Contrary to popular belief, stomatitis in children itself is not a complication of a childhood cold, although most often it occurs against the background. The second common misconception about this disease erroneously states that a pediatric dentist should treat stomatitis in a child. Both are wrong. Why stomatitis actually occurs in children, as well as who and how should treat it - let's figure it out!
Stomatitis causes children not only constant discomfort, but also severe aching pain.
View gallery 1 of 1
What is stomatitis and where to look for it in children?
Despite the fact that stomatitis in children often occurs as a consequence of acute respiratory viral infections, there is no direct connection between these diseases. The only thing is that while the child is sick with a cold, he Airways(including the oral cavity) dry out significantly. Saliva is almost not secreted, local immunity in the oral cavity is greatly weakened.
As a result, the mucous membranes of the mouth are left without the necessary protection, and when they are exposed to viruses or bacteria that are “unfriendly” to the body, inflammation occurs. It is precisely this inflammatory process on the mucous membranes of the mouth that is usually called “stomatitis”. Unfortunately, the development of stomatitis in children causes considerable pain to children.
Children often behave extremely restlessly, cry all the time, refuse to eat or drink, and cannot sleep peacefully. long time. In addition, even a mild inflammatory process in the oral cavity with stomatitis in children.
What kind of stomatitis does your child have: herpetic, aphthous or angular?
There are many options for stomatitis - there is no point in listing them all. It is enough for parents to know that in the vast majority of cases children encounter one of the three most common types of stomatitis - aphthous, herpetic and angular.
Aphthous stomatitis in children. Afta is special medical term, which usually hides a specific designation: “a small area of the mucous membrane on which there is damage.” Most often when aphthous stomatitis in children, foci of inflammation look like small round ulcers, covered with a yellowish or grayish coating and surrounded by a bright red rim.
Herpetic stomatitis in children. Herpetic stomatitis is contagious disease, which can affect a child at any age, but most often occurs in children 1-3 years old. Children in contact with each other (those who play with the same toys and often put them in their mouths, use the same utensils, etc.) easily transmit herpetic stomatitis each other. The causative agent of herpetic stomatitis is one of the variants of the herpes virus. Most other types of stomatitis (including aphthous) are not contagious and cannot be transmitted from one child to another.
Angular stomatitis in a child. This type of stomatitis is well known to everyone under a more “simple” everyday name - “jams”. IN medical reference books it is listed as “angular” stomatitis, and is manifested by severe irritation of the skin in the corners of the mouth. Over time, cracks appear there. Most often, angular stomatitis occurs due to an acute lack of iron in the body.
Causes of stomatitis in children
Stomatitis in a child's mouth can be caused by a number of factors. A child may bite the inner surface of his cheek in his sleep (or the baby simply has a jagged tooth) - and please, a place of irritation has appeared in the mouth. Stomatitis can also occur due to burns from hot food. Viral stomatitis in most cases occurs due to dryness of the mucous membranes of the oral cavity, against the background of which the pathological activity of viruses increases sharply.
The cause of herpetic stomatitis in children is the activity of the herpes virus of the first type (by the way, do not confuse stomatitis with genital herpes, which is caused by the activity of the herpes virus of the second type, as well as with any sexually transmitted diseases - there are no similarities here).
The exact causes of other types of aphthous stomatitis (not herpetic) have still not been established, although several main factors are under consideration. One of the factors is considered genetic predisposition to the development of ulcers, others – the connection of the disease with disorders in the immune system. In addition, stomatitis can be caused emotional stress; deficit nutrients, iron deficiency, lack of vitamin B12. Sometimes stomatitis occurs as a consequence food allergies or viral infection.
Stomatitis in a child’s mouth: symptoms
Basic (and common to most variants of the disease) symptoms of stomatitis in children are visible to the naked eye when examining the oral cavity. Ask the baby to open his mouth and slightly pull back the lower lip - most often this is where the aphthae-ulcers are located.
The size, lesions and color of the ulcers can vary greatly. For parents, any irregularity in the child’s mouth should be a signal of concern. In other words: normally, the oral mucosa is pink, moist, fairly smooth and the same in all areas. If somewhere you notice swelling, redness, a “pimple”, or even just irritation, etc. - this is already a reason to ask your treating pediatrician to examine the child’s mouth for stomatitis.
In addition to a visual examination of the child’s oral cavity, his behavior can also “hint” at stomatitis. Since the formation of ulcers causes real pain and discomfort in the baby, his behavior also changes dramatically - children become whiny and irritable, sleep poorly and refuse to eat.
In the case of herpetic stomatitis To these general symptoms, special ones will also be added:
- Aphthae appear in the mouth almost simultaneously - that is, in several places at once, of approximately the same size.
- The disease has a wave-like character: at first the mouth is covered with painful ulcers, which is accompanied by a sharp increase in temperature, then the disease seems to “freeze” (the child may become cheerful and stop complaining of pain; the temperature stabilizes), and after a few days a relapse occurs: new ulcers, an increase again temperature and painful sensations.
- The gums become swollen and it is observed.
TO characteristic symptoms aphthous stomatitis in children include:
- A day or two before aphthae (ulcers) appear and the temperature rises, small blisters appear on the tongue, which gradually begin to cause a burning sensation. Doctors usually call this symptom of aphthous stomatitis “geographic tongue.”
- Often, along with the blisters, a whitish coating appears on the tongue.
A characteristic whitish coating on the tongue is often a symptom of stomatitis in children.
The number of ulcers in the oral cavity with aphthous stomatitis is significantly less than with herpetic stomatitis - most often one or two, sometimes up to five or six. Whereas with herpetic stomatitis in children, the entire mouth may be “sprinkled” from the inside.
In addition, with any acute stomatitis (not only with aphthous, but also with herpetic and others), the lymph nodes under the lower jaw often enlarge and become painful.
How to treat stomatitis in children
Being a smart parent You should consult your doctor (pediatrician) if you find that:
- The child is unable to drink or swallow food.
- The child has a high temperature.
- The child is too fussy and cannot be calmed down.
- The child sleeps restlessly at night, or does not sleep at all.
- Bubbles and a light white coating appeared on the baby's tongue.
