Some diseases are accompanied by a decrease in oxygen levels in the blood. In such cases, oxygen therapy comes to the rescue. The procedure is carried out different ways:
- inhalation, during natural breathing or during artificial ventilation;
- non-inhalation, absorption of an oxygen cocktail subcutaneously or through the intestines.
Oxygen therapy is a procedure for treating with oxygen
For the normal existence of living organisms, it is necessary that there be 21% oxygen in the atmosphere. A decrease in concentration will lead to big problems, even death. But pure oxygen is also dangerous. For oxygen therapy, mixtures with a high oxygen content (20-80%) are used.
The term "oxygen therapy" comes from the Latin words "oxygenium" (oxygen) and "therapy" (treatment). The goal is to deliver more oxygen to the body. Indications for oxygen therapy:

Indications for the use of oxygen therapy also include helping in the action of certain medications and enhancing the effect of treatment for cancer.
The first experiments with oxygen therapy were carried out in the eighteenth century to revive newborns born without breathing. The method was the most primitive - a face mask connected to an oxygen bag. Oxygen therapy was even used to combat helminths (worms) by introducing oxygen into the intestines through a tube.
The gas composition for oxygen therapy usually contains 50-60% (up to 80%) oxygen, but in some cases other ratios are used. Indication for the use of carbogen (95% oxygen and 5% carbon dioxide) – poisoning carbon monoxide. In case of pulmonary edema with the release of foamy liquid, the gas mixture is passed through an antifoam agent (50% ethyl solution alcohol).
The safest composition for oxygen therapy contains 40-60% oxygen. Pure oxygen can cause burns respiratory tract. It can also be toxic to humans, resulting in dry mouth, chest pain, seizures, and loss of consciousness.
Before administering oxygen to the patient, it must be humidified. There are three types of humidification:
- Passing through water. The method is not very effective. Large gas bubbles do not have time to absorb enough water and its temperature drops slightly. Heating the humidifier and using a fine-mesh sprinkler will help correct the shortcomings.
- "Artificial nose" Air is passed through corrugated foil on the patient's face. The foil heats up from breathing and condenses exhaled moisture, giving it away when you inhale.
- An aerosol inhaler is the most reliable way. It creates a suspension of tiny droplets of water in a gas composition.
Inhalation methods of oxygen supply
Oxygen therapy can be carried out both in clinical and at home settings. At home, you can use concentrators, pillows or balloons. These methods are indicated for long-term oxygen therapy, but only a specialist can prescribe treatment and choose a method. Improper use of oxygen mixtures can be dangerous!
IN clinical settings There are the following types of submission:
- Using nasal catheters. To prevent the mucous membrane from drying out, the mixture is moistened by passing it through water. The patient is given the composition through a nasal catheter (cannula) under a pressure of 2-3 atmospheres. The equipment includes two pressure gauges indicating the pressure in the cylinder and at the outlet.
- Through a special mask that should fit tightly to the face. The supplied mixture is also moistened.
- Mechanical ventilation device. With this method, gas is supplied through an endotracheal tube.

There is an inhalation type of oxygen therapy
Algorithm for performing oxygen therapy through a nasal catheter (cannula):
- check the patency of the airways and, if necessary, clear them;
- open the package with the catheter and measure the distance from the tip of the nose to the patient’s earlobe;
- lubricate the inserted end of the catheter with Vaseline;
- lift the tip of the nose and insert the cannula along the lower nasal passage to the back wall of the pharynx (at a distance from the nose to the earlobe);
- ask the patient to open his mouth to check the catheter - the inserted end of the tube should be visible in the pharynx;
- connect the outer end of the catheter to a source of humidified gas and secure it with a bandage on the cheek, forehead or neck;
- open the supply valve, supply rate is 2-3 liters per minute;
- monitor the patient’s condition for 5 minutes;
- change the position of the cannula every half hour or hour to prevent bedsores and drying out of the mucous membrane.
If an oxygen cushion is used for inhalation, then before use you need to make sure that it is filled with gas from a cylinder (the external pressure gauge should show 2-3 atm.) and a clamp is applied to the outlet tube. The nurse should disinfect the funnel attached to the pillow. Algorithm for using an oxygen cushion:

Hyperbaric oxygenation (from the Greek “heavy”) combines both delivery methods. This is a method of saturating the body with oxygen under high pressure. The method is used for therapeutic and prophylactic purposes. Sessions are conducted in a special pressure chamber with increased pressure and gas concentration. Among the indications - thermal burns, frostbite, decompression, skin grafting, high blood loss, gangrene.
