Before the establishment clinical diagnosis or examination of the patient by a neuropathologist or neurosurgeon, sedatives should not be used to relieve possible excitation, since these drugs can affect the manifestation of focal and cerebral symptoms, which can lead to diagnostic errors. If patients have wounds on the head, it is necessary to treat the wound, stop bleeding, and apply an aseptic bandage.
Hospitalization is carried out in a traumatological, neurological, general surgical hospital.
Traumatic brain injury of moderate severity (brain contusion of moderate degree).
Symptoms. These victims are characterized by a longer shutdown of consciousness - from several minutes to several hours. Pronounced retro- and anterograde amnesia, patients are disoriented in time and place, somewhat inhibited Complains of diffuse headache. meningeal symptoms moderate, possibly psychomotor agitation. Focal neurological symptoms are detected that correspond to the localization of the brain contusion (inadequate behavior of coordination disorders, pyramidal symptoms, speech disorders, nystagmus, anisocoria, etc.). A number of patients have injuries to the bones of the vault and base of the skull, which are manifested by pronounced subaponeurotic hematomas, hematomas in the area mastoid processes(with a fracture of the pyramid temporal bone), in the region of the orbits (symptom of "glasses" - with a fracture in the region of the anterior cranial fossa), possible outflow of blood with an admixture of cerebrospinal fluid from the nose, ear, along back wall pharynx, to determine the presence of cerebrospinal fluid in the blood, a simple “double spot” method is used when wetting blood released from the nose or ear. In terms of diagnostics, it should be noted that a traumatic brain injury with the presence of liquorrhea is considered open.
Urgent Care. The same as with mild traumatic brain injury.
Hospitalization: urgently in a neurosurgical hospital.
Severe traumatic brain injury (severe brain injury).
Symptoms. Characterized by a long shutdown of consciousness violations of the respiratory and cardiovascular systems. There are tachycardia or bradycardia, arterial hypertension, shortness of breath, which are caused both by impaired airway patency and by the primary suffering of the corresponding brain stem regions. In the first hours after the injury, primary stem neurological symptoms predominate (floating movements of the eyeballs, respiratory disorders, bilateral constriction or dilation of the pupils, changing muscle tone, decerebrate rigidity, depression of deep reflexes), cerebral (depression of consciousness to the point of coma). Severe traumatic brain injury is usually accompanied by a fracture of the vault and base of the skull, as well as massive subarachnoid hemorrhage.
Urgent Care. Medical events are mainly aimed at correcting vital disorders (insertion of an air duct, tracheal intubation, mechanical ventilation), the introduction of plasma-substituting solutions (400 ml of polyglucin, reogluman, rocdex), dehydration drugs (40-80 mg of lasix intramuscularly or intravenously, up to 100 mg of hydrocortisone or up to 1000 mg IV prednisone). Often, patients are in a state alcohol intoxication which significantly changes the clinical manifestations of traumatic brain injury. In such cases, the introduction of 5-10 ml of a 05% solution of bemegride IV is indicated. Sedative therapy should be avoided.
Hospitalization: urgently in a neurosurgical hospital. With severe violations of vital functions, the possibilities of transporting the patient are limited, and the victim is hospitalized in the nearest intensive care unit.
Severe craniocerebral injury with compression of the brain (intracranial hematomas, depressed fractures, foci of crushing of the brain, etc.).
Symptoms. Patients with intracranial hematoma are characterized by a clear interval after injury, after which their condition progressively worsens, consciousness is depressed, signs of brain compression appear (bradycardia up to 40-50 beats per minute, unilateral mydriasis, increasing or persistent contralateral hemiparesis, bilateral pathological foot signs, focal or generalized seizures, etc.). Depending on the type of hematoma (epi- or subdural), this clinical picture may develop at different times after the injury - from several hours (with epidural hematoma) to several days and even weeks (with subdural). Pre-hospital diagnosis of intracerebral hematoma, foci of crushing of the brain is extremely difficult; the clinical picture corresponds to a severe brain contusion with a predominance of hypertensive-dislocation syndromes.
Urgent Care. Measures are being taken to correct vital disorders to prevent the development of progressive edema and dislocation of the brain (see severe traumatic brain injury). For wounds and compressed fractures of the bones of the cranial vault, after careful, sparing treatment, an aseptic dressing is applied using a cotton-gauze “donut” (in order to prevent further penetration bone fragments and brain damage).
Hospitalization: urgently to a neurosurgical hospital, as these victims are indicated for emergency surgery for health reasons.
DAMAGE (injury) are anatomical or functional disorders tissues and organs of the body under the influence of external factors.
Main types of damage depending on the reason causing them:
mechanical , arising under the influence of mechanical force (for example, during a fall, impact, exposure to a blast wave, etc.);
physical , arising from exposure to high or low temperatures (for example, burns, frostbite, etc.), electric current, penetrating radiation, etc.;
chemical , arising from exposure to tissues of various chemicals: acids, alkalis, agents, etc.
Depending on the condition of the skin and mucous membranes, there are:
open injuries (wounds), when the integrity of the external integument is violated to one degree or another (wounds, open dislocations and fractures, burns, etc.).
closed , i.e. those injuries in which the integrity of the skin and mucous membranes is not violated (soft tissue bruises, sprains, most dislocations and fractures, etc.). They can occur both in superficial tissues and in the organs of the chest and abdominal cavities, in the cranial cavity and joints.
End of work -
This topic belongs to:
Fundamentals of medical knowledge
Educational institution.. Vitebsk State University named after P M Masherov.. E D Smolenko..
If you need additional material on this topic, or you did not find what you were looking for, we recommend using the search in our database of works:
What will we do with the received material:
If this material turned out to be useful for you, you can save it to your page on social networks:
| tweet |
All topics in this section:
Vitebsk
Publishing house of UO “VSU im. P.M. Masherov" UDC LBC Published by decision of the Scientific and Methodological Council Educational Institution "Vitebsk
Principles of drug care
Formation among the population of skills to provide first medical care sick and injured at home and at the enterprise, while traveling and on the street are the main task of medical workers
Dosage forms
Dosage forms are forms that are convenient for practical use and given to medicines. Currently developed and put into practice many
Types of action of medicinal substances
ü Depending on location medicinal substances in the body, their action can be local and general. × Local action
Respiratory diseases
The respiratory system includes organs that perform: air-bearing function (oral cavity, nasopharynx, larynx, trachea, bronchi); gas exchange fun
Acute bronchitis
Bronchitis is an inflammation in the bronchi. According to the nature of the course, acute and chronic bronchitis are distinguished. ACUTE BRONCH
Bronchial asthma
Asthma is a paroxysmal suffocation. Depending on the mechanism of its development (pathogenesis), asthma is bronchial and cardiac. BRONCHIAL AST
Diseases of the cardiovascular system
General signs of diseases of the circulatory system: Palpitations - a feeling of rapid and increased heart rate. healthy person
Acute vascular insufficiency
Acute vascular insufficiency is a decrease in the tone of blood vessels, accompanied by sharp decline blood pressure. It manifests itself in the form of 3 clinical forms:
Diseases of the digestive system
Among the most common manifestations of diseases gastrointestinal tract include: Pain that differs in: × in nature: dull and sharp, aching and dir
Etiology and pathogenesis
Exogenous factors: × errors in nutrition (poor quality food; overeating, especially heavy meals at night; drinking alcohol, hot spices, etc.); ×
Treatment
Ø gastric lavage with warm water or chamomile infusion; Ø the bowels are emptied with a cleansing enema and / or the appointment of a saline laxative; Ø bed r
Medical therapy
Many different drugs have been proposed for the treatment of peptic ulcers, differing in composition and form. They are divided into 6 main groups: antacids and adsorbents
Clinical picture
The main objective signs of gastrointestinal bleeding are hematemesis and tarry stool. The color of the vomit depends on the location of the pathological process.
Acute cholecystitis
Etiology and pathogenesis. The main cause of acute inflammation of the gallbladder is the penetration of an infectious agent into it (Escherichia, Pseudomonas aeruginosa, staphylococcus, ent
Etiology and pathogenesis
The reasons for the development of cholelithiasis are: × hereditary features of lipid metabolism; × metabolic diseases (obesity, diabetes, atherosclerosis, gout); ×
Etiology and pathogenesis
Insulin-dependent diabetes mellitus develops in people with a genetic predisposition to this disease. Upon contact with β-tropic viruses (rubella measles, mumps
Coma in diabetic patients
Diabetic ketoacidotic coma is one of the most severe complications Diabetes mellitus occurs as a result of a growing lack of insulin in the body. Angle breaking
Diseases of the kidneys and urinary tract
Diseases of the urinary organs are accompanied by a relatively small number of symptoms. Some of them may be asymptomatic for a long time, only changes in the urine indicate
Pyelitis. Pyelonephritis
Pyelitis is an inflammation of the renal pelvis infectious origin, pyelonephritis - an inflammatory process in the kidneys and renal pelvis. In the pelvis infection
Antisepsis and asepsis
Modern surgery covers a large number of surgical specialties: general surgery, traumatology (the study of injuries), neurosurgery (the study of care
Types of wound infection, ways of penetration of its pathogens into the wound
According to the types of respiration, all microorganisms are divided into three groups: aerobic microbes, living and developing only in the presence of oxygen; anaerobic microbes,
Antiseptics
ANTISEPTICS is a complex of therapeutic preventive measures aimed at the destruction of microbes in the wound or the body as a whole. Types of antiseptics:
Antiseptic substances
Antimicrobials are medicines that are used to fight pathogenic microbes. Types of antimicrobial agents:
Asepsis
ASEPTICA (from the Greek a - denial and septicos - purulent) is a system of preventive measures aimed at the destruction of microorganisms in order to prevent possible
Anesthesia. resuscitation
Attempts to reduce pain reactions during operations have been made since time immemorial. However, most of the methods and means taken for this purpose were not only effective, but sometimes dangerous for
General anesthesia and its types
Narcosis (from the Greek narcosis - numbness) is an artificially induced deep dream with loss of consciousness and pain sensitivity, caused by narcotic drugs. To Nar
Preparation for anesthesia
Distinguish general training to anesthesia and special medical preparation - premedication. General training includes
resuscitation
REANIMATION - measures that are aimed at restoring severely impaired or lost essential vital functions of the body in order to revive the patient. It is carried out at the thermal
Bleeding. Transfusion of blood and its substitutes
BLEEDING, hemorrhage (Greek haima - blood and rhagos - torn, broken) - lifetime outflow of blood from blood vessels due to violation of their integrity
Risk of blood loss in children and adults
The mass of blood in an adult is 1/13 of the body weight, i.e. about 5 l. The volume of circulating blood (CBV) depends on body weight, age of a person and is approximately determined by the formula: CBV \u003d m
Ways to temporarily and permanently stop bleeding
The main means of artificially stopping bleeding are mechanical techniques: Ø Giving the limb an elevated position leads to stopping the bleeding
Agglutinins are special proteins that belong to gamma globulins and are contained in the blood serum. There are two types of them - α and β
Agglutination reaction - gluing of erythrocytes as a result of the combination of blood serum agglutinins with agglutinogens of the same name, followed by their dissolution (hemolysis).
Transfusion of blood and plasma replacement solutions
Types of blood transfusion: direct blood transfusion - direct injection of blood from the donor's vein into the recipient's vein with the help of
Complications from blood transfusion
Blood transfusion reactions - usually proceed without disruption of the function of vital organs, most often they are short-term and disappear in the next few hours without special treatment.
Plasma replacement solutions
Plasma-substituting solutions are divided into two groups: natural and blood substitutes. Natural substitutes are human blood products: ×
traumatic shock
TRAUMATIC SHOCK occurs most often and occurs when a vast mass of soft tissues is crushed, fractures of the bones of the skeleton, damage to the chest or abdominal cavity, or
Soft tissue injuries
A bruise is a closed injury to tissues or organs without visible anatomical disorders, resulting from a mechanical injury (falling or hitting a hard blunt object).
Sprains and ruptures of ligaments, tendons and muscles
Sprains and ruptures - damage to soft tissues due to a sudden overstrain that exceeds the physiological limits of the norm. Most often
Types of dislocations
By origin, dislocations are: congenital; acquired: - traumatic; - pathological. Traumatic
Syndrome of prolonged compression
Syndrome of prolonged crushing (traumatic toxicosis) occurs after prolonged squeezing of the limb during the collapse of houses, landslides in the mountains, which could
Drowning
Drowning is a form of mechanical asphyxia that occurs when a person is immersed in water. clinical picture. There are three options
Open damage. Surgical infection
OPEN DAMAGES (WOUNDS) WOUND - mechanical damage to body tissues with violation of the integrity of the skin or mucous membrane
Acute focal infection
Etiology. Pathogens: pyogenic bacteria (staphylococci, streptococci, coli, pneumococci, Pseudomonas aeruginosa). clinical picture. Unannounced
Infection of the skin and subcutaneous tissue
Furuncle - acute purulent inflammation sebaceous gland and hair follicle. Etiology. The causative agent is staphylococcus aureus. Facilitating conditions - non-observance of hygiene rules,
Acute general infection
SEPSIS is a general non-specific infectious disease resulting from the spread of a purulent infection throughout the body or poisoning of the body with waste products.
