Inflammatory disease mucous membrane of the oral cavity, often infectious or allergic genesis. Stomatitis in children is manifested by local symptoms (hyperemia, swelling, rashes, plaque, ulcers on the mucous membrane) and a violation of the general condition (fever, refusal to eat, weakness, adynamia, etc.). Recognition of stomatitis in children and its etiology is carried out by a pediatric dentist based on an examination of the oral cavity, additional laboratory tests. Treatment of stomatitis in children includes local treatment of the oral cavity and systemic etiotropic therapy.

General information
Causes of stomatitis in children
The condition of the oral mucosa depends on the influence of external (infectious, mechanical, chemical, physical agents) and internal factors(genetic and age characteristics, immune status, concomitant diseases).
Viral stomatitis ranks first in terms of frequency of spread; of these, at least 80% of cases are herpetic stomatitis in children. Less commonly, stomatitis of viral etiology develops in children against the background of chickenpox, measles, influenza, rubella, infectious mononucleosis, adenovirus, papillomavirus, enterovirus, HIV infection, etc.
Stomatitis of bacterial etiology in children can be caused by staphylococcus, streptococcus, as well as pathogens of specific infections - diphtheria, gonorrhea, tuberculosis, syphilis. Symptomatic stomatitis in children develops against the background of diseases of the gastrointestinal tract (gastritis, duodenitis, enteritis, colitis, intestinal dysbiosis), blood system, endocrine, nervous system, helminthic infestations.
Traumatic stomatitis in children occurs due to mechanical injury oral mucosa with a pacifier, toy; teething or biting lips, cheeks, tongue; brushing teeth; burns to the oral cavity from hot food (tea, soup, jelly, milk), damage to the mucous membrane during dental procedures.
Allergic stomatitis in children may develop as a reaction to local exposure to an allergen (ingredients in toothpaste, lozenges or chewing gum with artificial colors and flavors, medicines, etc.).
Prematurity, poor oral hygiene, accumulation of dental plaque, caries, wearing braces, frequent general morbidity, deficiency of vitamins and microelements (B vitamins, folic acid, zinc, selenium, etc.), application medicines, changing the microflora of the oral cavity and intestines (antibiotics, hormones, chemotherapy drugs).
The mucous membrane of the oral cavity in children is thin and easily injured, so it can be injured even with a slight impact on it. The microflora of the oral cavity is very heterogeneous and is subject to significant fluctuations depending on nutritional habits, the state of the immune system and concomitant diseases. When defenses are weakened, even representatives normal microflora oral cavity (fusobacteria, bacteroides, streptococci, etc.) can cause inflammation. The barrier properties of saliva in children are poorly expressed due to the insufficient functioning of local immune factors (enzymes, immunoglobulins, T-lymphocytes and other physiological factors). active substances). All these circumstances determine the frequent incidence of stomatitis in children.
Symptoms of stomatitis in children
Viral stomatitis in children
The course and features of herpetic stomatitis in children are discussed in detail in the corresponding article, so in this review we will focus on the general symptoms viral infection oral cavity, characteristic of various infections.
The main symptom of viral stomatitis in children is the appearance of quickly opening blisters on the oral mucosa, in place of which small round or oval erosions, covered with fibrinous plaque, then form. Vesicles and erosions can appear as separate elements or have the character of defects merging with each other.
They are extremely painful and, as a rule, are located against the background of a brightly hyperemic mucous membrane of the palate, tongue, cheeks, lips, and larynx. Local manifestations of viral stomatitis in children are combined with other signs of infection caused by this virus (skin rash, fever, intoxication, lymphadenitis, conjunctivitis, runny nose, diarrhea, vomiting, etc.) Erosions are epithelialized without a scar.
Candidal stomatitis in children
The development of specific local symptoms of candidal stomatitis in children is preceded by excessive dryness of the mucous membrane, a burning sensation and bad taste in the mouth, bad breath. Infants are capricious while eating, refuse the breast or bottle, behave restlessly, and sleep poorly. Soon on inside Small white dots appear on the cheeks, lips, tongue and gums, which, merging, form a rich white plaque of a cheesy consistency.
In severe forms of candidal stomatitis in children, the plaque acquires a dirty gray tint and is difficult to remove from the mucous membrane, revealing a swollen surface that bleeds at the slightest touch.
In addition to pseudomembranous candidal stomatitis described above, atrophic candidal stomatitis occurs in children. It usually develops in children wearing orthodontic appliances and occurs with scant symptoms: redness, burning, dryness of the mucous membrane. Plaque is found only in the folds of the cheeks and lips.
Repeated episodes of candidal stomatitis in children may indicate the presence of other serious illnesses – diabetes mellitus, leukemia, HIV. Complications of fungal stomatitis in children may include genital candidiasis (vulvitis in girls, balanoposthitis in boys), visceral candidiasis (esophagitis, enterocolitis, pneumonia, cystitis, arthritis, osteomyelitis, meningitis, ventriculitis, encephalitis, brain microabscesses), candidosepsis.
Bacterial stomatitis in children
The most common type of bacterial stomatitis in childhood is impetiginous stomatitis. It is indicated by a combination of the following local and common features: dark red color of the oral mucosa with merging superficial erosions; the formation of yellow crusts that stick together the lips; increased salivation; unpleasant putrid odor from the mouth; low-grade or febrile temperature.