Non-inhalation methods of oxygen therapy
Bypass oxygen supply respiratory system called non-inhalation oxygenation method. These methods include:
- Enteral (via gastric tract). Once in the stomach, oxygen passes into the intestines and is absorbed into the bloodstream. This technology has previously been used to revive newborns or for respiratory failure in adults. Nowadays, the method of oxygenation using oxygen cocktails– patients receive gas mixtures whipped into foam or mousse. This therapy is used for toxicosis, chronic respiratory failure, obesity, and acute liver failure.
- Intravascular. Blood or blood substitute transfused to a patient is pre-saturated with oxygen.
- Cutaneous. This method is most often used when cardiovascular diseases, complications from injuries, wounds or ulcers. It consists of taking general or local oxygen baths.

Non-inhalation oxygen therapy is also used
In addition to those listed, non-inhalation types include subcutaneous, intra-articular, and intracavitary methods of oxygen therapy. Indications for their use are wounds, inflammatory processes, ulcers.
Features of oxygen therapy in children
Hypoxia in children develops very quickly. This is due to the fact that the mechanism for compensating for the lack of oxygen begins to develop only at 5-6 months of life and is fully formed by 7-8 years. Any problems with the respiratory or circulatory system, anemia, or metabolic disorders can lead to hypoxia. Only a pediatrician has the right to prescribe therapy, self-treatment unacceptable!
For children, inhalation oxygen therapy is most often used. Oxygen tents or awnings and mouth masks are widely used. In some cases, it is inserted into the airways with a nasal catheter. Mouthpieces, funnels or nipples are not very convenient and are hardly used.
The optimal concentration for children is 40-60%. The mixture must be moistened to avoid drying out the mucous membrane. The duration of sessions is prescribed by the doctor based on the age and weight of the baby. For children born with asphyxia, oxygenation in a pressure chamber is increasingly used.

Oxygen treatment is indicated for children
Non-inhalation oxygenation techniques are practically not used for children. Sometimes oxygen is introduced into the intestines for enterobiasis, chronic colitis, urinary incontinence, and ascariasis.
The procedure causes anxiety in children, which can lead to disturbances in cardiac activity or breathing. To avoid complications, consultation with a specialist and compliance with the rules and technology of oxygenation are necessary.
Safety precautions
In high concentrations, oxygen is toxic. Up to 60% concentration it is harmless even with prolonged use. If pure oxygen is used for more than 24 hours, complications are possible: changes in the lungs, necrosis nerve cells, premature babies have blindness.
In the event of a leak, oxygen accumulates in the lower part of the room (it is heavier than air). Ethanol, any oil or organic fat forms an explosive cocktail with oxygen. One spark will be enough to cause a cylinder to explode or cause a fire if there is an oxygen leak.
Specially trained people must work with oxygen cylinders (change, connect) in compliance with safety regulations. Despite the apparent simplicity of the replacement algorithm, there is a great danger to life and health.
Posted June 7, 2015 4:25am MSK by admin Category. Other respiratory diseases
Lung tissue is very vulnerable. The final structure that ensures the transfer of oxygen and the release of carbon dioxide are tiny bubbles (acini). The lung lobule looks like a bunch of grapes. Imagine that each berry is entangled in a small network of vessels (arteries and veins). They do work when you inhale and exhale.
The accumulation of fluid in the lungs (edema) is possible only when the walls of the alveoli lose their protection, increase capillary permeability, and increase pressure from the right side of the heart in the bloodstream. In this case, the lung tissue is filled not with air, but with liquid.
The physiology of damage when the lungs fill with fluid can be divided into 3 possible causes:
- Overload of the pulmonary vessels with blood due to insufficient strength of heart contractions leads to high blood pressure inside. This causes the plasma to pass into the surrounding space, and then into the alveoli, where fluid accumulates.
- With a significant decrease in the level of protein in the blood, the body “levels” it, transferring the liquid part from the vessels to the extracellular part of the tissue.
- There may be direct damage to the alveolar wall (membrane), increased permeability and fluid filling.
Most often, one of the mechanisms prevails, but then the others come into play. Fluid in the lungs leads to disruption of gas exchange. The blood is not saturated with oxygen, the tissues do not receive the main substrate for life. Oxygen starvation develops.
All reasons for the accumulation of fluid in the lung tissue are divided into:
- associated with heart disease - this group can include all diseases leading to acute and chronic heart failure (myocardial infarction, decompensation of heart defects, hypertonic disease, myocardial dystrophy, pronounced arrhythmias, pulmonary embolism), primary weakness occurs in the left parts of the heart, which leads to stagnation in the small (pulmonary) circle and increased pressure in the pulmonary vessels;
- not related to cardiac pathology - here the causes and symptoms can be very diverse.