Treatment of stomatitis in children directly depends on the causes that caused it. The following treatment strategy is common to all types of stomatitis in children:
- A gentle diet with the exclusion of any solid foods that can “disturb” aphthae in the oral cavity and cause an exacerbation of inflammation. You should also remove spicy and sour foods from your diet, and make sure that the food is not too hot.
- Thorough oral hygiene: gentle brushing of teeth and tongue, as well as daily rinses with antiseptics.
- If a child's temperature rises above 38.5°C, he should be given an antipyretic medicine.
If you follow a gentle diet and proper oral hygiene, aphthae (ulcers) completely disappear 10-15 days after their appearance in any type of stomatitis.
To rinse your mouth during the day, you can use solutions of antiseptics - chlorhexidine, furatsilin, etc., as well as herbal decoctions - chamomile, calendula and others. The attending physician will tell you how to properly prepare the solution, and will also prescribe a rinsing regimen (it varies depending on the age of the child and the severity of his illness). In addition, if the ulcers are large and painful to the point that the child is acting too hysterically, the canker sores can be treated with antiseptic sprays from time to time.
However, remember that for stomatitis in children, aerosols should under no circumstances be used on children under one year of age. Pharmacy gels, which are usually used to relieve itching, will help these crumbs relieve pain.
Pediatric stomatitis can be aggravated by sharp edges of teeth or braces in the mouth - these problems are best addressed in the pediatric dentist's office.
Additional measures for the treatment of stomatitis in children
Besides common methods Therapy against stomatitis in children, of course, there are special treatment measures that correspond to each specific type of this disease. For example:
- If the diagnosis sounds like “herpetic stomatitis in a child,” the doctor will definitely prescribe a drug that suppresses the activity of the herpes virus (the main active substance which is acyclovir).
- If the stomatitis is angular (jams), then the child will probably be prescribed medications.
What parents always miss: alas, iron deficiency in the body cannot be replenished with food - it will take too long (not even a year). Iron-containing foods - beans, apples, meat or nuts - all of them can only maintain the level of iron that is already in the body. Only special medications can raise iron levels.
- If aphthous stomatitis in a child’s mouth does not go away for more than 15 days, immediately consult a doctor again.
Alas, there is no special prevention against stomatitis in children - the cause may be a banal injury to the oral mucosa caused by a hard piece of food or a children's toy. However, if the baby has a strong, stable immune system, the chances that the disease will develop are significantly less.
Stomatitis in a child is an inflammatory process in the oral mucosa caused by for various reasons. Almost all children suffer from this common disease. But the youngest are the most vulnerable to the disease due to the underdevelopment of the immune system and the inability to maintain personal hygiene. Let's look at how to quickly cure stomatitis in a child, as well as how to prevent infection.
The disease is an immune response to irritation caused by various pathogens. In young children, the mucous membranes are delicate, and protective system the body has not yet formed. There are not enough antibodies in saliva that can suppress the development of infection. In addition, babies tend to try everything by heart, which increases the risk of infection.
There are also additional reasons occurrence of the disease. These include insufficient hygiene oral cavity, injury or burn, as well as chronic diseases of the stomach and intestines.
All parents are concerned about whether stomatitis is contagious? Infectious stomatitis, that is, bacterial and especially viral - yes! How is stomatitis of these varieties transmitted? Children can catch the infection through dirty hands and household items. Stomatitis is also transmitted from child to child. And the closer the contact, the greater the risk of infection. Very often, stomatitis is “gifted” to the baby by kind relatives when they cuddle and kiss their dear little one. Moreover, adults themselves may not show signs of the disease - the immune system copes with pathogens. But this does not mean that they are not carriers of pathogenic bacteria and viruses.
Diagnosis of the disease
 This disease is characterized by the appearance of painful ulcers in the baby’s mouth. But there is also additional signs stomatitis in a child:
This disease is characterized by the appearance of painful ulcers in the baby’s mouth. But there is also additional signs stomatitis in a child:
- Swelling of the mucous membrane;
- Whitish or icteric coating;
- Excessive salivation or, conversely, dry mouth;
- Poor appetite;
- Smell from the mouth;
- Enlarged lymph nodes.
Sometimes the temperature rises with stomatitis in a child, and the gums bleed. Such symptoms are especially characteristic of stomatitis in a child under 1 year of age.
Only a doctor can accurately diagnose the disease. If signs of illness appear, you should go to pediatric dentist or a pediatrician.
Having confirmed the diagnosis, the doctor will suggest a therapeutic course. Self-medication is not recommended, because there are many varieties of this disease. Each case requires individual selection of pharmaceuticals depending on the pathogen and the age of the child.
Types of stomatitis and methods of treatment
Infectious agents causing inflammation, differ. In this regard, doctors identify several types of the disease.
Candidal stomatitis in children

Photo of candidal stomatitis in an infant
The detailed form of the disease is caused by intensive proliferation of the Candida fungus. These microorganisms are always present in the mouth, but in small quantities. When immunity decreases, the microflora becomes more active and provokes inflammation. This type of disease is also called fungal stomatitis or thrush. It is characterized by:
- Whitish coating on the mucous membrane;
- Small bleeding wounds;
- A sharp rise in temperature;
- Dry mouth;
- Swelling of the lymph nodes.
To get rid of the disease, you need to create in your mouth alkaline environment. Candida can't stand her. To do this, you need to treat the wounds in the child’s mouth using a gauze swab moistened with sodium tetraborate. Carefully remove plaque. The same product can be used to treat a baby's pacifier. Treatment of fungal stomatitis in children over 5 years of age is permitted with the pharmaceutical drug Fluconazole.
Bacterial stomatitis in children
It is classified as a so-called “disease of dirty hands,” although it can also be contracted from another person. The risk of infection increases with wounds and cracks in the mouth of children. Multiplying bacteria form a yellowish coating that smells unpleasant. As the disease develops, blisters filled with pus and crusts form on the lips.

Photo bacterial stomatitis The child has
At bacterial infections The attending physician usually prescribes antibiotics that are appropriate for the child’s age, for example, “,” Metrogyl Denta.” Older children additionally use rinses (Tantum Verde, Chlorophyllipt). Stomatitis in newborns is treated with antiseptic irrigation.