With diphtheria stomatitis in children, fibrinous films form in the oral cavity, after removal of which an inflamed, bleeding surface is exposed. With scarlet fever, the tongue is covered with a dense whitish coating; after its removal, the tongue becomes bright crimson in color.
Gonorrheal stomatitis in children is usually combined with gonorrheal conjunctivitis, in rare cases - with arthritis of the temporomandibular joint. The child becomes infected when passing through the infected genital tract of the mother during childbirth. The mucous membrane of the palate, back of the tongue, lips is bright red, sometimes lilac-red, with limited erosions, from which yellowish exudate is released.
Aphthous stomatitis in children
Prevention of stomatitis in children
Prevention of stomatitis in children consists of excluding any microtraumas, careful hygiene care for the oral cavity, treatment of concomitant pathologies. To reduce the risk of stomatitis in children infancy it is important to regularly disinfect pacifiers, bottles, toys; treat the mother's breasts before each feeding. Adults should not lick a baby's pacifier or spoon.
From the moment the first teeth erupt, it is necessary regular visit dentist for preventive measures. To clean children's teeth, it is recommended to use special toothpastes that help increase local immunity of the oral mucosa.
– a collective term that combines numerous types of inflammatory lesions of the oral mucosa. In the practice of a pediatric dentist, this is one of the most common reasons for treatment, and every child, at least once, has encountered this disease.
Table of contents:Prevalence of stomatitis
Stomatitis has an extensive classification, it is based on the causes of its occurrence: bacteria, viruses, fungi, or allergic reactions, injuries, manifestations of diseases internal organs. In children under one year of age, stomatitis has features of its course, diagnosis and treatment.
note
In children under one year of age, stomatitis occurs in a rather painful form and, despite treatment, a high percentage of their recurrence remains.
Analyzing the data, in children under one year old, stomatitis is most often provoked by microbes, viruses or fungi, less often it is a manifestation of allergies or diseases of internal organs. Each of these forms has its own specific symptoms and treatment recommendations.
But, despite all the diversity of reasons, we can identify commonality among all forms:
- predisposing factors;
- symptoms;
- general principles of treatment and prevention.
Predisposing factors for stomatitis
One of the main predisposing factors for the development of stomatitis will be a decrease in work immune defense. In children, the immune system is just learning to respond correctly to external and internal threats; its work is not perfect. Consequently, children are at risk for developing numerous diseases of the teeth and gums, including stomatitis.
How younger child, the greater the chance of developing stomatitis. As you grow older and your immune system improves, such risks decrease.
Stomatitis often forms against the background of infectious diseases, at the moment of teething, when children put everything that comes to hand into their mouths, sometimes these objects are contaminated with pathogens various diseases. Violation of the rules of basic hygiene is also one of the reasons for the formation of inflammation of the mucous membrane.
Sources of infection can be the parents themselves, licking the baby’s nipples for the purpose of “disinfection,” kissing the baby on the lips, etc. By the way, this is how caries-forming bacteria are transmitted. An adult body can cope with and suppress the growth of opportunistic microflora, but a baby under one year old may be at risk.
Predisposing factors also include poor oral hygiene, especially if the child is bottle-fed. The mixture is a nutrient medium for the proliferation of pathogenic flora, which, when the immune defense is reduced or against the background of teething, leads to the formation of stomatitis.
Trauma, often of a chronic nature (Bednar's aphthae), can become a predisposing factor for the development of stomatitis.
Types and symptoms of stomatitis in infants
What is common among all stomatitis is the manifestation of inflammation of the mucous membrane: redness, erosion, ulcers or the formation of dense plaque, sometimes this is a combination of all the main manifestations. Their severity will depend on the severity of stomatitis.
Despite the similarity of symptoms, dentists and pediatricians do not have any difficulties in diagnosis, and sometimes an examination of the oral cavity is sufficient to determine the form and cause of the disease.
note
In some cases, when stomatitis is caused by bacteria, scraping and culture may be required to identify the specific pathogen and determine its sensitivity to antibiotics.
In children under one year of age, the following forms of stomatitis are most often diagnosed:
- candida;
- allergic;
- microbial;
- Bednar aphthae
- herpetic;
- aphthous.
Each of these forms is characterized by specific symptoms and features of the baby’s condition, which are used for diagnosis.
Candidal stomatitis in infants (thrush)
To relieve the symptoms of allergic stomatitis, specialists prescribe: painkillers, antiseptics to prevent secondary infections, etc.
Microbial stomatitis
 Microbial stomatitis can be considered as an independent nosological form, or as a complication of another form of stomatitis, when a secondary infection occurs.
Microbial stomatitis can be considered as an independent nosological form, or as a complication of another form of stomatitis, when a secondary infection occurs.
The main causative agents of microbial stomatitis will be and.
Symptoms of primary stomatitis will be the appearance of islands of white to dirty yellow plaque on the mucous membrane, which gradually turns into ulcers and aphthae. There is redness of the mucous membrane and swelling. When ulcers form on the gum tissue, bleeding occurs.
