Hysteroscopy is a method of treating and diagnosing diseases in the uterine cavity. It is used in gynecology as a low-traumatic method of examination and treatment of diseases of the uterus.
Types of hysteroscopy
There are diagnostic, control and surgical hysteroscopy.
Diagnostic hysteroscopy is performed with a hysteroscope - a special device equipped with an optical fiber. One part of the hysteroscope is inserted into the uterine cavity through the vagina and cervical canal, the other part remains in the doctor's hands. The device displays an image from the cavity on the screen, and the gynecologist can carefully examine the cervical canal and the uterine cavity from the inside, including the mouth of the fallopian tubes, and identify the presence pathological changes such as polyps.
There are various optical systems built into the hysteroscope. Some of them allow you to increase the image of the endometrium from the uterine cavity by 20 times. So the doctor can catch the slightest changes in the tissues of the endometrium and mucous cervical canal. Separate systems allow you to magnify the image a hundred times and even examine the cells of the epithelium. This is important in the diagnosis of neoplasms in the uterine cavity, if there is a suspicion of cancerous degeneration of endometrial cells.
The surgical hysteroscope has built-in surgical equipment in addition to the optical one. Under the control of optics, the gynecologist removes defects on the walls of the uterus, at the entrances to its appendages. Visual inspection of the cavity allows minimizing surgical intervention and removing defects as carefully as possible. As a result, the healing of endometrial tissues is faster.
Hysteroscopy has undeniable advantages over analogue methods of diagnosis and treatment:
- does not require a significant expansion of the cervical canal (the canal that connects the vagina to the uterine cavity), so there is no risk of cervical rupture during examination or treatment;
- the probability of damage to the mucous membrane of the walls of the uterus is extremely low, since all surgical procedures are carried out under visual control;
- pain during the diagnosis is practically absent, women may feel some discomfort during the expansion of the cervical canal, but not pain.
When is a hysteroscopy performed?
Hysteroscopy is one of the most frequently used instrumental methods gynecological diagnostics.
Diagnostic hysteroscopy is recommended in the first half of the cycle, when menstrual bleeding has already ended. Best time- fifth or sixth day female cycle. At this time, the thickness of the endometrial layer is minimal, and the doctor has the opportunity to examine the uterine cavity as best as possible. If an urgent examination of the uterine cavity is required, then it is carried out on any day, regardless of the menstrual cycle.
Diagnostic hysteroscopy is performed when there is a suspicion of such diseases:
- endometriosis (growth of the endometrium);
- adhesions in the uterine cavity
- frozen pregnancy at a short time.
Symptoms of these diseases can be heavy menstrual or intermenstrual bleeding, spotting of obscure origin, pain in the lower abdomen and lower back, inability to conceive or bear a child, pain or discomfort during intercourse.
Hysteroscopy is also recommended after surgery or medical abortion or with spontaneous abortion to detect the remains of the membranes of the fetus in the uterine cavity. It is also shown when a woman suffers from copious and painful menstruation in the absence of other visible symptoms.
Control hysteroscopy is used to assess the condition of the uterine cavity after treatment. For example, after a serious hormonal treatment hysteroscopy helps to evaluate changes in the endometrium.
Doctors resort to surgical hysteroscopy to treat various pathologies of the uterine cavity, for example, intrauterine polyps. It helps to remove neoplasms and the overgrown layer of the endometrium and at the same time minimally injure the organ.
What diseases are treated with hysteroscopy

Hysteroscopy can be used as independent method treatment or in combination with other methods. It is usually combined with curettage (curettage).
Therapeutic hysteroscopy is performed:
- with thickening (hyperplasia) of the endometrium;
- with regressive (frozen) pregnancy;
- ectopic pregnancy or when the fetus is located at the exit of the fallopian tubes;
- the formation of adhesions in the uterine cavity, for example, when the walls of the uterus grow together or the formation of partitions inside the organ;
- ingrowth of intrauterine contraceptives (spirals, loops, rings) in the tissue of the walls of the uterus.
Hysteroscopy can also be used for termination of pregnancy at early dates. In case of abortion in late pregnancy, hysteroscopy can be used as an auxiliary method.
Preparation for hysteroscopy
Preparation for hysteroscopy begins with an examination by a gynecologist. The patient is examined using a speculum, a swab is taken from the vagina for bacteriological culture. In some cases, a cervical swab may be required. This is necessary to detect infection.
Before hysteroscopy, the patient undergoes a series of laboratory research. The doctor prescribes tests after listening to the woman's complaints and preliminarily outlining possible diagnoses.
The doctor may prescribe an ultrasound of the uterus and appendages. Ultrasound will help assess the thickness of the mucous membrane, identify overgrown epithelium or inflammation, find neoplasms or a fetus during pregnancy. Hysteroscopy will help clarify the diagnosis made after the ultrasound.