Acute anaerobic infection
GAS GANGRENE - a complication wound process, characterized by rapidly advancing and spreading necrosis of tissues, their necrosis, as a rule, with the formation of gases.
Acute specific infection
Tetanus is an acute specific infection caused by the penetration of tetanus bacillus into the body with open injuries, characterized by damage to the nervous system and
burn disease
Burn disease develops after thermal effects (ΙΙ - ΙV degree) on 10-15% or more than 50% of the body surface (with burns of Ι degree) with disorder
Frostbite and freezing
Frostbite - limited damage to body tissues caused by local action of low temperature. FREEZING - general exposure to low temperatures
Clinical picture
Local changes are manifested by tissue burns at the points of entry and exit of electric current, ruptures of all layers of tissues. Electrical burns are usually deep, slowly clearing,
bone fractures
FRACTURE - a complete or partial violation of the integrity of the bone, caused by the action of a mechanical force or a pathological process and accompanied by
Closed traumatic brain injury
CLOSED CRANIO-BRAIN INJURY (CBI) is accompanied by damage to the brain, without violating the integrity of the skin of the head and aponeurosis, including fractures of the bones of the arch or
Fractures of the bones of the vault and base of the skull
Fractures and cracks in the bones of the skull often correspond to foci of contusion or intracranial hematoma. Distinguish between open and closed skull fractures
Craniocerebral wounds
OPEN CRANIO-BRAIN INJURY (TBI) - damage to the skin of the head with damage to the aponeurosis and bones of the skull. Most often found in lacerated wounds
Nose injuries
Injury to the soft lining of the nose. In case of violation of the integrity of the skin and mucous membranes, the trauma of the nose is considered open. Simultaneous damage to the cartilage and bone base of the nose. Per
First aid
Ø Apply an aseptic bandage to the damaged eye. For penetrating wounds and eye contusions, a bandage is applied to both eyes. Ø Do not wash damaged eyes. Only
Wounds of the trachea, larynx, large vessels of the neck
Closed injuries include bruises, fractures of the hyoid bone, cartilage of the larynx and trachea. They arise from a blow with a solid object, falling, compression. Signs: notice
Spinal column injuries
Closed injury of the spine and spinal cord is not more than 0.3% of total all damage. However, the severity of this type of injury and the duration of the associated disability
First aid
Ø If there is a wound, apply an aseptic dressing. Ø Introduce painkillers and cardiovascular agents. Ø Immobilize the spine.
Chest injuries
Distinguish between closed and open injuries of the chest. CLOSED injuries of the chest include bruises, compression, concussions, fractures of the ribs, class
Traumatic asphyxia with chest compression
Traumatic asphyxia is a symptom complex, which is caused by a temporary cessation of breathing with a sharp compression of the chest during collapses, explosions, sometimes from multiple
chest wounds
There are penetrating and non-penetrating wounds of the chest. Non-penetrating wounds of the chest are wounds in which the integrity of the parietal pleura is not violated.
Diseases and injuries of the abdominal and pelvic organs
THE CONCEPT OF "ACUTE ABDOMINAL" Acute abdomen is a clinical picture in which there are signs of inflammation of the peritoneum or internal bleeding. Acute
Clinical picture
By clinical course distinguish between acute and chronic peritonitis. By prevalence, there are diffuse (general) and limited peritonitis: Diffuse peritonitis
Closed injuries of the abdomen
With closed injuries of the abdomen, there is no violation of the skin. Etiology. Closed injuries occur as a result of some kind of blunt trauma (explosive impact).
Abdominal wounds
When the abdomen is injured, the integrity of the skin is violated as a result of the use of firearms and cold steel, sharp objects. Clinical manifestations are very different
The clinical picture includes relative and absolute signs
Relative signs: increased heart rate, pain on palpation throughout the abdomen, tension in the muscles of the abdominal wall, positive Shchetkin-Blumberg symptom, cyx tongue, thirst. Voltage
Pelvic injuries
Pelvic injuries are divided into open and closed. Allocate damage to the soft tissues of the pelvis, fractures of the pelvic bones without damage and with damage to the pelvic organs.
Injuries of the urinary system
Damage to the kidneys and ureters Closed injuries to the kidneys and ureters occur from a blow to the lumbar region, during a fall, exposure to
Topic #8. CLOSED DAMAGE
1. The concept of bruises, signs, first aid and treatment.
2. Sprains and ruptures of ligaments, tendons and muscles, symptoms, first aid and treatment of such injuries.
3. Dislocations, their types and signs, first aid and treatment.
4. Post-traumatic toxicosis, symptoms, features of first aid and treatment.
5. Drowning, asphyxia during landslides and falling asleep with earth, first medical aid.
1. CONCEPT ABOUT INJURIES. SIGNS, FIRST AID AND TREATMENT
The name "trauma" comes from Greek word"trauma" and combines a number of damage to tissues and organs resulting from various external influences. Damage can be closed and open, it depends on the integrity of the skin and mucous membranes. Open injuries are called wounds. In this lecture, the following injuries will be considered: bruises, sprains, dislocations, etc.
The number of victims with closed injuries during wars increases (up to 50%) mainly due to the impact of the shock wave and "secondary projectiles".
The impact of these damaging factors can extend to various human tissues and organs.
This results in:
Soft tissue bruises;
Sprains and ruptures of the ligamentous apparatus;
Compression of soft tissues by the ground, structures of destroyed buildings and structures;
Fractures, etc.
A bruise is a tissue injury that is not accompanied by a violation of the integrity of the skin. The severity of tissue damage depends on:
The size, weight and shape of the object that was hit or hit by a person;
impact force;
The age of the victim;
Places of injury;
tissue resistance.
With bruises, to one degree or another, the subcutaneous fatty tissue with the lymphatic and blood vessels located in it, as well as the underlying tissues, is destroyed.
Clinical signs of a bruise are few, but they are so distinct that they do not cause difficulties in diagnosis:
Swelling;
Hemorrhage;
Dysfunction of the affected body part;
Local and general temperature increase.
Pain varies in intensity depending on the area of injury. Severe pain can sometimes lead to traumatic shock. The nature of pain is also influenced by individual susceptibility to pain.
Swelling in the bruised area is caused by tissue edema, which occurs due to the fact that the walls of capillaries and small vessels become permeable to blood plasma, which, leaving the vessels, impregnates the intercellular gaps. The magnitude of the swelling depends on the thickness of the fat layer: with its severity, the swelling can reach significant sizes.
When small vessels rupture, small hemorrhages are formed, called bruises. Damage to larger vessels causes extensive hemorrhages - hematomas. The more superficial the hemorrhage, the sooner it manifests itself in the form of a so-called bruise. In connection with the decomposition of the blood pigment, the color of the bruise changes from blue to green, and then yellow. For large accumulations liquid blood- hematomas that do not resolve for a long time, a connective tissue membrane can form, and then such an encysted hematoma is called a cyst.
Violation of the function is primarily a protective reaction of the body to injury and depends on the localization of the bruise, the reaction of the victim to pain and the nature of the changes that have occurred.
Local and general temperature increase is associated with the resorption of extensive hematomas and their suppuration.
With severe bruises, both fiber and muscles can be destroyed. Dead tissue becomes a "foreign body", i.e. unnecessary and superfluous material for the body. With large hematomas and a large number of destroyed tissues, an increase in the number of leukocytes in the blood (leukocytosis) occurs.
All the described phenomena occurring at the site of injury are characterized by signs characteristic of inflammation. However, with a bruise, the skin is not damaged, and, therefore, there is no infection in the depths of the damaged tissues, therefore this type of inflammation is called aseptic (microbial-free).
The provision of first aid for bruises begins with the appointment of rest. In order to reduce swelling of the injured limb, an elevated position is given.
A bubble filled with ice or cold water is applied to the site of injury for 40-50 minutes, then a break is made for 10-15 minutes, after which the procedure is repeated.
With extensive bruises with dysfunction of the limbs, transport immobilization and the introduction of painkillers are indicated.
Treatment of bruises is carried out by applying heat from 2-3 days after the bruise (heating pad, warming compress, bath and other thermal procedures), then - the use of massage and therapeutic exercises (active and passive movements).
With large hematomas that are not amenable to resorption, a puncture is performed followed by the introduction of antibiotics. If it is not possible to suck the blood, the hematoma is opened. Opening a large hematoma is necessary due to the possibility of suppuration or mechanical compression of blood vessels and nerve trunks. After opening, a pressure bandage is applied to the area of the former hematoma to avoid re-filling the cavity.
2. STRETCHING AND RUPTURES OF LIGANS, TENDONS AND MUSCLES,
SYMPTOMS. FIRST AID
AND TREATMENT OF SUCH DAMAGES
Sprain occurs when the range of motion in a particular joint exceeds the usual, normal. Clinically, sprains show the same signs as bruises, but often dysfunction will be most pronounced.
Ruptures of muscles, ligaments, tendons most often occur with sudden, abrupt movements and direct exposure to a damaging force. Partial or complete ruptures of ligaments, muscles, tendons, detachment of the ligament from the place of its attachment to the bone, detachment of the ligament together with a fragment of bone tissue can be observed.
Clinical ruptures of the ligamentous apparatus, tendons and muscles are divided into mild, moderate and severe.
For all degrees of damage, the common ones are:
The occurrence of acute sharp pains at the site of attachment of ligaments, tendons to the bone, as well as at the site of muscle rupture;
The presence of bruising, hemorrhage into the surrounding tissues or the joint cavity (hemarthrosis), hematoma and swelling in the area of damage;
Dysfunction of a joint or limb, dysfunction of a damaged muscle.
Most often, the ligaments of the trochlear (ankle, knee, wrist), and less often the spherical joints are damaged.
Rendering emergency care in case of rupture of ligaments and tendons in the lesion, it is reduced to creating rest for the damaged area by applying a pressure bandage, splint or immobilization with the help of improvised means, injecting narcotic substances from a syringe tube in case of severe pain, to applying cold in the area of injury, to timely evacuation of victims in OPM.
In APM with severe pain, drugs should be injected intramuscularly, and 5-10 ml of a 1% solution of novocaine should be injected into the area of \u200b\u200bmaximum pain, irrigation of the injury site with chlorethyl should be carried out.
Treatment in a specialized hospital begins with resting the damaged area. With mild injuries, the immobilization period is 7-10 days, with medium injuries, an average of 21 days, and with severe injuries, with the presence of aggravating factors (exposure to penetrating radiation), at least 4-6 weeks. Immobilization of the injury site is achieved by applying standard splints, fixing bandages and plaster splints (circular bandages).
Surgical intervention with a complete rupture of muscles, ligaments and tendons consists in suturing damaged ligaments, tendons and muscles, followed by early therapeutic exercises (active and passive movements), massage, physiotherapy (dry heat during the period of immobilization, paraffin and mud applications after removal splints or plaster splints).
3. DISTRUCTIONS. THEIR TYPES AND SIGNS.
FIRST AID AND TREATMENT
A dislocation is a permanent displacement of the articular ends of one or more bones that form a joint, accompanied by damage. joint bag and liaison apparatus.
There are dislocations:
Complete, when the articular surfaces do not touch each other;
Incomplete, when the articular surfaces are in partial contact with each other (subluxation).
A dislocation is named after the displaced bone. If, for example, there was a dislocation in the shoulder joint, then it is called a dislocation of the shoulder.
Dislocations occur more often in joints that have the shape of a ball or block (shoulder, elbow, hip).
Depending on the causes of origin, dislocations are divided into:
traumatic;
Pathological;
Habitual;
Congenital.
Traumatic dislocations are much more common than other types (up to 90% of all dislocations). The cause is usually indirect trauma. For example, a dislocation in the shoulder or elbow joint occurs when you fall on the hand with the arm extended forward.
When the articular ends of the bones are displaced, a rupture of the joint capsule occurs, through which the head of the dislocated bone passes and injures the surrounding tissues.
Due to the unequal strength of different parts of the capsule of the joints and varying degrees strengthening the joints with muscles and ligaments; dislocation of the articular end of the bone occurs, as a rule, in certain parts of the joint.
So, dislocation of the shoulder is more often anterior and downward, dislocation of the hip - anterior and posterior, etc.