Aphthous stomatitis in children

Photo of aphthous stomatitis in a child
Aphthous (ulcerative) stomatitis in the mouth is a disease that manifests itself against the background of other ailments: both the oral cavity and digestive system. Doctors cannot say with certainty what exactly causes this type of disease. Presumably in children the causes of this form of the disease are as follows:
- severe allergies;
- infection with staphylococci;
- problems with the digestive system and immunity.
With this disease, the temperature always rises, and characteristic ulcers with a clear scarlet rim appear in the mouth - aphthae. Aphthous stomatitis in a child can be easily identified using a photo by looking at the appropriate medical forum.
To get rid of a disease, you need to identify the cause and eliminate it. You can speed up the healing of ulcers if you smear the stomatitis with wound-healing and antiseptic agents, for example, Vinilin or Cholisal.
Viral stomatitis in children
This form of the disease is caused different types viral agents, it is the most contagious. Viruses are easily transmitted from a sick person to a healthy person.
One of the most common pathogens is the herpes virus.

Photo of herpetic stomatitis in a child

Swelling of the mucous membrane with herpetic stomatitis in a child
It is characterized by high fever, dry mouth, and nausea. Ulcers are located not only in the mouth, but can also appear. Sometimes gum swelling or inflammation occurs - gingivitis.
If the symptoms of viral stomatitis in children are confirmed, treatment is carried out locally antiseptic solutions, for example "Miromistin". Antiviral medications will also be required. For this type of stomatitis in young children, Viferon is suitable.
Traumatic stomatitis in children
It often appears when the first teeth erupt or when the mucous membrane is burned by hot or cold food. It can occur if the baby bites his tongue or injures his mouth with the sharp edges of a toy. This type of stomatitis usually occurs on the gum or tongue. Red, inflamed areas form there. The gums swell, and if stomatitis occurs on the child’s tongue, then it is difficult for the baby not only to eat, but also to speak.
How to treat such a disease? With the help of antiseptic and regenerating pharmaceuticals. This could be Solcoseryl, Chlorhexidine, sea buckthorn oil. If necessary, a course of antibiotic medications is prescribed.
Allergic stomatitis in children
Under the influence of allergens, the mucous membrane swells, redness and inflamed areas appear. In addition to local antiseptics, it is important to choose the right one antihistamine. It could be Parlazin or Suprastin.
At the same time, the child needs to choose a hypoallergenic menu and avoid contact with substances that can cause a painful reaction in the body.
Chronic stomatitis in children
At chronic disease necessary additional tests and consultations with specialists. For laboratory tests A scraping is taken from the oral mucosa and a blood test.
In case of chronic candidal stomatitis, it is necessary to conduct a blood test for glucose levels and a visit to a gastroenterologist.
For chronic aphthous stomatitis, it is necessary to visit a gastroenterologist, allergist and immunologist. In addition, you may need:
- Examination of stool for oviworm;
- Dysbacteriosis test;
- Ultrasound of the abdominal organs.
How long does stomatitis last?
According to medical statistics At one age or another, the risk of developing a certain type of stomatitis increases:
Stomatitis in children under one year of age is usually fungal in nature.
- A child aged 2 years and older develops herpetic and aphthous forms of stomatitis.
- Schoolchildren often have stomatitis of the allergic or aphthous type.
- Other forms of the disease may occur in children of different ages: like infant, and so does a teenager.
The regeneration process is quite slow. The body needs time to get rid of the irritant and recover. The speed of recovery depends on both the age and the general health of the child.
If we talk about how long they last external manifestations illness, then we can assume a certain time range. Symptoms of the herpes form of the disease last for about two weeks. How long fungal stomatitis is treated in children depends on the immune system. Time frames vary from a week to a month. Aphthous, traumatic and bacterial can go away in 10–15 days. Allergy symptoms can disappear even faster if the baby does not come into contact with the reagent.
Medicines suitable for all types of illness
 How to treat stomatitis in children: for each type of disease, remedies must be selected individually. Firstly, the causative agents of the disease vary greatly: antibiotics will not help against a viral disease. Secondly, pharmaceuticals for infants may not be suitable for stomatitis in a child 3 years of age or older. Thirdly, the location of the affected areas should be taken into account. So, stomatitis in a child’s throat is treated with a spray or gargle - gel cannot lubricate sores in the throat. If it is necessary to treat stomatitis on a child’s tongue, the pharmaceutical product must be gentle, pleasant to the taste and viscous so that it holds and does not roll off.
How to treat stomatitis in children: for each type of disease, remedies must be selected individually. Firstly, the causative agents of the disease vary greatly: antibiotics will not help against a viral disease. Secondly, pharmaceuticals for infants may not be suitable for stomatitis in a child 3 years of age or older. Thirdly, the location of the affected areas should be taken into account. So, stomatitis in a child’s throat is treated with a spray or gargle - gel cannot lubricate sores in the throat. If it is necessary to treat stomatitis on a child’s tongue, the pharmaceutical product must be gentle, pleasant to the taste and viscous so that it holds and does not roll off.
Drug therapy
Treatment of stomatitis with pharmaceuticals has analgesic, regenerative and anti-inflammatory effects.
What remedies are suitable for all types of stomatitis in children:
| Medications | Name | Application | |
| To relieve pain, inflammation, reduce fever | Taken orally | "Ibuprofen" | 10 mg per 1 kg of weight three times a day for no longer than five days. From three months. |
| "Paracetamol" | 15 mg per kg three times a day. Up to two years - rectal suppositories or syrup. | ||
| Local impact | "Holisal" | Apply to damaged areas three to four times a day. From nine months. | |
| "Kamistad" | Three to four times a day. | ||
| "Kalgel" | Six times a day. | ||
| Antiseptics | Sprays | "Hexoral" | Used after meals, effective for up to twelve hours. Apply twice a day |
| "Inhalipt" | Three to four times a day. | ||
| "Chlorophyllipt" | Two or three times a day. | ||
| Iodine-containing compounds | "Lugol" | Treat inflamed areas two to three times a day. | |
| "Iodinol" | Use to lubricate ulcers and rinse in the form of an aqueous solution (1:10) two to three times a day. From one and a half years. | ||
| Pharmaceutical rinses | "Stomatidin" | Two to three times a day with an interval of at least four hours. | |
| "Miramistin" | Two to three times a day. | ||
| "Chlorhexidine" | |||
| You need to dissolve half a tablet in a glass of warm water. Rinse your mouth three to four times a day or apply to sore areas. | |||
| "Stomatofit" | 10 ml of solution must be mixed with 70 ml of water. Rinse your mouth three to four times a day. | ||
| Gel for various stomatitis for children | "Metrogil denta" | Apply to inflamed areas three times a day. | |
When the ulcers begin to heal, vitamin complexes can be used to improve regeneration.