If surgical hysteroscopy is prescribed under general anesthesia, you should not eat 6 hours before the procedure, and drink 4 hours before the procedure. This General requirements to operations carried out under general anesthesia.
Before surgical intervention the patient should talk to the anesthesiologist, tell about the existing allergies to medications. The anesthesiologist will select the drug and calculate the dose. You also need to consult a cardiologist and a therapist: they will appreciate general state women and risks from anesthesia and procedure.
The course of the procedure
Hysteroscopy is considered a minimally invasive method of examination and treatment, therefore it takes place without hospitalization. Diagnostic procedures are carried out without anesthesia. Patients who have been examined with a hysteroscope note the painlessness of the procedure. Sometimes, at the request of the patient, can be used local anesthesia.
Surgical hysteroscopy requires general anesthesia. An anesthetic agent is administered immediately before surgery, when the woman is already on the operating chair or couch.
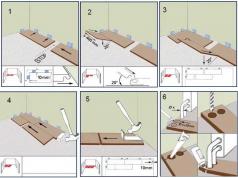
After anesthesia, the doctor opens the cervix. The degree of expansion required is small, since the device is quite miniature. After dilating the cervical canal, a part of the hysteroscope is carefully inserted into the cavity. This is a soft hollow tube or thin hard wire with a slight extension at the end. This extension contains the optical fiber and the light source. The other part of the hysteroscope remains in the hands of the doctor. The hysteroscope is connected to a large monitor, on which the image is displayed.
Through a hollow tube, a solution or gas mixture is introduced into the uterine cavity, expanding the uterine cavity and the mouth of the fallopian tubes. After expansion, you can better view each part of the inner shell of the organ and exits from it. The doctor gradually moves the hysteroscope inside the uterus, examining each part of it. It is possible to magnify the image a hundred times, which allows you to see the cells of the endometrium.
If hysteroscopy is performed for diagnostic purposes, this is the end of the procedure. If treatment is required, surgical equipment is inserted through the hysteroscope, pathological formations or an overgrown layer of the endometrium (hyperplasia) are removed. After the procedure is completed, the solution is removed from the uterine cavity. If required, the doctor inserts into the uterus medicinal product. Next, the hysteroscope is gently removed from the uterus through the vagina.
Rehabilitation
After diagnostic hysteroscopy, a woman may feel pulling pains of moderate intensity in the lower abdomen. So muscle layer The uterus reacts to an external intrusion of a foreign object. The sensations are similar to menstrual pain. If the sensations are very unpleasant, you can take an antispasmodic drug.
A small release of blood after manipulations with a hysteroscope is also considered the norm, especially after surgical removal pathological areas. Bloody issues should stop in 2-4 days. Women with poor blood clotting may need to prescribe hemostatic drugs.
After surgical hysteroscopy, the doctor prescribes antibiotics (to prevent postoperative inflammation). Other medications may be prescribed depending on the diagnosis.
For successful recovery after the procedure, a woman must observe a sparing regimen. Forbidden physical activity such as going to the gym or running for 2 weeks. You can not swim in the pool, take a bath - this can cause infection of tissues through water. The sauna should also be abandoned. Tampons during menstruation are best replaced with sanitary pads.
After hysteroscopy, a complete, vitamin-rich diet is shown. Food should be light, slightly laxative to prevent constipation.
A few days after the operation, the gynecologist conducts a follow-up examination. He finds out how tissue healing is going on, whether pathological formations have been completely removed. The examination also shows if there are any complications after the procedure.
Complications

Hysteroscopy is a minimally invasive method in surgical intervention in gynecology, so the likelihood of complications is rather low. Most possible complications hysteroscopy are:
- increased bleeding;
- endometritis (inflammation of the endometrium);
- violation of the menstrual cycle;
- rupture of the cervix;
- perforation of the uterine wall;
- incomplete removal of pathology, for example, polyps.
A slight disruption of the cycle after surgical hysteroscopy is allowed. So the body reacts to the operation, it needs time to recover before ovulation. The prolonged absence of menstruation after hysteroscopy should alert the patient, you should inform the doctor about this and find the cause.
Contraindications
Even the safest procedure has contraindications, and hysteroscopy also has them. This method should not be used during pregnancy, as it can cause miscarriage or injure the membranes.
In inflammatory and infectious diseases, hysteroscopy is not performed so as not to transfer the infection from the vagina to the uterine cavity and above. closure of the cervix and slime layer at the base of the cervix prevent the penetration of bacteria and fungi from the vagina. The hysteroscope can open the passage for infection and increase the infection.
With abundant uterine bleeding hysteroscopy is not performed, as it can increase bleeding, and the abundance of blood in the cavity will not allow the doctor to examine the organ properly.