With gross violence, when large vessels and nerves are damaged simultaneously with dislocation, muscle crushing or bone fracture occurs, the dislocation is called complicated.
With a simultaneous breakdown of the skin, the dislocation is called open.
Pathological dislocations are relatively rare and occur as a result of any disease in the joint or its surrounding tissues (syphilis, tuberculosis, osteomyelitis, etc.).
Habitual dislocations are noted in those patients who, due to stretching and rupture of the joint capsule, have a tendency to re-dislocation. They can come with the slightest violence or even with an awkward movement.
Congenital dislocations are rare, they occur in the form of unilateral or bilateral dislocation in hip joint that occurs in the prenatal period as a result of improper or insufficient development of the articular surfaces. They come to light after the children begin to walk, in the form of lameness or duck gait.
Symptoms of dislocations are quite clear, in most cases helping to accurately diagnose:
Pain that worsens when trying to change the position of the limb resulting from a dislocation;
Dysfunction of the joint;
Springing resistance when trying to bring the limb to its previous normal position due to a sharp spastic contraction of the muscles surrounding the joint area;
Forced position of the limb, characteristic in some cases for damage to a particular joint; for example, with a dislocation in the shoulder joint, the victim keeps his arm bent at the elbow joint and slightly retracted away from the body;
Changing the configuration of the joint (depletion of the articular bag or an increase in the volume of the joint due to significant bleeding into the joint cavity and into the tissues surrounding the joint);
The presence of symptoms accompanying dislocation of the joint (swelling of the limb, impaired sensitivity and movement in the peripheral part of the injured limb as a result of damage to the main vessels and nerves).
The provision of emergency care in the lesion in case of dislocation begins with the immobilization of the injured limb using standard splints, improvised means or using a fixing bandage (the upper limb is fixed to the body in a position bent at a right angle in the elbow joint, the lower limb - in the position in what she was like at the time of medical care).
With open dislocations, the wound is closed with an aseptic bandage before immobilization.
The reduction of a dislocation in the lesion is not performed, because it is not always possible to accurately determine the presence of a dislocation, reduction without anesthesia can lead to the development of shock, reduction is a medical manipulation.
In the focus, with severe pain, drug injections are made, cold is applied to the joint area. Patients are evacuated to the emergency room. In case of dislocations in the joints of the upper extremities, the victims can follow to the place of loading onto transport on foot, in case of dislocations in the joints of the lower extremities, evacuation is carried out on a stretcher.
In the OPM, the dislocation is reduced. Before reduction, anesthesia is performed by introducing 40-50 ml of a 1% solution of novocaine into the joint cavity and 1-2 ml of a 2% solution of morphine (pantopon, promedol), they are administered 30 minutes before reduction intramuscularly or subcutaneously.
The reduction is made taking into account the anatomical and physiological characteristics damaged joint.
Failure to comply with this condition can lead to severe secondary injuries: fractures of limbs, ruptures of blood vessels, nerves.
Classic ways reduction of dislocations is based on achieving relaxation of the muscles in the area of the damaged joint by anesthesia, local anesthesia, the use of muscle relaxants in doses that do not turn off spontaneous breathing in the victim.
The methods of reduction of dislocations according to Kocher, Dzhanelidze, Hippocrates, etc. are common.
After the reduction of any dislocation, it is necessary to immobilize in order to create rest and prevent re-dislocation. The hand is fixed on the scarf with a Deso bandage, a splint or a plaster splint for a period of at least 7-10 days.
At the end of the reduction of the dislocation of the lower limb, immobilization is performed using a splint, a plaster splint, bed rest for a period of 15-30 days (depending on the nature of the dislocation and the degree of damage to surrounding tissues).
With any type of immobilization, massage is performed from the very first days, physiotherapy(careful, gradually increasing in the load active and passive movements in the joint), physiotherapy procedures.
4. POST-TRAUMATIC TOXICOSIS. SYMPTOMS, PECULIARITIES OF MEDICAL CARE AND TREATMENT
Post-traumatic toxicosis ("syndrome of prolonged tissue crushing", "disease prolonged compression", etc.) - a kind of clinical picture, which is the result of a long (over 4-6 hours) compression of soft tissues by the ground, structures of destroyed buildings and structures.
The severity of the lesion depends on many reasons, but especially on the location, extent of damage and the duration of compression.
With a significant destruction of soft tissues, a large amount of protein breakdown products of tissues is released, a long-term neuroreflex effect of the flow of pain impulses at the site of injury occurs - all this is an etiopathogenetic factor in the development of the clinical picture of post-traumatic toxicosis.
According to the clinical course, there are three periods of post-traumatic toxicosis:
Intermediate;
Late.
The early period begins from the moment of soft tissue compression, when the flow of pain impulses causes a reflex disturbance of blood circulation in the kidneys. This period lasts 2-3 days and is characterized by acute edema and dysfunction of the kidneys and blood circulation in tissues freed from compression.
Usually, 4-6 hours after release from compression, a sharp deterioration in the general condition occurs, thirst, vomiting, lethargy, sometimes excitement, apathy, body temperature rises to 39 ° C. The pulse is frequent, blood pressure drops. Skin purple-bluish, cold to the touch, often covered with blisters with a yellowish or bloody fluid. The pulsation is sharply weakened or completely undetectable due to a sharp swelling of the tissues. There are severe pains.
In severe forms of damage, death from intoxication and acute renal failure can occur.
In cases of a favorable course, a temporary improvement in the patient's condition may occur.
The interim period is characterized by the development of acute renal failure. Again there are pains, mainly in the lumbar region. The excretion of urine sharply decreases, the content of protein, urea, nitrogenous slags (azotemia) increases in the urine. There is repeated vomiting. Consciousness is disturbed. Swelling of the whole body develops rapidly. In the presence of radiation sickness, the prognosis becomes even more unfavorable.
The late period (from 10-12 days) is manifested by the subsiding of the phenomena of acute renal failure, the edema completely disappears, but the pain in places subjected to compression increases due to the development of traumatic neuritis. IN subcutaneous tissue and other tissues, depending on the depth and extent of damaged tissues, purulent foci, trophic ulcers, scars, contractures, etc. may occur.
The provision of first aid for post-traumatic toxicosis in the lesion begins with the release of the victim from compression and tight bandaging of the limb from the center to the periphery.
In the presence of wounds, it is necessary to apply an aseptic bandage. Immobilization of the limb is mandatory even in the absence of suspicion of bone fractures.
Drugs are injected subcutaneously or intramuscularly. Antishock therapy is carried out in the OPM:
Case novocaine blockade above the affected areas, perirenal novocaine blockade, novocaine blockade of the main arterial trunks;
Placing an injured limb with ice packs;
Injections of cardiac agents and substances that stimulate respiration, intravenous administration of 10-20 ml of a 10% solution of calcium chloride;
First, drip intravenous injection of 100-150 ml of a 0.25% solution of novocaine, followed by the introduction of up to 2-3 liters of blood-substituting anti-shock solutions: polyglucin, plasma, complex saline anti-shock solutions, 5% glucose solution, 2% bicarbonate soda solution (in order to reduce intoxication body by toxic products of tissue decay and stabilization of hemodynamic parameters);
The introduction of antibiotics (prevention of various suppurative complications), antitetanus sera and tetanus toxoid;
Surgical interventions according to vital indications (amputation of a limb with multiple fractures in cases of its impossible preservation).
Anti-shock measures in full and the fight against intoxication of the body continue in the profiled hospital of the suburban area.
After normalization of hemodynamic parameters in order to eliminate extensive edema and increase intoxication, wide and deep dissections of the affected tissues are performed, followed by the application of a bandage with hypertonic saline sodium chloride.
To combat toxemia, it is advisable to continue drip intravenous infusions blood substitutes, polyglucin, glucose, 20% alcohol solution, 0.25% novocaine solution, 10-20 ml of 10% calcium chloride solution, abundant bloodletting (up to 1500 ml) with the same abundant transfusion of freshly citrated blood with a shelf life of not more than 5 days. The amount of fluid administered in various ways is controlled by hourly or daily diuresis.
Effective in the treatment of toxicosis are:
Hormones (ACTH, hydrocortisone);
Vitamins (A, C, PP, B1, B2, B6, B12, B15, E);
Antibiotics.
If the medical institution has the appropriate personnel and equipment in better ways treatment of kidney failure are peritoneal dialysis (permanent or intermittent washing of the abdominal cavity) and hemodialysis using an artificial kidney machine, as well as intestinal dialysis (when washing fluids enter the intestine through a thin rubber tube inserted through the nose, esophagus, stomach directly into small intestine).
In the late period of toxicosis occurring against the background of radiation sickness, the main attention is paid to the treatment of radiation sickness, as well as the surgical and physiotherapeutic treatment of paralysis, wounds, ulcers and abscesses.
5. DROWNING. ASPHYXIA DURING CLASSES AND EARTH FALLING. FIRST AID
Drowning is the most common cause of death among various injuries co fatal.
True drowning begins with an intense struggle for life. Excessive ventilation during diving disrupts the frequency, rhythm and depth of breathing. A large amount of water enters the lungs, which leads to a violation of gas exchange.
Being absorbed into the blood, water causes an increase in the amount of blood and the destruction of red blood cells (hemolysis). Hemolyzed blood loses the ability to carry O 2 to the tissues, which leads to their oxygen starvation (hypoxia).
Respiratory failure inevitably leads to circulatory failure. Due to the increase in the amount of circulating blood, the heart cannot cope with the load, the blood flow slows down, venous pressure rises, congestion occurs.
Clinically, true drowning is manifested by the absence or apparent insufficiency of respiratory movements, purple-blue coloration of the skin, especially the auricles, fingertips and mucous membranes of the lips. This coloration is due to superficial vessels are filled with blood containing an excessive amount of CO 2 (hypercapnia).
The veins of the head, neck, limbs are overflowing with blood and therefore stand out sharply on the surface of the skin. The face is edematous, a large amount of foam is discharged from the mouth and nose, which is often colored with blood.
In 10-15% of cases, another type is observed respiratory disorders. Drowning is preceded by inhibition of the central nervous system under the influence of alcohol intoxication, fright, trauma to the skull, hitting the water. A similar situation can arise when diving without scuba gear to great depths.
Hypocapnia (after preliminary hyperventilation) allows you to lengthen the breath hold so that the urge to inhale appears too late, when a critical decrease in the supply of O 2 leads to loss of consciousness.
In response to hitting Airways the first portion of water occurs laryngospasm, which can prevent further flow of water until the terminal phase. Water is swallowed in large quantities into the stomach, which creates the risk of vomiting, aspiration of vomit and pneumonia. This type of respiratory disturbance is, in fact, a simple asphyxia. The protein of the edematous fluid during pseudo-respiratory movements forms a persistent fluffy foam that fills the mouth and nose.
In 10-15% of all cases, reflex cardiac arrest occurs even before the period of critical respiratory disorders. Such syncopal drowning is facilitated by emotional stress, exposure to cold water.
This type of drowning is characterized by a sharp pallor of the skin, mucous membranes due to generalized vascular spasm. The cavities of the mouth and nose are free, foamy fluid is not released from the airways.
During collapses and falling asleep with earth, pulmonary gas exchange is also disturbed as a result of the penetration of dust, earth, sand into the lungs. Violations of gas exchange lead to asphyxia.
The main task in first aid is to restore pulmonary ventilation and maintain blood circulation.
Artificial ventilation of the lungs is begun, if possible, already during the extraction of the drowned person from the water and continues without interruption on the shore.
At true drowning success is possible if the stay under water does not exceed 3-6 minutes. For the syncope type of drowning, the period of stay under water, in which the effect is possible, can be 10-12 minutes. When drowning in cold water, the protective effect of hypothermia is manifested, which makes it possible to achieve success even after 20 minutes or more of being under water.
Artificial respiration must be done in the mouth-to-mouth or mouth-to-nose manner. Simultaneously with ID, an indirect heart massage should also be done. ID must be done until it appears spontaneous breathing(or cadaveric spots and rigor mortis, i.e. clear signs biological death). At the same time, measures are taken to warm the victim (especially in the cold season). As soon as circumstances allow, it is necessary to remove wet clothes from him, wipe his skin dry and wrap him in a dry sheet, blanket or dress in dry clothes.
After the restoration of cardiac activity and respiration, gentle transportation to a medical facility is carried out, accompanied by a nurse or other person who knows how to carry out resuscitation.
First aid for injuries
General concept of closed and open damage. The concept of a wound, the danger of injury (bleeding, contamination of the wound, damage to vital organs).
Penetrating wounds of the skull, chest, abdomen.
The concept of asepsis. Rules for handling sterile material.