Parents often have a question: why do I smear the baby’s affected areas, but the inflammation does not go away? The remedy is probably not suitable for treating this type of stomatitis. Before applying gel or balm, you should consult your doctor. But what to do before visiting the clinic? First aid for stomatitis in a child consists of antiseptic rinses. How to rinse your mouth for stomatitis? Compositions from the table or infusions are suitable medicinal plants: oak bark, calendula, sage, chamomile.
Treatment with traditional methods
 For stomatitis in children, the compositions will additionally help traditional medicine. But you should talk to your doctor first. In addition, you should not use home recipes to cure stomatitis in one year old child. Traditional methods are suitable for curing illness in children 2 years of age and older.
For stomatitis in children, the compositions will additionally help traditional medicine. But you should talk to your doctor first. In addition, you should not use home recipes to cure stomatitis in one year old child. Traditional methods are suitable for curing illness in children 2 years of age and older.
What compositions will be useful:
Chamomile with honey
One large spoon of herb is brewed in 250 ml of boiling water and mixed with two teaspoons of honey. Rinse with warm solution oral cavity three times a day.
Aloe on honey
The leaves are ground into puree and mixed with honey in equal proportions. Apply the balm to sore spots three times a day. It also helps with bleeding gums and if the gums are swollen.
Soda and salt
The components are taken in equal parts and dissolved in cool water (a small spoon of the composition per 250 ml). Rinse your mouth 4-5 times a day
No less important proper care for sick children and nutrition for stomatitis. What to feed a child with stomatitis? The diet should not contain spicy, sour and spicy, as well as excessively hot and cold foods. At sharp pain better to give liquid food and first numb the oral cavity with an anesthetic pharmaceutical. Stomatitis in infants involves treating nipples, feeding bottles and mother's breasts.
Warning! Sometimes, after looking at a forum with homemade tips, moms and dads mindlessly copy recipes. But they can be dangerous. So, children should not wipe sores with brilliant green, blue, fucorcin and borax in glycerin. This will only worsen the baby's condition.
Prevention of stomatitis in children is primarily aimed at oral hygiene. It is important to teach your baby to use a toothbrush and visit the dentist regularly. It is also important to disinfect your baby's toys, especially those with which he walks outside.
Remember that only a doctor can make a correct diagnosis; do not self-medicate without consultation and diagnosis. qualified doctor. Be healthy!
Stomatitis means inflammatory diseases oral mucosa. Stomatitis in a child is one of the most common in pediatric dentistry; a child can also suffer from it school age, and an infant. Newborn babies whose immunity is not yet stable are especially susceptible to infection with stomatitis. How to treat stomatitis in children and what types of disease there are, we will consider in this article.
It is easy to identify stomatitis in a child. The baby feels weak, his body temperature rises, often very strongly, he becomes capricious at the dinner table and refuses to eat. The child, if he can already speak, complains that his mouth or tongue hurts. In this case, parents need to examine their child’s oral cavity. If on inside If reddish or whitish spots or ulcers are visible on the cheeks and lips, palate or tip of the tongue, then the child has developed stomatitis.
What types of stomatitis can be observed in children?
In small children, the oral mucosa is still thin and delicate; a child can accidentally injure or bite through it. An infection gets into the wound, pathogenic viruses and bacteria rush in, causing inflammation. Reliable protection saliva fights infection, but in children it does not have such pronounced antimicrobial properties as in adults. Most often, stomatitis in children is caused by:
- influenza viruses, rubella, herpes, chickenpox;
- bacteria staphylococci and streptococci;
- fungal microorganisms;
- caries and plaque;
- immunity deficiency, anemia, hypovitaminosis;
- diabetes mellitus, allergies, dehydration;
- long-term use of antibiotics and other potent drugs;
- poor oral hygiene;
- wearing braces to correct the bite.
It is difficult to keep track of children of any age, so they can become infected with stomatitis completely unexpectedly. Teething babies put toys and any objects in their mouths into their mouths. Older children are lazy to brush their teeth or do it incorrectly, and forget to wash fruits and vegetables before eating. Schoolchildren eat on the go, consume low-quality and harmful products, from which people often suffer from allergies, do not wash their hands before lunch. Depending on the specific pathogen, doctors distinguish between types of stomatitis in children:
- allergic, occurring as a side process of an allergic reaction;
- herpetic, it manifests itself when infected with the herpes virus;
- aphthous, or advanced herpetic, which has taken a chronic form;
- viral, caused by a viral infection entering the body;
- catarrhal, caused by pathogenic microorganisms due to poor hygiene;
- bacterial, caused by pathogenic bacteria;
- candidiasis, which manifests itself when the oral cavity is colonized by fungal microorganisms;
- vesicular, occurring after contact with an infected insect or animal;
- traumatic, caused by injuries and burns of the oral mucosa.
Children of different ages experience certain types of stomatitis. Stomatitis in infants is most often caused by bacteria or an acquired herpes virus. Pathogenic microorganisms reach the baby through an unwashed pacifier or fingers, which the baby likes to put in his mouth.
One-year-old children often develop prolonged candidiasis and herpetic stomatitis. Children from three to six years old usually suffer from herpetic and aphthous forms of the disease. And school-age children often become infected with allergic stomatitis.
However, children of any age are most susceptible to bacterial, herpetic and aphthous stomatitis.