Hysteroscopy - examination of the uterine cavity using fiber optics, similar to endoscopic examinations stomach. This is a diagnostic procedure in which therapeutic manipulations can be performed at the same time: perform a biopsy, remove mucosal polyps and dissect intrauterine adhesions.
Office hysteroscopy carried out at the appointment of a gynecologist. Using a flexible endoscope (fibrohysteroscope) with a diameter of up to 3 mm under local anesthesia without dilating the cervical canal, the doctor examines the uterine cavity. If the patient wishes, the doctor can show her a hysteroscopic picture. Most invasive diagnostic and therapeutic procedures are impossible due to high sensitivity uterus.
Diagnostic hysteroscopy performed in the operating room under intravenous anesthesia or sedation. The doctor inserts a thin optical instrument - a hysteroscope - to examine the uterine cavity. Often this procedure is combined with curettage of the uterine cavity, cervical canal and biopsy. Manipulation lasts from 10 to 20 minutes and in most cases does not require further inpatient stay. After hysteroscopy, the patient is observed by a gynecologist and an anesthesiologist for 2-3 hours, after which she can leave the clinic. For postoperative monitoring in the clinic "Medicine 24/7" single and double rooms are used.
Hysteroresectoscopy - not only diagnostic but also medical procedure. It is performed in the operating room under intravenous anesthesia. Manipulations in the uterine cavity are performed with micro-instruments, which are enclosed in a hysteroscope tube. During hysteroresectoscopy, a larger amount of intervention can be performed under targeted optical control using electrosurgical instruments. The duration of hysteroresectoscopy is usually at least 30 minutes.
Depending on the degree of complexity, hysteroresectoscopy can also be performed in a hospital. day stay, and in a round-the-clock hospital, if necessary, a longer observation of the patient. After hysteroresectoscopy performed in the hospital for one day, the patient is observed by a gynecologist and anesthetist for 2-3 hours, after which she is discharged.
When is hysteroscopy used?
Manipulation is considered minimally invasive, that is, it does not violate the integrity of tissues. Nevertheless, the uterine cavity is fundamentally closed, and therefore each insertion, especially with an apparatus, must be justified.
Hysteroscopy is not used for preventive examinations cavity, as is done with endoscopy of the gastrointestinal tract, manipulation is carried out if there is a suspicion of pathological process, which showed ultrasound and other types of tests. This is a diagnostic hysteroscopy.
The advantage of hysteroscopy with the possibility of carrying out a one-stage therapeutic and diagnostic measure is undeniable: take a biopsy and remove the pathological focus - a polyp, an internal fibroid node, a focus of hyperplasia, connective tissue adhesions - synechia. This type of examination is called medical. With tubal infertility, endoscopy of the endometrial cavity restores the patency of the tubes almost throughout.
Diagnosis of the pathology of the development of internal genital organs, finding out the cause of postmenopausal bleeding and infertility, even evaluating the effectiveness hormone therapy uterine pathology is also included in the spectrum of indications.
Feedback from our patients

When is a hysteroscopy performed?
The survey is most informative about a week, starting from the fifth day of menstruation. Endoscopy of the uterine cavity is not performed for inflammatory and infectious diseases of the genital area, for cervical cancer and stenosis.
During pregnancy or heavy bleeding, severe chronic diseases and thrombophlebitis procedure can lead to backfire and therefore also contraindicated.
Indications for hysteroscopy and hysteroresectoscopy
- Suspicion of the presence of intrauterine pathology - endometrial polyps, submucous myoma uterus, endometrial cancer, internal endometriosis (adenomyosis), remnants of the fetal egg and placenta after childbirth and abortion, malformations of the uterus, endometrial hyperplasia, intrauterine synechia.
- Preparation for IVF programs.
- Infertility, early miscarriages and regular miscarriage.
- Menstrual irregularities in women different periods life.
- The need to control the therapy of endometrial hyperplastic processes.
- Control diagnostic study uterine cavity after previous operations, chorionepithelioma and hydatidiform mole.
- Complications after natural childbirth
- Uterine bleeding.
Sometimes one examination in the gynecological chair is not enough, and the doctor directs the woman to additional examinations. One of these is hysteroscopy of the uterus. This method is informative and efficient. It can be used both for the diagnosis and treatment of various diseases.
Collapse
What is a hysteroscopy of the uterus?
This procedure in gynecology involves the introduction of a mini-camera into the organ, which is located on a special probe. The hysteroscope (this is what the device is called) also has LEDs, with the help of which all the mucous membranes are visible.
There is a surgical and diagnostic hysteroscopy. If the doctor's goal is to examine the endometrium of the uterus to confirm or clarify the diagnosis, this is a diagnostic procedure. If you need to remove neoplasms without incisions and punctures, then surgical hysteroscopy is done.
In what cases is the operation performed?