Why does non-cardiac pulmonary edema occur?
The reasons that caused pathological disorders depend on correct activity other organs and systems.
- Toxic effect on the alveoli of bacteria and viruses in severe pneumonia.
- Liver and kidney diseases (cirrhosis, renal failure) in terminal stage promote the loss of blood protein.
- Acute exposure to vapors of toxic chemicals, inhalation and drug overdose.
- Injuries penetrating the chest with the formation of pneumothorax (air mass in the pleural cavity compressing the lung), hemothorax (the same thing, but compression with blood).
- Exudative pleurisy(tuberculosis or other etiology).
Edema can be provoked by excessive administration of fluid intravenously without taking into account excretion in the urine (to relieve intoxication in acute poisoning, infectious diseases).
The development of radiology in the treatment of malignant tumors has led to such a form of edema as radiation edema, associated with irradiation of lung tissue.
Classification of edema by time
Pathological changes form and lead to oxygen deficiency during different time. Therefore, the clinic distinguishes:
- swelling with a lightning-fast course - the onset is sudden, death occurs quickly, it is impossible to prevent;
- acute form edema - it takes two to four hours for symptoms to develop, the patient can be saved with medical treatment specialized assistance, if the disease is not associated with terminal stage cancer, hepatitis or renal failure;
- protracted form - develops gradually, lasts more than a day.
Symptoms of oxygen deficiency begin to appear with rapid breathing. A rate greater than 16 per minute is called shortness of breath.
- Harbingers of fluid accumulation in the lungs are nocturnal attacks of cardiac asthma (in non-acute forms): suffocation suddenly appears, the patient cannot lie down at all, and is agitated.
- The face is pale, the lips, fingers and toes are blue.
- Sticky cold sweat.
- Palpitations and arrhythmia.
- Pressing pain in the heart area radiating to the left.
- Paroxysmal cough changes from dry to wet. Coughing up sputum streaked with blood.
- General weakness increases, dizziness appears.
- The more fluid passes into the lung tissue, the more pronounced the shortness of breath, and moist rales can be heard at a distance.
In the terminal stage, blood pressure drops and consciousness is confused.
How to give first aid
If the listed symptoms occur in a loved one or are noticed in a random passerby, it is necessary to call “ Ambulance" The only thing not to forget to do is to eliminate the mechanical difficulty in breathing: tighten the tie, belt, unbutton the collar, provide as much air as possible to the patient. Try to make the patient sit comfortably.
At home, before the ambulance arrives, you can give Nitroglycerin under the tongue, symptoms of agitation are relieved with soothing drops, you can put mustard plasters on your calves. If there are expectorants, it is better to use liquid decoctions or simply hot water with honey.
If the patient is hypertensive, then blood pressure should be measured. If the numbers are elevated, take the tablets prescribed by your doctor or spray Isoket spray into your mouth.
For a patient with pulmonary edema, the ambulance doctors will try to increase the low blood pressure and transport him to the hospital. Here he is placed in the intensive care unit or intensive care.
To improve gas exchange it is necessary in treatment:
- Constantly allow breathing with an oxygen mixture with an antifoam agent (through alcohol solution).
- Diuretics are used to remove excess fluid fast acting.
- Narcotic analgesics are indicated to relieve suffocation, reduce high blood pressure in the pulmonary vessels.
- Treatment requires the use of medications that increase cardiac output.
At the same time, diagnostics are carried out to identify main reason swelling.
- For pneumonia, large doses of antibiotics and vascular strengtheners are needed.
- In acute myocardial infarction, thrombolysis is performed and vasodilators for the coronary arteries are administered.
Pulmonary edema as pathological condition there is no doubt about clinical manifestations. At acute development the reason remains unclear. Identification helps to select treatment faster.
- To exclude cardiac pathology, an ECG study is performed. The method allows us to identify acute heart attack myocardium and suspect its complications.
- Laboratory tests determine blood clotting and the tendency to form blood clots.
- Liver tests, residual nitrogen levels, creatinine, urine protein and blood albumin indicate severe liver and kidney damage.
- An experienced radiologist can determine signs of pneumonia behind the picture of general congestion using an x-ray.
If the patient's condition improves, other clarifying methods (ultrasound, catheterization of the cardiac cavities) are possible.
Pulmonary edema is a physiological condition of a person in which plasma from the pulmonary vessels penetrates the interstitium and alveoli, which significantly affects the quality of gas exchange between the lungs and the inhaled air, and this, in turn, leads to acute oxygen starvation all organs of the body.