The concept of antiseptic. Primary bandage.
Bandages on the head and neck, on the eyes, forehead, ear, hairy part head, lower jaw, chin.
The imposition of bandages in the order of self-help and mutual assistance. Mesh-tubular bandages.
Bandages on the chest, abdomen, perineum.
General concept of closed and open damage. The concept of a wound, the danger of injury (bleeding, contamination of the wound, damage to vital organs)
General concepts of closed and open damage
In emergencies, people are often injured.
Injury is a violation of the integrity and function of organs or tissues as a result of external influence(physical, chemical, mental), causing anatomical or physiological disorders in tissues or organs, which are accompanied by a local and general reaction of the body.
Depending on the impact mechanism distinguish the following types of injuries:
acoustic,
household,
closed,
open,
production,
generic,
combined,
combined,
Craniocerebral.
We will analyze open and closed injuries.
Closed injuries- this is damage to human organs and tissues without violating the integrity of the skin and its mucous membranes
open injury - these are injuries with a violation of the integrity of the surface of the human body (skin and mucous membranes). Such injuries are called wounds.
Thus : wound is a violation of the integrity of the skin, mucous membrane or organs of the body.
According to the degree of penetration, the wounds are divided into:
penetrating - with damage by a wounding projectile to internal organs (heart, lungs, stomach, intestines, liver, kidneys, uterus, bladder etc.);
non-penetrating- without damage to internal organs.
In addition, wounds can be:
superficial - shallow, when only one skin is damaged;
deep - exciting subcutaneous tissues, muscles, bones. Depending on the size, the wounds are small, medium and extensive.
According to the method of occurrence, there are wounds:
1) cut - applied with a sharp object, most often with a knife, razor, glass, etc.; they are characterized by smooth edges and bleed moderately or heavily;
2 ) chopped - caused by a descending object with a sharp edge, in their appearance resemble cut wounds. but differ in greater depth;
3) chipped - inflicted with a knife, dagger, nail, pitchfork or other sharp objects; they are narrow and deep wounds;
4) bruised - arise under the influence of a blunt injuring instrument of large mass or with high speed, when the body falls or is squeezed, the edges of the wound are uneven, bleeding is weak. Their shape is irregular (winding, "star-shaped"), the edges are uneven. It is observed with autotrauma, compression by heavy objects. Usually such wounds are heavily contaminated. The presence in the wound of a large number of dead, bruised tissues makes these wounds especially dangerous in relation to the development of infection. A variety of bruised wounds are lacerated and torn-bruised wounds.
5) torn - resulting from rupture of the skin during its tension; the edges of such wounds are uneven, the bleeding is weak, there is significant pain;
6) bitten- in appearance resembling bruised or lacerations, often, along with the saliva of rabid animals, they get an infection;
7) firearms- caused by bullets and shell fragments; these wounds are characterized by the presence of a small rounded inlet - the point of entry of the bullet, and a large exit hole - the point of exit of the bullet from the body; if the bullet penetrates the body and has two holes, then in this case they speak of a through wound; when a bullet gets stuck in the body, they speak of a blind wound.
8) Scalped Wounds- wounds in which detachment of the skin and fiber is observed with their complete separation from the underlying tissues. Part of the skin is usually lost.
The danger of wounds is the occurrence of shock, the formation of an entrance gate for infections, blood loss.
Sport, in the broad sense of the term, is a competitively organized physical or mental activity of people. Its main goal is to maintain or improve certain physical or mental skills. Besides sport games are entertainment for both participants in the process and for spectators.
General characteristics of sports injuries.
The concept of open and closed injuries, light injuries, moderate and severe injuries
Trauma is a violation of the anatomical integrity of tissues or organs with a disorder in their function, due to the influence of various environmental factors (mechanical, thermal, chemical, radiation, etc.).
A sports injury is a violation of the anatomical integrity of tissues or organs with a breakdown in their function, due to the influence of a mechanical factor that exceeds the physiological strength of the tissue during physical education and sports.
There are the following types of injuries:
- open (with them the skin is damaged);
- closed (with them the skin remains intact).
According to the severity of the injury are divided into:
- a) lungs are injuries that do not cause significant disturbances in the athlete's body and do not cause loss of general and sports performance;
- b) medium severity - these are injuries that cause significant disturbances in the athlete's body and cause loss of general and sports performance;
- c) severe - these are injuries that cause pronounced impairment of the health of the athlete, when hospitalization is necessary or long-term treatment on an outpatient basis.
In sports injuries, minor injuries predominate; also, sports injuries are characterized by a predominance of closed injuries: bruises, sprains of muscles and ligaments. Injuries in various types sports are different.
Pre-hospital care is care provided before the intervention of a doctor. It is divided into the first (self-help, mutual assistance) and medical, provided by paramedical personnel.
In most cases, first aid begins with the removal of clothes and shoes from the victim, partially or completely. In this case, additional traumatization of the victim must not be allowed; for this, the following rules must be observed:
- It is impossible to remove clothes and shoes from the victim completely without special need, especially in the cold season. In this situation, only the part of the body where the injury occurred is released.
- The clothes are removed from the victim, starting from the healthy side.
- If the clothing is stuck to the wound, then the fabric should not be torn off, it should be cut around the wound.
- At heavy bleeding you should quickly cut the clothes and, having unfolded, free the place of damage.
- In case of injuries to the shin and foot, the shoes must be cut along the seam of the heel, and only then removed, releasing the heel first.
- When removing clothes or shoes from an injured limb, an assistant must hold the injured limb.
Skin damage
Skin injuries include:
- abrasions;
- abrasions;
- wounds.
Abrasion is damage to the skin that occurs as a result of prolonged friction of a certain area of it on clothing, shoes, equipment, or contact of two areas of the skin.
An abrasion is a superficial injury to the skin that occurs when it is sharply rubbed against a hard object, when it slips or falls on a hard surface. Abrasions are accompanied by pain, a burning sensation, as the damage heals, a feeling of "tightness" appears.
A wound is tissue damage with a violation of the integrity of the skin or mucous membrane.
Wounds are one of the most frequent consequences of mechanical injuries. Wounds are dangerous due to the possibility of bleeding, infection of the wound and the likelihood of damage to deeper tissues and organs.
The main signs of a wound are:
- a) bleeding
- b) divergence of the edges of the wound;
- c) pain;
- d) dysfunction.
Pain, on the one hand, is an “internal distress signal”, and, on the other hand, pain is one of the main reasons for the deterioration of the general condition of the victim, impaired vital functions and the development of severe complications. Therefore, the fight against pain is one of the main tasks of first aid.
To eliminate or reduce pain, use the following:
- Closure of wounds with sterile dressings, which provides protection of damaged tissues from the irritating effect of air, additional ingress foreign bodies and excludes traumatization of damaged tissues by clothing, stretchers.
- Immobilization eliminates additional irritation of nerve endings in the area of damage.
- Proper placement on a stretcher relieves excessive muscle tension, which can adversely affect injured tissues.
- The application of cold (ice) relieves the incipient inflammation in damaged tissues.
- Careful carrying or transportation of the victim, excluding shocks and shaking.
- The use of available painkillers - analgin, aspirin.
Asepsis is a set of measures aimed at preventing the penetration of microorganisms into the wound and the body as a whole.
Antiseptic is a complex of therapeutic and preventive measures aimed at the elimination of microorganisms in the wound and the body as a whole.
The healing of skin lesions occurs due to the connective tissue and is accompanied by the regeneration of the epithelium. Light damage to the epidermis of the skin is completely restored due to the regeneration of the epidermis.
Regeneration is the process of restoring destroyed or lost tissues.
Wound healing is a typical process of pathological tissue regeneration that occurs after tissue damage.
The concept of bruises
A bruise is a closed mechanical damage to soft tissues or organs without a visible violation of the anatomical integrity.
Classification of bruises depending on the severity of damage:
- 1st degree - slight damage caused by a small blow, no edema, no restriction of movement, slight soreness;
- 2nd degree - damage that caused bleeding in the tissue, restriction of movement, movement causes pain, soreness at the site of damage, may be muscle spasm;
- 3rd degree - severe injury, strong pain, swelling, muscle spasm, there may be deformation, discoloration of the skin.
The concept of damage to muscles and ligaments
Stretching of muscles, tendons or ligaments.
Classification of sprains according to the severity of the injury:
- 1st degree - this is stretching or rupture of less than 25% of the fibers of the muscles, tendons or ligaments, accompanied by slight soreness, slight swelling, there are no restrictions on the mobility of muscles or joints;
- 2nd degree - this is a rupture of 25 to 50% of all fibers, accompanied by edema, bruising, painful sensitivity, some limitation of muscle mobility or joint instability;
- 3rd degree - from 50% to complete rupture of all fibers, accompanied by swelling, instability, rupture in the muscles can be felt through the skin.
Repeated prolonged stretching under the same load changes the structure and properties of the stretched tissues and can cause stretching or tearing. At the same time, the extensibility of tissues increases, and elasticity, recovery after the cessation of stretching decreases. This is observed with repeated sprains of the ligamentous apparatus of the joints.
"PLDP" - "Rest, Ice, Pressure and Elevation" - a method of self-treatment of sports injuries
The most important component of the treatment and self-treatment of almost all sports injuries is RICE. PLDP is Peace, Ice, Pressure, Rise. Treatment must begin immediately after injury. The use of PLDP in the first 15-20 minutes after injury for several days or even weeks accelerates the recovery of the athlete. The use of PLDP during the first 24 hours after injury reduces the rehabilitation time by 50-70%.
Early use of PLDP makes it possible to reduce and stop inflammation, which, on the one hand, is a local protective and adaptive process and acts as a restriction on the movement of the damaged area, and, on the other hand, delays recovery. And the more the initial inflammation is inhibited, the faster the recovery of the athlete will come.
- Rest - sports training after injury should be stopped. In the period from 24 to 72 hours (depending on the severity of the damage), complete immobilization is necessary for the use of the remaining components of PLDP.
Immobilization is the creation of immobility or a decrease in the mobility of body parts in case of damage.
Immobilization is necessary at the initial stage of injury management in order to provide rest, ice application, pressure bandages, and elevation.
It must be remembered that after the completion of the initial period, rest should be relative, since complete immobilization worsens the health of the athlete due to the occurrence of muscle atrophy, joint stiffness and a decrease in cardiovascular endurance.
On the contrary, early mobilization accelerates healing processes, stimulates the growth and reunification of damaged tissues, prevents the formation of adhesions in the joint capsules and helps maintain coordination and sports-related skills, trains the cardiovascular system, and accelerates a successful return to sports.
- Ice - cooling the injury site reduces signs of inflammation (swelling, pain, redness).
Treatment with ice is called cryotherapy.
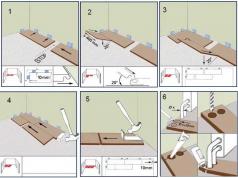
The most effective application of ice in the first 10-15 minutes after the injury. Method of application of ice: the damaged area is covered with a wet towel and ice is applied to it. The towel must always be wet, as a dry towel will insulate the skin from cooling. When using ice, there will be a cold, burning sensation, followed by pain and numbness.
A very effective method of cooling, called "ice massage". To do this, water is frozen in a plastic disposable cup, then the upper edge of the cup is torn off, while the bottom of the cup remains as an insulating gasket, allowing the athlete to massage the damaged area with slow circular movements. This type massage combines two elements of PLDP - the application of ice and pressure.
Ice should be applied as often as possible in the first 72 hours. In case of minor injuries, it is sufficient to apply ice during the first 24 hours. Ice is applied to the injury site for a period of 10 to 30 minutes at a time, the intervals between applications are 30-45 minutes.
- Pressure - compression of the injury site, the pressure should be constant and moderate. It is necessary to reduce swelling at the site of injury.
Compression of the injury site can be performed during and outside of cooling.
During cooling, pressure can be applied by applying ice massage, or by applying an ice pack and a pressure bandage to the injured limb.
In the period when cooling is not carried out, you can use an elastic bandage for a pressure bandage. An elastic bandage is applied 2-3 cm below the injury site and bandaged up in a spiral, overlapping turns, starting with a uniform greater compression, and then more freely. It is necessary to periodically check the color of the skin, temperature and sensitivity at the site of injury, so as not to pinch the nerve or artery.
- Elevation is necessary to prevent the accumulation of fluid formed during inflammation. To do this, you need to keep the site of damage in an elevated position from 24 to 72 hours. For example, an athlete with a lower limb injury should lie down using a pillow to elevate the injured limb.
PLDP is a method for first aid and the initial stage of treatment. If within 24-48 hours the symptoms of damage to muscles, tendons, ligaments do not decrease or the pain becomes stronger, then you should consult a doctor.