If you need to clearly find out the diagnosis of the patient, an examination of the uterus is performed, namely:
- when it is impossible to get pregnant;
- if intermenstrual bleeding is present;
- after systematic spontaneous abortions;
- with organ defects;
- if there is a suspicion of endometriosis, polyps, oncology.
Also performed for surgical purposes, for:
- elimination of placental remains after delivery;
- removal of neoplasms in the form of polyps, fibroids or adhesions;
- elimination of intrauterine rings, spirals, etc.
Types of hysteroscopy
As mentioned above, the procedure is of two types. Surgical and diagnostic. Let's consider in more detail.
Surgical
During this procedure, both optical and surgical equipment are used. Pathologies of the organ are treated in a radical way, while injuries are minimal. Here you need anesthesia for hysteroscopy of the uterus.

Diagnostic
When carrying out such manipulation, the integrity of the mucous membranes is not violated. The doctor examines the entire uterine cavity in detail. After this diagnosis, it is possible to confidently say whether a woman has a benign or malignant formation.
Contraindications for surgery
Cannot be used if present:
- an infectious disease;
- pregnancy;
- inflammation in the pelvic organs;
- stenosis of the uterine neck;
- bleeding.
Preparation for the procedure
How to prepare for a hysteroscopy of the uterus? Prior to the operation, the doctor must examine the patient in the gynecological chair using mirrors. This is necessary in order to study the condition of the vaginal walls and partially the cervix. In parallel with this, a bacteriological smear is taken, which will exclude various infections. If there are inflamed areas or the presence of infection, then hysteroscopy is not performed.
The woman herself needs:
- for one, two days to forget about sex;
- give up intimate gels and aromatic bath foams for a week;
- do not douche 5-7 days before the manipulation;
- wait 5 days using vaginal tablets, candles, creams, etc.;
- an enema should be given the day before the procedure;
- empty the urethra immediately before the procedure;
- in the morning it is forbidden to eat anything (if the procedure will be anesthetized).
also in without fail a woman undergoes tests before a hysteroscopy of the uterus:
- general (blood, urine);
- HIV research;
- Wasserman reaction.
In addition to laboratory tests, preparation for hysteroscopy of the uterus includes an examination by a therapist. After she does a fluorography, ultrasound diagnostics genitals and ECG. All the data obtained will help the gynecologist determine the auxiliary drug that is used during hysteroscopy. All are required preparations before surgery. On the basis of these will be selected postoperative treatment and a drug used in anesthesia.
Anesthesia for hysteroscopy
Before the operation, the doctor must decide on the choice of anesthesia. His choice will directly depend on the planned intervention and on the results of the preliminary examination.
Types of anesthesia
Used for hysteroscopy of the uterine cavity anesthesia:
- Local. An injection with an anesthetic drug is injected into the uterine cervix. Useful for diagnosis.
- General. Introduction intravenously. During medical sleep, the doctor performs all the manipulations.
- Regional. This concept refers to epidural anesthesia. The medicine must be injected into the region of the spine. At present this species the most popular.
Sometimes anesthesia is not used. The reason for this allergic reactions and other contraindications.
Let's consider each separately.
Local anesthesia
With the help of this type, only diagnostic hysteroscopy of the uterus is done. Under local anesthesia The procedure is performed on an outpatient basis. Before placing a hysteroscope in the uterine cavity, a specialist cuts off the uterine cervix with painkillers. After you need to withstand 10-15 minutes and carry out hysteroscopy. The best medicine for local anesthesia- lidocaine.
Keep in mind! After such anesthesia, severe pain will not be felt, but some discomfort will remain.
General anesthesia
Hysteroscopy under such painkillers is carried out in a hospital. If you need to remove a polyp, cyst, fibroid, adhesions or scrape the uterine cavity, local anesthesia can be used.
The drugs enter the body intravenously or maskally, after which the patient falls asleep. Preparations in the form of Propofol and Midazolam for injection into a vein and Sevoflurane and Isoflurane for inhalation can be used. They are the safest. After a woman comes out of drug sleep, she feels nausea, muscle soreness, weakness and dizziness. It all goes away within 24 hours.
Regional anesthesia
IN modern world regional anesthesia (spinal or epidural) is most preferable. The medicine is injected into the region of the spine. At the same time, the woman does not fall asleep, is in her right mind, but Bottom part her body loses sensation. To achieve normal (complete) anesthesia, you need to perform several manipulations. The hardest part is the insertion of the epidural tube.
Procedure technique and how long does it take?
Where and how is a hysteroscopy of the uterus performed? A woman enters the office and sits in a gynecological chair. Then comes the turn of the anesthesiologist. The specialist introduces a solution prepared in advance and monitors the patient's condition.

Then everything happens as follows:
- The doctor makes the treatment of the vagina, vulva and cervix with an antiseptic preparation.
- Produces an expansion of the cervical canal. For this, special metal expanders are used.