Pulmonary edema is of two types, and is divided among themselves by the pathogen:
Diagnostics
For correct diagnosis causes of pulmonary edema, the doctor should definitely and very carefully interview the patient if he is conscious. If the patient is not conscious or cannot answer questions, then it is necessary to comprehensive examination, during which it will be possible to assume possible reasons the occurrence of edema.
Laboratory tests may also be used to make a diagnosis, including:
| A blood test that confirms or refutes the presence of infection in the body due to an increased number of platelets. | |
| Blood biochemistry will determine the presence of heart disease that can cause edema. | |
| A coagulogram with an increased amount of prothrombin will confirm swelling of the lungs due to pulmonary thromboembolism. | |
| Study of the gas composition of the lungs. |
The patient may also be asked to undergo additional examinations to determine in more detail the cause of edema; these examinations are selected at the discretion of the doctor.
Symptoms of pulmonary edema
Symptoms of edema appear and develop very quickly. Symptoms strongly depend on the rate of penetration of plasma from the interstitium into the alveoli.
The rate of plasma penetration is determined by four different types edema:
| Spicy- in this form, the first symptoms of alveolar edema appear within 2-4 hours after the appearance of the very first symptoms of interstitial edema. The causes may be myocardial infarction and stress. | |
| Subacute- the duration of this edema ranges from 4 to 12 hours, usually develops due to the presence of renal or liver failure, or congenital disorders in the functioning of blood vessels. | |
| Protracted is swelling that lasts about 24 hours. This form of the disease appears in the presence of chronic diseases of the liver, kidneys, and lungs. | |
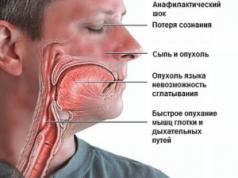
| Fulminant- such swelling is observed only after anaphylactic shock or extensive myocardial infarction, leads to rapid death. |
The main symptoms include:
| Loud breathing, even in a state of physical rest, shortness of breath is observed. | A sudden feeling of acute lack of air, which intensifies in a supine position. | ||
| Feelings of squeezing or pressing pain in the chest. | Rapid and intense heartbeat. | ||
| Sputum production with pinkish foam when coughing. | Pale or bluish skin. | ||
| Coma. |
Basic treatment methods
Pulmonary edema is acute condition organism, which can be fatal to a person, therefore, if any of its manifestations occur, you should immediately call medical care. During transportation to the hospital, the patient is placed in a semi-sitting position, oxygen inhalation is performed or, in case of severe shortness of breath, an artificial respiration apparatus is installed.
Subsequent treatment is carried out in the intensive care unit or intensive care unit, where the patient is under constant supervision.
Use of oxygen concentrators
For all types of pulmonary edema it is used oxygen therapy by using oxygen concentrators . Oxygen therapy has a positive effect on all organs and cells human body, and especially on the heart. Taking oxygen inhalation can reduce the permeability of the pulmonary membranes, which holds plasma in the vessels and does not allow them to penetrate to the alveoli.
With alveolar edema, the entire respiratory cavity is filled with pinkish foam, which prevents oxygen from entering the lungs; for this purpose, special drugs are used - defoamers, which can not only help a person receive a life-saving dose of oxygen, but also protect against asphyxia.
Take care of your health and the health of those you care about!
Thank you from the bottom of our hearts!
Pulmonary edema is a disease that is characterized by pulmonary failure, presented in the form of mass waste transudate from the capillaries into the pulmonary region, resulting in infiltration of the alveoli. Simple words, pulmonary edema is a process in which fluid seeping through blood vessels, stagnates in the lungs. The disease can be independent, or it can be a consequence of other serious ailments of the body.
The lungs are an organ that consists of alveoli filled with a large number of capillaries. The process of gas exchange occurs in this organ, as a result of which the body is filled with oxygen, which provides good performance body. If in the alveolus liquid penetrates, not oxygen– this contributes to the formation of pulmonary edema.
Important . Pulmonary edema is dangerous illness, which may have such dangerous consequences ka death. The disease affects both adults and children.
Prognosis and complications of the disease
Often the prognosis for pulmonary edema is unfavorable. This is due to the reasons that caused the disease. Non-cardiogenic edema is easy to treat, while cardiogenic edema is very difficult to treat. Even in case effective therapy Cardiogenic edema survival rate is only 50%. If the form is lightning, then the person cannot be saved. Toxic edema is a serious diagnosis and favorable outcome is possible only with the use of a large number of diuretics. It all depends on the individual characteristics of the body.