The secondary form of microbial stomatitis, which is a complication, has similar symptoms: films form on the primary lesions in the child’s oral cavity - from white to gray. Bad breath appears, and the baby’s condition worsens: whims intensify, body temperature rises, and appetite disappears. In children weakened by the disease, a reaction of the regional lymph nodes is observed.
To diagnose microbial stomatitis and prescribe qualified treatment, dentists can prescribe a number of research measures: a blood test, scraping from the mucous membrane, followed by determination of the pathogen and its sensitivity to antibiotics.
After diagnosis, dentists prescribe treatment: appointment or local use antiseptics, restorative measures and keratolytics - means that promote the rapid restoration of the mucous membrane. Treatment of microbial stomatitis cannot be considered complete without stopping the underlying disease, which has become a predisposing factor for its development.
Afty Bednar
Bednar's aphthae is one of the forms of traumatic stomatitis, characteristic of children in the first year of life. May occur in older children. Symptoms of the disease are ulcers that occur at the border of the soft and hard palate.
- chronic traumatic impact on this border: the use of incorrectly selected nipples or pacifiers. Essentially, this is a disease that threatens children who are artificial feeding. The pacifier is a traumatic agent;
- poor oral hygiene;
- vitamin deficiency;
- Availability bad habits– thumb sucking;
- decreased immune function.
Sometimes the development of Bednar's afts requires the action of several causes at once, which can also be considered as predisposing factors.
Bednar's aphthae are not characterized by variations in clinical symptoms; they are always the same manifestations: ulcers at the junction of the hard palate with the soft palate, their shape is round or oval, their location is symmetrical. Gradually they become covered with a yellowish coating.
note
In children born ahead of schedule, aphthae appear against the background of disease, are associated with decreased immunity, and the border of the lesion can be extensive.
 Children suffer from pain and refuse to eat. In some cases, feeding in the usual way (using a bottle) is not possible.
Children suffer from pain and refuse to eat. In some cases, feeding in the usual way (using a bottle) is not possible.
When ulcers appear, the body temperature rises, and the child’s condition worsens.
Treatment of Bednar's aphthae is carried out comprehensively and depends on the general condition of the baby. Initially, dentists, together with pediatricians, think through feeding tactics for the baby, and then develop treatment to alleviate symptoms and combat clinical manifestations.
Enzymes are often prescribed for the treatment of ulcers: treatment of the oral cavity with lysozyme, trypsin.
Usage medicinal plants with a pronounced antiseptic and anti-inflammatory effect is considered as therapeutic and prophylactic measures to prevent the addition of a secondary infection.
After assessing the condition of children and clinical symptoms, doctors can prescribe a course of means for the rapid restoration of the oral mucosa - keratolytics.
For almost all forms and types of stomatitis, which are accompanied by the formation of ulcers, aphthae and erosions, dentists prescribe drugs for rapid epithelization of the mucous membrane. These include oil solution vitamin A, sea buckthorn oil, solcoseryl ointment, etc.
How to treat stomatitis in infants?
Except individual treatment stomatitis, dentists are given general recommendations, regardless of the form and type of inflammation. These tips can be considered not only therapeutic, but also preventive, aimed at alleviating the baby’s condition.
As soon as parents notice the first signs of inflammatory changes in the baby’s oral cavity, it is necessary to take care of satisfactory oral hygiene.
Teeth brushing using a special one should begin as soon as the first tooth appears in the baby’s mouth. The use of toothpaste is not necessary. This decision is made by parents after consultation with the dentist.
Poor oral hygiene or lack thereof can be a predisposing factor for secondary infection. Parents should take care to prevent its spread to family members: a sick child should have individual cutlery, dishes, towels, and toys. During the stages of recovery it is necessary to change toothbrush, regardless of the timing of its use.
Your baby's toothbrush should be replaced every 2-3 months, or depending on its condition.
 It is necessary to take care of the baby’s adequate nutrition and the possibility of feeding him. During illness, it is recommended to avoid irritating foods and complementary foods. After each feeding, parents should take care of oral hygiene - at least rinse their mouth.
It is necessary to take care of the baby’s adequate nutrition and the possibility of feeding him. During illness, it is recommended to avoid irritating foods and complementary foods. After each feeding, parents should take care of oral hygiene - at least rinse their mouth.
After consultation with a pediatrician or dentist, therapy is selected aimed at alleviating the baby’s general condition: normalizing body temperature, increasing the body’s resistance, etc.
One of the main factors successful treatment any form of stomatitis in children under one year of age - check the parents. In most cases, the source of infection is the parents. In this case, care must be taken to treat and prevent the spread of infection.
Prevention of stomatitis
Preventive measures are aimed at eliminating the main cause of stomatitis - most often it is infection with bacteria, viruses and fungi. To achieve these goals, it is enough to follow basic hygiene rules: wash your hands more often, do not kiss the child on the lips, do not lick his nipples and all objects that can get into the child’s mouth.
note
Children born prematurely, with congenital or chronic diseases, and with reduced immune defense require special attention in terms of preventive measures. Such kids increased risks formation of stomatitis.
Improving oral hygiene in children younger age, timely treatment diseases of internal organs and contacting specialists will help not only quickly get rid of the symptoms of stomatitis, but also prevent the occurrence of complications.