- He introduces a special tube on which there is a light source and a video camera. With the help of these devices, the organ cavity is examined. During the passage of the instrument through the neck, the organ is filled with air. This is necessary so that the uterine walls straighten out, and everything can be inspected without hindrance.
- After that, the specialist gradually examines all parts of the uterus. The image is displayed through the camera on the monitor. The picture is enlarged several times and this makes it possible to draw appropriate conclusions and make a clear diagnosis.
- If necessary, a tissue sample is taken for further laboratory testing.
- At the end, the uterus is cleaned of the auxiliary solution and the patient is taken out of anesthesia.
The duration of the session will take half an hour, sometimes 10-15 minutes longer. It all depends on the complexity of the process.
If hysteroscopy is performed for surgical purposes, then the procedure is performed under general anesthesia. After the operation, the woman will stay in the hospital for another two or three days.
First, the surgeon will examine the organ, then remove the endometrial polyp or other formation. Video operation is very popular nowadays. Hysteroscopy allows you to remove a pathological neoplasm without violating the integrity of the skin.
If hysteroscopy with curettage is performed, then it is also desirable general anesthesia and stay at the hospital for 2-3 days.
During diagnostic procedure there is no pain, but women with a high pain threshold may have some minor pain and discomfort. During surgical hysteroscopy, an anesthetic is usually used. In this case, the woman does not feel anything. If there is no anesthesia (for example, when taking a biopsy), then there are quite noticeable painful sensations.
On what day of the cycle is the manipulation done? Hysteroscopy is performed from the sixth to the tenth day of the menstrual cycle. During this period, the uterine membranes thin out, and this contributes to better visibility. If the procedure needs to be carried out urgently, then this happens on any day.
Recovery period after the procedure
IN postoperative period a woman may feel pain in the lower abdomen of a pulling nature. It resembles menstrual pain. With severe pain, you can take any painkiller or antispasmodic.
Discharge after hysteroscopy of the uterus is also a frequent occurrence. It is ok if they are not more than five days old. If the bleeding continues more and every day increases, and does not decrease, you should immediately seek medical advice. medical care.
Practice shows that surgical hysteroscopy affects the menstrual cycle. The first time there are failures.
The patient should not do douching during the recovery period, put tampons or suppositories in the vagina, take hot baths or go to baths and saunas, and also have sex. Needs to be done regularly hygiene procedures.
You can get pregnant no earlier than after 3-5 months. This time period is purely individual and is adjusted by the doctor.
Possible consequences and complications
Complications after hysteroscopy of the uterus can be different nature. If the procedure was carried out correctly with preliminary preparation, then Negative consequences are reduced to a minimum. There is only discomfort and minor symptoms mentioned above. But, alas, there are exceptions.
Anesthetic complications
Complications of this nature are associated with an incorrect assessment of the anesthetic risk, impaired anesthesia technique, and an allergic reaction to the drug used.
If anesthesia is not suitable for the patient, it may begin:
- tachycardia:
- dyspnea;
- cyanosis;
- pulmonary edema;
- vasospasm;
- hives;
- loss of consciousness.
With improper removal from general anesthesia, there is:
- chills;
- shiver;
- development of thrombophlebitis;
- apnea;
- muscle weakness;
- paralysis;
- increased heartbeat;
- cyanosis;
- breathing difficulties.
Sometimes, with the introduction of small doses, anesthesia does not give the desired result, after which the woman feels everything that happens.
Surgical complication
If tissues were touched during the procedure, then the following may occur:
- Bleeding that does not decrease, but increases.
- The occurrence of endometritis (due to tissue infection). Characterized elevated temperature, pulling pain in the lower abdomen, the presence of purulent bloody discharge.
- Perforation of the uterine wall. At the same time, the woman feels sharp pain in the lower abdomen, she feels sick, dizzy, blood pressure drops due to severe blood loss.
In any case, you should immediately consult a doctor.
Other kinds of complications
Also, a woman can observe discharge from the genital tract, which smells unpleasant and contains pus. This also indicates the presence of a pathology that cannot be delayed. A timely appeal to a gynecologist will prevent further negative consequences.
How much does the operation cost?
How much does hysteroscopy of the uterus cost in Moscow? It all depends on the distance from the center, the qualifications and experience of specialists, the popularity of honey. center. Consider three clinics.
Conclusion
How hysteroscopy of the uterus is done and what it is is no longer a secret. The procedure does not take much time, when using anesthesia it does not cause pain. There is nothing wrong with her if you find good clinic and experienced qualified doctor. You must first undergo an examination that will make it clear if there are any contraindications to hysteroscopy. If there are any changes in the discharge for the worse in the postoperative period or if there are sharp increasing pains in the lower abdomen, you should immediately contact a gynecologist.