How does fungal stomatitis manifest in children?

Fungal, or candidal stomatitis in children is also called oral thrush, since general symptoms these ailments are very similar. A sick child first experiences a feeling of dryness and burning in the mouth, and the mucous membrane is very itchy. Then a whitish, cheesy coating appears on the inside of the lips, cheeks, tongue or gums, which is easily scraped off. The tissue under this plaque becomes inflamed and bleeds. The baby suffers from pain inside the mouth, but there is no increase in body temperature or enlargement of the lymph nodes. Fungal stomatitis in children is caused mainly by a pathogenic fungus of the genus Candida.
How to treat fungal stomatitis in a child?
The fungus actively multiplies in acidic conditions, so a child suffering from candidal stomatitis needs to create an alkaline environment in the oral cavity. You should exclude sweets, baked goods, and spices from the menu; it is not advisable to eat too hot and sour foods; you should pay attention to dental and oral hygiene. Ordinary soda reduces acidity well:
- two spoons of the product are dissolved in a glass of warm water,
- the solution is used to rinse the oral mucosa infected with fungus.
Young children are usually prescribed antifungal ointments "Clotrimazole" or "Pimafucin". Treatment of fungal stomatitis in older children is carried out using Diflucan or Fluconazole capsules. It is important not to interrupt the course of taking the medication, since pathogenic microorganisms tend to adapt to the effects of the drug. The immune system of a child who has had stomatitis needs to be strengthened, so the baby must take a complex of vitamins.
How to determine bacterial stomatitis in children?

Bacterial stomatitis in children initially manifests itself in the same way as intoxication due to poisoning. The child's body temperature rises, he is weak and drowsy, does not want to eat, and complains of pain in the head and limbs. Then the gums become inflamed, and when pressure is applied to them, they bleed and hurt. It becomes unpleasant for the baby to chew foods containing sour juice:
- fresh berries and fruits, especially citrus fruits,
- pickled vegetables,
- dishes with hot sauce.
The mucous membrane of the oral cavity is covered with round, yellowish, clearly defined ulcers. They burn, itch, and ooze putrid smell. Bacterial stomatitis in children is caused mainly by staphylococci and streptococci. If stomatitis in a child is not treated in time, bacteria can multiply so much that they cause tonsillitis - inflammation of the tonsils.
How to treat bacterial stomatitis in a child?
The easiest way to cure bacterial stomatitis in a child is with a soda solution. The baby will have to rinse the mouth after every meal. If the child is large, he can easily cope with this task on his own; an infant can be sprayed soda solution into the mouth using a container with a spray bottle. Excellent destruction harmful microorganisms potassium permanganate and hydrogen peroxide. From pharmaceuticals Furacilin, Tavegil, and Suprastin have proven themselves against bacterial stomatitis.
In order for the treatment of stomatitis in a child to be effective, you need to monitor oral hygiene. There should be no leftover food left between the teeth after eating - this is the most favorable environment for the growth of bacteria. Doctors recommend that if the baby has stomatitis, replace it for a while toothpaste ordinary laundry soap. It not only removes plaque well, but also restores the alkaline balance in the oral cavity. To relieve pain caused by the development of ulcers, you can treat the infected mucosa with Cholisal gel or Solcoseryl paste.
How to detect herpetic stomatitis in children?

Herpetic stomatitis is most common in infants. Stomatitis first appears in an infant infected with herpes through contact with the mother. Mother and relatives love to kiss the child, lick his spoon with the remains of half-eaten food or a dirty pacifier, thereby inadvertently transmitting the infection. Most often, the disease occurs in children aged six months to three years; at this age, their immune system does not yet have time to produce antibodies against herpes in sufficient quantities. The herpes virus remains in the body forever and makes itself felt when a person’s immunity decreases for some reason.
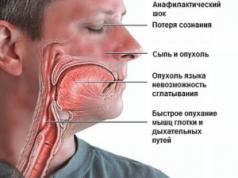
How strongly the herpes virus will manifest itself depends on the child’s immune strength. In some children, the disease is almost asymptomatic, while others suffer from many complications, such as:
- pain in muscles and head
- weakness
- with severe intoxication, the temperature rises to 38°C
- chills and nausea
- swelling of the cervical lymph nodes
The oral mucosa becomes inflamed and swollen, takes on a rich red color, and small transparent blisters appear on the tongue, inside the lips and cheeks. After a few days, these bubbles become covered with a yellowish coating and then burst. At the same time, the child feels a strong burning sensation. In place of the burst blisters, ulcers and cracks remain, which heal slowly.
How to treat herpetic stomatitis in a child?
Herpetic stomatitis is caused by a virus, however, treat herpetic stomatitis in a child with the usual antiviral ointments and creams used on skin, forbidden. Suitable for the inside of the mouth only rectal suppositories, tablets or special gels and pastes that are safe for mucosal tissues. Usually, doctors prescribe Viferon or Acyclovir suppositories or gel for herpetic stomatitis. These products should be applied directly to the blisters before they burst.
To relieve inflammation of the mucous membrane, the mouth is rinsed with infusions medicinal herbs. Chamomile and sage work well for this purpose. For small children who do not yet know how to rinse their teeth, their mouths are irrigated with a spray bottle or lubricated with a cotton swab with Miramistin solution, which not only relieves tissue swelling, but also suppresses the activity of the virus. To relieve pain and burning, the drug “Stomatidin” is applied to the infected areas. You can also give your child a Hexoral tablet to swallow.
Wounds from burst blisters should be treated with a propolis-based solution so that they heal faster. sea buckthorn oil or rosehip oil, Vinilin balm.
To boost immunity, it is advisable to give your baby a vitamin or immune complex to drink. Doctors usually prescribe Imudon or Immunal for children.
How to recognize aphthous stomatitis in children?

Aphthous stomatitis in children is actually a complex, advanced form viral disease. The child experiences weakness, suffers from high fever and lack of appetite, everything in his mouth becomes inflamed and burns. Only instead of small blisters, the oral mucosa is dotted with large painful ulcers - aphthae. At first these ulcers are whitish in color and have a red border, then they become covered with a cloudy coating and finally burst. They leave quite noticeable wounds that can become infected. Therefore, treatment of aphthous stomatitis should be accompanied by careful oral hygiene.