The consequences of pulmonary edema can be very diverse. Often there is a defeat internal organs. The most pronounced changes occur in tissues that are more supplied with oxygen - lungs, heart, brain, liver, kidneys, adrenal glands. Disturbances in the functioning of these organs can cause heart failure.  and even result in death. In addition, the following respiratory diseases occur:
and even result in death. In addition, the following respiratory diseases occur:
- Congestive pneumonia
- Pulmonary atelectasis
- Emphysema
- Pneumosclerosis.
Causes of pulmonary edema
The causes of pulmonary edema are very different, but they need to be known, since the consequences of the disease are very serious, even fatal. Most often, pulmonary edema manifests itself as a complication of some disease. The main causes of pulmonary edema include:
- Acute intoxication of the body. It manifests itself as a result of toxic elements entering the body, both non-infectious and infectious. Toxic elements have adverse effects on alveolar membranes. Intoxication of the body includes: excess medications, bacterial pneumonia, poisoning drugs or poison.
- General malaise of the left ventricle. As a result of this disease, pathological abnormalities cordially - vascular system(heart disease, myocardial infarction, angina pectoris, arterial hypertension). Pulmonary edema may occur as a result of these diseases.
- Chronic pulmonary disease. Among these are bronchial asthma, emphysema, pneumonia, malignant tumors lung cavities.
- Significant physical activity. For example, an athlete who climbs a mountain may experience pulmonary edema. It often occurs in female athletes rather than in males.
- TELA. Pulmonary edema may occur due to blockage pulmonary arteries blood clots This can be fatal.
- When oncotic pressure decreases. When pressure decreases, the amount of protein in the blood decreases, resulting in diseases such as liver cirrhosis and chronic hemorrhagic syndrome.
- Long-term use of medications, especially intravenous drugs, if renal excretory function is impaired.
- Severe head injuries
- With long-term artificial ventilation
- When vomit enters the respiratory organs. Often, this is observed in newborn children with incorrect posture during sleep.
- In case of drowning
- When various substances enter the respiratory tract.
Pulmonary edema may be cardiogenic and non-cardiogenic. Cardiogenic pulmonary edema occurs as a result of left heart failure. Insufficiency occurs for the following reasons:
- Ventricular pathology – heart disease, myocardial infarction, myocarditis, cardiosclerosis.
- Pathological abnormalities of the atrium.
Important . Non-cardiogenic edema occurs as a result of drug overuse.
Symptoms of pulmonary edema
Symptoms of the disease arise suddenly often at night (due to the patient’s supine position):
- Attacks of painful, severe suffocation are intensified in a supine position, so the patient sits or stands. This is due to a lack of oxygen.
- Shortness of breath occurs even at rest
- Painful sensations in chest due to insufficient oxygen.
- A sharp increase in breathing (due to stimulation of the respiratory center by carbon dioxide that has not been released).
- Palpitations
- Cough with pink sputum
- The patient's face has a gray-bluish tint, and after a while it affects all parts of the body. This is due to changes in the release of carbon dioxide from the blood.
- Pale skin and cold, clammy sweat
- Veins in the neck area swell due to stagnation in the pulmonary circulation
- Blood pressure increases
- Patient's confusion
- Thready, weak pulse
Diagnostics
In addition to a visual examination of the patient admitted with the first symptoms of pulmonary edema, the specialist must conduct instrumental and laboratory research, to confirm the accuracy of the diagnosis. Diagnostics involves the following procedures: 
- Carrying out blood gas studies.
- Biochemical blood test.
- Electrocardiogram
- Ultrasound of the heart
- Breast X-ray.
The results of the procedures will allow us to determine not only the treatment regimen, but also the cause of the disease.
Pulmonary edema in children
Pulmonary edema in children most often manifests itself as a result of pathology of the cardiovascular system. This may be an allergic reaction or due to inhalation of toxic components. Swelling can occur at any time, but most often occurs at night. The baby is worried and even frightened by a significant lack of air. Among the main symptoms of pulmonary edema in children are:
- Cough
- Dyspnea
- Foamy pink sputum
- Wheezing
- Blueness of the skin
In newborn babies, pulmonary edema can occur due to the following pathologies:
- Placental infarction is the death of cells in a separate area of the placenta. As a result, blood flows poorly to the fetus and hypoxia may occur.
- Aspiration of amniotic fluid is penetration of amniotic fluid into the lower respiratory tract.
- Prenatal or birth brain injury.
- Heart defects.
First aid for pulmonary edema
Before the ambulance arrives, you can do the following on your own:
- Sit the patient so that the legs are down
- Provide rapid access to a large peripheral vein
- Organize then fresh air
- Organize a hot foot bath
- Allow the patient to inhale alcohol vapor
- Track breathing and pulse
- Apply venous tourniquets to the extremities
- If the pressure is not reduced, you can take 1-2 tablets of nitroglycerin under the tongue.