Currently, for a full diagnosis in gynecological practice, clinical, laboratory, instrumental and endoscopic methods research. All this helps specialists to determine the status female body, identify serious pathologies and provide timely assistance that can save the patient's life.
Any patient has encountered an examination with the help of gynecological mirrors, but endoscopic research methods can cause a number of questions in women. So, a woman may be puzzled by what hysteroscopy is, how hysteroscopy is performed and what complications it can bring with it.
Types of procedure
Hysteroscopy is divided into 2 types: diagnostic (office) and surgical (resectoscopy). Each of them has significant differences.
Office hysteroscopy
The procedure implies the following actions:
- in the process, a visual examination of the uterine cavity occurs;
- the state of the mucous membrane of the uterus is examined;
- sample is taken biological material for histological examination;
- minor surgical manipulations are performed (removal of polyps, dissection of adhesions and septa).
- local anesthesia is used or is completely dispensed with;
- the duration of the procedure is 10–15 minutes;
- after hysteroscopy, a woman does not need to stay in a medical facility for a long time.
Thanks to hysteroscopy, you can carefully examine the cervical canal and the uterine cavity from the inside.
Hysteroresectoscopy
The main actions during hysteroresectoscopy: removal of pathological formations of various nature (large polyps, myoma nodes, adhesive bands), endometrial ablation (excision of the entire thickness), elimination abnormal bleeding from the uterus. Features of the procedure: carried out under general anesthesia (intravenous anesthesia), the duration of the procedure is from 30 minutes to 3 hours, the patient's hospitalization can last 2-3 days. The position of the patient during diagnostic (office) hysteroscopy does not differ from the position during hysteroresectoscopy. In both cases, manipulations are performed on a gynecological chair.
Indications and contraindications
Hysteroscopy is used against the background of such pathologies:
- with endometrial hyperplasia;
- benign growth of glandular tissue of the endometrium;
- neoplasms that occur in the myometrium;
- adhesive process in the uterus;
- oncopathology;
- malformations of the body and cervix.
Surgical hysteroscopy allows you to perform the following manipulations: excision and removal of connective tissue strands, elimination of the pathology of the bicornuate uterus, removal of benign growths of the glandular tissue of the endometrium and neoplasms of the myometrium, removal of the IUD from the uterine cavity, the remnants of an incompletely evacuated ovum, as well as the child's place, biopsy sampling .
Office hysteroscopy allows you to diagnose the impossibility of bearing a child, malformations of the reproductive organs, perforation of the uterine wall after abortion and cleansing. In addition, office hysteroscopy is performed for unstable menstrual cycle, gynecological bleeding of various nature, as well as, if necessary, to confirm or refute any diagnosis.
There are a number serious contraindications for hysteroscopy:
- inflammatory and infectious diseases of the reproductive organs during the period of exacerbation;
- bearing a child;
- cervical oncopathology;
- pronounced narrowing of the cervical canal;
- the general serious condition of the patient against the background of serious somatic diseases.
Hysteroscopy of the endometrium is considered to be a fairly gentle manipulation and actively replaces traumatic and dangerous interventions in the female reproductive system.
Preparation
During the preparatory period, the patient must do a number of studies:
- Standard gynecological examination using a mirror, as well as palpation of the uterus and its appendages.
- Vaginal smear. Thanks to the sampling of biomaterial in the urethra, cervical canal and vagina, it is possible to determine the state of the flora.
- Clinical Analysis blood, determination of the group and Rh factor, blood test for RW, hepatitis and HIV. Determine blood clotting (coagulogram).
- Macroscopic and microscopic examination of urine, which allows to identify kidney failure.
- Ultrasound of the pelvic organs (through the anterior abdominal wall or transvaginally).
- Electrocardiogram and fluorogram.
Before the planned hysteroscopy, the patient will be required to consult with related specialists: a general practitioner, a cardiologist, an anesthesiologist. In addition, she should tell her doctor if she has any drug allergy, if she is pregnant, and if she is taking permanent basis preparations.
Before conducting a hysteroscopy, a woman should adhere to the following recommendations: 2 days before the study, exclude sexual contact, a week before the scheduled procedure, do not douche and do not use store-bought gels and foams for washing.
One week before hysteroscopy, do not use medicinal vaginal suppositories(the exception is those prescribed by the gynecologist), with persistent constipation the day before the study, clean the intestines with an enema. Start taking 2 days before the procedure sedatives, if they were prescribed by a doctor, start taking antibiotics 5 days before hysteroscopy, if they were prescribed by a gynecologist.
On the morning of the procedure, you should stop eating and drinking. The patient must perform hygiene procedures, shave the pubic and groin, and immediately before entering the examination room, empty bladder. All unnecessary items (decorations, mobile phone) remain in the room. The patient should bring slippers, socks, a change of underwear, a bathrobe, as well as sanitary pads to the hospital, which will be needed after the procedure due to abundant vaginal discharge.