Fractures open and closed
Fractures are damage to the bone with a violation of its integrity. With a fracture, there is a deformation or change in the shape of the bone, swelling, pain, sensitivity to touch.
There are traumatic and pathological fractures. There are also fractures:
- Closed (when closed fracture the integrity of the skin is not affected).
First aid for a closed fracture is to carry out immobilization, apply cold (ice) to the injury site, ensure an elevated position of the injured limb and hospitalize the victim in the trauma department.
- open (with open fracture the integrity of the skin is broken and the ends of broken bones come out through the skin).
First aid for an open fracture is to stop bleeding, apply a sterile bandage, do not try to set bone fragments in place, immobilize, apply cold (ice) to the injury site, ensure an elevated position of the injured limb and urgently hospitalize the victim in a specialized department.
Immobilization is immobilization. Immobilization provides rest for the injured limb, eliminates additional trauma and reduces pain, and is a prevention of traumatic shock.
Immobilization rules:
- a) for reliable immobilization, two joints should be immobilized - above and below the fracture site;
- b) before splinting, it is necessary to put a soft cloth or a layer of cotton under the bony protrusions that are determined under the skin;
- c) it is necessary to apply tires carefully, without causing additional injuries to the victim;
- d) the immobilizing means should be durable and as light as possible.
Bleeding, types, signs. Ways to stop bleeding
Bleeding is the outflow of blood from blood vessels in violation of the integrity or permeability of their walls. Bleeding varies in origin:
- traumatic;
- non-traumatic.
Bleeding is divided depending on where the blood is poured from the damaged vessel into:
- outdoor;
- internal.
There are also bleeding:
- A. Arterial bleeding.
With arterial bleeding, scarlet blood flows out in a rapidly pulsating or gushing stream. A way to temporarily stop bleeding is to apply a tourniquet and urgent hospitalization of the victim in a hospital.
Rules for applying a tourniquet for arterial bleeding:
- the limb is lifted up before applying the tourniquet;
- before applying the tourniquet, the bleeding vessel above the wound is pressed with a finger, which allows you to prepare for the application of the tourniquet without too much haste. For the same purpose, it is possible to temporarily bend the limb to the limit in the joint overlying in relation to the wound;
- the tourniquet is applied above the wound at a distance of 5-7 cm from its upper edge;
- a tissue is preliminarily applied to the place of application of the tourniquet;
- the tourniquet should be tightened only until the bleeding stops;
- under the tourniquet it is necessary to put a note indicating the time of its application;
- to provide nutrition to the limb through intact vessels, the tourniquet must be loosened after 30 minutes, after pressing the damaged vessel above the wound with a finger.
- B. Venous bleeding.
With venous bleeding, the blood is dark, flows out in a continuous stream of dark red color. A way to temporarily stop bleeding is the imposition of a pressure bandage and urgent hospitalization of the victim in a hospital.
Rules for applying a pressure bandage:
- a sterile tissue is applied to the bleeding wound, a dense roller of bandage or cotton wool is placed on top of it, which is tightly bandaged;
- a sign of a correctly applied pressure bandage is the cessation of bleeding (the bandage does not get wet).
A pressure bandage with stopped bleeding can not be removed until the victim arrives at a medical facility.
- B. Capillary bleeding.
With capillary bleeding, blood flows out slowly in a spreading spot or rare drops. The method of temporary stopping is the imposition of a pressure bandage on the wound.
- G. Parenchymal bleeding.
Parenchymal - is internal bleeding from parenchymal organs.
First aid for parenchymal bleeding - cold (ice) on the abdomen, urgent hospitalization of the victim in a hospital.
Blood loss is a pathological process that occurs as a result of damage to blood vessels and the loss of part of the blood, characterized by a number of pathological and adaptive reactions. The cause of blood loss is bleeding.
A hemorrhage is an accumulation of outflowing blood in tissues or body cavities; hemorrhage is always the result of bleeding.
A decrease in the volume of circulating blood resulting from blood loss serves as a trigger mechanism that causes compensatory and pathological changes in the body.
Blood loss of more than 15 ml/kg of body weight (or more than 25% of the circulating blood volume) causes shock, and a simultaneous loss of more than half of the circulating blood volume is fatal.
There are the following stages of blood loss:
- Stage 1 - initial;
- Stage 2 - compensation;
- Stage 3 - terminal.
Traumatic dislocations
Dislocations are a persistent displacement of two articulating bones, in which their mutual contact is disturbed. With complete dislocation:
- the head of the bone comes out of the articular cavity or the bones that form the joint diverge to the sides.
With incomplete dislocation (subluxation), partial contact of the articular surfaces of the articulating bones is preserved.
Each dislocation is accompanied by a more or less pronounced bruise, sprain and partial rupture of the muscles and surrounding tissues. For most dislocations, a rupture of the articular bag is characteristic. Ruptures of small vessels always accompany traumatic dislocation, which causes intra-articular hemorrhages. Each dislocation causes a reflex contraction of the muscles, which determines the retention of the dislocated bone in a new position.
A characteristic feature for all dislocations is a change in the shape of the joint due to the displacement of the ends of the dislocated bones.
The most important sign of dislocation is dysfunction. Active movements are impossible or possible to a small extent, passive movements are also limited.
First aid consists in applying ice to the injury site, fixing the injured area with an elastic bandage, elevating the injured part of the body and urgent delivery of the athlete to the trauma department.
Reduction of dislocation refers to urgent measures, the more time passes from the moment of injury to reduction of dislocation, the more difficult it is to implement.
It must be remembered that it is impossible to set a dislocation on your own.
Brain concussion. Classification of traumatic brain injury
Traumatic brain injury is damage to the skull and brain as a result of mechanical impact.
Traumatic brain injuries (TBI) are divided into:
- 1. Closed TBI.
A closed craniocerebral injury is a brain injury in which the soft tissues and bones of the skull remain intact or are partially damaged (soft tissue wounds).
- 2. Open TBI.
An open craniocerebral injury is damage to the soft tissues of the head with a violation of the integrity of the aponeurosis, as well as fractures of the bones of the skull.
A concussion is a form of closed brain injury characterized by the reversibility of clinical symptoms. It occurs during shock movements of the contents of the cranium.
A brain contusion is a consequence of a direct trauma to the brain on the inner wall of the bones of the skull according to the mechanism of impact and counter-impact. This is a more severe brain injury.
Brain compression is one of the most dangerous forms closed craniocerebral injury. Compression of the brain in a closed craniocerebral injury is caused by bleeding due to damage to the arterial and venous vessels of the meninges.
A feature of brain compression is that the symptoms of compression do not appear immediately at the time of injury, but develop gradually (there is a so-called light period of time that lasts from one to several weeks).
Special attention should be paid to craniocerebral injuries in boxing.
Groggy is a condition that develops as a result of concussion vestibular apparatus with a strong blow to the lower jaw. The main symptom is dizziness.
Knockout is an acute emerging pathological condition characterized by a brief loss of consciousness.
Knockdown is a weakened expression of a knockout, consciousness is preserved, only loss of orientation, lack of coordination, dizziness, tinnitus are observed.
First aid for a closed craniocerebral injury - cold on the head (ice) and immediate hospitalization in a specialized medical facility.
The concept of fatigue and overwork
Fatigue is a temporary decrease in the functional capabilities of the body, caused by intensive or prolonged work and is expressed in a decrease in performance.
Fatigue is a condition that occurs under the influence of muscle activity, fatigue cannot be considered pathological, harmful to the athlete's body. With a slight degree of fatigue, metabolism increases, muscle tone increases, and the intensity of recovery processes increases. The effect of training is impossible without fatigue.
Overfatigue is a condition that occurs when the phenomena of fatigue are layered, when the athlete's body does not recover from one activity or competition to another for a certain time.
Overfatigue manifests itself in a longer than usual persistence of feeling tired after exercise, deterioration in well-being, sleep, increased fatigue, and unstable mood. At the same time, sports performance remains without significant changes or slightly decreases, difficulties may arise in the formation of new motor skills, in solving complex tactical problems, and errors in technique may also occur.
Objectively, it is possible to determine a decrease in strength indicators, deterioration in coordination, an increase in the recovery period after exercise.
Chronic physical stress
Overvoltage is a sharp decrease in the functional state of the body, caused by a violation of the processes of the nervous and humoral regulation various functions, metabolic processes and homeostasis. It is caused by a discrepancy between the body's needs for energy resources during physical activity and the functional capabilities to satisfy them.
Chronic physical overstrain is a violation of the function of the organs and systems of the body of athletes due to the impact of inadequate loads - both physical and mental. At the same time, the ratio of these loads is very important, since their joint negative impact can manifest itself even at relatively small values of each of them.
The main clinical forms of chronic physical overstrain:
- Chronic overexertion of the central nervous system (overtraining).
- chronic overexertion of cardio-vascular system.
- Chronic overexertion of the blood system.
- Chronic overvoltage of the non-specific protection system and immune system.
- Chronic overexertion of the digestive system.
- Chronic overexertion of the urinary system.
- Chronic physical overstrain of the musculoskeletal system.
Chronic physical overexertion of the central nervous system (overtraining)
Overtraining is a pathological state of the athlete's body, manifested by disadaptation, a violation of the level of functional readiness achieved during training, a change in the regulation of the body systems, the optimal relationship between the cerebral cortex and the underlying parts of the nervous system, the motor apparatus and internal organs.
Overtraining is based on overstrain of the processes of excitation, inhibition or their mobility in the cerebral cortex. Therefore, the pathogenesis of overtraining is similar to the pathogenesis of neurosis, in connection with this, the leading signs of this condition are changes in the central nervous system. Also great value In the pathogenesis of overtraining, the endocrine system, primarily the pituitary gland and the adrenal cortex, has.
According to G. Selye (1960), under the action of a stressor (strong stimulus), a general adaptation syndrome, or stress, develops in the body, during which the activity of the anterior pituitary gland and adrenal glands increases. These changes endocrine system determine the development of adaptive reactions in the body to intense muscle activity. However, chronic physical overstrain can lead to depletion of the adrenal cortex and, accordingly, to a violation of the adaptive reactions previously developed in the body.
With overtraining, the functional state of the underlying parts of the central nervous system also changes, which is manifested by various visceral disorders.
Overtraining develops in athletes due to chronic physical overstrain.
Overtraining can occur in an athlete:
- With an excessive training load (a sharp increase in the volume of training and their intensity) when the adaptive capabilities of the athlete's body are exceeded.
- When the competition schedule is too tight without adequate recovery intervals.
- With insufficient recovery, which is noted with a sharp intensification of the training process.
- In case of an increase in stress factors such as insufficient sleep and malnutrition.
Overtraining can occur during any period of training, however, in the preparatory period, it occurs very rarely. The probability of its development gradually increases as the state of fitness improves, i.e. during the main training period.
The state of overtraining includes the state of training, since in order to overtrain, it is necessary, as a rule, to have a high level of fitness.
Athlete with high level preparation and strong motivation is constantly on the fine line between the optimal level of training and "overtraining".
Especially often, overtraining occurs in athletes when they approach their previously achieved individual results and strive to surpass them, that is, when an athlete approaches the limit of his adaptive capabilities.
Overtraining can be difficult to distinguish from the fatigue that accompanies an intense training load. However, adequate recovery leads to an increase in the state of fitness and an increase in athletic performance. Insufficient recovery is accompanied by a constant feeling of fatigue, the athlete makes more effort in training, the results of training and competition are reduced.
L.A. Butchenko identifies 3 stages of overtraining (indistinctly demarcated from each other):
- there are no complaints, sleep disturbance is possible - poor falling asleep, frequent awakenings;
- lack of growth in sports results, less often there is a decrease in sports results.
Objectively:
- there is a deterioration in the adaptability of the cardiovascular system to high-speed loads (after a 15-second run, atypical reactions appear instead of the normotonic type of reaction);
- there is a disorder of the finest motor coordinations.
At this stage, in order to improve sports performance, the athlete increases the training load and this leads to the progression of overtraining.
- 2nd stage of overtraining: Numerous complaints appear:
- drowsiness, sleep disorders progress - the time to fall asleep lengthens, sleep becomes superficial, restless, with frequent dreams, often of a nightmarish nature, sleep does not provide the necessary rest and recuperation;
- apathy, lethargy, irritability, loss of appetite;
- discomfort in the region of the heart;
- fatigue, slow working out, loss of muscle acuity;
- the appearance of inadequate reactions at the end of complex exercise;
- reluctance to exercise.