Algorithm for the treatment of pulmonary edema
Therapy for pulmonary edema consists of 7 stages:
- Sedative therapy
- Defoaming
- Vasodilator therapy
- Diuretics
- Cardiac glycosides and glucocorticoids
- Blood exfusion
- Hospitalization of the patient.
Basic therapy includes:
- For liver cirrhosis, a course of hepatoprotectors is prescribed
- In case of pancreatic necrosis, drugs are initially prescribed that inhibit the functioning of the pancreas, and then drugs that stimulate the healing of necrosis.
- Comprehensive treatment of myocardial infarction
- For bronchopulmonary diseases, a course of antibiotics is required.
- In case of toxic edema, detoxification therapy is necessary. Salt mixtures help replenish fluid that was lost due to the use of diuretics.
- For asthma - expectorants, mucolytics, bronchodilators.
- For toxic shock - antihistamines
- Edema of any form requires the use of potent antibiotics and antiviral drugs.
Duration of therapy pulmonary edema depends on the form of the disease, concomitant diseases, general condition and the patient's age. Often times can vary from 1 to 4 weeks.
Additional Information. If the swelling proceeds without any complications and with effective therapy, the treatment period is no more than 10 days.
Possible consequences after emergency care:
- Transition to lightning-fast degree of edema
- Due to the rapid production of foam, airway obstruction occurs
- Respiratory depression
- Tachyarrhythmia
- Asystole
- Angious pain. The pain is so severe that the patient may go into painful shock.
- Inability to normalize blood pressure. Pulmonary edema often occurs with low or high blood pressure, which can alternate. The vessels cannot withstand these changes for a long period, as a result of which the patient’s condition worsens significantly.
- Pulmonary edema increases as a result of increased blood pressure.
Prevention
Prevention is based on early detection of the disease, causing swelling lungs. Patients suffering from chronic insufficiency should follow a diet that is based on: limiting the amount of salt consumed, liquids, avoiding fatty foods and reduction of physical activity. As a result of the presence of chronic pulmonary diseases, you should constantly consult with a specialist and carry out therapy in outpatient setting, twice a year, provide treatment in a hospital, prevent factors that can worsen the patient’s condition (interaction with allergens, acute respiratory diseases, smoking cessation).
– acute pulmonary failure associated with massive release of transudate from the capillaries into the lung tissue, which leads to infiltration of the alveoli and a sharp disruption of gas exchange in the lungs. Pulmonary edema is manifested by shortness of breath at rest, a feeling of tightness in the chest, suffocation, cyanosis, cough with foamy bloody sputum, bubbling breathing. Diagnosis of pulmonary edema involves auscultation, radiography, ECG, echocardiography. Treatment of pulmonary edema requires intensive therapy, including oxygen therapy, administration narcotic analgesics, sedatives, diuretics, antihypertensive drugs, cardiac glycosides, nitrates, protein drugs.
General information
Pulmonary edema - clinical syndrome, caused by the exudation of the liquid part of the blood into the lung tissue and accompanied by impaired gas exchange in the lungs, the development of tissue hypoxia and acidosis. Pulmonary edema can complicate the course of a variety of diseases in pulmonology, cardiology, neurology, gynecology, urology, gastroenterology, and otolaryngology. In case of untimely provision necessary assistance Pulmonary edema can be fatal.
Causes
The etiological reasons for pulmonary edema are varied. In cardiological practice, pulmonary edema can be complicated by various diseases. of cardio-vascular system: atherosclerotic and post-infarction cardiosclerosis, acute myocardial infarction, infective endocarditis, arrhythmias, hypertension, heart failure, aortitis, cardiomyopathies, myocarditis, atrial myxomas. Pulmonary edema often develops against the background of congenital and acquired heart defects - aortic insufficiency, mitral stenosis, aneurysm, coarctation of the aorta, open ductus arteriosus, ASD and VSD, Eisenmenger syndrome.
In pulmonology, pulmonary edema may be accompanied by a severe course chronic bronchitis and lobar pneumonia, pneumosclerosis and emphysema, bronchial asthma, tuberculosis, actinomycosis, tumors, pulmonary embolism, pulmonary heart disease. The development of pulmonary edema is possible with chest injuries accompanied by prolonged crush syndrome, pleurisy, pneumothorax.
In some cases, pulmonary edema is a complication of infectious diseases that occur with severe intoxication: ARVI, influenza, measles, scarlet fever, diphtheria, whooping cough, typhoid fever, tetanus, polio.