In order to better visualize the uterine cavity, it is expanded with the help of any medium.
Carrying out the procedure
Great importance what day do hysteroscopy. Planned hysteroscopy is best done from day 5 to day 7 of the cycle. At this time, the endometrium is thin and slightly bleeding. But sometimes the state of the endometrium is assessed in the luteal phase (after ovulation), approximately 3-5 days before the end of the cycle. In mature patients, as well as in emergency situations the time of hysteroscopy can be any.
After laying the patient on the gynecological chair, her thighs, external genitalia and vagina are treated with an antiseptic agent. A two-handed vaginal examination is performed to determine the location of the uterus and its size. lower segment The uterus is fixed with uterine single-tooth forceps, which pull the body of the uterus, align the direction of the cervical canal and determine the length of the uterine cavity. And then the cervical canal is bougienage with a Hegar dilator.
The hysteroscope is treated with an antiseptic and gently inserted into the uterine cavity enlarged with gas or liquid. During the inspection, its contents and size, shape and relief of the walls, the state of the entrance area to the the fallopian tubes. Upon detection of any foreign bodies, they are removed using instruments inserted through the hysteroscope channel. If necessary, a targeted biopsy is performed. The taken tissue sample is sent for histology.
According to indications, at the end of the procedure, the inner layer of the cervical canal and the uterine cavity can be removed. The anesthesiologist performs the final phase of anesthesia - brings the patient to consciousness. If there are no complications, then the patient is under the supervision of specialists for another 2 hours, and then she is transferred to the general ward. A hysteroscopic operation lasts an average of 30 minutes, and if laparoscopy is also performed, then the manipulation can last up to 3 hours.
Patients are often interested - how long after hysteroscopy can I do IVF? Experts say that these terms fluctuate and depend on the data obtained during hysteroscopy. Someone is prescribed IVF on the 10th day after hysteroscopy, and someone has to wait another six months for this moment. It all depends on the identified pathology, requiring varying degrees surgical intervention and therapeutic activities.
With the advent of minihysteroscopes, which are very small in diameter, Lately more and more often do hysteroscopy and even minor surgical procedures without dilating the cervical canal.

The medium used to expand the uterine cavity can be gas or liquid
Recovery period
After a hysteroscopic examination or surgical manipulations, complications are not excluded. In the postoperative period, the uterine mucosa and the natural volume of this reproductive organ, which was disturbed by artificial magnification during hysteroscopy. Against this background, after hysteroscopy, a woman can observe the following symptoms.
Pain syndrome. The pain is usually felt predominantly above the pubis. Feelings are expressed slightly and are somewhat reminiscent of pain during menstruation. In the first hours after the manipulation, the woman experiences pain, as during labor pains, as the uterus contracts and returns to its previous size.
Vaginal discharge. Due to damage to the endometrium, in the first hours after the procedure, there may be abundant bloody-mucous discharge. After the diagnostic procedure, discharge can be observed for 5 days, and after surgical procedures- up to 2 weeks.
A woman may experience general weakness and malaise. If a feverish condition appears, then one should, without delay, seek medical help. How long is the period full recovery after hysteroscopy, can vary greatly in each patient. As a rule, this takes up to 3 weeks on average. There are those who are pregnant naturally after hysteroscopy - this happened against the background of the removal of a polyp or atrophied endometrium.
If the patient adheres simple recommendations, That recovery period can be drastically reduced:
- In order not to provoke bleeding, the patient must refrain from intimacy with a man for 14 days.
- Monitor body temperature for a week, so as not to miss the complications that have arisen.
- From water procedures only hygienic shower is allowed. It is contraindicated to take baths, visit baths, saunas, swimming pools.
- Conscientiously take drugs prescribed by a doctor - antibiotics, analgesics, sedatives, vitamins.
- Follow the daily routine, eat right, play sports in a limited way.
When the patient has strong pain, bleeding opens and the body temperature rises sharply - all this is a serious reason to urgently seek help from a doctor.

Hysteroscopy itself does not affect the ability to conceive after the procedure.
Hysteroscopy of the uterus new method condition surveys reproductive system women using a special sensor. Timely determination of the reasons due to which conception cannot take place, and proper treatment are the key to successful pregnancy and childbirth. What is hysteroscopy, when is it necessary to undergo this procedure and what may be the consequences - the answers to these questions can be found below in the article.
What is this procedure and its types
Hysteroscopy of the uterus - examination method internal cavity uterus using a special device.
A hysteroscope is an illuminated instrument that is inserted into the internal genital organs. He perceives the image inside the uterus and transmits it to the screen, where it is analyzed by doctors.
- diagnostic:
- operational;
- control.
Diagnostic hysteroscopy is performed at the stage of diagnosis. reproductive system women are examined for the presence of pathologies, infectious and inflammatory processes or tumors.