Complications of stomatitis in children under one year of age
Complications of stomatitis are as varied as their forms. But it is still possible to highlight general complications, the most common of which is the addition of a secondary infection, for example, candidal stomatitis is complicated by a microbial one.
The second, no less common complication is the transition of the disease to a chronic form and frequent relapses. Typically, their occurrence is associated with infectious or somatic diseases.
Stomatitis is an inflammation of the oral mucosa. The name comes from the Latin word “stoma” (mouth). Stomatitis occurs in both children and adults, but most often it appears in infants and preschoolers. This happens because the mucous membrane at this age is thinner and more delicate. It is more common for everyone to say “stomatitis”, but it would be more correct to say “stomatitis”, since this is a general concept for a whole group of diseases.
Causes of stomatitis in children
What causes stomatitis in children? The causes of this disease in a child are different. These are both dirty hands and fragile children's immunity, and features of thermoregulation, on which the respiratory system directly depends. You need to understand that a child’s mucous membrane, unlike an adult’s, is a very thin and vulnerable substance, so any infection occurs very quickly. IN early age the child has not yet fully formed salivation, but the enzymes in saliva play a very important role important role in protecting the body. As a result, the mucous membrane often dries out, cracks appear, infection occurs, followed by stomatitis. Long-term use cannot be ignored medications, for example, antibiotics, also neuropsychiatric disorders, unfavorable living conditions, poor child care and poor oral hygiene among the parents themselves.
Often it is the parents who help the doctor find out the cause of the disease. Only they can try to analyze what caused the blister, ulcer or plaque to appear. For example, the child ate something wrong, they bought a new toothpaste or toothbrush, or maybe the baby suffered a temperature change.
What are the types of stomatitis in a child?
Depending on the causes, stomatitis can be divided into several types, each of which has a number of characteristics.
Viral, herpes, or herpetic stomatitis in children
One of the most common types of childhood stomatitis is caused by a virus. herpes simplex. Usually a child becomes infected with it through airborne droplets. The virus is also transmitted through dishes, toys, and household items. Most often, herpetic stomatitis appears in a child between the ages of one and four years. The disease begins like a cold, accompanied by lethargy and fever. Sometimes a runny nose and cough occur. Around the second day, small round or oval erosions of a light yellow color with a bright red border appear on the lips, tongue, and inside of the cheeks. Swelling appears, the gums begin to bleed, and the child refuses to eat.
Traumatic stomatitis The child has
The disease is caused by mechanical trauma to the oral cavity. For example, burns from hot food, a too-hard pacifier, the habit of chewing a pencil. Also, traumatic stomatitis often occurs in children with malocclusion due to frequent biting of cheeks and tongue.
Candidal stomatitis
Appears in children under one year of age. The cause is fungi of the Candida species. The main symptom is the appearance of white plaque in the baby’s mouth. It is worth noting that it should not be confused with the usual plaque after feeding. A cause for alarm is if the plaque does not go away and the child refuses to eat.
Drug-induced or allergic stomatitisin children
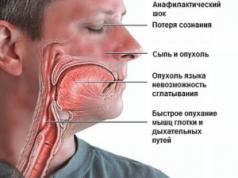
Caused by certain allergies or reactions to medications. If this type of disease is suspected, the allergen should be identified and removed, otherwise there is a risk of getting unpleasant consequences, up to anaphylactic shock.
Each type of stomatitis is characterized by a certain childhood. In young children, candidal or fungal infections (thrush) are often observed. At the age of “I want to know everything” in a child of 3-4 years old, stomatitis, as a rule, is infectious nature when the infection gets through dirty hands or objects. From three to six years old we often observe an acute herpetic type of disease.
Symptoms of stomatitis in children
For all types of stomatitis, the common and defining signs are inflammation of the oral mucosa and the appearance on any of its parts, such as the tongue, the inner side of the lips, cheeks, pharynx, of various formations in the form of erosions, blisters, characteristic plaque, and in cases of traumatic stomatitis - traces from burns and biting. It is important to understand that stomatitis is not just one acute or chronic illness with certain classical symptoms, each species has its own special reason, and they manifest themselves in the oral cavity in different ways, so they need to be treated differently.
How to treat stomatitis in children
As we have already found out, there is no single algorithm for treating stomatitis in children. Each case is individual in its own way. Very often it happens like this: a mother comes in the hope that the doctor will prescribe an ointment, and she will immediately cure the child with it. This doesn't happen! It is necessary to understand what preceded the inflammation, taking into account the child’s age, stage and severity of the disease. Treatment is carried out both locally and symptomatically, i.e. symptoms are relieved. Doctors - pediatric dentist and pediatrician - give their recommendations, it is possible to involve highly specialized specialists, such as ENT, mycologist, dermatologist. Of course, there are some textbook principles that experts follow to relieve or ease pain and prevent complications. We are talking about compliance with the rules of oral hygiene, diet and sleep, treatment of the mucous membrane special gels, solutions and applications. For example, for allergic stomatitis in children, antihistamines are recommended, for herpetic forms - antiviral drugs, and if there is a fever - antipyretics. It is important to immediately contact a specialist when you discover a problem.
Caring for a child with stomatitis
Parental involvement in treatment and proper care for the child are not just important - they are decisive. With stomatitis, it is necessary to strictly follow the treatment plan, which is often very labor-intensive, so the result depends on parental care and control. The oral cavity is a kind of epicenter of pain, so it is not surprising that the child will be capricious a lot. Therefore, it is important for parents to be patient and persistent.