Objectively:
- pallor of the face, bluish color of the lips, blueness under the eyes, sunken eyes, marbling of the skin (increased pattern of the venous network on pale skin);
- violation of the activity of the nervous system is manifested in changes in the daily periodicity of functions and the daily stereotype. As a result, the maximum increase in all functional indicators is noted in an athlete not during the hours in which he usually trains, but late in the evening or early in the morning when he does not train;
- there is a disorder of coordination of movements;
- the nature of the bioelectric activity of the brain changes;
- on the part of the cardiovascular system, there is an inadequate reaction (too large) to physical exertion, a slowdown in the recovery period after them, a violation of the rhythm of cardiac activity, a deterioration in the adaptation of the cardiovascular system to endurance loads (the appearance of atypical reactions after a 3-minute run). At rest, instead of moderate bradycardia and normal pressure, there is tachycardia and an increase in blood pressure or a sharp bradycardia and a decrease in blood pressure;
- violation of the functional state of the respiratory system - a decrease in VC at rest, a decrease in MVL;
- an increase in basal metabolism, a violation of carbohydrate metabolism - a decrease in the amount of glucose in the blood at rest;
- weight loss (due to increased protein breakdown in the body), a negative nitrogen balance is detected;
- increased sweating;
- violation menstrual function in athletes;
- violation of potency in athletes;
- reduction, in particular, resistance to infectious diseases;
- decrease in strength and elasticity of muscles, elasticity of ligaments, which contributes to the occurrence of sports injuries.
Sports performance continues to decline. 3rd stage of overtraining:
neurasthenia develops. There are hypersthenic and hyposthenic forms of neurasthenia.
The hypersthenic form is a consequence of the weakening of the inhibitory process, the hyposthenic form is due to an overstrain of the excitatory process in the cerebral cortex.
Clinical manifestations of the hypersthenic form of neurasthenia are increased nervous excitability, a feeling of fatigue, fatigue, general weakness, and insomnia.
Clinical manifestations of the hyposthenic form of neurasthenia are general weakness, exhaustion, apathy, fatigue, daytime drowsiness.
Asthenia is a condition characterized by increased fatigue, frequent mood swings, sleep disturbance, etc.
The treatment of overtraining will be successful only if all the causes that caused it are eliminated.
1st stage of overtraining:
- participation in competitions should be prohibited (it makes no sense to show a bad result);
- change the training regimen for 2-4 weeks (general physical training regimen with a small load);
- treatment must be started as early as possible, since the 1st stage is treated successfully, and the 3rd stage is unsuccessful.
2nd stage of overtraining:
- training sessions are canceled for 1-2 weeks and replaced with active rest;
- further 1-2 months - general physical training with a gradual inclusion of the usual training regimen;
3rd stage of overtraining:
- treatment in a hospital;
- then leisure;
- gradual inclusion in the training mode within 2-3 months;
- exclude participation in competitions.
Overtraining of the 1st stage is eliminated without consequences for the athlete.
Overtraining of the 2nd and especially the 3rd stage can lead to prolonged decline sports performance.
Prevention:
- to prevent the participation of athletes in training and competitions in a painful condition;
- it is necessary to sanitize foci of chronic infection;
- it is necessary in a state of "sports form" to alternate intense training loads with reduced ones, especially after the athlete participates in competitions;
- the modes of training, rest, study, nutrition should be optimized.
Chronic physical overexertion of the cardiovascular system
Chronic physical overstrain of the cardiovascular system has 4 variants of the course:
- 1) dystrophic;
- 2) arrhythmic;
- 3) hypertonic;
- 4) hypotonic.
1. Dystrophic variant.
Myocardial dystrophy (myocardial repolarization disorder syndrome) is a metabolic disorder of the myocardium due to chronic physical overstrain.
Classification A.G. Dembo:
- Stage 1 - a decrease in the T wave.
- Stage 2 - biphasic T wave.
- Stage 3 - negative prong T.
Myocardial dystrophy is a metabolic disorder of the myocardium.
2. Arrhythmic variant.
Arrhythmias occur in athletes 2-3 times more often than in non-athletes. The greatest differences are noted in the frequency of arrhythmias associated with the suppression of the sinus node. Only evidence of the absence of heart damage and extracardiac causes (osteochondrosis, foci of chronic infection, etc.) makes it possible to associate heart rhythm disturbances with inadequate physical activity.
In sports medicine, even relatively harmless arrhythmias require special attention, because at physical activity they can provoke the development of severe disorders.
3. Hypotonic variant.
It is most typical for women, often found in highly qualified athletes.
Chronic physical overexertion of the blood system
Chronic physical overstrain of the blood system is the occurrence of anemia in athletes.
Anemia is a pathological condition characterized by a decrease in the number of red blood cells or hemoglobin content per unit volume of blood due to their general decrease in the body.
Athletes are more likely to develop iron deficiency anemia.
Iron deficiency anemia is an anemia caused by iron deficiency in the body.
Most often, anemia is recorded in runners and runners for long and extra long distances.
Anemia affects the vital activity of the body, oxygen starvation of organs and tissues is observed - hypoxia, dystrophy develops.
Chronic physical overstrain of the non-specific defense system and the immune system
Immunological reactivity of athletes varies depending on physical activity. R.S. Suzdalnitsky and V.A. Levando (2003) proposed a classification of the dynamics of changes in the immune system of athletes, which includes 4 phases:
- i - mobilization phase;
- i - compensation phase;
- i - phase of decompensation;
- I am the recovery phase.
- The mobilization phase is characterized by an increase in immunological parameters, indicating a general mobilization of physiological reserves. The incidence of acute respiratory infections is reduced to a minimum, overall health is improving, working capacity is growing.
- The compensation phase is noted during the increase in the intensity of the load, there is an increase in some immunological parameters while reducing others. The incidence does not differ from the incidence in the first phase, due to the pronounced mobilization of immunological mechanisms.
- The decompensation phase is observed during the period of high loads - 80-90% of the maximum with a large amount of work. There is a sharp decrease in all immunological parameters. The physical reserves of the immune system are on the verge of exhaustion. The incidence in this phase reaches a peak. There is a secondary immunodeficiency.
- The recovery phase is noted in the post-competition period, at the time of load reduction. Immunological indicators gradually return to normal.
Chronic physical overexertion of the digestive system
Chronic physical overstrain of the digestive system is the result of a violation of the regulatory role of the central nervous system or hidden pathological processes. For the development of chronic overstrain of the digestive system, prolonged exposure to inadequate loads is required.
Chronic physical overstrain of the digestive system can be represented by two syndromes:
- dyspeptic and hepatic pain.
- Dyspeptic syndrome is manifested by vomiting during or immediately after a single, usually long-term load that exceeds the functional capabilities of the athlete's body.
- Hepatic pain syndrome is a pathological condition, the main symptom of which is sharp pains in the right hypochondrium, arising in athletes directly during the performance of long-term intensive training and competitive loads.
Hepatic pain syndrome most often occurs in athletes while running long and marathon distances, during cross-country skiing, cycling and other sports activities associated with the implementation of long and intense physical activity.
Causes of hepatic pain syndrome:
- hemodynamic;
- cholestatic.
First aid. To stop the pain attack, it is necessary to stop the load, this can lead to the disappearance of the pain syndrome. If the pain has not disappeared, then deep, rhythmic breathing and self-massage of the liver area are recommended.
Chronic physical overexertion of the urinary system
Physical activity places very high demands on the urinary system.
Chronic physical overexertion of the urinary system is expressed by proteinuric and hematuric syndromes, they can be isolated or joint.
- Proteinuria is the presence of protein in the urine.
- Hematuria is the presence of red blood cells in the urine.
The interpretation of proteinuria and hematuria in athletes is complex. There is an opinion about working, sports, marching proteinuria - 3-9% and hematuria of the order of 10 unchanged erythrocytes, while the maximum shifts should occur at the end of the load.
At the same time, proteinuria and hematuria in athletes may be the result of chronic physical overstrain, on the one hand, and a manifestation of diseases of the urinary system, on the other. Therefore, it is necessary to examine athletes with these syndromes.
Fainting states. Definition, causes and mechanisms of occurrence. Signs of fainting, first aid, prevention
Fainting (syncope) states.
Syncope (syncope) is a sudden, short-term, reversible loss of consciousness. Fainting is caused by acute, transient ischemia of the brain.
Ischemia is a decrease in the blood supply to an organ or tissue due to a decrease in blood flow to its vascular network. This is the most important pathological process, one of the most common causes hypoxia of body cells.
Fainting is the mildest form of acute vascular insufficiency.
The mechanism of development of these syncope. In athletes, there is a sharp decrease in blood pressure due to a decrease in peripheral vascular resistance with systemic vasodilation and a compensatory increase in heart rate.
Fainting can be manifested by a sudden loss of consciousness, but more often it is preceded by a presyncope (presyncope) state. This condition is characterized by a sudden slight clouding of consciousness, darkening of the eyes, dizziness, nausea, ringing in the ears, cold hands and feet, and general weakness. There is pallor, increased sweating, decreased blood pressure. In the presence of a fainting state, the victim slowly falls to the floor. With a sudden loss of consciousness, the fall occurs quickly and can cause bruises and injuries to the victim.
Fainting is also called syncope. The duration of loss of consciousness during fainting, as a rule, is from 5 to 22 seconds. Restoration of consciousness occurs quickly, orientation is restored immediately, anxiety persists for some time, a feeling of fear (especially if fainting has developed for the first time), general weakness.
There are syncope of reflex neurogenic genesis (psychogenic, orthostatic, gravitational, vasovagal) and symptomatic syncope.
Symptomatic fainting is a symptom of various diseases. Fainting can be the first, sometimes the only manifestations of the heart.
Psychogenic fainting.
The development of psychogenic syncope is associated with reflex expansion of peripheral vessels, causing a decrease in cardiac performance and, accordingly, brain hypoxia.
Most often occurs with stress in a standing position. Provoking factors are: sudden fear, taking blood from a vein, type of blood, surgery, negative emotions, pain, being in a stuffy room, transport, in a confined space, fatigue, etc.
First aid for psychogenic fainting.
After the return of consciousness, the victim should be gradually transferred to a vertical position. With a rapid transition, syncope can be repeated, and the duration of the repeated syncope is much longer than the previous one. In case of repeated loss of consciousness, medical assistance is necessary.
Vasovagal syncope.
Provoking factors are a sharp turn of the head, pressure on the area of the carotid sinus, a tight collar, and a strong compression of the chest.
The development of vasovagal syncope is associated with:
- with a sudden reflex expansion of peripheral vessels, leading to a sharp decrease cardiac output and the development of cerebral hypoxia;
- with sudden reflex suppression of cardiac activity by the vagus nerve up to complete cardiac arrest.
In the first case, there is a clinical picture of a simple syncope. First aid in this case the same as in psychogenic syncope.
In the second case, there is a clinical picture of a sudden cessation of blood circulation. First aid in this case is the same as in case of a sudden cessation of blood circulation.
Orthostatic fainting.
There are functional and organic orthostatic syncope.
Functional orthostatic syncope occurs during prolonged immobility in vertical position or when moving quickly from a horizontal to a vertical position.
The main cause of organic orthostatic syncope is arterial hypotension.
The development of orthostatic syncope is due to the deposition of blood in the vessels of the lower extremities, which is accompanied by a sharp decrease in cardiac output and, accordingly, brain hypoxia.
Factors provoking the occurrence of orthostatic syncope are high ambient temperature, overwork, taking some (especially diuretics), visiting a sauna.
It develops suddenly, there is general weakness, loss of balance, nausea, ringing in the ears, darkening of the eyes, cold sweat, pallor of the skin, bradycardia, decreased blood pressure, rapid shallow breathing. The fainting lasts for a few seconds. First aid for orthostatic syncope
The victim should be left in a horizontal position face up or should be laid on his back in a horizontal position, unfasten tight clothes and a collar, raise his legs, and provide fresh air. It is necessary to cause irritation of the receptors of the skin and mucous membranes, for this, spray with cold water, let ammonia be inhaled, moistening a cotton swab with it and bringing it to the nose. As a rule, these simple measures are enough, in a horizontal position, fainting quickly stops, consciousness returns, cheeks turn pink, eyes open.
Gravitational fainting.
Gravity syncope can occur in athletes after middle and long-distance running, skating, cycling, skiing, if the athlete, after passing the distance immediately after the finish, stops and remains motionless.
The development of gravitational syncope is due to the fact that during running there is a significant redistribution of blood in the body of an athlete, a significant expansion of the vessels of the lower extremities and their abundant supply arterial blood. When an athlete suddenly stops, one of the main factors in the movement of blood through the veins to the heart is turned off - the so-called "muscle pump" and there is a sharp decrease in venous return of blood to the heart, as a result of which cardiac output decreases sharply and brain hypoxia develops.