Operative is carried out at the stage of treatment of diseases. Typically used during surgical operations on the uterus.
In parallel with the visual examination, surgical instruments are inserted into the uterine cavity and treatment is carried out.
Control hysteroscopy is performed during the rehabilitation of a woman after surgery or treatment.
The technique of carrying out does not differ from diagnostic, but at this stage there is no diagnosis. The doctor checks the effectiveness of the treatment prescribed by him.
Indications
 It is prescribed for suspected of the following pathologies:
It is prescribed for suspected of the following pathologies:
- inflammation of the endometrium in the uterine cavity;
- various types of adhesions and adhesions in the uterine cavity and fallopian tubes;
- remnants of the fetal egg or membranes after termination of pregnancy;
- oncological neoplasms;
- violation of the integrity of the walls of the uterus after cleaning or abortion;
- intrauterine pathology of fetal development;
- pathology of the menstrual cycle;
- abnormal development of the uterus;
- the occurrence of vaginal bleeding after menopause;
- infertility;
- monitoring the state of the uterine cavity after termination of pregnancy or hormone therapy.
Indications during surgery:
- benign tumors in the uterus;
- adhesions and synechia in the uterus;
- polyps:
- excessive growth of the endometrium;
- removal of the intrauterine device.
It is carried out only according to the indications of a doctor after comprehensive examination genital organs and testing.
Contraindications
 Contraindicated in some cases:
Contraindicated in some cases:
- inflammatory processes of the genital organs in a woman. It is also not recommended to carry out hysteroscopy after the treatment of inflammation, little time has passed;
- active pregnancy. In this case, hysteroscopy can be performed only in case of a threat of death;
- severe internal bleeding in the uterus;
- pathological narrowing of the lumen of the cervix in a woman;
- oncological neoplasm in the cervix;
- period acute course infectious diseases(any viral infections);
- insufficiency of the cardiovascular system;
- pathology of the development and functioning of the kidneys;
- hepatic pathologies.
How is the study going
How is hysteroscopy done? A question that confronts every woman who has received a referral for this type of examination or treatment.
Depending on the type this procedure can be performed with or without anesthetics.
If prescribed for the purpose of diagnosing a disease, anesthesia is not used. During the surgical type The procedure uses general anesthesia for the woman.
 Stages of implementation:
Stages of implementation:
- expansion of the lumen of the cervical canal;
- insertion into the cervix of the hysteroscope;
- the introduction of saline into the uterine cavity to expand it. Instead of saline, carbon dioxide can be used.
The next stages of the procedure depend on the purpose of its implementation.
Diagnostic hysteroscopy lasts no more than 10 minutes.
With the help of a special caper on a gyroscope, the doctor examines the organ from the inside and makes a medical conclusion.
Operative hysteroscopy is longer and its duration depends on the complexity of the operation.
Complications
After hysteroscopy of the uterus, negative consequences and complications may occur. Most often appear:
- trauma to the cervical canal;
- trauma to the uterus;
- infection of the genital organs of a woman;
- internal bleeding;
- individual allergic reactions to the components of the anesthetic.
 The incidence of complications after hysteroscopy is very low. It does not exceed 1% of cases.
The incidence of complications after hysteroscopy is very low. It does not exceed 1% of cases.
If a woman notices anxiety symptoms you need to seek medical attention as soon as possible.
Symptoms to watch out for:
- pulling pain in the lower abdomen;
- bleeding from the vagina;
- vaginal discharge has a sharp unpleasant odor;
- Wrong selection color - yellow or green;
- general malaise;
- nausea or vomiting;
- dizziness and visual disturbances;
- increase in body temperature;
- weakness and loss of consciousness.
Complications can arise from improper preparation for the procedure and individual features woman's body.
Features of the postoperative period
Recovery after hysteroscopy is quite fast.
As a rule, within 2-3 days after the procedure, a woman may experience discomfort in the abdomen and minor discomfort.
 This is considered normal and should not cause concern.
This is considered normal and should not cause concern.
What is prescribed after
Women who have undergone a diagnostic hysteroscopy may be prescribed an anesthetic to relieve unpleasant symptoms.
After surgical procedure Patients are prescribed antibiotics and anti-inflammatory medicines. In some cases, the doctor may recommend hormonal therapy.
Recovery after surgery lasts about 14 days, in the presence of complications it can reach 1 month.
For successful rehabilitation, it is important to follow all the prescribed recommendations of the doctor.
Hysteroscopy is a technique for diagnosing and treating many pathologies of the female reproductive system.
It has been successfully used in the treatment of infertility, inflammation and tumor processes in the uterine cavity.
It has a number of contraindications, therefore, before passing it, it is necessary to undergo an examination and consult a doctor.
Interesting video: what is hysteroscopy