Pulmonary edema in newborns may be associated with severe hypoxia, prematurity, and bronchopulmonary dysplasia. In pediatrics, the danger of pulmonary edema exists in any condition associated with obstruction of the airway - acute laryngitis, adenoids, foreign bodies in the respiratory tract, etc. Similar mechanism the development of pulmonary edema is observed with mechanical asphyxia: hanging, drowning, aspiration of gastric contents into the lungs.
In nephrology, pulmonary edema can lead to acute glomerulonephritis, nephrotic syndrome, renal failure; in gastroenterology – intestinal obstruction, liver cirrhosis, acute pancreatitis; in neurology - acute stroke, subarachnoid hemorrhage, encephalitis, meningitis, tumors, head injury and brain surgery.
Pulmonary edema often develops as a result of poisoning chemicals(fluorine-containing polymers, organophosphorus compounds, acids, metal salts, gases), intoxication with alcohol, nicotine, drugs; endogenous intoxication in case of extensive burns, sepsis; acute poisoning medicines(barbiturates, salicylates, etc.), acute allergic reactions (anaphylactic shock).
In obstetrics and gynecology, pulmonary edema is most often associated with the development of eclampsia in pregnancy and ovarian hyperstimulation syndrome. It is possible to develop pulmonary edema against the background of prolonged mechanical ventilation with high concentrations of oxygen, uncontrolled intravenous infusion of solutions, thoracentesis with rapid simultaneous evacuation of fluid from pleural cavity.
Pathogenesis
The main mechanisms for the development of pulmonary edema include sharp increase hydrostatic and decreased oncotic (colloid-osmotic) pressure in the pulmonary capillaries, as well as impaired permeability of the alveolar capillary membrane.
The initial stage of pulmonary edema consists of increased filtration of transudate into the interstitial lung tissue, which is not balanced by the reabsorption of fluid into vascular bed. These processes correspond to the interstitial phase of pulmonary edema, which clinically manifests itself as cardiac asthma.
Further movement of protein transudate and pulmonary surfactant into the lumen of the alveoli, where they mix with air, is accompanied by the formation of persistent foam, which prevents the flow of oxygen to the alveolar-capillary membrane, where gas exchange occurs. These disorders characterize the alveolar stage of pulmonary edema. The shortness of breath resulting from hypoxemia helps to reduce intrathoracic pressure, which in turn increases blood flow to the right side of the heart. In this case, the pressure in the pulmonary circulation increases even more, and the leakage of transudate into the alveoli increases. Thus, a vicious circle mechanism is formed, causing the progression of pulmonary edema.
Classification
Taking into account the trigger mechanisms, cardiogenic (heart), non-cardiogenic (respiratory distress syndrome) and mixed pulmonary edema are distinguished. The term non-cardiogenic pulmonary edema combines various cases not associated with cardiovascular diseases: nephrogenic, toxic, allergic, neurogenic and other forms of pulmonary edema.
Depending on the course, the following types of pulmonary edema are distinguished:
- fulminant– develops rapidly, within a few minutes; always ending in death
- spicy– increases quickly, up to 4 hours; even if started immediately resuscitation measures It is not always possible to avoid death. Acute pulmonary edema usually develops with myocardial infarction, head injury, anaphylaxis, etc.
- subacute– has a wave-like flow; Symptoms develop gradually, sometimes increasing and sometimes subsiding. This variant of the course of pulmonary edema is observed with endogenous intoxication of various origins (uremia, liver failure, etc.)
- protracted– develops in the period from 12 hours to several days; may proceed smoothly, without characteristic clinical signs. Prolonged pulmonary edema occurs when chronic diseases lungs, chronic heart failure.
Symptoms of pulmonary edema
Pulmonary edema does not always develop suddenly and rapidly. In some cases, it is preceded by prodromal signs, including weakness, dizziness and headache, feeling of tightness in the chest, tachypnea, dry cough. These symptoms may occur minutes or hours before pulmonary edema develops.
The clinical picture of cardiac asthma (interstitial pulmonary edema) can develop at any time of the day, but more often it occurs at night or in the early morning hours. An attack of cardiac asthma can be provoked physical activity, psycho-emotional stress, hypothermia, disturbing dreams, transition to horizontal position and other factors. In this case, sudden suffocation or paroxysmal cough occurs, forcing the patient to sit down. Interstitial pulmonary edema is accompanied by the appearance of cyanosis of the lips and nails, cold sweat, exophthalmos, agitation and motor restlessness. Objectively, a RR of 40-60 per minute, tachycardia, increased blood pressure, and participation of auxiliary muscles in the act of breathing are detected. Breathing is increased, stridorous; On auscultation, dry wheezing may be heard; There are no moist rales.