First aid in case of gravitational syncope The athlete must be laid in a horizontal position with legs raised, tightly bandaged with an elastic bandage or squeezing strokes on the legs from the periphery to the center. After these events, the athlete, as a rule, quickly regains consciousness.
Prevention Consists of a gradual, rather than abrupt cessation of muscle work after the finish, for this the athlete needs to gradually move from a fast run to a slower run, and then move on to a walk, while deepening breathing.
The concept of hypoglycemia. Definition, causes and mechanisms of development of a hypoglycemic state during sports, signs of a hypoglycemic state, first aid, prevention
Hypoglycemia is a pathological condition caused by a decrease in blood glucose.
During physical exertion, athletes most often encounter disorders of carbohydrate metabolism. Intense physical activity can cause hypoglycemia in athletes.
Hypoglycemia can develop in athletes during ultra-long distance running competitions, many hours of road cycling, ultra-long distance skiing, many hours of swimming, etc.
The initial manifestations of a hypoglycemic state are an acute feeling of hunger, a feeling of fatigue, anxiety, mental irritation, speech impairment, and ridiculous actions are possible (for example, changing the movement from finish to start).
If carbohydrates are not taken at this moment, then hypoglycemic syncope develops.
Clinical manifestations of hypoglycemic syncope: dizziness, cold sweat, trembling, there may be loss of consciousness.
First aid for hypoglycemic condition If the hypoglycemic condition is not accompanied by loss of consciousness, then the victim should be given sweet tea to drink, eat a few lumps of sugar or a few teaspoons of granulated sugar.
In the absence of the necessary medical care, a hypoglycemic coma develops, requiring urgent hospitalization of the victim.
Hypoglycemic coma is the next stage of hypoglycemia. Coma is the most significant degree of pathological inhibition of the central nervous system, characterized by a deep loss of consciousness, the absence of reflexes to external stimuli, and a disorder in the regulation of vital body functions. Coma is a formidable complication of various diseases, significantly worsening their prognosis.
Heat and sunstroke. Definition, causes, signs of heat and sunstroke, first aid, prevention
Hyperthermia (overheating) is a violation of the thermal balance of the body, overheating of the body, which occurs, as a rule, as a result of an increase in ambient temperature and a violation of thermoregulation.
The main mechanism of overheating in this case is a significant decrease in heat transfer, since the higher the temperature external environment, the less heat is given off by the body, since the heat release vector is directed from the body or space with a higher intrinsic temperature to the body or space with a lower temperature.
Overheating occurs faster if, under conditions of elevated ambient temperature, it is necessary to perform increased muscular work (an increase in energy production against the background of a decrease in heat transfer), as well as under certain meteorological conditions. Thus, overheating develops more intensively at high ambient temperatures, with increased humidity and no air movement (wind), as this leads to a sharp drop in heat transfer due to a decrease in the intensity of sweat release and evaporation. Contributes to overheating and tight clothing, especially during physical work in conditions of high external temperature.
Heat stroke is a pathological condition that develops as a result of decompensation of thermoregulation under the influence of exogenous and endogenous heat, which is not released by the body to the external environment in a timely manner due to insufficient sweating.
Thermoregulation is a physiological function of maintaining a constant body temperature by regulating heat transfer and heat production of the body.
Violation of heat transfer mechanisms and excessive accumulation of heat in the body leads to serious disorders throughout the body, primarily in the central nervous system.
Sunstroke is heat stroke caused by intense or prolonged exposure to direct sunlight.
Mechanisms of development and clinical manifestations of solar and heat stroke are similar. They differ only in etiology: during sunstroke, the leading factor causing the accumulation of heat in the body above the physiological limit is the infrared radiation of the sun and the underlying soil of the mountainous desert area, and to a lesser extent, the convection heat of the surrounding air.
Provoking factors in healthy individuals are heavy physical exertion, neuropsychic stress and overweight.
Heatstroke (sunstroke) often develops suddenly, however, some patients may experience a delayed form of heatstroke, in which between the appearance of the first sign of damage (cessation of sweating) and the onset of distinct clinical manifestations (permanent hyperthermia, collapse, etc.) passes from 3 to 24 hours. With this form of heat stroke, the prodromal period is manifested by general weakness, severe headache, nausea, dizziness, ringing in the ears, and sometimes photophobia. Then comes motor restlessness and speech disorders. Possible changes in consciousness, psychomotor agitation, frequent urination, polyuria. When a heat stroke occurs, a coma develops, there may be delirium, hallucinations.
There are 3 degrees of heat (solar) stroke:
- 1st degree - easy.
There is a general malaise, headache, dizziness, tinnitus, blurred vision, drowsiness, the temperature is increased to 38 degrees, there is flushing of the face, head, moderate sweating, rapid breathing, tachycardia, blood pressure changes slightly.
- 2nd degree - medium.
Severe stupor, weakness, vomiting, severe headache, dizziness, temperature rises to 40 degrees, significant sweating, fainting spells, shallow, rapid breathing, severe tachycardia, and a decrease in blood pressure are observed.
- 3 I degree - heavy.
There is a coma, psychomotor agitation, delirium, hallucinations, the face and conjunctiva of the eyes are hyperemic, the pupils are dilated, the skin is dry, "burning", the temperature rises to 42 degrees, convulsions, progressive tachycardia, breathing is superficial, rapid, not rhythmic, pulse thready, a sharp drop in blood pressure.
First aid for heat stroke and sunstroke
In mild cases, quickly but carefully transfer the victim to the shade, to a cool place, lay him on his back with his head slightly raised, undress him, provide him with peace and sufficient access to fresh air, put a cold compress on his head.
In severe cases, first of all, it is necessary to transfer the victim to a shaded, cool place, to cool him, for this you can use pieces of ice or the cooling effect of a water or air jet. The head and neck should be cooled locally with ice packs, and ice packs should also be placed in the inguinal region in the projection of the femoral vessels and in the axillary region. Next, you need to urgently hospitalize the victim.
Thermal collapse is clinical syndrome due to overheating.
Collapse is an acutely developing vascular insufficiency, characterized primarily by a drop in vascular tone, as well as an acute decrease in circulating blood volume. In this case, there is a decrease in the flow of venous blood to the heart, a decrease in cardiac output, and a drop in blood pressure. Hypoxia of the brain occurs, vital functions of the body are inhibited.
Thermal collapse occurs due to an inadequate response of the cardiovascular system to hyperthermia.
Usually, the occurrence of collapse is preceded by headache, dizziness, feeling of heat, nausea, weakness, lethargy, darkening of the eyes, palpitations.
Thermal collapse develops suddenly, but it is usually short. The skin is pale, moist, severe weakness, tachycardia, blood pressure is reduced.
In contrast to heat stroke, during thermal collapse, the body temperature is increased, but not higher than 38.5 0 C; a characteristic sign of thermal collapse is profuse sweating. First aid for thermal collapse
It is necessary to quickly but carefully transfer the victim to the shade, to a cool place, remove tight, warm clothes, lay on his back with raised lower limbs, provide him with peace and sufficient access to fresh air, put a cold compress or ice pack on his head, give a cold drink .
Hypothermia (general cooling) and frostbite. Definition, signs, causes, first aid, prevention
Despite the extensive domestic and foreign literature on the problem of low temperatures, there is currently no unity in the classification of these lesions. Generally recognized is only the allocation of general and local pathological manifestations when exposed to cold.
Cryotrauma ( cold injury) are lesions resulting from the action on the human body of low ambient temperature.
TO acute lesions cold include:
- Hypothermia (freezing, pathological hypothermia, general cooling) are common pathological manifestations due to cold injury (their names are different, and there is no single generally accepted term).
- Frostbite - local pathological manifestations due to cold damage.
Etiological factors contributing to frostbite:
A. Meteorological conditions.
Main etiological factor, contributing to the occurrence of hypothermia, is the low temperature of the external environment. The lower the temperature and the longer its exposure, the greater the likelihood of frostbite and general hypothermia. The damaging effect of low temperature is promoted by:
- increased air humidity;
- wind and blizzard;
- sudden and rapid change in temperature;
- the duration of the cold.
B. Factors that mechanically impede blood circulation:
- tight, tight clothes and shoes.
B. Factors that reduce local tissue resistance:
- previous frostbite;
- immobility and excessive flexion of the limbs;
- paralysis;
- vascular diseases of the extremities.
D. Factors that reduce the overall resistance of tissues:
- blood loss;
- traumatic shock;
- exhaustion;
- languor;
- hunger;
- alcohol
- smoking.
Common to all types of cold lesions are a decrease in tissue temperature, circulatory disorders due to vasospasm, blood stasis, blood clots, leading to tissue hypoxia, and then to necrosis.
In the pathogenesis of frostbite, the violation of peripheral circulation and, above all, the microcirculation system is of great importance. Early restoration of blood circulation in the affected area is the basis of effective treatment.
1. Frostbite.
Frostbite is a local injury resulting from exposure to cold, in which the temperature decreases only in any part of the body.
Frostbite is tissue damage caused by their cooling. In the affected area of the body, a spasm of blood vessels occurs and the blood supply deteriorates sharply, and sometimes the blood supply stops completely, which leads to tissue damage, up to their necrosis.
During frostbite during pathological process distinguish the following periods:
- a) the pre-reactive (hidden) period of frostbite is the period from the onset of low temperatures to the start of restoration of tissue temperature. This period is characterized by a decrease in tissue temperature, which leads to a violation
- blood circulation and tissue metabolism in the area exposed to cold. Paleness and lack of sensitivity ("stiffness") are noted. In to jet period it is impossible to determine the degree of frostbite;
- b) the reactive period of frostbite is the period after warming, restoration of tissue temperature. In the reactive period, depending on the depth and severity of the lesion, signs of inflammation appear: pain, swelling, congestive hyperemia or necrosis. It is in this period that the degree of frostbite is determined.
According to the severity of frostbite lesions (local cold lesions) are divided into 4 degrees:
- I degree - the mildest degree - the skin is initially pale, then it becomes cyanotic, marbled, swelling and pain appear (impaired blood circulation in the skin without irreversible damage), after 5-7 days these phenomena disappear without consequences;
- I degree - the skin is pale, cyanotic and edematous, during the first days blisters are formed, filled with transparent exudate; healing without scarring occurs in 2-3 weeks;
- I degree - the skin is sharply pale and edematous, there is no sensitivity, blisters form with hemorrhagic exudate, skin necrosis. After a few days, the skin darkens, turning into a dry or moist scab, which is then sloughed off, forming granulating wounds, later scarring;
- I degree - necrosis of soft tissues, sometimes there is necrosis of the bones of the limb.
First aid for frostbite
First of all, it is necessary to stop further exposure to cold and warm the victim. It is necessary to give the victim hot, sweet tea or coffee to drink.
The limbs (hands and feet), nose, cheeks, auricles are most often exposed to frostbite.
In case of frostbite of the auricles, cheeks, nose, to restore blood circulation in these areas, it is necessary to rub them with a clean hand or a soft cloth until reddened, then treat with alcohol and apply an aseptic bandage. It is impossible to rub frostbitten areas with snow, since this not only does not contribute to warming, but even more cools the affected tissues, the temperature of which is always higher than the temperature of snow. In addition, when rubbing with snow, the surface layer of the skin can be damaged and these microtraumas can become a gateway for infection.
With frostbite of the limbs, it is necessary to warm the affected area as soon as possible. For this purpose, rub the affected area with a clean woolen glove, a soft cloth until signs of active hyperemia appear, then treat with alcohol, apply heat-insulating dressings, give the limb an elevated position and urgently hospitalize the victim in a hospital.
The technique of applying heat-insulating bandages
Sterile dry wipes are applied to the frostbite area, a thick layer of cotton wool is placed on top of them, it is desirable to apply metal foil to the cotton wool. The whole bandage is fixed with a bandage. Woolen or fur things, blankets, etc. can be used as a heat-insulating bandage. A heat-insulating bandage is applied as early as possible and is not removed until a feeling of warmth and tingling appears in the affected areas.
2. Hypothermia (general cooling).
Hypothermia is a condition that occurs as a result of the exhaustion of the adaptive mechanisms of thermoregulation, when the temperature of the entire human body progressively falls under the influence of external cooling and all vital functions are inhibited up to their complete extinction.
Hypothermia is a condition that occurs with a sharp decrease in body temperature as a result of exposure to the external environment.
With hypothermia, there is a violation of the adaptive mechanisms of thermoregulation of the body, maintaining the constancy of body temperature, the decrease of which begins to progress. This leads to inhibition of metabolic processes, which is manifested by disturbances in the activity of the central nervous system, cardiovascular and respiratory systems, and other vital functions.
Hypothermia can occur not only at ambient temperatures below 0 0 C, but also at temperatures above 0 0 C.