How to treat aphthous stomatitis in a child?
Treatment of aphthous stomatitis in children is the most difficult, not only because ulcers are difficult to heal, but also because the cause of their occurrence can be very different. Most often, aphthous stomatitis in a child is caused by the herpes virus, but the cause of the disease can be allergies and food poisoning. Therefore, treatment of aphthous stomatitis is carried out by doctors of various specializations: an allergist, a gastroenterologist or a dentist.
From the diet of a sick child, it is necessary to exclude sour and spicy foods, foods that can cause an allergic reaction:
- fruits
- berries
- nuts
- sweets
- spices
If the disease manifests itself as a result of poisoning or disruption of the digestive system, the baby’s diseased organ is first cured, and then he is prescribed vitamin complex containing ascorbic acid and B vitamins. If stomatitis in a child is caused by allergies, he needs, first of all, to take an antiallergic drug. Doctors usually prescribe it for children
- "Tavegil"
- "Suprastin"
- "Cetrin".
- If the cause of stomatitis is a virus, doctors prescribe the child an antiviral drug, usually Miramistin irrigation solution or Bonafton ointment.
To relieve inflammation of the mucous membrane, you can rinse your mouth with the antiseptic drug "Rotokan", as well as just a solution of soda or boric acid, lubricate the cavity with Cholisal gel. Hexoral and Vinilin relieve swelling and pain well. When the ulcers begin to gradually heal, the doctor prescribes a remedy for the baby to restore mucosal tissue, usually Solcoseryl gel. To strengthen the immune system, the child needs to take a vitamin or immune complex.
An article about how to treat stomatitis in infants, we want to start with a warning. Many young parents rely more on their grandmother's and mother's advice, which, they say, has always helped - and will help now. We don’t argue - folk remedies are effective and often with their help you can easily get rid of inflammation in the baby’s mouth, including thrush, which occurs in mild form.
Treatment of stomatitis
Many doctors recommend rinsing with chamomile, but this must be done very carefully, placing the baby on his side so that he does not choke. Although most traditional methods- rinsing with decoctions of sage, St. John's wort, cabbage juice, etc., are not very suitable for a newborn who, in addition to mother's milk, does not even receive complementary foods. In addition, some methods are categorically unacceptable for children, for example, in no case should you burn sores with brilliant green or peroxide. Firstly, it is very painful (try it for yourself), and, secondly, burns are obtained on the delicate mucous membrane of the baby, which are very difficult to heal.
We also consider it contraindicated to lubricate erosions with honey, because a sweet nutrient medium, on the contrary, promotes even greater development of bacteria and fungi. Moreover, there is no need to shove a mixture of yogurt with garlic or aloe juice into your baby’s mouth. Self-treatment may lead to the opposite results - the disease will develop and enter a difficult-to-treat stage. Parents often ask the question: which doctor treats stomatitis? Thrush and other mild stomatitis are treated by pediatricians, with more complex cases You should contact your pediatric dentist.
How to treat stomatitis in children under one year of age?
In general, the treatment of stomatitis, like all other diseases of the mouth, is the prerogative of dentists. After all, treatment depends on the type of stomatitis and the causes of its occurrence. And only a doctor can assess the severity of the disease and the necessary list of medications and manipulations. To carry out treatment, the child should be isolated from other children, since stomatitis is a contagious disease. You should strictly adhere to cleanliness, feed the baby only warm and liquid food, and give plenty of unsweetened drinks. Before feeding, you should wash your breasts well with warm water (without soap or alcohol solutions!). Treatment of stomatitis in infants and older children has a number of differences, because you cannot force a baby to rinse his mouth, he will not talk about his feelings. When the baby has eaten, you need to put him on his side and rinse his mouth with a special irrigation bottle, pouring the solution (chamomile, pimafucin) behind his cheek and collecting it with a diaper. After this, the mouth is lubricated with special ointments, which are prescribed by the doctor depending on the type of stomatitis - antifungal, antiviral or, in the case of traumatic stomatitis, a solution of vitamin A in oil or Shostakovsky balm.
To treat thrush, a Candide solution is used, which destroys the fungus. The duration of use of the drug is strictly 10 days; treatment cannot be stopped, even if there is no longer visible thrush, since the fungus may not be completely eliminated, and if it returns, it will be resistant to the drug and difficult to cure. For candidiasis, it is also recommended to lubricate the mouth with a solution of soda (or boric acid) to change the pH, which kills the fungus. Under no circumstances should you use drugs prescribed for older children for infants! Dosages for children are completely different, in addition, there may be intoxication of the body, because the functions of the liver and kidneys are still in their infancy. For infants Also, lubrication with aniline dyes (methylene blue) is not used. The doctor may prescribe lubrication of the mucous membrane with 1% clotrimazole or 5% nystatin ointment.
How to treat viral stomatitis?
How to treat stomatitis in infants, if he has viral origin? Herpetic stomatitis in infants requires a more responsible attitude. At acute course illnesses - treatment only in a hospital. The main reason is acute viral stomatitis occurs against the background sharp increase temperatures up to 40°, which often causes convulsions and can cause respiratory arrest.
In case of a mild form of herpes (and aphthous stomatitis, which is more rare in infants), a course of acyclovir (in the form of an ointment), vitamins and immunostimulants is given, but only on an individual prescription from a doctor. In addition to antiseptic rinses using chamomile decoctions, for children over 8 months old, you can use a decoction of sage, pimafucin, keratoplasty is also prescribed - substances that actively restore damaged oral mucosa - vitamin A, sea buckthorn or rosehip oil, Vinylin ointment. If a child refuses food, there are options to relieve pain, for example, with gels for anesthetizing teething - Kamistad, Kalgel and Baby Doctor. The latter does not contain icecaine, which allows it to be used for children with allergies.
An infant, and even children under 3 years old, are very vulnerable creatures. It is better not to self-medicate, but to trust experienced doctors. Dentists children's center“Utkinzub” have extensive practical experience in treating the youngest patients for all types of stomatitis - contact us at the first suspicion. And also carefully read the article “Prevention of stomatitis in children under 1 year of age” - and you will not need to treat stomatitis in your baby.