Nutritional Features
Most mothers and fathers are concerned about the question of how to feed a child with stomatitis. Firstly, it is necessary to eat only soft, warm and mushy foods, for example in the form of purees. The main thing is that the food is high in calories and positive, because the child’s immunity is already weakened. After eating, be sure to rinse your mouth so as not to provoke or add any additional infection. If a child is ill, the diet should include the exclusion of spicy, sour, sweet foods and citrus fruits.
Pain relief and care
For stomatitis in children, pain relief is necessary. It is carried out with the help of various medications in order to avoid food refusal and poor sleep. In addition, for stomatitis in children, proper treatment of the oral cavity is very important. A doctor should recommend what to treat and rinse a child’s mouth with.
How to treat stomatitis in children at home?
On the Internet you can find descriptions of many ways to treat stomatitis in children at home. However, experts consider many of these virtual tips not only useless, but also dangerous. There is always a risk of allergies, so you should not use infusions and decoctions, even if you are absolutely sure that it will not harm the child. Instead of wasting time, it is necessary to undergo diagnostics and consultation with a dentist and pediatrician, who will prescribe the correct treatment regimen.
Why is stomatitis dangerous in a child?
Complications of stomatitis in children manifest themselves in the form of inflammation, which from the oral cavity can spread to the skin of the face, the corners of the lips and the lips themselves or penetrate into the body, and secondary infections are also possible. Against this background, severe general state, accompanied by fever, general intoxication, damage to the nervous system, convulsions, etc. In medical practice, there have even been recorded deaths caused by odontogenic infections.
Prevention of stomatitis in children
If a person has had stomatitis at least once in his life, there will always be a risk of its recurrence, so prevention comes to the fore:
Strengthening the immune system to prevent the disease from returning.
Both parents and children should follow simple rules of oral hygiene.
Mandatory observation by a dentist 2 - 3 times a year, even if nothing bothers the child, with a period of dental clinic professional hygienic cleaning.
It is advisable when selecting funds personal hygiene follow the recommendations of your treating dentist.
Remember, the main thing is to eliminate the cause of stomatitis. Therefore, the child simply needs to be shown to a doctor. Only he can tell you how to treat childhood stomatitis. Self-medication can only worsen the course of the disease and prolong the suffering of your baby.
Young children may suddenly develop a high fever, become capricious, and turn away from food. Older children complain of pain in the mouth. Upon careful examination, parents may notice redness or sores on the cheeks, tongue, palate, or inside of the lip. All these are signs of stomatitis. This disease can be caused by different types of pathogens, such as the herpes virus, ordinary bacteria, and fungi. In addition, stomatitis can be toxic or allergic. So how to treat stomatitis in children? Let's try to figure this out.
Types of stomatitis
Interesting, but each type of stomatitis is characteristic for a certain age of the child.
- Children under one year of age are susceptible to candidal stomatitis, which is caused by a fungus. It is found on the skin and mucous membranes, but if the child has a weakened immune system or takes antibiotics, the fungus begins to multiply rapidly. Forms in the mouth white coating, the mucous membrane begins to dry. If the disease is not treated, cracks appear.
- A child between one and three years of age suffers from herpetic stomatitis. It is transmitted through shared utensils from parents.
- Schoolchildren often experience allergic or aphthous stomatitis. Allergic stomatitis occurs when consuming certain foods or medications. With aphthous disease, the entire oral cavity is covered with painful small formations.
- Children of all ages suffer from bacterial stomatitis, which occurs due to thermal or mechanical trauma to the oral cavity, due to poor personal hygiene, and due to eating unwashed fruits. In very young children, bacterial stomatitis occurs when they put everything in their mouth while teething.
Causes
There are many reasons for this disease. Basically the very delicate mucous membrane of a child's mouth easily injured, as a result of which harmful bacteria begin their attack on the body. The baby's immune system is still very weak to resist them. In an adult, saliva perfectly protects the body from a variety of harmful microorganisms, but in small children it does not yet contain the required amount of enzymes that have antiseptic properties. Because of this, stomatitis occurs, causing inflammation of the mucous membrane in the oral cavity, manifested in the form of sores.
Thus, stomatitis in children occurs for three reasons:
- Due to traumatic damage to the oral mucosa.
- As a result of the harmful effects of various bacteria, herpes viruses, measles, and influenza. Often develops after the use of antibiotics.
- Due to allergies.
Symptoms of stomatitis in children there are the following:
- Increased body temperature, sometimes up to 40 degrees, if herpetic stomatitis. Weakness and malaise appear, the child begins to feel sick. The nose becomes stuffy, the mucous membrane begins to slowly swell and turn red.
- The entire mouth is covered with a white, gray or yellowish coating, blisters and erosions. It is important not to miss this moment and start treatment in a timely manner, otherwise stomatitis may progress to a more severe form.
- Unpleasant, sourish odor from the mouth.
- The baby begins to refuse food due to the painful process of swallowing.
- Salivation greatly increases.
- Often enlarges on the neck The lymph nodes.