In the development of general hypothermia, two periods of the pathological process are also distinguished:
- pre-reactive (latent) period - this is the period from the onset of low temperatures to the start of tissue temperature recovery;
- the reactive period is the period after warming, after the restoration of tissue temperature.
There are 3 stages in the development of hypothermia:
- Stage 1 - light (adynamic form) - this is an adaptive reaction of the whole organism. There is an increase in all body functions (nervous, cardiovascular, respiratory systems, metabolism). The body responds to cooling with increased heat production. However, at the end of this stage, vital activity indicators begin to fall.
Body temperature - 35-33 0 C. Characterized by blanching or moderate cyanosis of the skin, marbling of the skin, the appearance of "goosebumps", chills. The movements are slow, sluggish, the limbs are as if "fettered". The victim feels severe weakness, speech is difficult (stretches words, pronouncing them in syllables), consciousness is clearly depressed. Bradycardia may be noted, blood pressure is normal, breathing is not disturbed.
- Stage 2 - of moderate severity (stuporous form) - is a reaction of protective inhibition. The basic vital forces are oppressed.
Body temperature - 32-29 0 C. Pale, cyanotic, marble, cold to the touch skin integuments are characteristic. There is a sharp drowsiness, depression of consciousness, a meaningless look, lack of facial expressions. Movement is sharply hampered - beginning rigor. Bradycardia - up to 52-32 beats per minute, blood pressure is normal or slightly reduced, breathing becomes more rare and superficial (8-12 per minute).
- Stage 3 - severe (convulsive form) - is the extinction of vital functions.
Body temperature is below 29 0 C, consciousness is absent. Convulsions are observed, especially prolonged convulsive contraction chewing muscles, the tongue may be bitten. Upper limbs flexed elbow joints, it is difficult to straighten them, sometimes it is impossible due to stiffness. The lower limbs are bent, the abdominal muscles are tense. The skin is pale, cyanotic, cold. Bradycardia - 34-32 beats per minute, blood pressure is sharply reduced or not detected at all. Breathing is very rare, 3-4 per minute, superficial, intermittent, wheezing. The pupils are constricted, weakly react to light. At a body temperature below 25-22 0 C, recovery is unlikely. First aid for hypothermia
Hypothermia is a very serious injury, but with timely and properly provided medical care, recovery of the victims, including those with severe hypothermia, can be achieved.
With mild hypothermia, warming the victim alone is enough to eliminate all disorders caused by exposure to cold.
Local warming, and especially general warming, takes a long time, and it is necessary to shorten the period of hypothermia as much as possible, since the severity of the lesions depends not only on the degree of decrease in the body temperature of the victim, but also on the duration of hypothermia. Therefore, the victim is urgently hospitalized in a hospital, wrapping him up for warming and warming the victim on the road to recover. normal temperature body. If the victim can swallow, then it is necessary to drink hot sweet tea or coffee. best method Restoration of tissue temperature is warming from the inside, for which, when providing first aid, heat-insulating bandages are applied to the limbs.
Intensive and prolonged warming of the victim is carried out already in the hospital.
Prevention
Prevention of hypothermia and frostbite is:
- on the one hand, in protection (the use of rational warm, light, waterproof, well-chosen clothes and shoes);
- on the other hand, in increasing the resistance of the body to the effects of cold.
Diseases of the nervous system in athletes
Most often, athletes have neurocirculatory dystonia (NCD) and neuroses.
1. Neurocirculatory dystonia.
Neurocirculatory dystonia is a condition caused by a violation of the central and autonomic regulation of the activity of organs and systems. The main reason is stress or emotional overstrain, which provoke an increase in the activity of the sympathetic or parasympathetic division of the autonomic system, which is manifested by functional changes in the cardiovascular system, respiratory and other systems.
There are the following forms of neurocirculatory dystonia:
- a) NDC by hypertonic type;
- b) NCD by hypotonic type;
- c) NCD by cardiac type;
- d) NDC for mixed type.
NDC for hypertensive type is "border arterial hypertension". It is characterized by small and transient rises in blood pressure and a variety of neurovegetative symptoms ( emotional lability, sleep disturbances, fatigue, increased heart rate, sweating, etc.).
NDC by hypotonic type is "neurocirculatory asthenia". It is characterized by a decrease in blood pressure below 100/60 and a variety of symptoms (weakness, headache, dizziness, fatigue, drowsiness, lethargy, a tendency to faint, motion sickness, etc.).
NDC by cardiac type is a disease based on a disorder of the functions of the central nervous system. Athletes complain of discomfort and pain in the region of the heart, pain is often associated with excitement, feelings a few days before important competitions.
NDC for mixed type.
2. Neuroses.
Neuroses are diseases of the central nervous system caused by the influence of psychotraumatic factors, the hallmark of which is autonomic disorders. Characterized by a temporary decrease in mental and physical performance.
In sports practice, the following forms of neurosis are most common:
- a) neurasthenia
- b) obsessive-compulsive disorder,
- c) cardioneurosis.
Neurasthenia is a psychogenic disease from the group of neuroses, the main manifestation of which is a state of irritable weakness - an increase in exhaustion and a slowdown in recovery mental processes.
Obsessive-compulsive disorder: the main thing in the clinical picture is the various manifestations of obsession. Among obsessive states, athletes have obsessive thoughts about losing in competitions, fear of illness (phobia), fear of staying indoors (claustrophobia). Phobias are essentially pathological passive-defensive reactions.
Cardioneurosis is a disease, which is based on a disorder of the functions of the central nervous system. Athletes complain of discomfort and pain in the region of the heart, pain is often associated with excitement, feelings a few days before important competitions.
Diseases of the cardiovascular system in athletes
1. Hypertension (AH) - essential hypertension.
This is a primary increase in blood pressure as a result of a persistent violation of higher nervous regulation. Hypertension is a disease, the leading symptom of which is an increase in blood pressure due to neuro-functional dysregulation vascular tone.
HD should be distinguished from symptomatic hypertension, in which an increase in blood pressure is one of the symptoms of the disease.
The main importance in the occurrence of GB is given to overstrain of the central nervous system caused by prolonged or strong unrest, mental and neuropsychic overload.
You need to know that hypertension can develop after a concussion.
Distinguish between benign and malignant hypertension.
Classification of hypertension according to A.L. Myasnikov, he distinguishes 3 stages of the disease, each of which is divided into phases (A and B).
GB along with coronary artery disease are the main causes of death.
2. Ischemic heart disease (CHD).
Ischemic heart disease (CHD) is a group of diseases that include:
- a) angina pectoris
- b) myocardial infarction,
- c) coronary cardiosclerosis.
The main causative factor of these diseases is atherosclerosis of the coronary arteries.
At the heart of the pathological process is a violation of the correspondence between the need of the myocardium for blood supply and its actual implementation. This discrepancy can occur with a decrease in blood supply or with a sharply increased need for blood supply to the myocardium.
A. Angina pectoris (angina pectoris) is a common disease, the main clinical symptom of which is attacks of pain behind the sternum, caused by an acute onset, but transient violation of the coronary circulation.
Pain in angina pectoris - intense, compressive, localized behind the sternum, radiating to left hand, left shoulder, accompanied by a sense of fear of death. This pain is relieved by taking nitroglycerin.
At the heart of an attack of angina pectoris is myocardial ischemia, which develops in conditions when the blood flowing through the coronary arteries to the working myocardium becomes insufficient.
Distinguish:
- exertional angina and
- rest angina.
The most common causes of angina pectoris is coronary sclerosis (atherosclerosis of the coronary arteries of the heart); maybe - coronary spasm (temporary narrowing of the lumen of the coronary arteries of the heart as a result of spasm).
B. Myocardial infarction is a disease characterized by the formation of a necrotic focus in the heart muscle as a result of a violation of the coronary circulation.
Atherosclerosis of the coronary arteries is the main cause of myocardial infarction.
Atherosclerosis is a chronic disease characterized by systemic lesion arteries due to metabolic changes in the tissues of the vascular wall.
Conditions that contribute to the occurrence of a heart attack are overwork, stress, smoking.
The pathogenesis is complex. It is based on coronary thrombosis (atherosclerosis of the coronary arteries and disorders of the anticoagulant blood system).
V.P. Obraztsov and N.D. Strazhesko identified 3 options for the course of myocardial infarction:
- anginal (most common and manifested pain syndrome, the pain is prolonged and is not relieved by nitroglycerin);
- asthmatic (begins with an attack of cardiac asthma and pulmonary edema);
- abdominal (pain occurs in the abdomen).
For diagnosis, electrocardiography is of particular importance (with the help of an ECG, the presence of myocardial infarction, its localization, depth and extent of the lesion is established).
Myocardial infarction, ending with the formation of scars, leads to the development of focal, post-infarction cardiosclerosis.
B. Cardiosclerosis is a disease of the heart muscle caused by the development of scar tissue in it.
Distinguish cardiosclerosis:
- atherosclerotic (a consequence of atherosclerosis of the coronary arteries) and
- myocarditis (outcome of myocarditis of any etiology). Atherosclerotic cardiosclerosis is prone to progression of the process.
3. Myocarditis.
Myocarditis is focal or diffuse inflammation of the myocardium. According to the prevalence of lesions, myocarditis is divided into:
- focal,
- diffuse.
The etiological factors causing the development of myocarditis are viral and bacterial infections.
Myocarditis most often occurs 2-3 weeks after acute respiratory infections, follicular tonsillitis. There is a sharp weakness, tachycardia, pain in the region of the heart, shortness of breath during physical exertion, blood pressure decreases, fainting occurs, persists subfebrile temperature. It is urgent to conduct an ECG and echocardiographic study. You need to know that unrecognized, sluggish myocarditis can cause death.
Inflammatory changes in the myocardium in various infections are the result of an allergic reaction of the organism sensitized by the microbe. The microbial antigen or its toxin, acting on the heart muscle, causes the formation of autoantigens in it. In response to this, the body produces autoantibodies, which cause extensive changes in the myocardium.
According to the course, myocarditis is divided into:
- sharp,
- subacute.
Myocarditis in most cases proceeds favorably and ends in recovery. In some cases, sclerosis of the heart muscle may develop - myocardial cardiosclerosis.
4. Subacute septic endocarditis.
Endocarditis is an inflammatory lesion of the endocardium with damage to the heart valves.
Subacute septic endocarditis is a disease in which, against the background of a septic condition, an inflammatory lesion of the endocardium occurs with ulceration of the heart valves. This disease is manifested by weakness, shortness of breath, fatigue, subfebrile condition, excessive sweating.
5. Rheumatism.
Rheumatism is a common infectious-allergic disease in which an inflammatory lesion of the connective tissue occurs, mainly of the cardiovascular system, with frequent involvement of the joints in the process (however, the damage to the joints proceeds benignly and is not accompanied by their subsequent deformation). Rheumatism is a systemic disease.
Rheumatism is caused by group A beta-hemolytic streptococcus.
The disease develops 1-2 weeks after a streptococcal infection (tonsillitis, scarlet fever). Subfebrile condition, weakness, sweating appear. After 1-3 weeks, new ones join, indicating damage to the heart - palpitations, a feeling of interruptions in the work of the heart, a feeling of heaviness or pain in the heart, shortness of breath, then pain in the joints (ankle, knee, shoulder, elbow). Joint pain is characterized by volatility and symmetry of the lesion.
With rheumatism, the heart muscle is affected - rheumatic myocarditis. Rheumatic myocarditis is combined with rheumatic endocarditis - rheumatic heart disease. The mitral valve is most commonly affected. A heart defect develops. With timely treatment, rheumatic heart disease can end without the formation of heart disease.
In severe rheumatism, myocardial and endocardial damage can be combined with rheumatic pericarditis, i.e. all membranes of the heart (pan-carditis) are involved in the rheumatic process.
6. Heart defects.
Heart disease is an anatomical defect of the heart that impairs its function.
Heart disease is a persistent pathological change in the structure of the heart that disrupts its function.
Heart defects are:
1. Congenital.
Congenital heart defects are:
- non-closure of the interatrial or interventricular septum;
- cleft arterial duct;
- stenosis of the pulmonary artery.
Congenital malformations are caused by a violation of the development of the heart in the embryo at 1-5 weeks of gestation. Causes:
- sharp infectious diseases;
- intoxication;
- severe mental trauma;
- taking certain medicines;
- irradiation.
2. Acquired.
Acquired heart defects are much more common.
Acquired heart defects are lesions of the valvular apparatus (valvular insufficiency associated with damage to their cusps, or valvular ring stenosis with secondary deformation of the heart chambers).
The main cause of acquired heart defects is rheumatism, less often - septic endocarditis, atherosclerosis, heart injury.