Stomatitis in children is a concept that unites a group of diseases accompanied by inflammation of the oral mucosa. This is the most common diagnosis in pediatric dentistry, occurring even in newborns and children under 1 year of age.
Ulcers that appear in the mouth often cause unpleasant taste sensations, and as a result, children often refuse food. But with the development of stomatitis, not only difficulties with eating arise, sometimes they increase The lymph nodes, the child may experience elevated temperature or general lethargy and deterioration in health.
Relevance of the problem in childhood due to the high prevalence and contagiousness of the disease. As a result of imperfect local and general immunity, infants and children of early and preschool age are most vulnerable to stomatitis.
What is stomatitis
Stomatitis – common name various inflammatory processes on the mucous membrane of the child’s mouth. According to statistics, children from one to five years old suffer from stomatitis. Children under one year of age are still quite well protected by antibodies obtained from breast milk and rarely encounter stomatitis; children over five can already boast of their own developed immunity.
Disease provoked by two main conditions:
- Low immune protection the child's body.
- Features of the structure of the mucosa.
The mucous membrane in children is very thin and easily injured. The resulting cracks often become infected, since the saliva of a child, especially under the age of one year, does not yet have the same bactericidal properties as the saliva of an adult. So, during inflammation, stomatitis forms.
Symptoms of stomatitis in children
With stomatitis in children, the main symptom of the disease is damage to the oral mucosa in the form of a light gray coating that can develop into erosions and aphthae (ulcers).
Depending on the location of the lesion and the degree of spread of the disease, several types of stomatitis are distinguished:
- is the most common type of disease that can occur in both children and adults. With this type of disease, active irritation of the mucous membrane in the mouth is observed, which gradually turns into small bubbles with liquid. Acute form accompanied by high temperature, which is difficult to bring down with antipyretic drugs, dizziness, nausea, chills and others may occur.
- . Caused by a fungus of the genus Candida. This type of stomatitis mainly affects children under one year of age due to breastfeeding. Milk is a breeding ground for fungal growth. Therefore, this stomatitis is also called “thrush”. It is characterized by the appearance of persistent white plaque in the baby's mouth. Do not confuse this with normal plaque after feeding.
- Aphthous stomatitis in children it manifests itself on the oral mucosa in the form of aphthae measuring from 5 to 10 mm on the inner sides of the lips and cheeks, the outer and inner sides of the tongue. Unlike herpes stomatitis, with aphthous stomatitis, only one ulcer forms in the oral cavity, in rare cases - two or three.
- Allergic stomatitis manifests itself in the form of redness of the gums and tongue. Subsequently, microbial flora can join and cause bacterial, fungal or viral stomatitis. The temperature may be normal or it may rise. If pathogenic flora has not joined, then such stomatitis is not contagious.
- Bacterial stomatitis. This type of disease is typical for children of different ages and occurs due to mechanical or thermal trauma to the oral cavity, as well as violation of personal hygiene rules, during teething in babies, etc.
How to treat stomatitis in children directly depends on the type of pathogen that caused the inflammation. Most often, the disease develops against the background of a general decrease in the child’s immunity. Sometimes the cause of stomatitis in children, especially small ones, is a simple injury to the oral cavity, because children constantly pull different objects into their mouths.
Stomatitis in children: photo
What does stomatitis look like in children's mouths? The photo shows the initial and other stages.
Click to view

[collapse]
Aphthous stomatitis
Clinically, the ulcers resemble those of herpetic stomatitis. But there are also differences: aphtha is a round or oval-shaped erosion with smooth edges and a smooth bottom, the bottom of the aphtha is painted bright red. The main location of such ulcers is on the mucous membrane of the lips and cheeks.
As the disease progresses, the aphtha changes and becomes covered with a cloudy film. After the film breaks through, a secondary infection may occur, which can complicate the course of the disease. At the same time, the child’s condition changes, drowsiness, whims, lack of appetite, and often refusal to eat appear. Body temperature rarely rises, but can stay within 38º.
View photos

[collapse]
This type of stomatitis is provoked by yeast-like fungi of the genus Candida, which enter the child’s body through household items, birth canal. Fungi multiply under favorable conditions (trauma to the mucous membrane, taking antibiotics) and cause disease.
Typically, candidal stomatitis at the first stage is not accompanied by obvious symptoms. The child experiences dry mouth, mild itching and burning. Infants under 12 months may latch on to the breast more often to compensate for the feeling of dry mouth, while older children, from 2–3 years old, on the contrary, refuse to eat.
Children aged 5–6 years complain about bad taste and bad breath. During an external examination of the oral cavity, you can notice a grayish or yellowish coating on the mucous membrane. It bears some resemblance to drops of sour milk or cottage cheese.
As the condition worsens, the mucous membrane quickly becomes increasingly covered with a white coating, but if the form is advanced, the mucous membrane is almost completely covered with such a coating, and “jams” form in the corners of the mouth.
View photos

[collapse]
Herpes stomatitis in children appears when infected with the herpes simplex virus. The source of infection is both children and adults who develop herpes on the lips and nose. The virus is transmitted immediately to the mucous membrane of a child’s mouth, especially a newborn, which is vulnerable to any disease. The virus can be contracted not only through airborne droplets, but also through household items. Even an ordinary pacifier can become a source of infection.
The disease develops very quickly, the incubation period is up to five days and the disease can be mild, moderate and very severe.
- In mild forms, there are no symptoms of intoxication; initially, an increase in temperature to 37.5º is observed. The oral mucosa becomes bright red and bubbles form, which is called the vesicle stage. Then they begin to burst, erosion of the oral mucosa occurs - this is the second stage of stomatitis. The rash becomes marbled in color as the disease begins to subside.