As soon as the baby has it in his mouth white coating, it is necessary to urgently show him to the pediatrician. The disease progresses very quickly at an early age, and frequent severe complications. Only a doctor can determine from the symptoms what type of stomatitis a child has and prescribe the correct treatment.
How to treat stomatitis in children (general information)
 U different types stomatitis in children symptoms and treatment is also different. As soon as the doctor makes the correct diagnosis, treatment must begin immediately. Parents, if they suspect their child has this disease, should give him as much to drink as possible. Water irrigates the mucous membrane and promotes the removal of intoxication products from the body.
U different types stomatitis in children symptoms and treatment is also different. As soon as the doctor makes the correct diagnosis, treatment must begin immediately. Parents, if they suspect their child has this disease, should give him as much to drink as possible. Water irrigates the mucous membrane and promotes the removal of intoxication products from the body.
In addition to water, you can give your child fruit drinks, compotes, children's herbal teas. Sweet and sour are prohibited. It is strictly forbidden to give carbonated drinks and concentrated juices, which only begin to irritate the inflamed mucous membrane more strongly.
So what treatment does the baby need to make everything go quickly and less painful for him?
To start the mucous membrane should be anesthetized so that the child can eat normally. Products containing lidocaine or choline salicylate are mainly used.
Teething products, for example, Kamistad or Dentinox-gel, help well. It is best to use gels because they quickly penetrate the mucous membrane. Sprays with lidocaine cannot be used for children under one year old, because they provoke bronchospasm in them. After this, all ulcers must be treated with an anti-stomatitis agent.
If stomatitis is herpetic, then they help well antiviral ointments. For bacterial stomatitis, creams and solutions with antiseptics or antibiotics are suitable. Fungal stomatitis is treated with antifungicides.
For the speedy healing of cracks and ulcers, products that promote rapid tissue restoration help. These can be actovegin and solcoseryl gels, as well as vinylin balm.
The most important thing in the fight against this disease is compliance with the rules of oral hygiene. You should brush your teeth twice a day and rinse your mouth after eating.
A one-year-old child cannot yet carry out all these procedures on his own. It is necessary to wrap a piece of gauze around your finger and clean the baby’s mouth.
If stomatitis is allergic, use antihistamines, such as suprastin, fenistil, diphenhydramine.
 Viral stomatitis is effectively combated antiviral ointments with acyclovir, such as acic, virolex, herpevir. Viferon and oxolinic ointment are also used. If viral stomatitis recurs very often, it is necessary to strengthen the immune system with interferon, Immunal or Viferon in suppositories.
Viral stomatitis is effectively combated antiviral ointments with acyclovir, such as acic, virolex, herpevir. Viferon and oxolinic ointment are also used. If viral stomatitis recurs very often, it is necessary to strengthen the immune system with interferon, Immunal or Viferon in suppositories.
The most wonderful remedy for combating this type of stomatitis is considered Cholisal gel. It contains choline salicylate and cetalkonium chloride. This gel reduces inflammation, heat, relieves swelling, eliminates pain and destroys viral pathogens. For children under one year old, it can also be used as part of a complex treatment.
The gel is applied to a clean finger and rubbed into the oral mucosa with massaging movements 2-3 times a day.
Treatment of candidal stomatitis
Candidal stomatitis occurs due to a fungus, so treatment is carried out antifungal ointment. This could be candizol, candid, clotrimazole. In addition, doctors may prescribe rinsing with soda solution. It promotes the creation in the mouth alkaline environment, which has a detrimental effect on fungi and pathogenic flora. The use of soda is especially suitable for children under one year of age, because at this age many antifungal drugs prohibited.
To make the solution, you need to dilute a teaspoon of soda in a glass of warm water. A piece of bandage is wrapped around the finger, dipped into the solution and the child’s mouth is wiped. This way the treatment is carried out after each meal. Older children rinse their mouths on their own.
Treatment of aphthous stomatitis
With this type of disease, it is necessary to begin treatment of wounds and numb them as quickly as possible. For this they use water solution methylene blue, which is popularly called blue.
An aqueous solution should be used, because if you replace it with an alcohol solution, you can easily burn the delicate mucous membrane of the child’s mouth and cause poisoning. A cotton swab is moistened with the solution and the wounds are treated with it 5-6 times a day.
Treatment of traumatic stomatitis
A 2-year-old child often develops traumatic stomatitis. A companion to this disease is bacterial infection, therefore treatment occurs with the help wound healing and antiseptic agents.
Up to two years of age, children are prescribed Cholisal gel, solcoseryl, Actovegin, and the oral cavity is treated with a soda solution or chlorhexidine.
 Bacterial stomatitis cures well antiseptics, such as hexoral, tantum verde, orasept sprays, but they are contraindicated for children under one year of age. Medicinal lozenges can be used, but they are contraindicated in children under 6 years of age due to the possibility of asphyxia.
Bacterial stomatitis cures well antiseptics, such as hexoral, tantum verde, orasept sprays, but they are contraindicated for children under one year of age. Medicinal lozenges can be used, but they are contraindicated in children under 6 years of age due to the possibility of asphyxia.
It is best to use antiseptic gels with metronidazole and mouth rinses for treatment. Most popular antiseptic solution is miramistin, which effectively destroys microorganisms and promotes healing of the mucous membrane. It must be injected into the mouth three times and rinsed 4 times a day. For children under one year of age, the oral cavity is treated with Miramistin using a gauze swab.