At the stage of alveolar pulmonary edema, severe respiratory failure, severe shortness of breath, diffuse cyanosis, puffiness of the face, and swelling of the neck veins develop. In the distance, bubbling breathing can be heard; Auscultation reveals moist rales of various sizes. When breathing and coughing, foam is released from the patient's mouth, often having a pinkish tint due to sweating shaped elements blood.
With pulmonary edema, lethargy, confusion, and even coma quickly increase. In the terminal stage of pulmonary edema, blood pressure decreases, breathing becomes shallow and periodic (Cheyne-Stokes breathing), and the pulse becomes thready. The death of a patient with pulmonary edema occurs due to asphyxia.
Diagnostics
In addition to assessing physical data, laboratory and laboratory parameters are extremely important in the diagnosis of pulmonary edema. instrumental studies. All studies are performed as quickly as possible, sometimes in parallel with emergency care:
- Blood gas study. Pulmonary edema is characterized by certain dynamics: at the initial stage there is moderate hypocapnia; then, as pulmonary edema progresses, PaO2 and PaCO2 decrease; on late stage there is an increase in PaCO2 and a decrease in PaO2. Blood CBS indicators indicate respiratory alkalosis. Measurement of central venous pressure during pulmonary edema shows its increase to 12 cm of water. Art. and more.
- Biochemical screening. In order to differentiate the causes that led to pulmonary edema, a biochemical study of blood parameters (CPK-MB, cardiac-specific troponins, urea, total protein and albumin, creatinine, liver tests, coagulogram, etc.).
- ECG and EchoCG. An electrocardiogram with pulmonary edema often reveals signs of left ventricular hypertrophy, myocardial ischemia, and various arrhythmias. According to cardiac ultrasound, zones of myocardial hypokinesia are visualized, indicating a decrease in left ventricular contractility; ejection fraction is reduced, end-diastolic volume is increased.
- X-ray of the chest organs. Reveals expansion of the borders of the heart and roots of the lungs. With alveolar pulmonary edema in the central parts of the lungs, a homogeneous symmetrical darkening in the shape of a butterfly is detected; less often - focal changes. Possible availability pleural effusion moderate or large volume.
- Pulmonary artery catheterization. Allows you to conduct differential diagnosis between non-cardiogenic and cardiogenic pulmonary edema.
Treatment of pulmonary edema
Treatment of pulmonary edema is carried out in the ICU under constant monitoring of oxygenation and hemodynamics. Emergency measures in the event of pulmonary edema include:
- giving the patient a sitting or half-sitting position (with the head of the bed raised), applying tourniquets or cuffs to the limbs, hot foot baths, bloodletting, which helps reduce venous return to the heart.
- It is more expedient to supply humidified oxygen during pulmonary edema through antifoam agents - antifomsilan, ethyl alcohol.
- if necessary, transfer to mechanical ventilation. If there are indications (for example, to remove a foreign body or aspiration of contents from the respiratory tract), tracheostomy is performed.
- administration of narcotic analgesics (morphine) to suppress the activity of the respiratory center.
- administration of diuretics (furosemide, etc.) to reduce blood volume and dehydration of the lungs.
- administration of sodium nitroprusside or nitroglycerin to reduce afterload.
- the use of ganglion blockers (azamethonium bromide, trimethaphan) can quickly reduce pressure in the pulmonary circulation.
According to indications, patients with pulmonary edema are prescribed cardiac glycosides, antihypertensive, antiarrhythmic, thrombolytic, hormonal, antibacterial, antihistamines, infusions of protein and colloidal solutions. After stopping the attack of pulmonary edema, treatment of the underlying disease is carried out.
Prognosis and prevention
Regardless of the etiology, the prognosis for pulmonary edema is always extremely serious. In acute alveolar pulmonary edema, mortality reaches 20-50%; if edema occurs against the background of myocardial infarction or anaphylactic shock, the mortality rate exceeds 90%. Even after successful relief of pulmonary edema, complications are possible in the form of ischemic damage to internal organs, congestive pneumonia, pulmonary atelectasis, and pneumosclerosis. If the root cause of pulmonary edema is not eliminated, there is a high probability of its recurrence.
A favorable outcome is greatly facilitated by early pathogenetic therapy undertaken in the interstitial phase of pulmonary edema, timely detection of the underlying disease and its targeted treatment under the guidance of a specialist in the appropriate profile (pulmonologist, cardiologist, infectious disease specialist, pediatrician, neurologist, otolaryngologist, nephrologist, gastroenterologist, etc.) .