- Moderate and severe form The disease manifests itself in symptoms of intoxication in the child’s body. Before the rash occurs, general state The baby is deteriorating, there are signs of weakness, drowsiness, the child does not want to eat. At first, parents may think that it is an acute respiratory infection or a common cold. The lymph nodes enlarge, the temperature rises to 38º. When the rash begins to appear, the temperature reaches 38 - 39º, nausea and vomiting are possible. It can sprinkle not only the oral cavity, but also the surrounding tissues of the face. In addition, saliva becomes sticky and the gums become inflamed.
In every tenth child suffering from herpetic stomatitis, it can develop into chronic stage and relapses may occur periodically. Most often occurs in children aged 1.5 to 3 years.
View photos

[collapse]
How to treat stomatitis in children
It is clear that the question of how to cure stomatitis in a child is of great concern to all parents. First of all, you should contact your dentist. He will put accurate diagnosis, determining the nature of the disease, and only then appropriate therapy is prescribed. The task of any parent is to strictly follow all the instructions of the specialist, because children, especially small ones, will not be treated on their own.
For any form of stomatitis, it is important to adhere to a diet that excludes the intake of irritating foods; after each dose, rinse the mouth with herbal decoctions or antiseptics until the signs of the disease disappear (infants receive oral irrigation from a spray can).
The principles of treatment of stomatitis in children can be reflected as follows:
- Anesthesia. This can be a very convenient drug to use, Lidochlor Gel, the effect of which begins almost immediately after application to the surface of the cheeks and gums, and its duration of action is 15 minutes. Also, for pain relief for stomatitis, a three to five percent anesthetic emulsion is used.
- Treatment of not only affected areas, but also healthy tissue (to prevent damage) pharmacological drug, affecting the main cause of the disease (antiviral, antibacterial, antifungal, antiseptic).
Treatment of fungal stomatitis
To prevent the growth of fungus in the mouth, it is necessary to create an alkaline environment in the oral cavity. For this purpose, antiseptic solutions are used, which can be easily prepared at home. This:
- Soda solution (2–3 tsp per 250 ml).
- Boric acid solution.
- Blue.
You need to treat the oral cavity 2-6 times a day. In this case, the preparations are especially carefully applied to the cheeks and gums, since this is where accumulations of harmful microorganisms are located.
Another drug for the treatment of stomatitis is Candide solution. Its active substance destroys the walls of fungal cells. The course of treatment is carried out for 10 days. When the first signs of improvement appear, you should never stop treatment, otherwise, as in the case of taking antibiotics, the pathogen will develop resistance to the drug.
In rare cases, Diflucan can be used; it is prescribed to children in adolescence, the dosage is prescribed by a doctor.
Herpetic stomatitis: treatment
Just like with fungal stomatitis, they are excluded from the diet. sour foods, especially citrus fruits, canned food, salty and spicy foods. At herpes stomatitis in children, treatment includes local procedures and the use of general therapeutic agents:
The main way to treat stomatitis in a child is to take special antiviral drugs(acyclovir, viferon suppositories, viferon ointment). The disease is based on the herpes virus, which cannot be eliminated forever, but its activity can be suppressed through well-planned treatment. Immunostimulants are also recommended, because weakened immunity allows the disease to progress.
For rinsing, it is optimal to use Miramistin solution. You should rinse your mouth 3-4 times a day for 1 minute (by the way, after a short time after rinsing, you can immediately apply Viferon-gel, unless of course you are using gel and not suppositories). Miramistin can be used in young children as follows: moisten a gauze swab and treat the oral cavity with it, or spray the oral cavity from a spray nozzle (included).
During illness, the child needs semi-bed rest. Avoid walks and active games. Remember that stomatitis is an infectious disease that is highly contagious (it can be transmitted to others, especially weakened children and the elderly). Give the sick child a separate towel and your own cutlery, and try to reduce his contact with other family members.
It is very important to correctly distinguish herpetic stomatitis from aphthous stomatitis, because they are completely treatable various drugs. Therefore, it is advisable to treat stomatitis not on your own, but by contacting a pediatric dentist!
Treatment of aphthous stomatitis in children
For aphthous stomatitis in a child, treatment is aimed at accelerating the healing of aphthae and pain relief. Still widely used water solution methylene blue, or in common parlance - blue. The wounds are treated cotton swab, soaked in the solution, at least 3 times a day, preferably 5-6 times.
Treatment should also take into account possible reason, which caused the disease, because there are a lot of reasons and they all require different approach in treatment. Therefore, immediately after you discover aphthae in a child, you must immediately exclude it from the diet. allergenic products(honey, strawberries, chocolate, nuts, citrus fruits...), and it is also necessary to exclude hot, spicy, rough foods from the diet.
Antiseptic selection, antimicrobial agents often carried out by trial and error, since the course of any inflammatory process individually, for some, Lugol spray, Hexoral spray, or rinsing with Iodinol, Miramistin help, for others, Vinilin or methylene blue dye - Blue - helps a lot. Rotokan, an antiseptic with a healing effect (for mouth rinsing), has proven itself well.
Treatment of bacterial stomatitis
The mucous membranes of a one-year-old child are thin and easily injured, and the saliva does not yet contain enough enzymes to protect the body from external “enemies.” Therefore, if you have stomatitis, you should often rinse your mouth with solutions of chamomile, chlorhexidine, furatsilin, manganese, soda, strong tea or any other antiseptic.
The main treatment for bacterial stomatitis is chlorophyllipt (solution), oxolinic ointment. When the wounds begin to heal, they can be smeared with rosehip oil, propolis, aloe or Kalanchoe juice, vitamin A solution, and solcoseryl.
Treatment of stomatitis in children: Dr. Komarovsky
The famous pediatrician Dr. Komarovsky will tell you how to treat stomatitis in a child, depending on its type, and what can be done at home.
Prevention
The main way to prevent stomatitis is to follow the rules of hygiene. It is necessary to ensure that small children do not lick dirty objects or hands.
It has been noticed that children who are on breastfeeding, are less likely to suffer from all forms of stomatitis. Elders need to be explained how important it is to wash their hands, brush their teeth, and not put toys in their mouths in kindergarten.
Hardening, eating with a minimum amount of sugar and frequent exposure to fresh air will help strengthen the immune system, the child will not get sick, even if the infection gets into the oral cavity.
(Visited 19,316 times, 5 visits today)