Diet
While the wounds in the mouth are healing, food should be soft and as gentle as possible. It is best to give your child cooked pureed vegetables, omelettes, pureed soups, and cottage cheese.
Children who are over 6 months old should definitely add yogurt or unsweetened yogurt to their diet. It is extremely undesirable to give sweets, because sugar promotes the growth of fungi and bacteria, and this only aggravates the situation.
Prevention
To prevent stomatitis from occurring, you should observe the rules of hygiene. Young children should wash their hands frequently and avoid putting dirty objects in their mouth. Older children should be taught why they need to wash their hands and brush their teeth. The child needs to increase his immunity so that he gets sick as little as possible.
Examples of stomatitis in children










If Small child begins to be capricious, refuses to eat, body temperature rises to high levels, older children complain of pain in the mouth, and upon examination the mother discovers redness or ulcers on the cheeks, palate, tongue or the inside of the lip - this is stomatitis.
In children, the treatment of this disease depends on the causes that caused it, since there are several types of pathogens that provoke the development of inflammation in the oral cavity - common bacteria, the herpes virus, fungi of the genus Candida albicans, and stomatitis can also be toxic-allergic. So, how to treat stomatitis in a child? How to get rid of stomatitis in children as quickly as possible? We will talk about this in this article.
Childhood stomatitis - its classification and causes
An interesting fact is that a certain type of stomatitis is characteristic of a specific age of the child, however, of course, there are exceptions:
The reasons for the appearance of any type of stomatitis are that in children the mucous membrane of the oral cavity is so delicate and thin, injury to which occurs very easily, and the immune system is not yet able to cope with the mass of infectious agents that enter the mouths of “ubiquitous” children. Human saliva is an excellent defense for the oral cavity against the massive invasion of microbes, bacteria and viruses, but in young children it does not yet produce a sufficient amount of enzymes with antiseptic properties. Therefore, stomatitis occurs - inflammation of the mucous membrane in the mouth, which manifests itself either insignificantly - single ulcers, or creating extensive foci of inflammation.
Candidiasis, fungal stomatitis in children
Any stomatitis can occur in an acute form, mild degree severity or be chronic, recurrent, fungal stomatitis is no exception. Distinctive features fungal, candidal stomatitis or oral thrush:

Treatment of fungal stomatitis
Local procedures consist of creating a more alkaline environment in the oral cavity, since an acidic environment has a very beneficial effect on the progression of the process and promotes the proliferation of pathogenic bacteria, including fungus. Local treatment of fungal stomatitis in children is as follows:
- Treatment of the oral cavity 3-6 times a day with a soda solution - 2 teaspoons of soda for 1 glass of water, as well as special aniline dyes - “Blue”, 2% solution boric acid. For older children, these solutions can be used as mouth rinses.
- Treatment of affected areas with Clotrimazole, Nystatin ointments, Pimafucin cream. The bulk of fungal agents accumulate in the area of the teeth, so when processing, care should be taken Special attention gum and cheek areas.
- There is a special solution, gel, cream “Candide”, which contains Clotrimazole, which has a powerful antifungal effect. Treatment with this drug should be prescribed by a doctor, the course of which should not be interrupted or stopped prematurely, since fungi may develop drug resistance to this drug.
- For older children and adolescents, a doctor may prescribe antifungal agents in tablets or suspensions, such as Diflucan, Fluconazole.
- To strengthen the immune system during and after stomatitis, vitamin therapy is prescribed; Imudon absorbable tablets can be prescribed, which are indicated only for children over 3 years of age.
- During any stomatitis, a diet is required, with candidal stomatitis sour fruits and drinks, hard, coarse foods, too hot or cold are excluded, the amount of carbohydrate foods, spices, confectionery, and sweets in the diet is reduced.
- At high temperatures above 38C, of course, you should take.

Herpetic stomatitis in children
This is one of the most common forms of stomatitis in both children and adults. This is explained by the fact that 95% of the population sooner or later becomes infected with the herpes virus, but whether a herpes infection will develop in a particular child or adult directly depends on the person’s immune system.
The danger of the virus lies in the fact that it does not disappear from the body, but is either in a latent state, or with a weak immune response in the child, it becomes chronic with periods of remission and relapses.
Most often, herpetic stomatitis occurs in children from 1 to 3 years of age, since the antibodies received from the mother have already weakened and been eliminated from the body, and their own have not yet been developed.
Therefore, when encountering the herpes virus for the first time, a child often develops a violent reaction, the body actively fights the virus, which is manifested by high fever and symptoms of intoxication.
Again, we repeat, it all depends on the state of the child’s defenses; in some children, infection and development of herpetic stomatitis occurs in an acute form, while in others it does not cause high temperature and it goes quite easily. How to treat stomatitis in a child if it is caused by the herpes virus?
Distinctive features of herpetic stomatitis:
- Upon examination, first redness forms in the oral cavity, then vesicles appear, after the bubbles burst, the baby develops erosion, ulcers, and cracks in the oral mucosa. When the rash heals, the mucous membrane has a marbled pattern.
- The child also becomes capricious due to pain, burning, itching in the mouth, and his appetite decreases.
- In an acute process of moderate severity, the child exhibits all the symptoms of ARVI, the body temperature reaches 38C, and the lymph nodes become enlarged. When the rash begins, the temperature jumps to 39C and is not always brought down by antipyretic drugs; it may be accompanied by vomiting, nausea, headaches, and chills. In this condition, the number of bubbles is usually significant - 15-20 pieces; they can also be on the outside of the lips, on the wings of the nose or around the mouth, while the gums become inflamed and dry mouth appears.
- At mild form There are no more than 4-6 such stomatitis vesicles, the temperature rarely reaches 38C, it is easily reduced by antipyretics and the inflammatory process subsides quite quickly.
Treatment of herpetic stomatitis in children
In case of an acute process with severe symptoms, children are hospitalized, where they are provided with symptomatic therapy. For mild to moderate severity inflammatory process the child can undergo treatment on an outpatient basis. Just like with fungal stomatitis excluded from the diet sour foods, especially citrus fruits, canned food, salty and spicy foods. At herpes stomatitis in children, treatment includes local procedures and the use of general therapeutic agents:
- To provide an anti-inflammatory effect, it is best for children to treat the affected areas with decoctions. medicinal herbs 3-4 times a day - sage, chamomile, Kalanchoe juice, for this you should use cotton buds or cotton pads soaked in the broth. In pharmacies there are ready-made herbal mixtures, such as Ingafitol, Evcarom, which can also be used to treat ulcers or rinse the mouth in older children.
- For pain relief for children over 4 years old you can use the drug Stomatidin - an antiseptic for local application, which has an antimicrobial and mild analgesic effect on the mucous membrane in the mouth, as well as Hexoral Tabs - lozenges with Benzocaine and Chlorhexidine, they have a local analgesic and antimicrobial effect.
- Treating ulcers with propolis is very effective, for example Propolis spray, has a restorative effect on any skin damage, ulcers, herpes.
- The use of antiherpetic ointments is also indicated for local treatment, ointments used are Zovirax, Acyclovir, Oxolinic ointment, Viru-merz-serol (a highly effective drug for herpetic eruptions, used for initial clinical manifestations, when bubbles or vesicles form, use should be discontinued), tebrofen ointment.
- Bonafton ointment, an antiviral drug used to treat herpetic stomatitis, may be recommended.
- Promote the healing of wounds Karotolin - an oil solution with vitamin A, sea buckthorn oil (only natural, which also has an antiviral effect, and cosmetic pharmaceutical oil is an infusion of sea buckthorn on vegetable oil), And .
- , also known as Shostakovsky's balm, is able to cleanse wounds, also has an anti-inflammatory effect, accelerates the process of healing, epithelization and tissue regeneration.
- Lugol and Rotokan are used as antiseptics.
- At frequent relapses For herpetic stomatitis, the doctor can prescribe antiviral drugs orally, that is, in tablets, such as Valtrex, Acyclovir, etc.
- Vitamin therapy and absorbable Imudon tablets are also indicated, which should be taken 6-8 pieces per day for a week.
Until now, medicine cannot definitively name the reasons for the appearance of this type of stomatitis; some authors believe its occurrence is associated with disturbances in normal functioning gastrointestinal tract(for example,), others see the allergic origin in its occurrence (chocolate, strawberries, tomatoes, eggs), possible reason indicate injury to the mucous membrane or penetration of infection into the oral cavity, and clinical picture it resembles herpetic stomatitis.
Treatment in children aphthous stomatitis complicated precisely by the uncertainty of the causative agent of the disease. Most often it affects school-age children when they develop following symptoms stomatitis:

- At first, the ulcers resemble ulcers as with herpetic stomatitis, with the same characteristic redness, burning, itching, and a possible increase in temperature. However, then not blisters appear, but aphthae - these are painful white ulcers with bright redness around them, they are round in shape with clear, smooth edges.
- Then the aphthae becomes covered with a cloudy film, and if a secondary infection occurs after it breaks through, the inflammatory process worsens, the child may develop a fever, become drowsy, and refuse to eat.
Treatment of aphthous stomatitis in children
Treatment of this stomatitis, due to the uncertainty of the cause, is carried out by several doctors, this may be a dentist, an allergist or a gastroenterologist.
- If installed allergic nature occurrence of aphthous stomatitis, then contact with the allergen is excluded, antihistamines are prescribed - Suprastin, (children over 2 years old), see all.
- Solutions of soda, boric acid, herbal decoctions, and Blue are also used to treat canker sores.
- Antiseptic selection, antimicrobial agents It is often carried out by trial and error, since the course of any inflammatory process is individual, for some people Hexoral spray or Miramistin help, for others Vinilin or methylene blue dye - Blue helps a lot. Rotokan, an antiseptic with a healing effect (for mouth rinsing), has proven itself well.
- If gastrointestinal disorders are detected, then appropriate treatment of the concomitant disease is carried out.
- Vitamins C, B1, B2, B12 are prescribed.
- From antiviral drugs Bonafton may be prescribed.
- At chronic course stomatitis, to correct immunity, an immunologist can prescribe Decaris, Pyrogenal.
However, in any case, you should not self-medicate; treatment of stomatitis in children should be under the supervision of a qualified doctor.